Professional Documents
Culture Documents
Hesi Review For Maternity
Uploaded by
Steam LcOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hesi Review For Maternity
Uploaded by
Steam LcCopyright:
Available Formats
Watch a newborn APGAR test and find out what the scores mean.
Activity (muscle tone) 0 Limp; no movement 1 Some flexion of arms and legs 2 Active motion Pulse (heart rate) 0 No heart rate 1 Fewer than 100 beats per minute 2 At least 100 beats per minute Grimace (reflex response) 0 No response to airways being suctioned 1 Grimace during suctioning 2 Grimace and pull away, cough, or sneeze during suctioning Appearance (color) 0 The baby's whole body is completely bluish-gray or pale 1 Good color in body with bluish hands or feet 2 Good color all over Respiration (breathing) 0 Not breathing 1 Weak cry; may sound like whimpering, slow or irregular breathing 2 Good, strong cry; normal rate and effort of breathing CEPHALAHEMATOMA A cephalohematoma is a collection of blood under the periosteum. It is almost always a complication of childbirth. It most commonly occurs when the fetal head is forced through the birth canal; the head is propelled forward while the cervix grips the scalp tenaciously. This sliding, tearing force can tear tiny veins that nourish the periosteum from the bone side. This tearing of vessles causes bleeding (hemorrhage) under the tough covering of each bony plate (the periosteum), and a tense pocket of blood collects. This is apparently a painless process. The course of a newborn's uncomplicated cephalohematoma in itself is benign. The trapped blood cells break down and the component parts are reabsorbed into the system for recycling or disposal EYE PROPHYLAXIS Eye drops or ointment containing an antibiotic medication are placed in a newborn's eyes after birth. This is required by law to protect the baby from an unknown gonorrhea infection in the mother's body. Antibiotics are used in most hospitals. Another preparation, called silver nitrate, is sometimes used. The ointment or drops may cause a baby's eyes to appear cloudy and some newborns' eyes may become very irritated with redness or swelling. This is a temporary condition and the medication should not be washed or cleaned out of the eyes.
NEW BORN THERMOREGULATION neonates produce body hat by non shivering thermogenesis, this process requires increased oxygen and glucose consumption to burn brown fat, subcutaneous fat acts as an insulator and helps conserve body heat. A flexed position decreases exposed surface area and conserves body heat. Gestational age assessment BALLARD SCALE An assessment that evaluates six neuromuscular and six physical characteristic performed during the first few hours of birth. A score of 1 to 5 is assigned to each characteristic and the total score correlates to a gestational age, term babies get a score of 3 for each characteristic scores an 18 for the musculature assessment and a 18 for the physical characteristics: the total [points is 36 points coordinates to 38+ week gestation. PRETERM BIRTH born prior to 37 weeks and 7 days. ATTACHMENT/BONDING The process by which a parent comes to love and accept a child and a child comes to love a parent is referred to attachment. VERY important for mother and baby to bond after birth. Four Stages of Labor: First Stage Effacement and dilation of cervix - Latent Phase Cervical dilation is 1 to 4 cm. Uterine contractions occur every 15 to 30 min, are 15 to 30 sec in duration (mild intensity). Mother is talkative and eager to be in labor. Changes position without reminder. - Active Phase Cervical dilation is 4 to 7 cm. Uterine contractions occur every 3 to 5 min.; are 30 to 60 seconds in duration (moderate intensity). Mother becomes restless and anxious as contractions become stronger. Mother is usually serious, intense, has a need for increased concentration, will answer in short phrases only. May need reminders to change positions. - Transition phase Cervical dilation is 8 to 10 cm. Uterine contractions occur every 2 to 3 min, are 45 to 90 seconds in duration. (Strong intensity) Mother is working hard with intense concentration and will give one-word answers to questions only between contractions; anxiety increases, fears loss of control and abandonment, senses helplessness and may state I cant do this anymore. Interventions: Monitor maternal VS. Monitor FHR via ultrasound Doppler, fetoscope, or electronic fetal monitor. Assess FHR before, during, and after a contraction (normal is 120 to 160 beats/min. Monitor uterine contractions by palpation or monitor, determining frequency, duration, and intensity. Assess status of cervical dilation and effacement. Assess fetal station presentation and position by Leopolds maneuver. Assist with pelvic examination and prepare for a fern test. Assess the color of the amniotic fluid if the membranes have ruptured (meconiumstained fluid can indicate fetal distress.
Second Stage Expulsion of the fetus. Pushing stage. Extends from complete dilatation to Delivery. Cardinal movements- adaptations that the fetus undertakes to maneuver through the pelvis during labor and birth. Every darn fool in Rotterdam eats rotten egg rolls everyday. Engagement of the presenting part occurs Descent of the fetus into the pelvis Flexion of the fetal head; (descent and flexion often occur simultaneously) Internal rotation of the fetal head must take place to accommodate the maternal pelvis and occurs at the anterior-posterior diameter of the fetal head, the largest diameter of the fetus, aligns with the anterior-posterior dimension of the maternal pelvis Extension of the fetal head occurs as it comes under the maternal symphysis pubis and emerges from the vagina Restitution occurs at the fetal head turns 45 degrees to untwist the neck after the head has delivered. External rotation viewed as the head turns an additional 45 degrees as the second-largest fetal diameter, the lateral diameter of the fetal shoulders, rotates into alignment with the anterior-posterior dimension of the maternal pelvis. Expulsion occurs as the anterior shoulder slips beneath the symphysis pubis which facilitates delivery of the body. Third Stage: extends from the birth of the newborn to delivery of the placenta; average length is 30 minutes for nulliparas and multiparas. Mother is excited and relieved after babys birth; usually very tired. Fourth Stage: immediate recovery phase: includes the first 1 to 4 hours after delivery of the placenta. Tired, may find it difficult to rest because of excitement; eager to become acquainted with newborn.
Magnesium Sulfate: CNS depressant; relaxes smooth muscle, including the
uterus; used to halt preterm labor contractions; used for preeclamptic clients to prevent seizures. Adverse Reactions: resp; deep tendon reflexes (DTRs); hypotension; extreme muscle Weakness; flushing; urine output; pulmonary edema; serum magnesium levels >9mg/dl Nursing Interventions: Use controller pump for administration. Follow agency protocol For administration. D/C infusion and notify physician if adverse reactions occur. Monitor for resp ,12/min, urine output ,100ml/4hr (25-30ml/hr). Monitor DTRs. Monitor magnesium levels and report values outside therapeutic range (5 to 8 mg/dl)
PIH/Preeclampsia: A condition unique pregnancy; s/s develop only during pregnancy and Disappear soon after birth of the fetus and placenta. Risk factors: nulliparity, family hx, multifetal gestation, preeclampsia in previous pregnancy, preexisting medical or genetic condition ( chronic htn, renal disease, Type 1 diabetes) Methods used prevent preeclampsia: High-protein and low-salt diet; Calcium; Magnesium; Zinc; fish and evening primrose oil; antihypertensive drugs, including diruetics; antithrombotic agents; low dose aspirin; dipridamole; heparin; vit E and C.
Induction/Pitocin: Deliberate initiation of uterine contractions that stimulates labor. Oxytocin (Pitocin) stimulates the smooth muscle of the uterus and induses contraction of the myocardium. Promotes milk letdown. Routes of administration include intranasal. Intramuscular, and intravenous (IV). Uses: Induces or augments labor. Controls postpartum bleeding Promotes milk letdown and facilitates breastfeeding (intranasal route). Induces or completes an
abortion Adverse Reactions: Rare but may include allergies, dysrhthmias, changes in blood pressure, uterine rupture, and water intoxication. May produce uterine hypertonicity, resulting in fetal or maternal injury High doses may cause hypotension, with rebound hypertension Postpartum hemorrhage can occur because the uterus may become atonic when the medication wears off. Interventions: Monitor maternal VS q15 min. especially BP and hear rate, wt, I&O, LOC, and lung sounds. Monitor frequency, duration, force of contractions. Monitor FHR q 15 min. and notify health provider if significant changes occur. Do not leave the client unattended while the oxytocin is infusing. Administer oxygen. Monitor for hypertonic contractions. Stop medication if uterine hyperstimulation or a nonreassuring FHR occurs; turn the client on her side, Increase IV rate of the NS and administer oxygen and notify provider. Monitor for signs of water intoxication. Have emergency equipment available. Document time medication started, increased, maintained, and discontinued.
Prolapsed Cord: Umbilical cord is displaced, between the presenting part and the amnion or protruding through the cervix, causing compression of the cord and compromising fetal circulation. Assessment: mother has a feeling that something is coming through the vagina. Umbilical cord is visible and palpable. FHR is irregular and slow. Fetal heart monitor will show variable deceleration or bradycardia after rupture of the membranes. Interventions: Relieve cord pressure immediately. Place in trendelenburg or a modified Sims postion, or a knee-chest position. Elevate the fetal presenting part that is lying on the cord by apply finger pressure with a sterile glove hand. Do not attempt to push the cord into the uterus. Monitor the FHR. Assess the fetus for hypoxia. Administer oxygen by face mask to the mother. Prepare for emergency cesarean birth.
Hypovolemic Shock: Loss of circulatory fluid volume, which usually is caused by hemorrhage Assessment: Restlessness. Weak and rapid pulse. Hypotension. Tachypnea. Dull, clammy skin. Reduced urine output. Interventions: Elevate the legs. If pt had spinal anesthesia, do not elevate legs any higher than placing them on the pillow; otherwise, the diaphragm muscles could be impaired. Notify the physician. Determine and treat the cause shock. Administer oxygen, as prescribed. Monitor LOC. Monitor VS for pulse or decreased BP. Monitor I&). Assess color, temp, turgor and moisture of the skin and mucous membranes. Admin. IV fluids, blood, and colloid solutions as prescribed.
Contraction Assessment: The forces acting to expel the fetus. Effacement: Shortening and thinning of the cervix during the first stage of labor Dilation: Enlargement of cervical os and cervical canal during the first stage of labor. Measure intensity, frequency and duration. Vena Cava Syndrome p. 242 & 255 (also called supine hypotensive syndrome) The pressure of the gravid uterus compresses the vena cava when the mom is lying supine. Results in decreased blood flow to the right atrium and a decrease in blood pressure. Uteralplacental and renal perfusion is also decreased. S/S: pallor, dizziness, clammy skin, sweating, breathlessness, nausea What to do: position mom on right side, pillow under hips, knees slightly flexed until S/S subside and VS are WNL Diuresing effect p.528 (postpartum-begins within 12 hrs caused by estrogen) During pregnancy women accumulate excess tissue fluid, have increased blood volume and increased venous pressure in lower extremities. After birth, estrogen decreases, some blood volume is lost which decreases venous pressure in lower extremities, and body begins diuresis. Fluid is lost through perspiration (especially at night for first 2-3 days) and increased urine output. What to do: this is normal, but encourage mother to empty bladder or else Fundus can shift from midline. Neonatal resuscitation (I didnt find info in book or companion guide, here is a
link, or if you have trouble opening it, you can google it) www.som.tulane.edu/departments/peds_respcare/neores.html Infants of Diabetic mothers p. 308 companion guide Hormones secreted during pregnancy increase maternal resistance to insulin. Insulin requirements increase. In diabetics, pancreas cant secrete (any, or enough) insulin. Glucose levels rise. The moms insulin doesnt cross the placenta, but the glucose does. Fetal glucose levels rise. The babys pancreas responds by secreting more insulin, but it metabolizes the additional glucose and acts like a growth hormone. When the baby has increased insulin needs, surfactant production decreases. S/S in baby: Big baby, shoulder dystocia, birth trauma, enlarged internal organs: heart, liver and spleen. Hypoglycemia, hypocalcemia, hyperbilirubinemia, Resp distress syndrome, risk for congenital anomolies, particularly cardiac and spinal defects. What to do: assess for birth trauma to baby, respiratory, Assess blood glucose at 30 min, 1,2,4,6,9,12 and 24 hrs after birth. Treat hypoglycemia per order Teen pregnancy p. 47-48 The info in the book is brief, but it focuses on education and prevention. Consistently reinforcing abstinence or birth control is the most important component of effective sex education programs. Pregnant teens lack the maturity to avoid teratogens or to have prenatal and follow up care. The babies are at risk for abuse and neglect. Teens are already in a stressful developmental period and pregnancy introduces additional stress. Referrals to community and school resources for continuing education, parenting classes, prenatal care, finances, etc.
Diaphragm sizing p.57 companion guide (non-hormonal, barrier method) Flexible, dome shaped rubber device to cover the cervix to prevent sperm from entering cervix. Used with tsp. spermicidal cream or jelly around the rim and inside the cup. 94% effective with perfect use. 80% with typical use. Must be fitted by doc, dont share with anyone, replace annually. Problem: Risk for Toxic Shock Sydrome. Warning signs: temp 101.4, diarrhea, vomiting, weakness, fainting, muscle aches, sore throat, sunburn type rash, painful urination, abdominal or pelvic fullness, foul smelling vag d/c. What to do: education Use visual aids to demonstrate insertion and removal, encourage practice when healthcare provider is present so proper placement can
be checked. Can be inserted 4 hrs before, and left in 6 hrs after sex. If its inserted more than 4 hrs. before sex, use condom or apply more spermicide. If you want to do it again within 6 hrs. apply more spermicide without disturbing the diaphragm or some of the lil fellas may be successful in swimming up. Be sure to take it out at least once during a 24 hr period to avoid rist of TSS. Clean it with soap and water, observe for damage or thinning, dust with cornstarch, put in its case. Dont use during period, if you have abnormal vaginal d/c , or uti. Increases risk of TSS. Infants of substance abuse mothers p. 755-766 in book, p. 308 companion The book has information on so many drugs, but here is info on MOST COMMON. The focus on maternal substance abuse used to be identifying the baby who is going through withdrawals. However, not all babies will go through withdrawals, and sometimes withdrawals will begin after theyre discharged. Neonatal Abstinence Syndrome (NAS) assesses withdrawal S/S. Uses Neonatal Abstinence Scoring system p. 763 in book. Dont use term drug addicted baby use drugexposed NB instead. S/S of Neonatal Abstinence Syndrome (withdrawals): poor feeding, vomiting, diarrhea, excessive sucking, irritability, tremors, shrill cry, little sleep, excessive crying, nasal congestion, tachypnea, sweating, frequent yawning. Alcohol: FAS see pg. 757 for pic. Short eyelid opening, flad midface, thin , long upper lip. Developmental delays, microcephaly, attention deficits. Cocaine: preterm birth, small for gest age, microcephaly, poor feeding, irregular sleep, diarrhea, attention problems, hypersensitivity to noise, irritability Marijuana: Neonatal tremors, low birth weight, growth restriction. Uterine atony- a failure of the uterine muscle to contract firmly, it is the most frequent cause of excessive bleeding after child birth * important interventions for preventing excessive bleeding are good uterine tone and preventing bladder distention If uterine atony occurs the relaxed uterus distends with blood and clots, blood vessels in the placental site are not clamped off, and excessive bleeding occurs. Accurate visual estimation of blood loss is an important nursing responsibility. A perineal pad saturated in 15 minutes or less or pooling of blood under the buttocks is an indication of excessive blood loss requiring immediate assessment and intervention and notification of the physician. The nurse always checks under the mothers buttocks as well as the peri pad. Blood may flow between the buttocks onto the linens under the mother, although the amount on the peri pad
is slight: thus excessive bleeding goes undetected.
Miscarriage- (Text bk pg 353) The types of miscarriage include, threatened, inevitable, incomplete, complete and missed. All types of miscarriage can lead to infection except the threatened miscarriage. s/sx- uterine bleeding, uterine contractions or uterine pain are ominous signs in early pregnancy. Some women report a heavy menstrual flow, moderate discomfort and blood loss. Symptoms of a threatened miscarriage include spotting with a closed cervical os, with possible mild uterine cramping. Inevitable and complete miscarriages involve a moderate to heaving bleeding with an open os (tissue may be present with bleeding). An inevitable miscarriage may is often accompanied by rupture of membranes and dilation, products of the conception pass. An incomplete miscarriage involves the expulsion of the fetus with retention of the placenta. In a complete miscarriage all fetal tissue is passed, the cervix is closed and there may be slight bleeding. Mild uterine bleeding may be present. The term missed miscarriage refers to a pregnancy in which the fetus has died but the products of conception are retained in utero for up to several weeks. When a woman has vaginal bleeding early in pregnancy, a thorough assessment should be obtained, such as, chief complaint, V/S, last menstrual period, N,V, pain, bleeding or coagulation problems, LOC, emotional status, amniotic membrane status, vaginal discharge, EDB, and uterine activity. Evaluation of the hCG is used for the diagnosis of pregnancy and pregnancy loss. If infection is pregnant the WBC is greater than 12,000. D&C- Dilation and curettage is a surgical procedure in which the cervix is dilated and a curette is inserted to scrape the uterine wall and remove uterine contents. It is commonly used to treat inevitable and incomplete miscarriages. For late incomplete, inevitable, or missed miscarriages misoprostal can be given orally or vaginally to induce labor of the fetus. Special care may be needed of management of side effects of Prostaglandin suppositories such as nausea, vomiting and diarrhea. After evacuation of the uterus 10-20 units of oxytocin in 1000ml of fluid can be given to prevent hemorrhage. The woman is usually discharged after delivery or after the D&C when vital signs are stable, vaginal bleeding remains minimal and she has recovered from anesthesia.
Immunizations in pregnancy- immunizations with live or attenuated live viruses are contraindicated during pregnancy because of potential teratogenicity. Vaccines such as varicella or MMR. Vaccines consisting of killed viruses that may be administered during pregnancy include tetanus, diphtheria, recombinant Hep B and rabies vaccines. Post partum discharge teaching- patient to be aware of fever once at home, anorexia, chills, pelvic discomfort or pain, vaginal discharge that is malodorous. Be aware of vaginal discharge that has a fleshy odor of the odor is similar to that which occurs with a menstrual period. Pertaining to breasts the mother should be looking for localized heat and swelling to the breast. Pain and tenderness to the axillary nodes , elevated temperature and complaints of flu like symptoms. For pulmonary embolism be aware of dyspnea, tachycardia and tachycardia. Cough, lung crackles, hemoptysis, pleuritic chest pain , feeling of impending doom may be present. Nurses are strategically positioned to offer anticipatory guidance , assess the mental health of new mothers, offer therapeutic interventions and make referrals when necessary. Diabetic screening in pregnancy it is recommended that all women be screened for gestational diabetes, either by history, clinical risk factors or lab glucose testing. predisposing factors include: over 35 years, obesity, multiple gestation, family history of diabetes. Gestational diabetes occurs in pregnancy in clients not previously diagnosed as diabetic. Pregnant women should be screened for diabetes between 24 and 28 weeks gestation. A 3 hour oral glucose test (GTT) will be performed to confirm gestational diabetes mellitus. Gestational diabetes can frequently be treated by diet alone; however may need insulin. Women at high risk should be screened at the first prenatal visit and again at 24 to 28 weeks. Assessment: polydipsia, polyphagia, polyuria, blurred vision, weight loss, recurrent UTI, glycosuria and ketonuria. Rupture of Membranes- rupture of the membranes or (PROM) premature rupture of the membranes refers to the spontaneous rupture of the amniotic fluid membrane before the onset of labor. Gestational age usually determines the plan and interventions. When rupture of the membranes is before term and delivery will be delayed, infection becomes a risk. Assessment: 1) evidence of fluid pooling in the vaginal vault; nitrazine test positive. 2) amount, color, consistency and odor of fluid. 3) Vital signs, elevated temp. 4) Fetal monitoring: tachycardia may indicate infection.
Interventions: assist with tests to determine gestational age, monitor maternal and fetus status for signs of compromise and infection, administer ABX. Acrocyanosis- persistent blue discoloration to the extremities, most common in the hands but may occur in the and feet. This is normal for a newborn in the first few hours. Usually caused by the sluggish circulation of blood peripherally. Herpes SimplexMaternal Effects- A primary or recurrent infection. Painful vesicular genital lesions. Ceasarean delivery recommended during active lesion breakout. Fetal Effects- Disseminated or localized skin infection. CNS abnormalities Tx- Acyclovir (Zovirax) in pregnant clients has not been established; should be used in pregnant clients only when infection is life threatening Breastfeeding-Advantages of breast feeding is that there is a low cost. Milk production is stimulated by the decrease in postpartum estrogen production which allows release of prolactin for the pituitary Let down Reflex- Cause by action of oxytocin released from posterior pituitary, which stimulates myoepithelial cells around milk ducts and sinuses . Breast size has no relationshiop to successful breast feeding Inverted and retracted nipples- Women with inverted or retracted nipples can weat shields, which may help the infant latch onto the nipple. Diet- Avoid dieting, Add 500 calories to prepregnancy intake. Drink 8 glasses of non caffeinated beverages daily. Avoid smoking, drugs, ETOH, caffeine ( Stress is the most common reason for decreased milk supply Promote Rest Care of the Breast- Newborn should remain of first breast 10 min , then switch and suckle til satisfied. Use Warm water, Avoid drying soaps on nipples. Let nipples air dry for 15 min 2-3 times daily. No creams should be used. Engorgement- Nurse frequently, and manually express milk to soften areola before feeding. Wear a supportive bra. Take hot or warm showers( water over breasts promotes milk flow) Watch for s/s of mastitis ( commonly occurs when breasts arent emptied)
Positioning- Incorrect positioning of baby on breast in most common reason for sore nipples. Make sure baby has as much of the areola as possible in the mouth. Break suction with insertion of little finger into the babys mouth Fetal Position- Fetal station- location of presenting part in relation to midpelvis or ischial spines, expressed as cm above or below spine
Station 0 is engaged Station -2 is 2 cm above ischial spines Fetal presentation; the part of the fetus that present to the inlet. Shoulder-Acromion Breech- Buttocks Mentum- chin Fetal position- The relationship of the point of reference ( occiput, sacrum acromian) on the fetal presenting part ( vertex, breech, shoulder) to the mothers pelvis. Most common is LOA ( left occiput anterior). The point of reference on the vertex (occiputed) is pointed up toward they symphysis and directed toward the left side of the maternal pelvis. Cytotec- Misoprostol is used to prevent ulcers in people who take certain arthritis or pain medicines, including aspirin, that can cause ulcers. It protects the stomach lining and decreases stomach acid secretion. Misoprostol comes as a tablet to take by mouth. It is usually taken 4 times a day, after meals and at bedtime with food. Misoprostol is also used sometimes to treat ulcers and to induce labor. Misoprostol is used in combination with mifepristone to end an early pregnancy Fetal Distress- Compromise of the fetus during the antepartum period (before labor) or intrapartum period (birth process). The term "fetal distress" is commonly used to describe fetal hypoxia (low oxygen levels in the fetus). The concern with fetal hypoxia is it may result in fetal damage or death if not reversed or if the fetus is not promptly delivered. Fetal distress can be detected due to abnormal slowing of labor, the presence of meconium (dark green fecal material from the fetus) or other abnormal substances in the amniotic fluid, or via fetal monitoring with an electronic device showing a fetal scalp pH of less than 7.2.
Common discomforts during pregnancyN/V occur in 1st trimester. Caused by and increase in Hcg- Eat crackers before arising and avoid brushing the teeth immediately after arising. Eat small frequent meals. Drink liquids between meals. Urinary Frequency and Urgency- Drink lots of fluids during the day and limit at night. Void at regular intervals. Sleep on your side. Kegel excercises are good. Breast Tenderness- occurs all 3 trimesters. Wear supportive bra and avoid soap on nipple Vag discharge- occurs throughout- Use proper hygiene. Wear cotton undies. Avoid douching. Fatigue- occurs throughout. Rest often, regular exercise is great. Heartburn- in 2nd and 3rd trimesters. Eat small frequent meals, sit upright for 30 min following meals. Drink milk between meals. No fatty or spicy food. Ankle Edema- Elevate legs. Sleep on side. Wear supportive stockings. Avoid standing or sitting for long periods of time. Vericose veins- Wear supportive hose. Elevate feet when sitting. Dont cross legs. No tight clothing. Hemorroids- Soak in warm sitz bath. Sit on soft pillow eat high fiber. To avoid constipation increase fluids. Cardiavascular changes in mom: 1. Cardiac output increases 30-40% over nonpregnant output with an increase in pulseof 10-=15 beats/min. 2. Pulmonary and peripheral vasc resistance decreases 40-50%, lowering the bp throughout the 1st and 2nd trimesters: in the 3rd trimester, it begins to increase to pre-pregnant levels: postural hypotension may result as the pregnant uterus presses on pelvic and femoral vessels limiting blood return to the heart. 3. Supine hypotensive syndrome or vena cava syndrome results as the gravid uterus compresses the vena cava resulting in decreased blood flow to the right atrium and a decrease in bp. a. Sx : pallor, dizz, and clammy skin b. Prevent by lying on left side with a pillow under her right hip
4. Blood volume increases 45% over pre-pregnant levels a. Rbcs increase 18-30% depending on the amt or iron supplements b. Plasma increases by 50% c. The greater increase in plasma over RBCs results in physiologic anemia with decrease in hgb(10-14 gram/dl) and hct 32-42% the drop in hct is approx 5-7% Birth control 1. Mechanical methods: blocks sperm entering the cervix: some may have latex, watch for latex allergies 2. Male condom: a sheat made of latex, plastic or natural membranes placed over an erect penis to collect semen: 97% effectiveness with perfect use and 87% with typical use. a. Ed: check exp. Date b. Avoid using oil-based lubricants. Foam or water-based may be used c. Teach how to place condom d. After intercourse the erect penis should be withdrawn from the vagina while holding the rim o f the condom to prevent leakage. e. Inspect condom for tears or holes. f. Do not flush in toilet, discard in trash g. Comes in diff sizes and styles at low cost. 3. Female condom: a think, polyurethane sheath with flexible rings at each end, covers the cervix, lines the vagina and partially shields the perineum. a. Ed: insert the closed end of the condom into the vagina so the ring fits loosely against the cervix b. Partner needs to insert his penis into the open end leaving approx. 1 inch of sheat from the flexible ring outside the introitus c. After intercourse remove the condom before standing by squeezing and twisting the outer ring to close the sheath while gently pulling it out of the vagina
d. May be inserted up to 8 hrs before intercourse e. Clients can use this method if allergic to latex f. Both partners protected against STIs g. Breast-feeders can use h. Disadvantages: condom can twist or slip during intercourse, noisy during intercourse, altered sensation, insertion may be difficult or awkward. 4. Spermicides: a chemical barrier preventing pregnancy by killing sperm or neutralzing vaginal secretions and are available in a variety of forms including creams, gels, melting supp., foaming tabs, aerosol foams, and vaginal contraceptives film. a. Ed: apply spermicide inside the vagina close to the cervix before the penis is placed near the introitus. b. Must be applied with each act of sexual intercourse c. When used alone effects last no longer than 1 hr d. Can be irritating, and messy 5. Diaphragm; dome-shaped appliance mad of rubber with flexible rim that fits over the cervix, is used with spermicidal cream or jelly, and prevents sperm from entering the cervix. a. Ed: insert and remove the diaphragm. i. Apply tsp of spermicidal cream or jelly around the rim and inside the cup ii. Squeeze the sides of the diaphragm together, insert through the vagina, place the side of the device containing spermicide over the cervix and push the upper edge under the symphysis pubis. iii. Remove the diaphragm by grasping the rim to dislodge from the cervix and pull down to remove through the vagina b. Effective for up to 4 hrs before intercourse and should be left in place for atleast 6 hrs after. c. If diaphragm is placed for more than 4 hrs prior to intercourse or coitus is desired again within 6 hrs use a condom or additional spermicide should be used without disrupting the diaphragm.
d. Device needs to be removed atleast once during a 24hr period to decrease toxic shock syndrome. e. Clean with soap and water, inspect for tears, holes punctures, thinning. f. Store in case away from light and heat. Dust with cornstarch before. g. Do not use during menstrual can increase toxic shock syndrome. h. Assess for toxic shock: increase temp, diarreah, vomit, wkns, faint, muscle ache, sore throat, sunburn type rash, diff urination, abd or pelvic fullness, foul-vag dc. i. Refitting may be necessary j. Contraindicated with pts who have hx of Utis, toxic shock syndrome 6. Cervical cap a. A small thimble-shaped device made of soft rubber that fits over the cervix, is held in place by suction, and acts a s a barrier between sperm and the cervix . b. Ed: apply spermicide inside the cap c. Instruct the client to insert the cap at least 20 min but not longer than 4 hrs prior to intercourse d. Can be left in place up to 48 hrs e. Teach client to reapply spermicide with repeated intercourse is not needed. f. Do not use during menstruation, if abnormal dc present or sx of infection or inflammation present g. Contact pcp if sx develop: toxic shock syndrome h. Advantages same as diaphragm i. More difficult to fit, needs to be replaced annually, clients need to be rechecked for fit following pregnancy or 15lb wt gain or loss: effectiveness is reduced for parous women. j. If the device dislodges, or slips during sexual intercourse, the risk for contraceptive failure or acquiring a sexually transmitted infection is increased
k. Some clients may have difficulty inserting and removing the cervical cap. 7. Contraceptive sponge: a small, round polyurethane sponge containing nooxynal-9 spermicide. a. Ed: moisten the sponge with water prior to insertion into the vagina to activate the spermicide. b. Place the concave side of the sponge next to the cervix for a better fit. c. Leave the sponge in place for at least 6 hrs after intercourse d. Remove by pulling the polyester loop on the nonconcave side of the sponge downward and out of the vagina e. Provides protection up to 24 hrs f. Do not leave >24 to 30 hrs increased risk for toxic shock syndrome g. Low cost 8. IUD: achieved by triggering a spermicidal-type reaction with local inflammation of the endometrium, therby preventing fertilization a. Usually for woman who are stable monogamous relationship low risk for sti;s or pelvic inflammatory dz or norma uterine anatomy, nulliparous woman at low risk for STI or women with a hx of PID who are in stable monogamous relationship and have had a a pregnancy since the PID episode may also be considered on an individual basis b. Bleeding may occur for 2-6 wks after insertion c. First few menses after placement may be irregular d. f/u exam in 4-8wks e. check for string once a wk f. contact healthcare provider if she is exposed to a string or any warning signs for pain g. increased risk for pelvic inflammatory dz for the first 3 weeks following 9. oral contraceptives (birth control pills): act by inhibiting the release of an ovum, blocking the cyclical release of gonadotropin-releasing hormone, and changing cervical mucus.
a. When starting an oral pill, teach client to begin pills on the 1st Sunday after the onset of menstrual period and take one pill at the same time each day b. If client misses a pill at any time during the cycle, the missed pill should be taken immediately and the next pill taken at the regular time c. S/E: can be estrogen-related (such as thromboembolic dz, ha, fluid retention andnausea) or progestin-related (acne, increased HDL cholesterol level, depression, and hirsutism) d. Contact md if abdominal pain, chest pain, cough and or sob, HA, dizz, wkns, or numbness, blurring vision or speech problem, sever leg, calf or thigh pain e. May decrease effects of insulinan doral anticoagulants such as warfarin f. Contraceptive pill may be decreased by dilantin, tegretol, primidone, tpirimate, griseofulvin, rifampin, ampicillin, and tetracycline g. C/I: woman who have hx of thromboembolic or cardio disorders, breast cancer or estrogen-dependent neoplasms h. Subdermal implants: six silastic capsules containing levonorgeste, a progestin, implanted subdermally into the womens upper inner arm during the 1st 7 days of the menstrual cycle i. Prevent ovulation and stimulating production of thick cervical mucus, which prevents penetration of sperm j. ED: S/e spotting, irregular bleeding, amenorrhea, wt gain, HA, Fluid retention, mood changes, and depression k. Watch for s/s x infection l. Requires minor surgery to insert and remove the implants m. May be visible under the skin n. Higher failure rates have been reported in women >154 pounds in the 5th yr using 10. Long-acting progestin injections: Depo-Provera, an injectable hormone contains medroxyprogesterone aecetate 150mg, long-acting progestin that blocks the luteinizing hormone surge, prevents pregnancy by suppressing ovulation, and thickens the cervical mucus to prevent penetration of sperm with 97.7% effectiveness with both perfect and typical use.
a. Ed: s/e wt gain, HA, irregular menstrual, breast tenderness, depression b. Pt must follow the 3 mont injecgtion regimen to maintain effects. Subsequent dose must be given 80-90 days after the previous dose for continuous protection c. Contact md if abdominal pain, chest pain, cough and or sob, HA, dizz, wkns, or numbness, blurring vision or speech problem, sever leg, calf or thigh pain d. C/I in clients that have cardio disorder, breast cancer e. Fertility may be delayed up to 1 yr after stopping the method 11. Short acting combination injection: Lunelle contains medroxyprogesterone acetate an destradiol cypionate. a. ED: no back-up method needed if started within 5 days of menses b. Client returns every 22-33 days for next injection c. Early menses approx 2-3 wks after 1st injection d. Inflammation at site may occur 12. Transdermal contraceptive patch: releases small amts of estrogen and progestin to suppress ovulation a. Ed: s/e bleeding, breast tenderness, HA and skin reactions b. Remove patch once a wk on the same day and apply new patch to abdomen, buttock, upper outer arm or trunk for 3wks. Avoid placing the patch on areas with great deal of movement c. No patch used during week 4 and menstrual period typically occurs d. Not recommended for obese women e. Precaution same as oral contraceptives 13. Vaginal contraceptive ring: releases small amts of estrogen and progestin to suppress ovulation a. Ed: s/e vaginal infection, irritation, increased discharge, HA, or URI b. Insert vaginal ring and leave in for 3 wks
c. No ring used in wk 4 and the menstrual occurs d. Do not remove ring during intercourse, but can be removed for up to 3 hrs with no back up method e. Application once q 4 wks f. No special fitting g. c/I same as oral pill h. Postcoital contraception: emergency pill method and not be used on a regular basis i. Adm asap after unprotected intercourse. j. Usually within 72 hrs of intercourse (MAP) morning after pills k. An antiemetic can be given 1 hr prio to adm of this pill to control nausea, not given to pts with epilepsy. A/E; depression and suicidal thoughts 14. Surgical Methods: voluntary sterilization of the male or female a. Need consent b. Vasectomy: the vas deferens is resected through a small incisions made in each side of the scrotum resulting in blockage of the passage of sperm. Permanent procedure. i. Ed: procedure takes 15-20 min in clinical setting under local anesthesia ii. Do not drive immediatle after and remain with client for 24 hrs after iii. Minimal activilty for 48 hrs post iv. Avoid tubs for 48hrs v. Wear scrotal support for comfort vi. Use ice packs intermittently to dec. discomfort and swelling vii. Sitsz baths after 48hrs viii. No strenuous activity fo r1 wk
ix. Contact MD if fever >100.4, excessive pain, dysuria, redness, swelling , bruising, drainage, or skin edges of the incision that are not closed, bleeding at site. x. Sterility is not achieved until semen is free of sperm, takes 4-6 wks, use contraceptive method for back up xi. Semen samples needed for verification of sterility xii. Semen rechecked 6-12 months 15. Tubal ligation: fallopian tubes are accessed through 2 small incisions into the abd. And visualized using a laparoscope then cut, tied, cauterized, or banded to block the passage of sperm and prevent ovum from fertilization. a. Procedure takes approx 30 min under general or local anasth. b. Npo prior to procedure c. Pain is experienced for several days post . normal d. Avoid tubs for 48hrs e. Avoid strenuous activity, driving, lifting for 1 wk f. Contact MD if fever >100.4, excessive pain, dysuria, redness, swelling , bruising, drainage, or skin edges of the incision that are not closed, NV, difficulty defecation g. Risk for eptopic if defect in ligation h. Reversal may or maynot be possible Fundal Assessment * Involution: reduction in uterine size after delivery to the prepregnant state caused by uterine contractions that constrict and occlude underlying blood vessels at eh placental site o Enhance involution: good labor and delivery, breast feeding, early ambulation, complete expulsion of placenta and membranes o Slow involution: long labor and difficult delivery, anesthesia, grand multiparity, retained placental fragments or membranes, full bladder, infection, overdistended uterus. * Fundus: the top portion of the uterus: a palpable indicator of involution, if
contractions of the uterine muscles are interrupted a boggy uterus, one that is soft, relaxed, and likely to cause hemorrahage results. * Lochia rubra, lochia serosa and lochia alba: are discharges of blood and debris following delivery. Should not contain large clots; * Unexplained Increase amt of lochia rubra is not good. * After pains are intermittent uterine contractions following delivery , more painful in multiparous or breast feeders. * Cervix: soft, irregular and edematous: may look bruised with multiple, small lacerations. Closes to 2-3 cm after several days, admits a fingertip after 1 wk. * Assessment of the uterus post partum: place the nondominant hand on the lower uterine segment just above the symphysis pubis: the dominant hand palpates the top of the fundus o Determine the firmness and position of fundus midline of abd: fundus is 5 cm below umbilicus post delivery and rises to umbilicus in 6-12 hrs o Expect descent of 1 cm from umbilicus each postpartal day o Inspect abd incisions, cesarean delivery, or tubal ligation for REEDA: redness , edema, ecchymosis, DC, and approximation of the skin edges. o Teach patient to void q6-8 hrs after delivery. This will prevent hemorrhaging. If fundus is boggy massage fundus, but do not over massage. * Infertility (pg 38 in companion, pg 129 in text) Increases with the age of women esp. those over 40 y/o Diagnosis and treatment require considerable physical, emotional, psychologic, and financial investment over an extended period Assessment of FEMALE infertility: Obtain data relevant to fertility through interview and physical exam ID whether fertility is primary or secondary Note religious, cultural, and ethnic data b/c these may place restrictions on tests and treatments Obtain results from diagnostic tests
DX: FEMALE -Hysterosalpingogram (HSG) Detects UTERINE anomalies and tubal anomalies or blockage Sedation/anesthesia obtained Iodine based dye instilled through a catheter into uterus and tubes (CHECK ALLERGY TO SHELLFISH!) x-rays taken to document findings Postcoital exam Occurs 8-12hrs after intercourse, 1 or 2 days before expected ovulation 10ml syringe with catheter attached collects secretions from vagina Secretions are examined for signs of infection, number of active and nonmotile spermatozoa, sperm-mucus interaction, and consistency of cervical mucus look for normal motile sperm in cervical mucus Endometrial biopsy Endometrial tissue for examination Position client on exam table in stirrups Vaginal speculum inserted to visualize cervix, sharp tip catheter suctions tissue out Paracervical block given to reduce pain and decrease cramping Checking for luteal phase defect (lack of PROGESTERONE) PRE-OP Advise client of cramping discomfort BOTH during paracervical block admin and during tissue aspiration POST-OP Provide sanitary napkins as vaginal bleeding will occur, asses for sudden fainting caused by Hypotension induced by vagus nerve stimulation Basal Body Temp (BBT) resting body temperature Take oral temp q day prior to arising from bed and record it on a month-long graph A sudden dip occurs the day PRIOR to ovulation Followed by a rise of .5 to 1 degree indicating OVULATION Rise in temp will remain until menstruation begins *Fertility awareness* -- monitoring BBT and cervical mucus changes to detect ovulation (cervical mucus should have LOW viscosity)
Serum hormone testing Venous blood drawn to assess levels of FSH and LH, which are indicators of ovarian function! MALE Semen analysis Minimum of two analyses must be performed several weeks apart to assess male fertility Client ejaculates into clean specimen container (after 2-5 days of NO ejaculation) Semen examined w/in 2 hrs, keep away from extreme hot or cold If results in fertile range no further examination If results not in range, test repeated if below normal again, further examination needed. Implementation/Interventions/RN care: Psychosocial Guilt -- on behalf of the partner with the identified problem may regret past choices s/a sexual practices resulting in STDs Isolation -- occurs when couples feel different from those who have no problem conceiving, to avoid emotional pain, isolating from sources of support as a result Depression challenges ones sense of control and self-image, may become judgmental and angry with others Stress on the relationship Partners may feel unloved b/c of self esteem problems, Men often find it difficult to perform on demand for semen specimens, relationship may become for clinical rather than loving and supportive **Be considerate of cultural and religious views infertility treatments and techniques may not be accepted by a culture or religion, especially if it involves the male Assisted Reproductive Techniques (ARTs) are used often now in helping couples achieve having children be knowledgeable about how these techniques do bring on some ethical and legal factors for families SUPPORT the couple Encourage discussion and acceptance of feelings Ambivalence about a pregnancy after working so hard to achieve it is normal in the beginning
Increase couples sense of control as much as possible Suggest relaxation techniques, support groups, and other stress-mgmt methods Remember, only the person(s) involved can make the decision, but the nurse can help explore feelings Medications given to induce ovulation increase the risk for MULTIPLE gestations * Rhogam **GIVEN TO AN RH-NEGATIVE MOTHER WHO DELIVERS AN RH-POSITIVE FETUS AND HAS A NEGATIVE DIRECT COOMBS TEST. No need to give Rhogam to a mother with a positive coombs test (already sensitized) Prevention of Rh isoimmunization with next pregnancy No adverse reaction known RN care: *Given to Rh NEGATIVE women AFTER miscarriage, abortion, or any procedure or complication that increases the risk for maternal-fetal blood exchange (amniocentesis, PUBS, abdominal trauma) Routinely given at 28 weeks gestation to Rh-NEGATIVE with a negative antibody titer GIVEN postpartally to RH-negative mother after delivery or abortion when fetus is Rh-positive NEVER given to an infant or father Must be given within 72 HOURS of delivery Always given IM This is a BLOOD PRODUCT! -Must be checked by 2 nurses -Syringe must be returned to lab with label -Not given to a mother with positive indirect Coombs she is ALREADY sensitized to fetal cells and has developed antibodies *If receiving Rubella vaccine, test for rubella immunity at 3 months! (suppresses immune system)
* Terbutaline Stops preterm labor contractions! S/E: **TACHYCARDIA Take PULSE prior to admin and withhold med if pulse is not within parameters (Usually withheld if pulse is LESS THAN 120-140 Nervousness, tremors, HA, palpitations, tachycardia, chest pain, pulmonary edema, N/V, diarrhea, LOW POTASSIUM, hyperglycemia RN: Admin via IV Baseline ECG and lab values Monitor fetus continuously FHR should NOT exceed 180 Maternal VS q15min, PULSE should not exceed 140 Antidote = Propranolol (Inderal) MD if high pulse, FHR changes, abnormal lab values and signs of HF (dyspnea, dry cough, rales, JVD) * Vaginal discharge Lochia Rubra blood-tinged discharge, including shreds of tissue and decidua; Lasts 2-3 Days Postpartum Serosa Pale pinkish to brownish discharge lasting 1 week PP Alba thicker, whitish-yellowish discharge with leukocytes and degenerated cells; lasts up to 4 weeks PP **Check for presence of fragments in lochia to rule out uterine atony due to placental fragments *Suspect laceration is fundus is firm and bright-red blood continues to trickle Always check perineal pad AND under buttocks! C-section births have the SAME lochial changes
Heavy foul smelling lochia usually indicates infection * Cesarean section Pt may receive antacid to reduce the production of gastric secretions that damage lung tissue if aspiration Pre-op: Place wedge under one hip to displace uterus laterally Keep client warm with blankets Monitor and document fetal heart tones Post-op: Fundal height and consistency assessment may be difficult due to abdominal bandage and pain note if unable to determine, but gentle attempts should be made Asses temp and VS I&O Pain med as ordered Morphine (Duramorph), Fentanyl, Demerol Splinting of Abd., coughing deep breathing, incentive spirometer to prevent stasis of lungs Assess incisional healing Scrupulous perineum care and pad changes Asses lochia for foul odor (infection) Assess for paralytic ileus Early ambulation is key! At risk for infection, paralytic ileus, thromboembolism, resp complications, impaired maternal-infant bonding * Assessment of fetal heart rate (deceleration/acceleration/variability) FHR Most important indicator of the health of the fetal CNS
Detectable 10-12 wks by Doppler 15-20 wks by fetoscope 110-160 bpm = NORMAL Changes in FHR are the FIRST AND MOST important indicators of compromised blood flow to the fetus they require ACTION! Duration Length of each contraction from beginning to end Frequency beginning of one contraction to beginning of the next (3-5 contractions must be measured!) Intensity measure by external monitoring but in mmHg by internal monitoring AFTER amniotic membranes have ruptured ranged from 30mmHg (mild) to 70mmHg (strong) Obtain a baseline FHR Variability Short-term variability change in FHR from one beat to the next presence is reassuring sign Long-term variability averages 6-10 changes per min, ie. HR may average 140 bpm but may change from 137 to 149 during that minute when LTV can be evaluated **Nonreassuring Warning Signs: Variability FHR is absent or minimal STV is absent LTV is minimal Causes Hypoxia, Acidosis, maternal drug ingestion (esp. MAG Sulfate), fetal sleep Accelerations Caused by sympathetic fetal response Occur in response to fetal movement Indicative of a reactive, healthy fetus Early Decelerations Benign pattern caused by HEAD COMPRESSION Heart rate slowly and smoothly decelerates at beginning of contraction and returns to baseline at end of contraction Monitor and document progress of labor Bradycardia FHR is below 100 causes: Fetal hypoxia, medication induced, maternal hypotension, fetal heart block, prolonged umbilical cord compression Tachycardia FHR above 160 Causes: early sign of fetal hypoxia, fetal anemia, dehydration, maternal infection/fever, maternal hyperthyroid disease, medication-induced (terbutaline)
Variable deceleration Most common periodic pattern Caused mainly by CORD COMPRESSION Can indicate rapid fetal descent Occasional variable is usually benign RN: change maternal position (place on LEFT side) stimulate fetus if indicated D/C oxytocin if infusing Admin 10L of O2 by face mask Vag exam to check for cord prolapsed Report findings SEVERE Variable decelerations FHR below 70bpm lasting longer than 30-60secs slow return to baseline decreasing or absent variability LATE DECELERATIONS Potentially disastrous sign Uteroplacental Insufficiency RN: Immediately turn client on SIDE D/C oxytocin if infusing Admin O2 10L by face mask Elevate legs to increase venous return Determine presence of FHR variability Important to remember!! *Early Decels = HEAD COMPRESSION and fetal descent -- check progression of labor *Late Decels = BAD! Uteroplacental insufficiency *Variable decelerations = Cord Compression change maternal position, D/C oxytocin, admin O2, notify MD *If cord prolapsed is detected position mother to relieve pressure on the cord (knee-chest position, or left side) OR push the presenting part off of the cord until IMMEDIATE c-section can be accomplished * Epidural Given in 1st or 2nd stage of labor to deaden pain of contractions **Causes HYPOtension so monitor for that! Prehydrate pt to counteract hypotension First signs of effectiveness is warmth and tingling in ball of foot or big toe! May result in assisted (forceps or vacuum) delivery b/c of inability to push effectively in 2nd stage of labor If hypotension occurs Turn pt on her left side, admin O2, increase IV rate *metallic taste in mouth and ringing in ears can be sign that med is in bloodstream *N/V among first signs of hypotension
You might also like
- BDSM Checklist ShevahDocument208 pagesBDSM Checklist Shevahslackjack86% (36)
- The Anatomy of BreathingDocument6 pagesThe Anatomy of BreathingmihaiylaNo ratings yet
- Ebook PDF The Phlebotomy Textbook 4th Edition PDFDocument41 pagesEbook PDF The Phlebotomy Textbook 4th Edition PDFmelody.bowers405100% (29)
- Hesi Hints MaternityDocument4 pagesHesi Hints MaternityThomas Stewart91% (11)
- NCLEX Test Taking TipsDocument3 pagesNCLEX Test Taking TipsjrilleraNo ratings yet
- Garlic - Toxic and A Brain Synchronization DestroyerDocument6 pagesGarlic - Toxic and A Brain Synchronization Destroyerxreader0No ratings yet
- NCLEXDocument95 pagesNCLEXrikkapupuNo ratings yet
- 2009 HESI Practice - Comprehensive ExamDocument26 pages2009 HESI Practice - Comprehensive ExamQueennitaNo ratings yet
- Gastrointestinal: Nclex-Rn ReviewerDocument34 pagesGastrointestinal: Nclex-Rn ReviewerJohnasse Sebastian NavalNo ratings yet
- NCLEX Questions and AnswersDocument16 pagesNCLEX Questions and AnswersJoslyn Gross100% (3)
- Med Surg Proctored Concept GuideDocument4 pagesMed Surg Proctored Concept GuideKiayaraNo ratings yet
- Labor and DeliveryDocument56 pagesLabor and DeliveryeliNo ratings yet
- DDocument56 pagesDDarren Balbas100% (1)
- Peds Exam 1 ReviewDocument19 pagesPeds Exam 1 ReviewMahreen UmatiyaNo ratings yet
- New Text DocumentDocument3 pagesNew Text DocumentTro Wact100% (1)
- Peds ATI TakeawaysDocument4 pagesPeds ATI TakeawaysNiki95% (19)
- Hemorrhagic Stroke CBLDocument106 pagesHemorrhagic Stroke CBLJessica NadiaNo ratings yet
- NCLEX RNdemo PDFDocument14 pagesNCLEX RNdemo PDFHarrington KalumbwaNo ratings yet
- NCLEXstudyguidevmDocument31 pagesNCLEXstudyguidevmAnonymous vqG0paWG100% (1)
- NCLEX-RN Test Plan (Detailed Candiate Version)Document62 pagesNCLEX-RN Test Plan (Detailed Candiate Version)Filipino Nurses CentralNo ratings yet
- Obstetric Questions: Please State Whether The Following Statements Are TRUE or FALSEDocument8 pagesObstetric Questions: Please State Whether The Following Statements Are TRUE or FALSEjulialeo90% (10)
- Every Monday in May Live Facebook ReviewDocument4 pagesEvery Monday in May Live Facebook ReviewChelle RocoNo ratings yet
- Maternal and Child NursingDocument13 pagesMaternal and Child NursingCarrel Relojero CarlosNo ratings yet
- MaternityDocument4 pagesMaternityErica Sanchez100% (5)
- Ati Comp ExitDocument53 pagesAti Comp Exitpretty shiks100% (1)
- Delegation To LPN & Nap: Prepared byDocument7 pagesDelegation To LPN & Nap: Prepared byJamilla louise Valencia100% (1)
- Hesi Community Health ExamDocument12 pagesHesi Community Health ExamAna BienneNo ratings yet
- NCLEX Tips On ProceduresDocument4 pagesNCLEX Tips On Proceduresromin_soledad100% (7)
- Hesi ReviewDocument59 pagesHesi ReviewKrista Howe100% (3)
- Obstetrics Nursing Questions Answer KeyDocument13 pagesObstetrics Nursing Questions Answer Keyicy431100% (2)
- Capstone Final ExamDocument19 pagesCapstone Final ExamEileen Arboleda100% (3)
- Antidote: Calcium Gluconate or Calcium Chloride: Excessively Frequent Uterine Contractions During PregnancyDocument3 pagesAntidote: Calcium Gluconate or Calcium Chloride: Excessively Frequent Uterine Contractions During PregnancyCohort Six100% (1)
- Hns Nclex-Rn Prep: Bilingual Prep for the Bilingual NurseFrom EverandHns Nclex-Rn Prep: Bilingual Prep for the Bilingual NurseNo ratings yet
- Stages of LaborDocument3 pagesStages of Labormiss RN100% (8)
- NATIONAL COUNCIL LICENSURE EXAMINATION FOR REGISTERED NURSES (NCLEX-RN): Passbooks Study GuideFrom EverandNATIONAL COUNCIL LICENSURE EXAMINATION FOR REGISTERED NURSES (NCLEX-RN): Passbooks Study GuideNo ratings yet
- Study Guide HESI CommunityDocument29 pagesStudy Guide HESI CommunityBeth Ann100% (1)
- Pediatric DiseasesDocument10 pagesPediatric DiseasesKira100% (4)
- Positioning principles and protocols for common medical conditionsDocument48 pagesPositioning principles and protocols for common medical conditionsShazaNo ratings yet
- Ob Ati StudyDocument22 pagesOb Ati Studylpirman0580% (5)
- OB Answer KeyDocument23 pagesOB Answer Keyicy431No ratings yet
- Nclex-Rn Test Study GuideDocument199 pagesNclex-Rn Test Study GuideSusan BensonNo ratings yet
- ATI PN Maternal Newborn NotesDocument13 pagesATI PN Maternal Newborn NotesDiamond Blackwell100% (6)
- AtiDocument4 pagesAtirunnermn88% (8)
- Medsurg ATIDocument7 pagesMedsurg ATIloveoverpride12% (17)
- Pediatric RemediationDocument5 pagesPediatric RemediationAlvin L. Rozier67% (3)
- Pediatric Drug ReferenceDocument54 pagesPediatric Drug Referenceapi-3712326100% (1)
- Pediatric Doses For Commonly Used OTCsDocument7 pagesPediatric Doses For Commonly Used OTCsCharles Xavier KimNo ratings yet
- NclexDocument7 pagesNclexanon-834511100% (2)
- Pedia NotesDocument47 pagesPedia NotesArgee AlonsabeNo ratings yet
- Maternity NursingDocument41 pagesMaternity Nursingbajaoc100% (1)
- DBQ FOCUS: Columbian Exchange: Document-Based Question FormatDocument5 pagesDBQ FOCUS: Columbian Exchange: Document-Based Question Formatbaruc barranco50% (2)
- NCLEX Success PrayerDocument377 pagesNCLEX Success Prayerjkrix100% (2)
- Maternity NursingDocument28 pagesMaternity Nursingja100% (11)
- MSDS KleratDocument4 pagesMSDS KleratSadhana Sentosa100% (2)
- Ati PedsDocument13 pagesAti PedsVanessaMUeller100% (8)
- Placenta PreviaDocument6 pagesPlacenta Previamiss RN93% (14)
- Ati Community Health Study GuideDocument6 pagesAti Community Health Study Guidelpirman05100% (5)
- The Surgical Team: Intraoperative NursingDocument4 pagesThe Surgical Team: Intraoperative NursingGiselle Chloe Baluya icoNo ratings yet
- Peds HESI Study GuideDocument5 pagesPeds HESI Study Guidemscostello985367% (9)
- Maternal Newborn AtiDocument4 pagesMaternal Newborn Atiapi-243590841100% (3)
- Pediatric HESI Review 2016Document9 pagesPediatric HESI Review 2016Brittany78% (9)
- NCLEX Study GuideDocument2 pagesNCLEX Study GuideLogin Nurse100% (1)
- Hesi v4 Sample 2015Document2 pagesHesi v4 Sample 2015james67% (3)
- NCLEX Study GuideDocument35 pagesNCLEX Study Guidedchirinos90100% (1)
- Ati RN 2016 Proctor PedsDocument6 pagesAti RN 2016 Proctor PedsStan Tan50% (2)
- Newborn Assessment and CareDocument17 pagesNewborn Assessment and CareMatthew Lee100% (1)
- Ob Exam Study Guide The Bible 001 49pgsDocument50 pagesOb Exam Study Guide The Bible 001 49pgsVin Lorenzo CampbellNo ratings yet
- Pharm Review For Hesi From JanaDocument8 pagesPharm Review For Hesi From Janacheyenne.black5205100% (1)
- Anatomy and Physiology Digestive System GuideDocument214 pagesAnatomy and Physiology Digestive System Guideyisel56100% (6)
- When Can I Register For The NCLEX-RN Exam?Document3 pagesWhen Can I Register For The NCLEX-RN Exam?mimNo ratings yet
- U World ReproductiveDocument5 pagesU World ReproductiveAce LabosNo ratings yet
- Exit Hesi Study Plan #1 10 5 11Document1 pageExit Hesi Study Plan #1 10 5 11mmgoodall22100% (1)
- OB Version BDocument6 pagesOB Version Bisapatrick8126100% (1)
- Maternal Hesi Q RDocument1 pageMaternal Hesi Q RSho Ngo25% (4)
- My Nclex Study GuideDocument4 pagesMy Nclex Study GuideLogin Nurse100% (1)
- Practical nursing jeopardy game questions and answersDocument29 pagesPractical nursing jeopardy game questions and answersfairwoods80% (5)
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideFrom EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNo ratings yet
- FL 341 CDocument1 pageFL 341 CSteam LcNo ratings yet
- FL 342 InstructionsDocument5 pagesFL 342 InstructionsSteam LcNo ratings yet
- BlankDocument1 pageBlankSteam LcNo ratings yet
- FL 342 InstructionsDocument5 pagesFL 342 InstructionsSteam LcNo ratings yet
- (247588053) Risk Management, 2nd Edition, BookDocument53 pages(247588053) Risk Management, 2nd Edition, BookSteam LcNo ratings yet
- Mosby S Pathophysiology Memory NoteCardsDocument192 pagesMosby S Pathophysiology Memory NoteCardsSteam Lc86% (7)
- Biliary Tract and PancreasDocument10 pagesBiliary Tract and Pancreassarguss14No ratings yet
- Female Genital TractDocument5 pagesFemale Genital Tractsarguss14100% (1)
- BlankDocument1 pageBlankSteam LcNo ratings yet
- Kidney Part 2Document9 pagesKidney Part 2Steam LcNo ratings yet
- Endocrine System - Part 3 (Robbins)Document10 pagesEndocrine System - Part 3 (Robbins)sarguss14No ratings yet
- US Army Medical Course - Environmental Injuries MD0548Document86 pagesUS Army Medical Course - Environmental Injuries MD0548billcloNo ratings yet
- US Army Medical Course MD0556-100 - Basic Patient Care ProceduresDocument122 pagesUS Army Medical Course MD0556-100 - Basic Patient Care ProceduresGeorgesNo ratings yet
- US Army Medical Course MD0851100 Anatomy and Physiology Related To Clinical PathologyDocument113 pagesUS Army Medical Course MD0851100 Anatomy and Physiology Related To Clinical PathologySteam LcNo ratings yet
- Neonatal Assessment Guide Independent StudyDocument10 pagesNeonatal Assessment Guide Independent StudyoapsdoaksdokaNo ratings yet
- L 5 Pediatric History Clinical Examination 08Document44 pagesL 5 Pediatric History Clinical Examination 08Steam LcNo ratings yet
- Maternal Health Nursing SkillsDocument279 pagesMaternal Health Nursing SkillsNacel CelesteNo ratings yet
- Doreen NewbornDocument18 pagesDoreen NewbornSteam LcNo ratings yet
- Nle Review MaternitynsgDocument35 pagesNle Review MaternitynsgRitamariaNo ratings yet
- Ob Study PacketDocument93 pagesOb Study PacketJamie ParkerNo ratings yet
- Hypoxia: Deficiency in Oxygen Delivery or Utilization at Tissue LevelDocument37 pagesHypoxia: Deficiency in Oxygen Delivery or Utilization at Tissue LevelandrenicholastobingNo ratings yet
- Lesson 3 Gas ExchangeDocument7 pagesLesson 3 Gas ExchangeBrent PatarasNo ratings yet
- Build A Virus Lesson Plan 2 20 12Document8 pagesBuild A Virus Lesson Plan 2 20 12M9094No ratings yet
- Nervous System WorksheetDocument3 pagesNervous System WorksheetaNo ratings yet
- Drug Dosage FormsDocument56 pagesDrug Dosage FormsHamid HamidNo ratings yet
- Family Case Study of the Bucasas FamilyDocument27 pagesFamily Case Study of the Bucasas FamilyKristel AnneNo ratings yet
- Animal Science Thesis ExamplesDocument4 pagesAnimal Science Thesis Examplesnikkismithmilwaukee100% (2)
- Blood Lectures 2014 PIO 205Document84 pagesBlood Lectures 2014 PIO 205Philip Abayomi VincentNo ratings yet
- PSM 2 PypDocument186 pagesPSM 2 PypsuriNo ratings yet
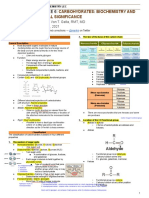
- Carbohydrates Clinical SignificanceDocument10 pagesCarbohydrates Clinical SignificanceMay Ann EnoserioNo ratings yet
- Risk factors of diabetic retinopathy and vision threatening diabetic retinopathy and vision threatening diabetic retinopaty based on diabetic retinopathy screening program in greater bandung, west java.astriDocument14 pagesRisk factors of diabetic retinopathy and vision threatening diabetic retinopathy and vision threatening diabetic retinopaty based on diabetic retinopathy screening program in greater bandung, west java.astriSi PuputNo ratings yet
- Investigation of Blood Culture Using BACTEC SystemsDocument36 pagesInvestigation of Blood Culture Using BACTEC SystemsGregorio De Las CasasNo ratings yet
- Gastro Intestinal Tract: Dr. Indu MandalDocument18 pagesGastro Intestinal Tract: Dr. Indu Mandalankit ahirNo ratings yet
- Cara Hitung MPAP, CO, dan Penilaian Regurgitasi dan Stenosis Valve JantungDocument6 pagesCara Hitung MPAP, CO, dan Penilaian Regurgitasi dan Stenosis Valve JantungwinNo ratings yet
- Round Cell Tumors - Classification and ImmunohistochemistryDocument13 pagesRound Cell Tumors - Classification and ImmunohistochemistryRuth SalazarNo ratings yet
- 4 Agroecology IPMDocument16 pages4 Agroecology IPMZahara AmalinaNo ratings yet
- Turbinate HypertrophyDocument8 pagesTurbinate HypertrophyNurhayati Akila JNNo ratings yet
- 30802Document16 pages30802YAMINIPRIYANNo ratings yet
- The "Wits" Appraisal of Jaw Disharmony - Wits PDFDocument14 pagesThe "Wits" Appraisal of Jaw Disharmony - Wits PDFCynthia AlfaroNo ratings yet
- GENERAL EDUCATION Test Material 198 ItemsDocument13 pagesGENERAL EDUCATION Test Material 198 ItemsBM Ayunnie VlogNo ratings yet
- Judi Januadi Endjun: Gatot Soebroto Army Central Hospital/ Medical Faculty, University of Indonesia ISUOG, Bali, 2009Document66 pagesJudi Januadi Endjun: Gatot Soebroto Army Central Hospital/ Medical Faculty, University of Indonesia ISUOG, Bali, 2009Judi Januadi Endjun, MD, ObsGynNo ratings yet