Professional Documents
Culture Documents
Nursing Patient Interaction
Uploaded by
kyeriaOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Nursing Patient Interaction
Uploaded by
kyeriaCopyright:
Available Formats
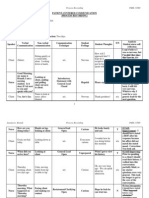
Nursing-Patient Interaction
Is the use of oral, gestures and facial expression of the client and nurse in
establishing a nurse-patient relationship.
Phases of Nurse-Patient Interaction
1. Orientation - During this phase, the individual has a felt need and seeks
professional assistance. The nurse helps the individual to recognize and
understand his/ her problem and determine the need for help.
2. Identification - The patient identifies with those who can help him/ her. The
nurse permits exploration of feelings to aid the patient in undergoing illness as an
experience that reorients feelings and strengthens positive forces in the
personality and provides needed satisfaction.
3. Exploitation - During this phase, the patient attempts to derive full value from
what he/ she are offered through the relationship. The nurse can project new
goals to be achieved through personal effort and power shifts from the nurse to
the patient as the patient delays gratification to achieve the newly formed goals.
4. Resolution -The patient gradually puts aside old goals and adopts new goals.
This is a process in which the patient frees himself from identification with the
nurse.
Techniques Effective in Nurse-Patient Interaction
1. Reflection. Repeating content or feelings. You might simply repeat what
the patient has said, to give him time to mull it over or to encourage him
to respond. Or, and often more effectively, you can reflect on what you
think the patient is feeling. "It sounds like you're concerned about your
family." or "I don't think you're very happy about this." By reflecting on his
feelings, you may be encouraging him to talk about something he may
have been hesitant to bring up himself. Or you may be helping the patient
to identify his own feelings about something.
2. Restating. Rephrasing a question or summarizing a statement. "You're
asking why these tests are needed?" or "In other words, you think you're
being treated like a child."
3. Facilitation. Occasional brief responses, which encourage the speaker to
continue. A nod of the head; an occasional verbal cue, such as "go on" or
"I see;" and maintaining eye contact throughout the conversation all imply
that you are listening and that you understand. (
4. Open-ended questions. Questions that encourage the patient to expound
on a topic. If you want to encourage the patient to speak freely, you might
ask "How are you feeling?" rather than "Are you in pain?"
5. Closed-ended questions. Questions, which focus the patient on a specific
topic. If you want a short, straight answer, ask a question which will allow
only for a direct response, such as "When was your accident?" or "Do you
have pain after eating?"
6. Silence. A quiet period that allows a patient to gather his thoughts. Of
course, this would be an occasional practice, used when you feel that the
patient could use a little time to think about his response to a question or
just to think.
7. Broad openings. A few words to encourage the patient to further discuss a
topic; for example, "and after that..." or "you were saying..."
8. Clarification. Statements or questions that verify a patient's concern or
point. "I'm a bit confused about...Do you think you could go over that
again please?"
Barriers in Nurse-Patient Interaction
1. Transference – development of an emotional attitude of the patient either
positive or negative towards the nurse.
2. Resistance - development of ambivalent feelings toward self exploration.
3. Counter Transference – transference as experienced by the nurse.
You might also like
- Process Recording - SampleDocument3 pagesProcess Recording - SampleMara Magsanoc70% (10)
- IPR SampleDocument4 pagesIPR SampleOliver Leeper100% (4)
- Nursing Patient InteractionDocument10 pagesNursing Patient Interactiondaphne_xhete0789% (9)
- Process RecordingDocument8 pagesProcess RecordingNaomi Masuda75% (4)
- Process RecordingDocument3 pagesProcess Recordingapi-353044299100% (4)
- 360 Process Recording TemplateDocument13 pages360 Process Recording Templateapi-252910411100% (9)
- Process Recording Psychiatric NursingDocument17 pagesProcess Recording Psychiatric NursingAaLona Robinson100% (4)
- Process RecordingDocument3 pagesProcess Recordingdyosa 433% (9)
- Rohingya Poems in RohingyalishDocument32 pagesRohingya Poems in RohingyalishMohammed Siddique Basu100% (7)
- 360 Process RecordingDocument11 pages360 Process Recordingapi-34006085780% (5)
- NURSING CARE PLAN Sensory-Perception DisturbanceDocument2 pagesNURSING CARE PLAN Sensory-Perception DisturbanceBernadette100% (1)
- 360 Process Recording Template - Posted Spring 2016 - This OneDocument11 pages360 Process Recording Template - Posted Spring 2016 - This OneNaya Kayala0% (1)
- Process RecordingDocument28 pagesProcess Recordingkristine86badgirl0% (1)
- Case Study On Chronic Kidney Disease Probably To Secondary HypertensionDocument18 pagesCase Study On Chronic Kidney Disease Probably To Secondary Hypertensionkyeria77% (26)
- RLE 105: Nurse-Patient Interaction: Mariano Marcos State UniversityDocument8 pagesRLE 105: Nurse-Patient Interaction: Mariano Marcos State UniversityAna Denise QuinajonNo ratings yet
- Nursing Patient InteractionDocument7 pagesNursing Patient Interactionnoronisa talusob100% (1)
- PMH Process RecordingDocument9 pagesPMH Process Recordingapi-316030498100% (2)
- Nurse Patient Analysis Verbal Non-Verbal Verbal Non - Verbal Therapeutic Technique AnalysisDocument6 pagesNurse Patient Analysis Verbal Non-Verbal Verbal Non - Verbal Therapeutic Technique AnalysisJay VillasotoNo ratings yet
- Therapeutic Communication Techniques 2Document3 pagesTherapeutic Communication Techniques 2Marc King MagsambolNo ratings yet
- NPI 3rd YrDocument3 pagesNPI 3rd Yrshin_2173No ratings yet
- Nurse-Patient Interaction FormatDocument1 pageNurse-Patient Interaction FormatRose Marie Castro100% (1)
- Process Recording NCMHDocument15 pagesProcess Recording NCMHKarl Angel B. Fabe100% (18)
- Nurse Patient InteractionDocument5 pagesNurse Patient InteractionMarius Clifford BilledoNo ratings yet
- Nurse Patient InteractionDocument3 pagesNurse Patient InteractionRozeru Matto DurenoNo ratings yet
- Mental Status ExaminationDocument3 pagesMental Status ExaminationjinahyangNo ratings yet
- Process Recording No 1Document7 pagesProcess Recording No 1Aiza Oronce100% (1)
- Communication TechniquesDocument10 pagesCommunication TechniquesNur Aleah MedtimbangNo ratings yet
- Advertisement and Sponsorship-Price ListDocument4 pagesAdvertisement and Sponsorship-Price ListzulkiplyNo ratings yet
- Iep CritiqueDocument11 pagesIep Critiqueapi-357058154No ratings yet
- Expository Essay Rough DraftDocument4 pagesExpository Essay Rough Draftapi-292792461No ratings yet
- Processing Recording 1 (1) .LGreenDocument24 pagesProcessing Recording 1 (1) .LGreenlmgreenNo ratings yet
- NPI Working PhaseDocument7 pagesNPI Working PhaseClaudette Sanvictores100% (2)
- Jesse Bishop Process Recording FormDocument8 pagesJesse Bishop Process Recording FormVijaya Rani100% (1)
- NPIDocument3 pagesNPIKenny NadelaNo ratings yet
- Nurse Patient Interaction CompileDocument87 pagesNurse Patient Interaction CompilemalindaNo ratings yet
- Pathophysiology of Bipolar 1 DisorderDocument1 pagePathophysiology of Bipolar 1 Disordermyer pasandalanNo ratings yet
- Nurse Patient InteractionDocument7 pagesNurse Patient InteractionGlaizalyn Fabella Tagoon100% (1)
- Orientation Phase Cruz Ronniella Diane S. Process RecordingDocument7 pagesOrientation Phase Cruz Ronniella Diane S. Process RecordingMARK JERIC G. FLORESNo ratings yet
- Process RecordingDocument14 pagesProcess RecordingPrince Mark Badillo100% (1)
- Psychiatric Reflection JournalDocument2 pagesPsychiatric Reflection JournalKatherine TanNo ratings yet
- Nurse Patient InteractionDocument8 pagesNurse Patient Interactionian_mendoza_30% (1)
- Verbal / Non-Verbal Communication Therapeutic Communication Used Rationale & Feelings of Nurse Evaluate / ResultDocument3 pagesVerbal / Non-Verbal Communication Therapeutic Communication Used Rationale & Feelings of Nurse Evaluate / ResultJoric Magusara50% (2)
- NCMH Newspaper ReadingDocument1 pageNCMH Newspaper ReadingRye AnchNo ratings yet
- Process RecordingDocument7 pagesProcess RecordingDannah TolentinoNo ratings yet
- Nurse Patient InteractionDocument14 pagesNurse Patient InteractionAldrich Mabasa100% (4)
- ReflectionDocument1 pageReflectionDawn MarcoNo ratings yet
- Working PhaseDocument7 pagesWorking PhaseSytrose MoralesNo ratings yet
- Process Recording and MSADocument21 pagesProcess Recording and MSAleomar gonzales67% (3)
- Altered Sensory and Disturbed Thought ProcessDocument4 pagesAltered Sensory and Disturbed Thought ProcessRosecinie Torrente100% (2)
- NpiDocument9 pagesNpiBernardNo ratings yet
- ORIENTATION PHASE-Undifferentiated SchizopreniaDocument7 pagesORIENTATION PHASE-Undifferentiated SchizopreniaIrish Eunice FelixNo ratings yet
- Process RecordingDocument12 pagesProcess Recordingapi-302732994100% (4)
- Re Motivation TherapyDocument2 pagesRe Motivation Therapyhulaanmuako67% (3)
- NCP For SchizoDocument6 pagesNCP For SchizoGILIANNE MARIE JIMENEANo ratings yet
- Psychiatric Nursing Structured ActivitiesDocument5 pagesPsychiatric Nursing Structured ActivitiesGabrielle AcaboNo ratings yet
- Communication Skills: By: Glenn Catan Chavez, RNDocument36 pagesCommunication Skills: By: Glenn Catan Chavez, RNGlenn ChavezNo ratings yet
- Non TherapeuticDocument9 pagesNon TherapeuticBrooke Contreras100% (1)
- Skills of CounselingDocument20 pagesSkills of Counselingfathimath fathunNo ratings yet
- Hildegard E. Peplau Nursing Nurse: - Client Relationship inDocument4 pagesHildegard E. Peplau Nursing Nurse: - Client Relationship inNicolette LeeNo ratings yet
- Part 1 AnswerDocument4 pagesPart 1 AnswerJose Karl Jr. Cataytay ApasNo ratings yet
- Therapeutic CommunicationDocument26 pagesTherapeutic Communicationristy dian puspitaNo ratings yet
- Therapeutic CommunicationDocument1 pageTherapeutic Communicationshiella mae leynesNo ratings yet
- Communication Skills 2014Document40 pagesCommunication Skills 2014Em KayNo ratings yet
- Therapeutic Communication TechniqueDocument18 pagesTherapeutic Communication TechniqueAngel Gaddi LarenaNo ratings yet
- Therapeutic Communication TechniquesDocument3 pagesTherapeutic Communication TechniquesGlads D. Ferrer-JimlanoNo ratings yet
- Process Recording On Mentally Ill PatientDocument6 pagesProcess Recording On Mentally Ill Patientkyeria40% (5)
- Process Recording On Mentally Ill PatientDocument6 pagesProcess Recording On Mentally Ill Patientkyeria40% (5)
- Erickson Theory of Psycho Social Development and Sigmund Freud of Psycho Sexual DevelopmentDocument5 pagesErickson Theory of Psycho Social Development and Sigmund Freud of Psycho Sexual Developmentkyeria100% (5)
- MeaslesDocument2 pagesMeasleskyeriaNo ratings yet
- Carbohydrate MetabolismDocument38 pagesCarbohydrate Metabolismwidya nurrohmanNo ratings yet
- MIT 6.00 Notes From Lessons 1,2 and 3.Document8 pagesMIT 6.00 Notes From Lessons 1,2 and 3.Nikola Nino IvankovićNo ratings yet
- A Survey On Sentiment Analysis of (Product) Reviews: A. Nisha Jebaseeli E. Kirubakaran, PHDDocument4 pagesA Survey On Sentiment Analysis of (Product) Reviews: A. Nisha Jebaseeli E. Kirubakaran, PHDvarunendraNo ratings yet
- Accu MAX3000Document2 pagesAccu MAX3000ynod70No ratings yet
- FMD PPT For SeminarDocument15 pagesFMD PPT For Seminarucantseeme0000No ratings yet
- Dimensional Engineering SeminarDocument71 pagesDimensional Engineering Seminardramilt100% (4)
- Psychosocial Problem and Its Associated Factors Among Adolescents in The Secondary Schools in Pasir Gudang, JohorDocument11 pagesPsychosocial Problem and Its Associated Factors Among Adolescents in The Secondary Schools in Pasir Gudang, JohorMaysoun AtoumNo ratings yet
- LNAT EssayDocument2 pagesLNAT EssayFaisal . BathawabNo ratings yet
- Bartletts TestDocument67 pagesBartletts TestRajendra KumarNo ratings yet
- Gupta R. S., Principles of Structural Design Wood, Steel, and Concrete, 2nd Ed, 2014Document58 pagesGupta R. S., Principles of Structural Design Wood, Steel, and Concrete, 2nd Ed, 2014reyNo ratings yet
- REVISION For END COURSE TEST - Criticial ThinkingDocument14 pagesREVISION For END COURSE TEST - Criticial Thinkingmai đặngNo ratings yet
- Pages From ABB Power Factor Correction and Harmonic Filtering in Electrical PlantsDocument7 pagesPages From ABB Power Factor Correction and Harmonic Filtering in Electrical Plantsrajpre1213No ratings yet
- Memory Management and LatchingDocument34 pagesMemory Management and Latchingrockerabc123No ratings yet
- PTSD, Assessment, Ies, TDocument2 pagesPTSD, Assessment, Ies, TKrishnaNo ratings yet
- HOTS How To Answer QuestionsDocument3 pagesHOTS How To Answer QuestionsEldad KarniNo ratings yet
- Viltam User Manual enDocument13 pagesViltam User Manual enszol888No ratings yet
- Younified LevelupDocument9 pagesYounified LevelupMitesh NagpalNo ratings yet
- Vxworks Kernel Programmers Guide 6.8Document802 pagesVxworks Kernel Programmers Guide 6.8hisahinNo ratings yet
- Photo-Realistic 3D Model Extraction From Camera Array CaptureDocument11 pagesPhoto-Realistic 3D Model Extraction From Camera Array CaptureJohn NaylorNo ratings yet
- GulfSea HT Oil 32 PDFDocument1 pageGulfSea HT Oil 32 PDFObydur RahmanNo ratings yet
- Gui 0001 EngDocument102 pagesGui 0001 EngBalaji MysoreNo ratings yet
- Polynomial Functions 1Document19 pagesPolynomial Functions 1Arafath Basheer100% (1)
- Solucionario Capitulo 13 Física Serway and FaughnDocument13 pagesSolucionario Capitulo 13 Física Serway and FaughnRafael Colindres100% (1)
- Vibration MeasurementDocument20 pagesVibration MeasurementDae A VeritasNo ratings yet
- Doc 01 DE 20190115144751 PDFDocument20 pagesDoc 01 DE 20190115144751 PDFAdi MNo ratings yet
- Semantics Course BookDocument67 pagesSemantics Course BookJosipa Blažević50% (2)