Professional Documents
Culture Documents
Maternity Evolve Exam
Uploaded by
friendofnurseCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Maternity Evolve Exam
Uploaded by
friendofnurseCopyright:
Available Formats
Maternity Evolve Exam
1. A nonstress test is performed, and the physician documents accelerations lasting less than 15 seconds throughout fetal
movement. The nurse interprets these findings as:
A. Normal
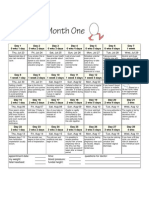
B. Reactive
C. Nonreactive Correct
D. Inconclusive
Rationale: A reactive nonstress test is a normal, or negative, result and indicates a healthy fetus. The result requires two
or more fetal heart rate accelerations of at least 15 beats/min lasting at least 15 seconds from the beginning of the
acceleration to the end, in association with fetal movement, during a 20-minute period. A nonreactive test is an abnormal
test, showing no accelerations or accelerations of less than 15 beats/min or lasting less than 15 seconds during a 40-
minute observation. An inconclusive result is one that cannot be interpreted because of the poor quality of the fetal heart
rate recording.
Test-Taking Strategy: Use the process of elimination. Eliminate a reactive nonstress test and a normal nonstress test first
because they are comparable or alike. To select from the remaining options, note the relationship between less than 15
seconds in the question and nonreactive in the correct option. If you had difficulty answering this question, review the
interpretation of nonstress test results.
2. A nurse caring for a client in labor performs an assessment. The client is having consistent contractions less than 2
minutes apart. The fetal heart rate (FHR) is 170 beats/min, and fetal monitoring indicates a pattern of decreased
variability. In light of these findings, the appropriate nursing action is:
A. Contacting the physician Correct
B. Documenting the findings
C. Continuing to monitor the client
D. Reassuring the client and her partner that labor is progressing normally
Rationale: Signs of potential complications of labor include contractions consistently lasting 90 seconds or longer,
contractions consistently occurring 2 minutes or less apart, fetal bradycardia, tachycardia, persistently decreased
variability, or an irregular FHR. The normal FHR is 110 to 160 beats/min. Therefore, because the finding is abnormal, the
physician must be contacted. Continuing to monitor the client delays necessary intervention. Reassuring the client that
labor is progressing normally is incorrect. The nurse would document the data, actions taken, and the clients response,
but, of the options provided, contacting the physician is the most appropriate.
Test-Taking Strategy: Use the process of elimination and focus on the data in the question. Eliminate the options that are
comparable or alike and indicate that the data in the question are normal findings. Review normal assessment findings
during the labor process if you had difficulty with this question.
3. A stillborn infant was delivered a few hours ago. After the birth, the family remains together, holding and touching the
baby. Which statement by the nurse is appropriate?
A. I know how you feel.
B. This must be hard for you. Correct
C. Now you have an angel in heaven.
D. Youre young. You can have other children.
Rationale: Therapeutic communication helps the mother, father, and other family members express their feelings and
emotions. This must be hard for you is a caring and empathetic response, focused on feelings and encouraging
communication. The other options are nontherapeutic and may devalue the family members' feelings.
Test-Taking Strategy: Use your knowledge of therapeutic communication techniques. The correct option is the only option
that is focused on the family members feelings. Review therapeutic communication techniques if you had difficulty with
this question.
4. A rubella antibody screen is performed in a pregnant client, and the results indicate that the client is not immune to
rubella. The nurse tells the client that:
A. A rubella vaccine must be administered immediately
B. A rubella vaccine must be administered after childbirth Correct
C. She will not contract rubella if she is exposed to the disease
D. She does not need to be concerned about being exposed to rubella
Rationale: A prenatal rubella antibody screen is performed in every pregnant woman to determine whether she is immune
to rubella, which can cause serious fetal anomalies. If she is not immune, rubella vaccine is offered after childbirth to keep
her from contracting rubella during subsequent pregnancies. The vaccine is a live virus, and defects might occur in the
fetus if the vaccine were administered during pregnancy or if the mother were to become pregnant soon after it was
administered. Administering a rubella vaccine immediately places the fetus at risk. Telling the client that she does not
need to be concerned about being exposed to rubella is incorrect, because the possibility of exposure, which could be
harmful to the fetus, does exist.
Test-Taking Strategy: Use the process of elimination. Eliminate first the options that are comparable or alike (i.e., the
client will not acquire rubella and does not need to be concerned about exposure). To select from the remaining options,
recall that rubella vaccine is a live virus; this will direct you to the correct option. Review rubella vaccine and its
implications during pregnancy if you had difficulty with this question.
5. A nurse caring for a client in the active stage of labor assesses the fetal status and notes a late deceleration on the
monitor strip. In light of this finding, which nursing action is the priority?
A. Documenting the finding
B. Preparing for immediate birth
C. Administering oxygen by way of face mask Correct
D. Increasing the rate of the oxytocin (Pitocin) infusion
Rationale: Late decelerations are a result of uteroplacental insufficiency stemming from decreased blood flow and oxygen
transfer to the fetus during uterine contractions. This causes hypoxemia; therefore oxygen is necessary, making the
administration of oxygen the correct choice. Late decelerations are considered an ominous sign but do not necessarily
require immediate birth of the baby. The oxytocin infusion should be discontinued when a late deceleration is noted. The
oxytocin would cause further hypoxemia, because the medication stimulates contractions, leading to increased
uteroplacental insufficiency. Although the finding needs to be documented, documentation is not the priority action in this
situation.
Test-Taking Strategy: Note the strategic word priority in the question. Use your knowledge of the ABCs airway,
breathing, and circulation to answer the question. This will direct you to the correct option, the one that addresses
oxygen. Review content on late decelerations if you had difficulty with this question.
6. A nurse provides instructions regarding postpartum exercises to a client who has delivered a newborn vaginally. The
nurse tells the client that:
A. The exercises should be delayed for 1 month to allow healing
B. Performing such exercises in the postpartum period may result in stress urinary incontinence
C. Alternating contraction and relaxation of the muscles of the perineal area should be practiced Correct
D. Abdominal exercises will be started while the client is in the hospital as a means of evaluating tolerance
Rationale: Postpartum exercises may be started soon after birth, although the woman should be encouraged to begin with
simple exercises and gradually progress to more strenuous ones. Abdominal exercises are postponed until approximately
4 weeks after a cesarean birth. Kegel exercises (alternated contraction and relaxation of the muscles of the perineal area)
are extremely important in strengthening the muscle tone of the perineal area after vaginal birth. Kegel exercises help
restore the muscle tone that is often lost as pelvic tissues are stretched and torn during pregnancy and birth. Women who
maintain muscle strength may benefit years later, experiencing continued urinary continence.
Test-Taking Strategy: Use the process of elimination. Note the relationship between the word vaginally in the question
and perineal area in the correct option. Review the purpose and benefit of Kegel exercises if you had difficulty with this
question.
7. A client in the first trimester of pregnancy arrives at the clinic and reports that she has been experiencing vaginal bleeding.
Threatened abortion is suspected, and the nurse provides instructions to the client regarding care. Which statement by
the client indicates the need for further instruction?
A. I need to stay in bed for the rest of my pregnancy. Correct
B. I need to avoid having sex until the bleeding has stopped.
C. I need to watch for stuff that looks like tissue coming from my vagina.
D. I need to count the number of perineal pads that I use each day and make a note of the amount and color
of blood on each pad.
Rationale: Strict bed rest throughout the remainder of the pregnancy is not required. The woman is advised to curtail
sexual activities until bleeding has ceased and for 2 weeks after the last evidence of bleeding, as recommended by the
physician or nurse-midwife. The woman is instructed to count the perineal pads she uses each day and to note the
quantity and color of blood on each pad. The woman should also watch for the evidence of the passage of tissue.
Test-Taking Strategy: Use the process of elimination. Note the strategic words need for further instruction in the
question, which indicate a negative event query and the need to select the incorrect client statement. Noting the words
stay in bed for the rest of my pregnancy will direct you to this option. Review therapeutic management for threatened
abortion if you had difficulty with this question.
8. A nurse is assessing the respiratory rate of a newborn. Which finding would the nurse document as normal?
A. 20 breaths/min
B. 25 breaths/min
C. 50 breaths/min Correct
D. 70 breaths/min
Rationale: The normal respiratory rate for a newborn infant is 30 to 60 breaths/min. All of the other options are outside the
normal range.
Test-Taking Strategy: Knowledge regarding the normal respiratory rate of a newborn is required to answer this question. If
you are unfamiliar with the normal ranges for newborn vital signs, review this content.
9. A nurse notes that the laboratory report of a pregnant client with suspected HIV infection indicates leukopenia,
thrombocytopenia, anemia, and an increased erythrocyte sedimentation rate. Which laboratory test that would further
confirm the presence of HIV does the nurse anticipate that the physician will prescribe?
A. Platelet count
B. Angiotensin level
C. Glomerular filtration rate
D. T-lymphocyte determination Correct
Rationale: HIV has a strong affinity for surface marker proteins on lymphocytes. This affinity of HIV for T-lymphocytes
leads to significant cell destruction. Angiotensin is produced in the kidney and plays a role in blood pressure control.
Glomerular filtration rate is an indicator of kidney function. The platelet count is important and may be used as an indicator
of the effects of HIV, but the platelet count (thrombocytopenia) has already been addressed in the question.
Test-Taking Strategy: Use the process of elimination, focusing on the subject, the presence of HIV. Eliminate the platelet
count, because this has already been addressed in the question (thrombocytopenia). Next eliminate the options that are
comparable or alike in that they are related to kidney function. If you had difficulty with this question, review the clinical
manifestations and pathology of HIV infection.
10. A nurse palpates the anterior fontanel of a neonate and notes that it feels soft.
This nurse interprets this assessment data as:
A. A normal finding Correct
B. Indicative of dehydration
C. Indicative of increased intracranial pressure
D. Indicative of decreased intracranial pressure
Rationale: The anterior fontanel, which is diamond shaped, is located on the top of the head. It measures 1 to 4 cm but
varies because of molding and individual differences. It normally closes by 12 to 18 months of age. It may be described as
soft, which is normal, or full and bulging, which may be indicative of increased intracranial pressure. Conversely, a
depressed fontanel could mean that the neonate is dehydrated.
Test-Taking Strategy: Use the process of elimination, noting the strategic words feels soft in the question. Remember
that the anterior fontanel is soft in the neonate. If you had difficulty answering this question, review normal assessment
findings in the neonate.
11. A nurse provides information about the treatment for hypoglycemia to a client with gestational diabetes who will be taking
insulin. The nurse tells the client that if signs and symptoms of hypoglycemia occur, she must immediately:
A. Lie down
B. Contact the physician Incorrect
C. Drink 8 oz of diet soda
D. Check her blood glucose level Correct
Rationale: If signs and symptoms of hypoglycemia occur, the client should immediately check the blood glucose level. The
results will determine the required treatment. If the blood glucose is less than 60 mg/dL, the client should immediately eat
or drink something that contains 10 to 15 g of simple carbohydrate. Examples include a half cup (4 oz) of unsweetened
fruit juice, a half cup (4 oz) of regular (not diet) soda, 5 or 6 LifeSavers candies, 1 tablespoon of honey or corn (Karo)
syrup; 1 cup (8 oz) of milk; or 2 or 3 glucose tablets. The blood glucose is tested again 15 minutes after intake of the
carbohydrate. If the glucose level is still below 60 mg/dL, the client should eat or drink another 10 to 15 g of simple
carbohydrate. The blood glucose is tested once again 15 minutes after intake of the carbohydrate, and the physician is
notified immediately if it is still below 60 mg/dL, because further intervention is necessary. Lying down will not increase the
blood glucose level and will delay necessary intervention.
Test-Taking Strategy: Use the process of elimination and note the strategic word immediately. Remember that if
hypoglycemia is suspected, a blood glucose test is needed to confirm its occurrence and then treatment measures must
be taken immediately. Review the treatment measures for hypoglycemia if you had difficulty with this question.
12. A nurse is providing nutritional counseling to pregnant client with a history of cardiac disease. What does the nurse advise
the client to eat?
A. Water and pretzels
B. Low-fat cheese omelet
C. Nachos and fried chicken
D. Apple and whole-grain toast Correct
Rationale: The pregnant woman needs a well-balanced diet high in iron and protein and adequate in calories for weight
gain. Iron supplements that are taken during pregnancy tend to cause constipation. Constipation causes the client to
strain during defecation, inadvertently performing the Valsalva maneuver, which causes blood to rush to the heart and
overload the cardiac system. The pregnant woman, then, should increase her intake of fluids and fiber. An unlimited
intake of sodium (pretzels, cheese, nachos) could cause overload of the circulating blood volume and contribute to the
cardiac condition.
Test-Taking Strategy: Use the process of elimination and note that the client has a history of cardiac disease. Recalling
the concepts of care of the client with cardiac disease and noting that the question involves a client who is pregnant will
direct you to the correct option. Review dietary requirements and examples of foods containing those requirements for a
cardiac client who is pregnant if you had difficulty with this question.
13. A neonate is irritable, cries incessantly, and has a temperature of 99.4F. The neonate is also tachypneic, diaphoretic,
feeding poorly, and hyperactive in response to environmental stimuli. The nurse determines that these signs and
symptoms are consistent with:
A. Sepsis
B. Hypercalcemia Incorrect
C. Intraventricular hemorrhage
D. Neonatal abstinence syndrome Correct
Rationale: Neonatal abstinence syndrome is the term given to the group of signs and symptoms associated with drug
withdrawal in the neonate. Drug withdrawal causes a hyperactive response in the infant because of the increased central
nervous system (CNS) stimulation. This hyperactive response and the signs and symptoms of drug withdrawal seem to be
most apparent around 1 week of age. Sepsis, hypercalcemia, and intraventricular hemorrhage cause symptoms of CNS
depression.
Test-Taking Strategy: Use the process of elimination, focusing on the data in the question. Note the strategic word
hyperactive, which indicates CNS stimulation and should direct you to the correct option. If you had difficulty with this
question, review the signs and symptoms of drug withdrawal in the neonate.
14. A nurse is assisting a physician in performing a physical examination of a client who has just been told that she is
pregnant. The physician tells the nurse that the Goodell sign is present. The nurse understands that this sign is indicative
of:
A. The presence of fetal movement
B. A high risk for spontaneous abortion
C. An increase in vascularity and hyptertrophy of the cervix Correct
D. The presence of human chorionic gonadotropin (hCG) in the urine Incorrect
Rationale: In the early weeks of pregnancy, the cervix becomes more vascular and slightly hypertrophic; this is referred to
as the Goodell sign. The edematous appearance of the cervix will be noted during pelvic examination by the examiner.
hCG is noted in maternal urine in a urine pregnancy test. The Goodell sign does not indicate the presence of fetal
movement or a risk for spontaneous abortion.
Test-Taking Strategy: Knowledge regarding the Goodell sign is required to answer this question. It is necessary to know
that the sign consists of increased vascularity and hypertrophy of the cervix. If you had difficulty with this question, review
the changes in the cervix that occur during pregnancy.
15. A nurse is monitoring a client in labor for signs of intrauterine infection. Which sign, indicative of infection, would prompt
the nurse to contact the healthcare provider?
A. Maternal fatigue
B. Clear amniotic fluid
C. Strong-smelling amniotic fluid Correct
D. A fetal heart rate of 140 beats/min
Rationale: Signs associated with intrauterine infection includes fetal tachycardia (rising baseline or faster than 160
beats/min, a maternal fever (38C or 100.4F), foul or strong-smelling amniotic fluid, or cloudy or yellow amniotic fluid.
The normal fetal heart rate is 110 to 160 beats/min. Clear amniotic fluid is normal. Maternal fatigue normally occurs during
labor.
Test-Taking Strategy: Focus on the subject of the question, a sign of intrauterine infection. Eliminate the options that are
comparable or alike in that they are normal expectations during labor. Review the signs of intrauterine infection if you had
difficulty with this question.
16. A nurse is assessing the uterine fundus of a client who has just delivered a baby and notes that the fundus is boggy. The
nurse massages the fundus, and then presses to expel clots from the uterus. To prevent uterine inversion during this
procedure, the nurse:
A. Has the client void before the uterine assessment
B. Tells the woman to bear down during fundal message
C. Simultaneously provides pressure over the lower uterine segment Correct
D. Asks the client to take slow, deep breaths during fundal assessment
Rationale: After massaging a boggy fundus until it is firm, the nurse presses the fundus to expel clots from the uterus. The
nurse must also keep one hand pressed firmly just above the symphysis (over the lower uterine segment) the entire time.
Removing the clots allows the uterus to contract properly. Providing pressure over the lower uterine segment prevents
uterine inversion. Having the client void before uterine assessment will not prevent uterine inversion. Telling the woman to
bear down while the nurse performs fundal message and asking the client to take slow, deep breaths during fundal
assessment also will not prevent uterine inversion.
Test-Taking Strategy: Use the process of elimination, focusing on the subject, prevention of uterine inversion. Visualizing
each of the actions in the options and relating the action to the subject of the question will direct you to the correct option.
Review fundal assessment and massage if you had difficulty with this question.
17. A nurse assists a pregnant client who is in the second trimester into lithotomy position on the examining table in the
obstetricians office. The client suddenly becomes dizzy, lightheaded, nauseated, and pale. The nurse immediately:
A. Positions the client on her side Correct
B. Calls the physician to see the client
C. Places a cool washcloth on the clients forehead
D. Checks the clients blood pressure, pulse, and respirations
Rationale: Supine hypotension may occur during the second and third trimesters when a woman is placed in the lithotomy
position, in which the weight of the abdominal contents may compress the vena cava and aorta, causing a drop in blood
pressure and a feeling of faintness. Other signs and symptoms include pallor, dizziness, breathlessness, tachycardia,
nausea, clammy (damp, cool) skin, and sweating. The nurse would immediately position the woman on her side. Placing a
cool washcloth on the clients forehead or checking the clients vital signs will not eliminate this problem. The physician
must be contacted if the symptoms do not subside, but this would not be the immediate action.
Test-Taking Strategy: Use the process of elimination and note the strategic word immediately. Focusing on the data in
the question and determining that the client is experiencing supine hypotension will direct you to the correct option.
Review the manifestations of supine hypotension and the interventions for treating this occurrence if you had difficulty with
this question.
18. A nurse is monitoring a newborn who has been admitted to the nursery. The nurse notes that the anterior fontanel
measures 4 cm across and bulges when the infant is at rest. In light of this observation, what is the appropriate nursing
action?
A. Notifying the physician Correct
B. Documenting the finding
C. Assessing the infants blood pressure
D. Reassessing the fontanel in 30 minutes
Rationale: The anterior fontanel, which is diamond shaped, is located on the top of the head. It should be flat and soft. It
measures 1 to 4 cm, varying as a result of molding and individual differences. It normally closes by 12 to 18 months of
age. Although the anterior fontanel may bulge slightly when the infant cries, bulging at rest may indicate increased
intracranial pressure. If this is suspected, the physician is notified. The other options would delay necessary treatment.
Test-Taking Strategy: Use the process of elimination and note the strategic words bulges when the infant is at rest.
Recalling that the fontanel should be soft and flat will direct you to the correct option. Review normal newborn assessment
findings if you had difficulty with this question.
19. A nurse midwife performs an assessment of a pregnant client and documents the station of the fetal head as it is reflected
in the figure below. The nurse reviews the assessment findings and determines that the fetal presenting part is:
A. At +1 station
B. At 1 station
C. At zero station Correct
D. Stationed at the bottom of the coccyx
Rationale: Station is the relationship of the presenting part to an imaginary line drawn between the ischial spines. It is
measured in centimeters and is noted as a negative number above the line, a positive number below the line, and zero at
the line.
Test-Taking Strategy: Knowing that station is measured in centimeters, with the ischial spines as a reference point, will
assist you in answering this question. Focus on the figure and note that the fetal head is at zero station. Review station if
you had difficulty with this question.
20. A client is admitted to the hospital for an emergency cesarean delivery. Contractions are occurring every 15 minutes, the
client has a temperature of 100F, and the client reports that she last ate 2 hours ago. The client also states that
everything happened so fast" and that she has had no preparation for the cesarean delivery. Which of the following
actions should the nurse take first?
A. Continuing to time the contractions
B. Beginning teaching about the cesarean delivery
C. Reporting the time of last food intake to the physician Correct
D. Giving acetaminophen (Tylenol) to lower the clients temperature
Rationale: The nurse should report the time of last food intake to the physician. General anesthesia may be used for an
emergency cesarean delivery. Gastric contents are very acidic and can produce chemical pneumonitis if aspirated.
Continued monitoring and client instruction are correct nursing actions but are of lesser priority than reporting the time of
last oral intake. Giving acetaminophen (Tylenol) is incorrect because it requires a physicians prescription.
Test-Taking Strategy: Note the strategic word first and use your knowledge of the ABCs airway, breathing, and
circulation to find the correct option, which pertains to breathing (maintaining an open airway). Review client
preparation for an emergency cesarean delivery if you had difficulty with this question.
21. A nurse is monitoring a client who was given an epidural opioid for a cesarean birth. The nurse notes that the clients
oxygen saturation on pulse oximetry is 92%. The nurse first:
A. Contacts the physician
B. Documents the findings
C. Instructs the client to take several deep breaths Correct
D. Administers 100% oxygen by way of face mask
Rationale: If the client has been given an epidural opioid, the nurse should monitor the clients respiratory status closely. If
the oxygen saturation falls below 95%, the nurse instructs the client to take several deep breaths to increase the level.
Although the finding would be documented, action is required to increase the oxygen saturation level. It is not necessary
to contact the physician. If the deep breaths fail to increase the oxygen saturation level, the physician is notified and may
prescribe oxygen.
Test-Taking Strategy: Use the process of elimination and focus on the data in the question. Noting the oxygen saturation
level will assist you in eliminating this option. Noting the strategic word first will direct you to the correct option. Review
care of the client after a cesarean birth if you had difficulty with this question.
22. A nurse is monitoring a client in the third trimester of pregnancy who has a diagnosis of severe preeclampsia. Which
finding would prompt the nurse to contact the physician?
A. Complaint of feeling hot
B. Enlargement of the breasts
C. Diaphoresis and tachycardia Correct
D. Periods of fetal movement followed by quiet periods
Rationale: Disseminated intravascular coagulation (DIC) is a complication of preeclampsia. Physical examination reveals
unusual bleeding, spontaneous bleeding from the womans gums or nose, or the presence of petechiae around a blood
pressure cuff placed on the womans arm. Excessive bleeding may occur from a site of slight trauma such as a
venipuncture site, an intramuscular or subcutaneous injection site, a nick sustained during shaving of the perineum or
abdomen, or injury inflicted during insertion of a urinary catheter. Tachycardia and diaphoresis indicate impending shock
as a result of blood loss. Breast enlargement, fetal movement with rest periods, and complaints of feeling hot are all
normal occurrences in the last trimester of pregnancy.
Test-Taking Strategy: Use the process of elimination. Eliminate the options that are comparable or alike in that they are
normal occurrences in pregnancy. Review the complications associated with severe preeclampsia if you had difficulty with
this question.
23. A nurse is monitoring a pregnant client with sepsis for signs of disseminated intravascular coagulopathy (DIC). Which of
the following laboratory findings causes the nurse to suspect DIC?
A. Increased platelet count
B. Increased fibrinogen level
C. Shortened prothrombin time
D. Increased fibrin degradation products Correct
Rationale: DIC is a state of diffuse clotting in which clotting factors are consumed, leading to widespread bleeding.
Petechiae, oozing from injection sites, and hematuria are indicative of DIC. Platelets are decreased because they are
consumed by the process; coagulation studies show no clot formation (and therefore prolonged times); and fibrin plugs
may clog the microvasculature diffusely rather than in an isolated area. Fibrinogen and platelets are decreased,
prothrombin and activated partial thromboplastin times are prolonged, and fibrin degradation products are increased.
Test-Taking Strategy: Use the process of elimination. Recalling the pathophysiology of DIC will direct you to the correct
option. Review laboratory findings in DIC if you had difficulty with this question.
24. A nurse is caring for a client experiencing hypotonic labor contractions. The client is discouraged by the lack of progress
with labor but refuses an amniotomy or oxytocin (Pitocin) stimulation. The nurse determines that the clients behavior may
be a result of:
A. Concern about her own and the babys well-being Correct
B. The high level of pain caused by these contractions
C. Inability to rest between the frequent contractions
D. The normal lack of control clients feel during the transition phase of labor
Rationale: Clients have concerns when labor does not proceed as expected and often are worried about the effects of
treatments and invasive procedures on themselves and on the fetus. Hypotonic contractions generally occur during the
active phase of labor, after a normal latent phase. These contractions are typically of poor intensity and infrequent; they
are not painful but cause a very slow progression of labor. Therefore the high level of pain, inability to rest between
contractions, and normal lack of control felt during the transition phase of labor are all incorrect.
Test-Taking Strategy: Use the process of elimination, focusing on the subject, hypotonic labor contractions. Thinking
about the pathophysiology of hypotonic labor will direct you to the correct option. Also, noting that the client is refusing
treatments will assist you in answering correctly. Review the characteristics of hypotonic labor contractions and the
psychosocial reactions associated with this disorder if you had difficulty with this question.
25. A woman with severe preeclampsia delivers a healthy newborn infant and continues to receive magnesium sulfate
therapy in the postpartum period. Twenty-four hours after delivery, the client begins passing more than 100 mL of urine
every hour. The nurse recognizes this volume of urine output as an indication of:
A. Imminent seizures
B. Hyperkalemia
C. High-output renal failure
D. Diminished edema and vasoconstriction in the brain and kidneys Correct
Rationale: In this client, diuresis is a positive sign, indicating that edema and vasoconstriction in the brain and kidneys
have decreased. Diuresis also reflects increased tissue perfusion in the kidneys. Clients with severe preeclampsia are not
considered out of danger until birth and diuresis have taken place. Diuresis is not an indication of impending seizures.
Although renal failure is a complication of severe preeclampsia, it is not the high-output type of failure. Potassium is lost
through the urine; therefore hyperkalemia is not associated with diuresis.
Test-Taking Strategy: Use the process of elimination. Recalling that oliguria is associated with severe preeclampsia will
help you determine that diuresis in this scenario is associated with an improvement in preeclampsia. This will direct you to
the correct option. If you had difficulty with this question, review the expected responses to treatment of severe
preeclampsia.
26. A pregnant woman reports to the clinic complaining of loss of appetite, weight loss, and fatigue, and tuberculosis is
suspected. A sputum culture reveals Mycobacterium tuberculosis. The nurse, providing instructions to the mother
regarding therapeutic management of the disease, tells the mother that:
A. The infant must be isolated from the mother after birth
B. Maternal medication will not be started until the baby is born
C. The infant will require medication therapy immediately after birth
D. The mother may need to take isoniazid (INH), pyrazinamide, and rifampin (Rifadin) for a total of 9
months Correct
Rationale: More than one medication may be used to prevent the growth of resistant organisms in the pregnant woman
with tuberculosis. Treatment must be continued for a prolonged period. The preferred treatment for the pregnant woman is
isoniazid plus rifampin for a total of 9 months. Ethambutol is added initially if drug resistance is suspected. Pyridoxine
(vitamin B6 ) is often administered with isoniazid to prevent fetal neurotoxicity. The infant will be tested at birth and may be
started on preventive isoniazid therapy. Skin testing of the infant should be repeated at 3 months, and isoniazid may be
stopped if the result remains negative. If the result is positive, the infant should receive isoniazid for at least 6 months. If
the mothers sputum is free of organisms, the infant does not need to be isolated from the mother while in the hospital.
Test-Taking Strategy: Knowledge regarding the therapeutic management of the mother with tuberculosis and that of the
infant is required to answer this question. Eliminate the options containing the closed-ended words must, not, and
immediately. If you had difficulty with this question, review treatment measures for the mother with tuberculosis.
27. A nurse is performing an assessment of a client who is at 20 weeks of gestation. The nurse asks the client to void, then
measures the fundal height in centimeters. Which approximate measurement does the nurse expect to see?
A. 20 cm Correct
B. 28 cm
C. 32 cm
D. 40 cm
Rationale: During the second and third trimesters (weeks 18 to 30), the height of the fundus in centimeters is
approximately the same as the number of weeks of gestation, if the womans bladder is empty at the time of
measurement. If the fundal height exceeds the number of weeks of gestation, additional assessment is necessary to
investigate the cause for the unexpectedly large uterine size. An unexpected increase in uterine size may indicate that the
estimated date of delivery is incorrect and the pregnancy is more advanced than previously thought. If the estimated date
of delivery is correct, more than one fetus may be present.
Test-Taking Strategy: Knowledge regarding the expected findings in fundal height during the second or third trimester is
required to answer this question. Remember that the height of the fundus in centimeters during the second and third
trimesters is approximately the same as the number of weeks of gestation. If you are unfamiliar with the interpretation of
fundal height, review this content.
28. A client who delivered a healthy newborn 11 days ago calls the clinic and tells the nurse that she is experiencing a white
vaginal discharge. The nurse tells the client:
A. To perform a vaginal douche
B. To come to the clinic for a checkup
C. That this is an indication of an infection
D. That this is a normal postpartum occurrence Correct
Rationale: For the first 3 days following childbirth, lochia consists almost entirely of blood, with small particles of decidua
and mucus, and is called lochia rubra because of its red color. The amount of blood decreases by about the fourth day,
and which time the lochia changes from red to pink or brown-tinged; this stage is called lochia serosa. By about the 11th
day, the erythrocyte component of lochia has decreased and the discharge becomes white or cream-colored. This final
stage is known as lochia alba. Lochia alba contains leukocytes, decidual cells, epithelial cells, fat, cervical mucus, and
bacteria. It is present in most women until the third week after childbirth but may persist for as long as 6 weeks. Lochia
alba is a normal finding during the postpartum course, and no intervention is required, so the other options are incorrect.
Test-Taking Strategy: Use your knowledge of expected postpartum findings to answer the question. Recalling the normal
expected occurrences in regard to vaginal discharge will direct you to the correct option. Also, noting that the incorrect
options are comparable or alike will direct you to the correct option. Review normal postpartum findings in regard to lochia
if you had difficulty with this question.
29. A nurse is caring for a client receiving an intravenous infusion of oxytocin (Pitocin) to stimulate labor. Which of the
following findings would prompt the nurse to stop the infusion?
A. Contractions every 3 minutes
B. Nonreassuring fetal heart rate pattern Correct
C. Soft uterine tone palpated between contractions
D. The presence of three contractions every 10 minutes
Rationale: The goal of labor augmentation is to achieve three good-quality contractions (of appropriate intensity and
duration) in a 10-minute period. The uterus should return to resting tone between contractions, and there should be no
evidence of fetal distress. If a nonreassuring fetal heart rate pattern is detected, the oxytocin infusion is stopped. A
nonreassuring fetal heart rate pattern is associated with fetal hypoxia.
Test-Taking Strategy: Use the process of elimination and your knowledge of the ABCs (airway, breathing, and circulation).
Eliminate the options that are comparable or alike (i.e., contractions every 3 minutes and occurrence of three contractions
every 10 minutes). The correct option, of the two that remain, is the one that indicates a problem with circulation. Review
the expected outcomes and the signs of complications associated with oxytocin infusion if you had difficulty with this
question.
30. A nurse assessing a pregnant woman in labor notes the presence of early decelerations on the fetal monitor tracing.
Which of the following situations would the nurse suspect in light of this observation?
A. Umbilical cord compression
B. Pressure on the fetal head during a contraction Correct
C. Adequate pacemaker activity of the fetal heart
D. Uteroplacental insufficiency during a contraction
Rationale: Early decelerations, which result from pressure on the fetal head during a contraction, are not associated with
fetal compromise and require no intervention. Variable decelerations suggest umbilical cord compression. Late
decelerations are an ominous pattern in labor because they suggest uteroplacental insufficiency during a contraction.
"Short-term variability" refers to the difference between successive heartbeats, indicating that the natural pacemaker
activity of the fetal heart is working properly.
Test-Taking Strategy: The ability to interpret and evaluate fetal monitoring patterns is required to answer this question.
Relate early decelerations to pressure on the fetal head during a contraction to assist in answering questions similar to
this one. If you are unfamiliar with early decelerations and their significance, review this content.
31. A delivery room nurse performing an initial assessment on a newborn notes that the ears are low set. In light of this
finding, which nursing action is appropriate initially?
A. Notifying the physician Correct
B. Documenting the finding
C. Taping the ears so they lie flat against the head
D. Covering the ears with gauze pads and taping the pads to the head
Rationale: Low or oddly placed ears are associated with a variety of congenital defects, including Down syndrome, and
should be reported immediately. Taping the ears and covering them with gauze are unacceptable nursing interventions.
Although the finding would be documented, the appropriate initial action is notification of the physician.
Test-Taking Strategy: Knowledge regarding the normal assessment findings in a newborn is required to answer this
question. Recalling that low-set ears are an abnormal finding will direct you to the correct option. Review normal
assessment findings in a newborn if you had difficulty with this question.
32. A nurse is reviewing the criteria for early discharge of a newborn infant. Which of the following, if noted in the infant, would
indicate that the criteria for early discharge have been met? Select all that apply.
A. The infant has urinated. Correct
B. The infant has passed 1 stool. Correct
C. Vital signs are documented as normal. Correct
D. The infant has completed one successful feeding.
E. The infant has shown no evidence of jaundice in the first 6 hours of life.
Rationale: Criteria for early discharge in the newborn infant include no evidence of significant jaundice in the 24 hours
after birth. The infant should have urinated and passed at least one stool, completed at least two successful feedings, and
have normal vital signs for at least 12 hours.
Test-Taking Strategy: Note the strategic words have been met. Read each option carefully and think about the expected
assessment findings for a newborn. This will direct you to the correct options. Review the criteria for early discharge of a
newborn if you are unfamiliar with them.
33. A nurse is performing assessments every 30 minutes on a client who is receiving magnesium sulfate for preeclampsia.
Which of the following findings would prompt the nurse to contact the physician?
A. Urine output of 20 mL
B. Deep tendon reflexes of 2+
C. Respirations of 10 breaths/min Correct
D. Fetal heart tone of 116 beats/min
Rationale: Magnesium sulfate depresses the respiratory rate. If the rate is 12 breaths/min or slower, continuation of the
medication must be reassessed. Acceptable urine output is 30 mL/hr or more. Urine output of 20 mL in 30 minutes is
adequate. Deep tendon reflexes of 2+ are normal. The fetal heart tone is within normal limits for a resting fetus.
Test-Taking Strategy: Note the strategic words contact the physician. Use the process of elimination, noting the
assessment finding that is abnormal and requires further intervention. Also, use your knowledge of the ABCs (airway,
breathing, and circulation) to identify the correct option. Review assessment findings in preeclampsia and the effects of
magnesium sulfate if you had difficulty with this question.
34. A nurse provides instructions to a breastfeeding mother who is experiencing breast engorgement about measures for
treating the problem. The nurse tells the mother to:
A. Take a cool shower just before breastfeeding
B. Avoid breastfeeding during the night time hours to ensure adequate rest
C. Gently massage the breasts during breastfeeding to help empty the breasts Correct
D. Apply heat packs to the breasts for 15 to 20 minutes between feedings to reduce swelling
Rationale: Gently massaging the breasts during breast feeding will help empty the breasts. The mother should not avoid
breastfeeding during the night; instead, she should breastfeed every 2 hours or pump the breasts. The nurse instructs the
woman to apply ice packs, not heat packs, to the breasts between feedings to reduce swelling. It may be helpful for the
mother to stand in a warm shower just before feeding to foster relaxation and letdown.
Test-Taking Strategy: Focus on the subject, breast engorgement, and think about its characteristics. Use the process of
elimination and visualize each of the descriptions in the options to identify the measure that will be helpful. If you had
difficulty answering the question, review the measures for breast engorgement.
35. A nurse is caring for a postpartum client who had a low-lying placenta. The nurse assesses the client most closely for:
A. Seizures
B. Infection
C. Hemorrhage Correct
D. A vaginal hematoma
Rationale: The lower uterine segment does not contain the same intertwining musculature as the fundus of the uterus,
making this site more prone to bleeding. The client with a low-lying placenta is not at greater risk for seizures, postpartum
infection, or vaginal hematoma.
Test-Taking Strategy: Focus on the clients diagnosis, a low-lying placenta. Recalling the anatomy and physiology of the
lower segment of the uterus will direct you to the correct option. Review the complications associated with a low-lying
placenta if you had difficulty with this question.
36. When, during the normal postpartum course, would the nurse expect to note the fundal assessment shown in the figure?
A. 4 days after delivery
B. The day after delivery
C. Immediately after delivery Correct
D. When the clients bladder is full
Rationale: Immediately after delivery, the uterine fundus should be at the level of the umbilicus or one to three
fingerbreadths below it and in the midline of the abdomen. Location of the fundus above the umbilicus may indicate the
presence of blood clots in the uterus that need to be expelled by means of fundal massage. A fundus that is not located in
the midline may indicate a full bladder. The fundus descends 1 or 2 cm every 24 hours, so it should be located farther
below the umbilicus with every succeeding postpartum day.
Test-Taking Strategy: Focus on the figure and note that the fundus is at the level of the umbilicus. Recalling normal
postpartum assessment findings in the mother and recalling the normal anatomy will assist in directing you to the correct
option. If you had difficulty with this question, review normal postpartum assessment findings in regard to involution.
37. A nurse is caring for a client in labor who has sickle cell anemia. Which intervention does the nurse implement to help
prevent a sickling crisis?
A. Maintaining strict asepsis
B. Monitoring the maternal vital signs
C. Administering oxygen as prescribed Correct
D. Placing a wedge under the clients hip
Rationale: Oxygen is administered continuously during labor to the client with sickle cell anemia to help ensure adequate
oxygenation and prevent sickling. Maintaining asepsis, monitoring vital signs, and placing a wedge under the hip are
interventions required of all clients, with or without sickle cell anemia. Although they are appropriate nursing interventions,
they are not used to prevent sickling crisis.
Test-Taking Strategy: Use the process of elimination, focusing on the subject, prevention of sickling crisis. Also, use your
knowledge of the ABCs (airway, breathing, and circulation). The correct option involves oxygenation. Review care of the
client in labor who has sickle cell anemia if you had difficulty with this question.
38. A client arrives at the clinic for her first prenatal assessment. The client tells the nurse that the first day of her last
menstrual period (LMP) was September 19, 2013. Using Nageles Rule, the nurse calculates the estimated date of
delivery as:
A. May 26, 2014
B. June 12, 2014
C. June 26, 2014 Correct
D. May 12, 2014
Rationale: Accurate use of Nageles Rule requires that the woman have a regular 28-day menstrual cycle. It is calculated
by subtracting 3 months from the first day of the LMP, adding 7 days, and then adding 1 year to that date.
First day of the LMP: September 19, 2013; subtract 3 months: June 19, 2013; add seven days: June 26, 2013; add 1 year:
June 26, 2014.
Test-Taking Strategy: Knowledge regarding the use of Nageles Rule is required to answer this question. Use this rule to
calculate the estimated date of delivery. Review Nageles Rule if you had difficulty with this question.
39. A nurse is preparing to care for a client experiencing dystocia. To which of the following interventions does the nurse give
priority?
A. Monitoring fetal status Correct
B. Providing comfort measures
C. Changing the clients position
D. Informing the clients partner of the progress of the labor
Rationale: The priority intervention is monitoring fetal status. Once this is done, the nurse provides maternal comfort
measures, including positioning the client, because this may decrease anxiety and hasten the progression of labor.
Keeping the clients partner informed of the progress of the labor is also an important aspect of client care during labor but
is not an immediate priority.
Test-Taking Strategy: Note the strategic word priority. Use Maslows Hierarchy of Needs theory and your knowledge of
the ABCs (airway, breathing, and circulation) to answer the question. Remember that physiological needs are the priority.
Review priority nursing interventions for the client with dystocia if you had difficulty with this question.
40. A nurse in the labor room is preparing to care for a client with hypertonic uterine dysfunction. The nurse is told that the
client is experiencing uncoordinated contractions that are erratic in their frequency, duration, and intensity. What is the
priority nursing intervention in the care of this client?
A. Providing pain relief Correct
B. Preparing the client for amniotomy
C. Monitoring the oxytocin (Pitocin) infusion closely
D. Encouraging the client to ambulate every 30 minutes
Rationale: Management of hypertonic uterine dysfunction depends on the cause. Relief of pain is the primary intervention
in promoting a normal labor pattern. Therapeutic management of hypotonic uterine dysfunction includes oxytocin
augmentation and amniotomy to stimulate labor progression. The client with hypertonic uterine dysfunction would be
encouraged to rest, not to ambulate every 30 minutes.
Test-Taking Strategy: Use the process of elimination, focusing on the strategic words hypertonic and priority. This, plus
knowledge of the management of this condition, should direct you to the correct option. Also eliminate the options that are
therapeutic measures for hypotonic uterine dysfunction and would stimulate labor (i.e., oxytocin augmentation and
amniotomy). If you had difficulty with this question, review the management of hypertonic uterine dysfunction.
41. Placental abruption is suspected in a client who is experiencing vaginal bleeding. On assessment, which of the following
findings would the nurse expect to note?
A. Abdomen soft to palpation
B. Uterine tender to palpation Correct
C. Uterine contractions every 3 to 5 minutes
D. Lack of uterine irritability or tetanic contractions
Rationale: Vaginal bleeding in a pregnant client is most often caused by placenta previa or a placental abruption. Uterine
tenderness accompanies placental abruption, especially with a central abruption and trapped blood behind the placenta.
The abdomen will feel hard and board-like on palpation as the blood penetrates the myometrium, causing uterine
irritability and maternal tenderness. A normal uterine contraction pattern is unusual in the presence of a placental
abruption. A sustained tetanic contraction may occur if the client is in labor and the uterine muscle cannot relax.
Test-Taking Strategy: Focus on the diagnosis, placental abruption. Remember that uterine pain and tenderness occurs
with an abruption. Review the characteristics of placental abruption if you had difficulty with this question.
42. A client admitted to the maternity unit 12 hours ago has been experiencing strong contractions every 3 minutes but has
remained at station 0. The fetal heart rate on admission was 140 beats/min and regular. The fetal heart rate is slowing,
and a persistent nonreassuring fetal heart rate pattern is present. The appropriate nursing action in this situation is:
A. Preparing to induce labor
B. Turning the client on her left side
C. Preparing the client for a cesarean delivery Correct
D. Continuing to monitor the fetal heart rate pattern
Rationale: Dystocia, failure of labor to progress, and a persistent nonreassuring fetal heart rate pattern are indications of
the need for cesarean delivery. Induction of labor is not indicated in this case because the client has been in labor for 12
hours without progress and signs of fetal distress are present. Placing the client on her left side will increase oxygen to the
uterus by relieving pressure on the aorta and the inferior vena cava. However, this intervention would be implemented
with any client in labor, not specifically with a client experiencing dystocia. Monitoring the fetal heart rate pattern is also
appropriate for any client in labor and is not the appropriate nursing action in this situation.
Test-Taking Strategy: Focus on the data presented in the question. Eliminate turning the client on her left side and
monitoring the fetal heart rate pattern first, because these are nursing actions for all clients in labor. Induction of labor is
not indicated in this case, because the client has been in labor for 12 hours and the fetus is in distress. Review the
indications for cesarean delivery if you had difficulty with this question.
43. A nurse is caring for a client experiencing a partial placental abruption. The client is uncooperative, refusing any
interventions until her husband arrives at the hospital. The nurse analyzes the clients behavior as most likely the result of:
A. Emotional immaturity
B. A stubborn personality
C. Anxiety and the need for support Correct
D. An undiagnosed psychiatric disorder
Rationale: Any of the situations identified in the options could contribute to the clients behavior, but the most likely reason
is anxiety. Anxiety is the only emotion that supports the information identified in the question. The client may be anxious
about the unknown effects of complications and want the presence of a support person while she deals with the crisis.
There is no information in the question to support the other options.
Test-Taking Strategy: Use the process of elimination, focusing on the data in the question. Noting the strategic words
refusing any interventions until her husband arrives will direct you to the correct option. Additionally, there is no
information in the question to support the remaining options. Review the psychosocial aspects of care for a client with a
partial placental abruption if you had difficulty with this question.
44. During a prenatal visit, the nurse notes that an adolescent pregnant client with diabetes mellitus has lost 10 lb during the
first 15 weeks of gestation. The nurse discusses the weight loss with the client, and the client states, I dont eat regular
meals. The appropriate response is:
A. Weight loss could hurt your baby.
B. Lets make a list of what youre eating. Correct
C. Ill have the doctor review your diet history.
D. Its all right to gain weight during pregnancy.
Rationale: It is important for the nurse to obtain additional information from the client. The nurse is using the therapeutic
communication tool of validation and clarification to obtain more information about the clients diet. The other options will
block communication. The statement regarding harm to the baby devalues the client and shows disapproval. Informing the
physician is avoiding the issue, and telling the client that it is all right to gain weight provides false reassurance.
Test-Taking Strategy: Use your knowledge of therapeutic communication techniques. Note that making a list of what the
client is eating will encourage communication. It is also a means of gathering assessment data, the first step in the
nursing process. Review therapeutic communication techniques if you had difficulty with this question.
45. A nurse instructs a pregnant client about foods that are high in folic acid. Which item does the nurse tell the client is the
best source of folic acid?
A. Milk
B. Steak
C. Chicken
D. Lima beans Correct
Rationale: The best sources of folic acid are liver; kidney, pinto, lima, and black beans; and fresh dark-green leafy
vegetables. Other good sources of folic acid are orange juice, peanuts, refried beans, and peas. Milk is high in calcium.
Chicken and steak are high in protein.
Test-Taking Strategy: Use the process of elimination and focus on the subject, the best source of folic acid. Eliminate the
options that are comparable or alike in that they are high in protein. Next eliminate milk, recalling that milk is high in
calcium. Review the foods high in folic acid if you had difficulty with this question.
46. Rho(D) immune globulin (RhoGam) is prescribed for a client after delivery. Before administering the medication, the nurse
reviews the clients history. Which of the following findings is a contraindication to administration of the medication?
A. A previous hypersensitivity reaction to immune globulin Correct
B. Delivery of an Rh-positive infant by an Rh-negative woman
C. Amniocentesis in an Rh-negative woman carrying an Rh-positive fetus
D. Known or suspected entry of Rh-positive fetal blood cells to the circulation of an Rh-negative woman
Rationale: One contraindication to the administration of Rho (D) immune globulin is previous hypersensitivity to immune
globulin. Rho (D) immune globulin is indicated when an Rh-negative client is exposed to Rh-positive fetal blood cells in any
way, including amniocentesis. The other options are all indications for administering RhoGam.
Test-Taking Strategy: Use the process of elimination and focus on the subject, a contraindication. Read each option
carefully and note the word hypersensitivity in the correct option. Review the contraindications to and precautions for the
administration of this medication if you had difficulty with this question.
47. A nurse is assisting a midwife who is assessing a client for ballottement. Which action does the nurse anticipate that the
midwife will employ to test for ballottement?
A. Assessing the cervix for thinning
B. Auscultating for fetal heart sounds
C. Performing a sudden tap on the cervix Correct
D. Palpating the abdomen for fetal movement
Rationale: Near midpregnancy, a sudden tap on the cervix during a vaginal exam may cause the fetus to rise in the
amniotic fluid and then rebound to its original position, a phenomenon known as ballottement. The examiner feels the
rebound when the fetus falls back down. Ballottement has no relationship to cervical assessment findings, fetal heart
sounds, or external palpation of fetal movement.
Test-Taking Strategy: Knowledge regarding the assessment of ballottement is required to answer this question. It is
necessary to know that when the cervix is tapped, the fetus floats upward in the amniotic fluid and that the rebound is
known as ballottement. If you are unfamiliar with this assessment technique, review this procedure.
48. A nurse is preparing to assess the fetal heartbeat in a pregnant woman who is at gestational week 12. Which piece of
equipment does the nurse use to assess the fetal heartbeat?
A. Fetoscope
B. Adult stethoscope
C. Electronic Doppler Correct
D. Fetal heart monitor
Rationale: The fetal heartbeat can be heard with the use of a fetoscope at 18 to 20 weeks gestation. When an electronic
Doppler ultrasound device is used, the fetal heartbeat can be detected as early as 10 weeks gestation. An adult
stethoscope will not adequately produce the fetal heartbeat. A fetal heart monitor is used during labor or in other situations
when the fetal heart rate requires continuous monitoring.
Test-Taking Strategy: Use the process of elimination. Eliminate an adult stethoscope first by focusing on the subject, fetal
heart rate. To select from the remaining options, note the words gestational week 12, which will direct you to the correct
option. If you had difficulty with this question, review the methods of assessing the fetal heart rate.
49. A postpartum client asks a nurse when she may safely resume sexual activity. The nurse tells the client that she may
resume sexual activity:
A. At any time
B. In 2 to 4 weeks Correct
C. After the 6-week physician checkup
D. When her normal menstrual period has resumed
Rationale: Usually a woman may engage safely in sexual intercourse during the second to fourth week after childbirth as
long as she experiences no discomfort during intercourse. The other options are incorrect. Engaging in intercourse too
early in the postpartum course could result in further injury to perineal tissues damaged during childbirth. It usually takes
about 3 weeks for an episiotomy to heal; therefore, it is unnecessary to wait 6 weeks. Menstruation may not resume in a
postpartum woman for 12 weeks to 6 months after childbirth.
Test-Taking Strategy: Knowledge of the instructions given to a new mother regarding sexual activity after delivery is
required to answer this question. Recalling that it takes about 3 weeks for an episiotomy to heal will direct you to the
correct option. Review postpartum instructions if you had difficulty with this question.
50. A clinic nurse is developing a plan of care for a pregnant client with AIDS. Which problem does the nurse identify as the
priority to be addressed in the plan of care?
A. Poor hygiene
B. Inverted nipples
C. History of IV drug use Correct
D. Intake of fewer than 6 glasses of fluid daily
Rationale: AIDS is a breakdown in immune function caused by a retrovirus known as human immunodeficiency virus, or
HIV. The infected person contracts opportunistic infections or malignancies that ultimately are fatal. For this reason, the
prevention of infection is a priority of nursing care. Although poor hygiene may affect the clients risk for infection,
addressing and helping the client cease her use of IV drugs, which is an immediate contributor to the risk for infections, is
priority. Inverted nipples and intake of less than 6 glasses of fluid daily are not specifically related to this syndrome.
Test-Taking Strategy: Note the strategic word priority. Recalling that AIDS affects the bodys immune system and
remembering the factors that increase the risk for infections will direct you to the correct option. If you had difficulty with
this question, review the priority concerns related to the client with AIDS.
51. A home care nurse is instructing a client with hyperemesis gravidarum about measures to ease the nausea and vomiting.
The nurse tells the client to:
A. Eat foods high in calories and fat
B. Lie down for at least 20 minutes after meals
C. Eat carbohydrates such as cereals, rice, and pasta Correct
D. Consume primarily soups and liquids at mealtimes
Rationale: Low-fat foods and easily digested carbohydrates such as fruit, breads, cereals, rice, and pasta provide
important nutrients and help prevent a low blood glucose level, which can cause nausea. Soups and other liquids should
be taken between meals to avoid distending the stomach and triggering nausea. Sitting upright after meals reduces
gastric reflux. Additionally, food portions should be small and foods with strong odors should be eliminated from the diet,
because food smells often incite nausea.
Test-Taking Strategy: Use the process of elimination and focus on the clients diagnosis and the subject, ways to ease
and prevent nausea and vomiting. Knowing that foods high in fat may be difficult to digest will assist you in eliminating this
option. Next eliminate the option that involves consuming primarily soups and fluids at meals, recalling that liquids will
cause distention of the stomach. To select from the remaining options, recall that lying down after meals can cause gastric
reflux; this will direct you to the correct option. Review measures to ease and prevent nausea and vomiting if you had
difficulty with this question.
52. After an unplanned cesarean section, the nurse finds the client in emotional distress, tearfully expressing bewilderment,
sadness, and feelings of failure and regret because she could not deliver vaginally. Which of the following conclusions
should the nurse make?
A. The client is experiencing anger.
B. The client is experiencing low self-esteem. Correct
C. The client is experiencing extreme discomfort.
D. The client is experiencing an inability to manage the stressors of surgery.
Rationale: Situational-low self-esteem represents temporary negative feelings about self in response to an event. This is a
normal response to cesarean section. Anger is commonly a response to a lack of information or the ability to perform
psychomotor skills in connection with a condition or treatment. When a person is unable to manage stressors adequately,
the emotional condition is usually one of hopelessness and helplessness. Extreme discomfort is usually evidenced by
writhing, moaning, screaming, or total withdrawal. The condition described in the question is not one of extreme
discomfort. The information provided in the question best supports the conclusion stated in the correct option.
Test-Taking Strategy: Use the process of elimination, focusing on the data in the question. Focusing on the strategic
words feelings of failure and regret will direct you to the correct option. Review the defining characteristics of low self-
esteem if you had difficulty with this question.
53. A nurse assists the primary healthcare provider in performing an amniotomy on a client in labor. In which order should the
nurse perform the following actions after the amniotomy? Assign the number 1 to the first action and the number 5 to the
last action.
The correct order is:
1. Determining the fetal heart rate
2. Noting the quantity, color, and odor of the amniotic fluid
3. Taking the clients temperature, pulse, and blood pressure
4. Replacing soiled underpads from beneath the clients buttocks
5. Planning evaluation of the client for signs and symptoms of infection
Rationale: After amniotomy, the fetal heart rate is assessed for at least 1 full minute for changes associated with prolapse
or compression of the umbilical cord and the characteristics of the fluid are noted as an indicator of fetal risk. After the
fluid has been assessed, the next concern is evaluation of the maternal vital signs. The clients comfort (i.e., the soiled
underpads) is considered next. With the ruptured membranes comes an increased risk for maternal infection. For this
reason, the client is frequently assessed for signs and symptoms of infection throughout the course of labor.
Test-Taking Strategy: Use principles of prioritizing and your knowledge of the ABCs (airway, breathing, and circulation) to
answer this question. Fetal heart rate is associated with fetal breathing and circulation. Once the fetal condition has been
assessed, the focus is turned to the mothers condition. The amniotic fluid is checked next because this action will take
little time, followed by vital signs. Finally client comfort is provided, followed by the planning of further care. If you had
difficulty with this question, review the priority nursing actions after amniotomy.
54. A nurse assessing a pregnant clients deep tendon reflexes notes a reflex of 2+. The nurse should:
. Document the finding Correct
A. Reassess the reflexes in 15 minutes
B. Report the finding to the physician immediately
C. Ask another nurse to check the reflexes to verify the finding
Rationale: The normal deep tendon reflex response is an extension and upward thrusting of the foot. A 1+ response
indicates a diminished response; 2+ indicates normal response; 3+ indicates increased response, brisker than average;
and 4 + indicates a very brisk, hyperactive response. The nurse would document the finding. The actions set forth in the
remaining options are unnecessary. If the reflexes were 3+ or 4+, the physician would be notified, because these findings
suggest preeclampsia.
Test-Taking Strategy: Knowledge regarding assessment of the deep tendon reflexes and the interpretation of assessment
findings is required to answer this question. Remember that 2+ is a normal response. Review this assessment technique if
you had difficulty with this question.
55. Immediately after the delivery of a newborn infant, the nurse prepares to deliver the placenta. The nurse initially:
. Pulls on the placenta as it enters the vaginal canal
A. Pulls on the umbilical cord as the mother bears down
B. Applies strong traction on the cord when signs of separation occur
C. Instructs the mother to push when signs of separation have occurred Correct
Rationale: To assist in the delivery of the placenta, the woman is instructed to push when signs of separation have
occurred. If possible, the placenta should be expelled by means of maternal effort during a uterine contraction. Alternate
compression and elevation of the fundus plus minimal controlled traction on the umbilical cord may be used to facilitate
delivery of the placenta and amniotic membranes.
Test-Taking Strategy: Use the process of elimination. Noting the strategic word initially and recalling that the placenta is
attached to the uterine wall will direct you to the correct option. Pulling on the umbilical cord and placing excess traction
on the cord when signs of separation occur may put the client at risk for uterine inversion. Review the procedure for
placental delivery if you had difficulty with this question.
56. A nurse is caring for a client with preeclampsia who is receiving a magnesium sulfate infusion to prevent eclampsia.
Which finding indicates to the nurse that the medication is effective?
. Clonus is present.
A. Magnesium level is 10 mg/dL.
B. Deep tendon reflexes are absent.
C. The client experiences diuresis within 24 to 48 hours. Correct
Rationale: Magnesium sulfate is effective in preventing seizures (eclampsia) if diuresis occurs within 24 to 48 hours of the
start of the infusion. As part of the therapeutic response, renal perfusion is increased and the client is free of visual
disturbances, headache, epigastric pain, clonus (the rapid rhythmic jerking motion of the foot that occurs when the clients
lower leg is supported and the foot is sharply dorsiflexed), and seizure activity. Hyperreflexia indicates cerebral irritability.
Clonus is normally not present. The therapeutic magnesium level is 4 to 8 mg/dL. Reflexes range from 1+ to 2+ but should
not be absent.
Test-Taking Strategy: Use the process of elimination and focus on the strategic words medication is effective. Recalling
the actions of this medication and expected assessment findings after a client receives magnesium sulfate will direct you
to this option. Review the expected assessment findings for a client receiving magnesium sulfate if you had difficulty with
this question.
57. A delivery room nurse is preparing a client for a cesarean delivery. The client is placed on the delivery room table, and the
nurse positions the client:
. Prone
A. In a semi-Fowler position
B. In the Trendelenburg position
C. Supine with a wedge under the right hip Correct
Rationale: The pregnant client is positioned so that the uterus is displaced laterally to prevent compression of the inferior
vena cava, which causes decreased placental perfusion. This is accomplished by placing a wedge under the hip.
Positioning for abdominal surgery necessitates a supine position. The Trendelenburg position places pressure from the
pregnant uterus on the diaphragm and lungs, decreasing respiratory capacity and oxygenation. A semi-Fowler or prone
position is not practical for this type of abdominal surgery.
Test-Taking Strategy: Focus on the type of surgical procedure and the anatomy of a pregnant woman. Use the process of
elimination and visualize each of the positions. This will direct you to the correct option. Review care of the client
undergoing a cesarean delivery if you had difficulty with this question.
58. A nurse is conducting a home visit with a mother and her 1-week-old infant, who is at risk for acquired neonatal congenital
syphilis. Which finding specific to this disease does the nurse look for while assessing the infant?
. Diarrhea
A. Hypothermia
B. Vigorous feeding
C. A copper-colored rash Correct
Rationale: Signs of congenital neonatal syphilis including poor feeding, slight hyperthermia, and snuffles (copious
clear serosanguinous mucous discharge from the nose) may be nonspecific at first. By the end of the first week,
however, a copper-colored maculopapular dermal rash is characteristically observed on the palms and soles, in the diaper
area, and around the mouth and anus. Diarrhea is not specifically associated with this condition.
Test-Taking Strategy: Specific knowledge regarding the signs and symptoms of acquired neonatal congenital syphilis in a
1-week-old infant is required to answer this question. If you had difficulty with this question, review the signs of this
infection.
59. A nurse is preparing to perform the Leopold maneuvers on a pregnant client. The nurse should first:
. Locate the fetal heart tone
A. Position the woman supine
B. Ask the client to empty her bladder Correct
C. Count the fetal heart rate for 1 minute
Rationale: In preparation for the Leopold maneuvers, the nurse first asks the woman to empty her bladder, which will
contribute to the womans comfort during the examination. Next the nurse positions the client supine with a wedge placed
under the hip to displace the uterus. Often the Leopold maneuvers are performed to aid the examiner in locating the fetal
heart tones. Counting the fetal heart rate is not associated with Leopold maneuvers.
Test-Taking Strategy: Note the strategic word first. Knowing that Leopold maneuvers are often used to help locate fetal
heart tones and involve palpation will assist you in determining that asking the client to empty the bladder is the first
action. Review the procedure for the Leopold maneuvers if you had difficulty with this question.
60. A nurse is assessing a newborn infant with a diagnosis of gastroschisis. The nurse expects to note that the bowel is
located:
. Inside the abdominal cavity, under the skin
A. Inside the abdominal cavity, under the dermis
B. Outside the abdominal cavity and not covered with a sac Correct
C. Outside the abdominal cavity but inside a translucent sac covered with peritoneum and amniotic
membrane
Rationale: Gastroschisis is the herniation of the bowel through a defect in the abdominal wall to the right of the umbilical
cord. The bowel is located outside the abdominal cavity and is not covered with a sac. Inside the abdominal cavity, under
the dermis or skin, is the description of an umbilical hernia. Outside the abdominal cavity but inside a translucent sac
covered with peritoneum and amniotic membrane is the description of an omphalocele.
Test-Taking Strategy: Use the process of elimination. Eliminate first the options that are comparable or alike (i.e., under
the skin and under the dermis). To select from the remaining options, it is necessary to recall the description of
gastroschisis. Review the characteristics of gastroschisis if you are unfamiliar with it.
61. A nurse answers a call light in the room of a woman who was just admitted in early latent labor. The woman is lying flat on
her back on the bed. The husband reports excitedly, I think my wife is going into shock or something! She was just lying
there, and then she turned so pale, and her hands are so clammy. She said she was dizzy and sick to her stomach. The
nurse notes on the noninvasive blood pressure monitor that the womans pulse is 58 beats/min and her blood pressure is
90/50 mm Hg. The nurse interprets these findings as indications that the woman is experiencing:
. Anxiety related to the onset of labor
A. Progression from latent to active first-stage labor
B. Hyperventilation related to excitement at her first labor experience
C. Altered tissue perfusion related to hypotensive syndrome (vena cava syndrome) Correct
Rationale: In a pregnant woman, the supine position adds gravity pressure to the inferior vena cava, which is already
displaced and partially compressed by the full-term gravid uterus. The increased compression decreases cardiac output,
leading to beginning tissue hypoxia, which brings on the signs and symptoms described in the question. The signs and
symptoms identified in the question are not indicative of progression to active first-stage labor. There is no information in
the question to indicate that the client is experiencing hyperventilation or anxiety.
Test-Taking Strategy: Use the process of elimination, focusing on the data in the question. Recognizing that there is no
information in the question to indicate that the client is experiencing hyperventilation or anxiety will assist you in
eliminating these options. To select from the remaining options, note that the pulse and blood pressure are low and
remember the pathophysiology of hypotensive syndrome (vena cava syndrome), which will direct you to the correct
option. Review the signs and symptoms of hypotensive syndrome (vena cava syndrome) if you had difficulty with this
question.
62. A nurse teaching a pregnant client about measures to strengthen the pelvic floor instructs the client to:
. Walk half a mile 3 times a week
A. Drink at least 2 quarts of fluid per day
B. Perform Kegel exercises in 10 repetitions, three times per day Correct
C. Perform pelvic tilt exercises in 10 repetitions, three times per day
Rationale: Kegel exercises strengthen the pelvic floor (pubococcygeal muscle). The increased tone of this muscle is
beneficial during pregnancy and afterward. Walking is a general healthy measure but does not specifically strengthen the
pelvic floor. Fluid intake is an indicator of hydration, which is important for normal physiological function. Pelvic tilt
exercises ease backache.
Test-Taking Strategy: Use the process of elimination and focus on the subject, ways to strengthen the pelvic floor. This
focus will direct you to the correct option. Remember that Kegel exercises help strengthen the pelvic floor muscles. If you
had difficulty with this question, review the purpose of Kegel exercises.
63. A nurse is reviewing the records of the clients admitted to the maternity unit during the past 24 hours. Which of the
following clients does the nurse recognize as being at risk for the development of disseminated intravascular coagulation
(DIC)? Select all that apply.
. A client with septicemia Correct
A. A client with mild preeclampsia
B. A client with diabetes mellitus who delivered a 10-lb baby
C. A client who had a cesarean section because of abruptio placentae Correct
D. A client who delivered 12 hours ago and has lost 475 mL of blood
Rationale: DIC is a pathologic form of clotting that is diffuse and consumes large amounts of clotting factors, including
platelets, fibrinogen, prothrombin, and factors V and VII. In the obstetric population, DIC occurs as a result of abruptio
placentae, amniotic fluid embolism, dead fetus syndrome (in which the fetus has died but is retained in utero for at least 6
weeks), severe preeclampsia, septicemia, cardiopulmonary arrest, or hemorrhage. A loss of 475 mL is not considered
hemorrhage .A mild case of preeclampsia is not a risk factor for DIC. It is not unusual for a client with diabetes mellitus to
deliver a large baby, and this condition is unrelated to DIC.
Test-Taking Strategy: Use the process of elimination and focus on the subject, the client at risk for DIC. Thinking about
the pathophysiology of DIC and the conditions listed in the options will assist in answering correctly. Review the risk
factors associated with DIC if you had difficulty with this question.
64. A pregnant client is seen in the clinic for the first time. This is the clients first pregnancy, and the client tells the nurse that
she has diabetes mellitus. The nurse provides instruction to the client regarding health care during pregnancy. Which
statements by the client indicate the need for further instruction? Select all that apply.
. I need to follow the prescribed diabetic diet.
A. I need to limit my exercise while Im pregnant. Correct
B. I need to report signs of infection to my physician.
C. My insulin requirements may change while Im pregnant.
D. Ill come back for a prenatal visit every month during my first trimester. Correct
Rationale: Exercise is necessary for the pregnant diabetic client to help maintain control of her diabetes. Concepts related
to the timing of exercise, control of food intake, and insulin around the time of exercise should be reviewed with the client.
The prenatal visit schedule for clients with a history of diabetes mellitus is more frequent than the normal prenatal course.
In the first and second trimesters, prenatal visits should be scheduled every 1 to 2 weeks. The remaining statements are
correct, representing important information for the pregnant client with diabetes mellitus.
Test-Taking Strategy: Note the strategic words need for further instruction, which indicate a negative event query and
the need to select the incorrect client statement. Use the general principles of diabetic care to answer correctly. Recalling
that diet, medication, prenatal visit scheduling recommendations, infection risk, and exercise are important components of
diabetic care, which will direct you to the correct options. If you had difficulty with this question, review the prenatal
interventions and instructions for a diabetic client.
65. After the delivery of a newborn, a nurse performs an initial assessment and determines that the Apgar score is 8. The
nurse interprets this score as indicating that the infant:
. Requires vigorous resuscitation
A. Is adjusting well to extrauterine life Correct
B. Requires some resuscitative intervention
C. Is having difficulty adjusting to extrauterine life
Rationale: One of the earliest indicators of successful adaptation of the newborn infant is the Apgar score. Scoring ranges
from 0 to 10. A score of 7 to 10 indicates that the infant should have no difficulty adjusting to extrauterine life. A score of 4
to 6 indicates moderate difficulty that may require some resuscitative intervention. A score of 0 to 3 indicates severe
distress and the need for vigorous resuscitation.
Test-Taking Strategy: Recall that the Apgar score ranges from 0 to 10. Noting that the question addresses a score of 8
will direct you to the correct option. Also note that the incorrect options are comparable or alike in that each indicates a
problem with the newborn. If you had difficulty with this question, review this assessment test.
66. A clinic nurse is performing an assessment of an HIV-positive pregnant woman during the 32nd week of gestation. Which
finding requires further follow-up?
. Weight gain of 22 lb
A. Active fetal movement
B. Slight lower extremity edema
C. Increased shortness of breath and bilateral crackles in the lungs Correct
Rationale: HIV infection in a pregnant woman may result in both maternal and fetal complications. Fetal compromise may
occur as a result of premature rupture of the membranes, preterm birth, or low birth weight. Potential maternal effects
include an increased risk for opportunistic infections. Individuals in the later stages of HIV infection are susceptible to
other invasive conditions, such as tuberculosis and a wide variety of bacterial infections. The assessment finding in the
correct option could be indicative of an opportunistic infection and requires follow-up.
Test-Taking Strategy: Use the process of elimination. Eliminate the incorrect options because these are normal findings.
Additionally, use your knowledge of the ABCs airway, breathing, and circulation to direct you to the correct option.
Review care of the HIV-positive pregnant woman if you had difficulty with this question.
67. A nurse is monitoring a client who delivered a healthy newborn 12 hours ago. The nurse takes the clients temperature
and notes that it is 38C (100.4F). The most appropriate nursing action would be to:
. Contact the physician
A. Recheck the temperature in 1 hour
B. Encourage the intake of oral fluids Correct
C. Tell the client that antibiotics will be prescribed
Rationale: A temperature of 38C (100.4F) is common during the 24 hours after childbirth. It may be the result of
dehydration or normal postpartum leukocytosis. If the increased temperature persists for longer than 24 hours or exceeds
38C, infection is a possibility, and the fever is reported to the physician or nurse midwife. Because the client delivered
her baby just 12 hours ago, the most appropriate nursing action is to encourage the intake of oral fluids.
Test-Taking Strategy: Use the process of elimination. Note the strategic words 12 hours ago. Recalling that a low-grade
temperature is a common postpartum assessment finding will direct you to the correct option. Review normal vital sign
findings during a postpartum assessment if you had difficulty with this question.
68. A pregnant woman at 38 weeks gestation arrives at the emergency department, reporting bright-red vaginal bleeding but
denying pain. On the basis of this information, the nurse determines that the client may be experiencing:
. Placenta previa Correct
A. Abruptio placentae
B. Passage of the mucus plug
C. Rupture of the amniotic sac
Rationale: The primary symptom of placenta previa is painless vaginal bleeding in the second or third trimester of
pregnancy. Findings of abruptio placentae include dark-red vaginal bleeding and abdominal pain. A ruptured amniotic sac
is characterized by findings such as watery vaginal drainage. Passage of the mucus plug is manifested as pink or as
blood-tinged mucus.
Test-Taking Strategy: Use the process of elimination. Focus on the data in the question and recall that painless vaginal
bleeding occurs in placenta previa. If you had difficulty with this question, review the assessment signs associated with
the conditions identified in the options.
69. A nurse is assessing the lochia of a client who delivered a viable newborn 1 hour ago. Which type of lochia would the
nurse expect to note at this time?
. Lochia alba
A. Lochial clots
B. Lochia serosa
C. Dark-red lochia rubra Correct
Rationale: When the perineum is assessed, the lochia is checked for amount, color, and the presence of clots. The color
of the lochia during the fourth stage of labor (1 to 4 hours after birth) is dark red (rubra). This is an expected occurrence
until the third day after delivery. Then, from days 4 through 10, the discharge is brownish pink (serosa). Alba is a white
discharge that occurs on days 11 to 14.
Test-Taking Strategy: Use the process of elimination. Noting that the question refers to a client who gave birth 1 hour ago
will direct you to the correct option. Review postpartum assessment findings and the types of lochia if you had difficulty
with this question.
70. A woman being seen in the prenatal clinic and complains of morning sickness that continues throughout the day. What
does the nurse tell the client to do to overcome this discomfort?
. Drink fluids with meals
A. Eliminate the morning meal
B. Eat fatty or spicy foods only at the noontime meal
C. Eat dry crackers every 2 hours to prevent an empty stomach Correct
Rationale: Morning sickness, which is common during the first trimester of pregnancy, is associated with an increased
level of human chorionic gonadotropin (hCG) and changes in carbohydrate metabolism. Morning sickness most often
occurs when the pregnant woman arises (hence the name), although a few women experience it throughout the day. Self-
care measures include eating dry crackers or toast before getting out of bed, eating dry crackers every 2 hours to prevent
an empty stomach, eating small frequent meals, avoiding fatty or spicy foods, consuming fluids separately from meals,
and rising slowly from a lying or sitting position to help prevent orthostatic hypotension. The client should not eliminate
meals.
Test-Taking Strategy: Use the process of elimination. Noting the strategic words continues throughout the day and their
relationship to every 2 hours will direct you to the correct option. Review measures to relieve morning sickness if you
had difficulty with this question.
71. A client with preeclampsia who is receiving magnesium sulfate in an intravenous infusion exhibits signs of magnesium
toxicity. The nurse immediately prepares for the administration of:
. Vitamin K
A. Protamine sulfate
B. Calcium gluconate Correct
C. Naloxone hydrochloride
Rationale: Calcium gluconate is the antidote to magnesium sulfate because it antagonizes the effects of magnesium at
the neuromuscular junction. It should be readily available whenever magnesium is administered. Vitamin K is the antidote
in cases of hemorrhage induced by the administration of oral anticoagulants such as warfarin sodium (Coumadin).
Protamine sulfate is the antidote in cases of hemorrhage induced by the administration of heparin. Naloxone
hydrochloride is administered to treat opioid-induced respiratory depression.
Test-Taking Strategy: Focus on the subject of the question, the treatment for magnesium toxicity. Specific knowledge
regarding antidotes and the process of elimination will assist in directing you to the correct option. Review common
antidotes if you had difficulty with this question.
72. A nurse is caring for a client in precipitous labor. In which position does the nurse place the client?
.
A.
B.
C. Correct
Rationale: Priority nursing care of the woman in precipitous labor includes promotion of fetal oxygenation and maternal
comfort. A side-lying (lateral Sims) position enhances placental blood flow and reduces the effects of aortocaval
compression. Added benefits of this position are slowing of rapid fetal descent and minimization of perineal tearing. The
lateral Sims position also places less stress on the perineum. Because the upper leg is supported, the perineum can be
better visualized as well. The other options are not the most optimal positions.
Test-Taking Strategy: Focus on the subject, a client in precipitous labor. Recalling that precipitous labor is one in which
birth occurs within 3 hours of the onset of labor and visualizing each position in the options will direct you to the correct
option. Review care of the client in precipitous labor if you had difficulty with this question.
73. A nurse provides instruction regarding prenatal care to a client with a history of heart disease. The nurse tells the client
that:
. It is best to lie supine for sleep
A. Physical activity should be limited Correct
B. The amount of weight gained is not important
C. It is necessary to avoid contact with all individuals to help prevent infection
Rationale: Physical activity should be limited so that demand does not exceed the functional capacity of the heart. It is not
necessary to avoid contact with all individuals as a means of preventing infection, but contact with individuals with active
infections should be avoided. The client should avoid excessive weight gain, which increases demand on the heart. Too
much weight gain causes an increase in body requirements and stress on the heart. The client should lie on the left side
to promote blood return.
Test-Taking Strategy: Use the process of elimination. Eliminate the options containing the closed-ended words not and
all. To select from the remaining options, recall the concepts of blood return during pregnancy, which will assist you in
answering correctly. If you had difficulty with this question, review care of the pregnant client with heart disease.
74. After a vaginal delivery, a woman suddenly begins to complain of severe pelvic pain and extreme fullness in the vagina,
and the nurse suspects uterine inversion. The nurse immediately prepares to:
. Insert a Foley catheter
A. Perform fundal massage
B. Administer oxytocin (Pitocin)
C. Assist in repositioning the uterus through the vagina into a normal position Correct
Rationale: Uterine inversion occurs when the uterus turns completely or partially inside out, usually during the third stage
of labor. The physician tries to replace the uterus, by way of the vagina, in a normal position. If this is not possible,
laparotomy with replacement is performed. A hysterectomy may be required. Two intravenous lines are established to
allow rapid fluid and blood replacement. A tocolytic medication or general anesthesia usually is needed to relax the uterus
enough to replace it. To help ensure that the inverted fundus is not trapped in the cervix, oxytocin is not given until the
uterus has been repositioned. Fundal massage should be avoided if possible, but, if it is prescribed, it should be
conducted very carefully. A Foley catheter may be inserted to keep the bladder empty so that the uterus can contract well,
but this is not the immediate action.
Test-Taking Strategy: Use the process of elimination and note the strategic word immediately. Note the relationship
between the words uterine inversion in the question and the option in which the uterus is repositioned, through the
vagina, in its normal place. Review nursing interventions for the client with uterine inversion if you had difficulty with this
question.
75. A multigravida asks a nurse when she will be able to start feeling the fetus move. The nurse responds by telling the
mother that fetal movements will be noted as early as:
. 8 to 10 weeks of gestation
A. 11 to 13 weeks of gestation
B. 14 to 16 weeks of gestation Correct
C. 18 to 20 weeks of gestation
Rationale: The first recognition of fetal movements by the multigravida may occur as early as the 14th to 16th week of
gestation. The primigravida may not notice these sensations until week 18 or later. Therefore the other options are
incorrect.
Test-Taking Strategy: Use the process of elimination and your knowledge regarding quickening and the detection of fetal
movement by the mother. Note the strategic word multigravida. It is important to note that multigravidas usually detect
fetal movements earlier in pregnancy than do primigravidas. If you are unfamiliar with the timing of quickening, review this
assessment finding.
76. A nurse is monitoring a client after vaginal delivery notes a constant trickle of bright-red blood from the client's vagina. In
which order would the nurse perform the following actions? Assign the number 1 to the first action and the number 5 to
the last.
The correct order is:
0. Assessing the client's fundus
1. Checking the client's vital signs
2. Contacting the physician
3. Changing the client's peripads
4. Documenting the findings
Rationale: A constant trickle of bright-red blood may indicate abnormal bleeding and requires immediate attention. The
nurse first checks the clients fundus. Once it has been determined that the bleeding is not the result of a boggy uterus,
the nurse should check the vital signs to determine whether the blood loss has compromised the clients condition. Next
the nurse would contact the physician and report the bleeding, fundal height and condition, and vital signs. After
contacting the physician the nurse would attend to the clients comfort needs, including, in this case, frequent changes of
peripads. The nurse would document the findings once assessment and implementation had been completed and the
clients condition was considered stable.
Test-Taking Strategy: Think about the normal and abnormal postpartum assessment findings related to lochial flow. A
constant trickle of bright-red lochia indicates bleeding, and further assessment to determine the origin of bleeding should
be performed and the results reported to the physician. Once the physician has been contacted, the clients comfort needs
and documentation would be the final priority. Review postpartum assessment findings and actions to take if they are
abnormal if you had difficulty with this question.
77. A multigravida woman with a history of multiple cesarean births is admitted to the maternity unit in labor. The client is
experiencing excessively strong contractions, and the nurse monitors the client closely for uterine rupture. Which
assessment findings are indicative of complete uterine rupture? Select all that apply.
. Fetal bradycardia Correct
A. Maternal tachypnea Correct
B. Excessive vaginal bleeding
C. Increased uterine contractions
D. Maternal complaint of sudden sharp abdominal pain Correct
Rationale: In a complete uterine rupture, the woman may complain of sudden sharp, shooting abdominal pain and may
state that she felt like something gave way. If she is in labor, her contractions will cease and the pain is relieved. In a
complete uterine rupture, bleeding will be concealed, and therefore the client will exhibit signs of hypovolemic shock
resulting from hemorrhage (hypotension, tachypnea, pallor, and cool, clammy skin). The fetus is the most common
indicator of uterine rupture. Such changes in the fetal heart rate as late or variable decelerations, a decrease in baseline
variability, or an increase or decrease in rate are commonly exhibited during a rupture. If the placenta separates, the fetal
heart rate will be absent and fetal parts may be palpated through the abdomen.
Test-Taking Strategy: Focusing on the subject, complete uterine rupture, will assist you in eliminating increased uterine
contractions. Recalling that in a complete uterine rupture bleeding is concealed will assist you in eliminating excessive
vaginal bleeding. To select from the remaining options, recall the signs of shock; this will direct you to maternal
tachypnea. Fetal bradycardia and sudden sharp abdominal pain are also common indicators of complete uterine rupture.
Review the signs of complete uterine rupture if you had difficulty with this question.
78. A pregnant woman reports that she has just finished taking the prescribed antibiotics to treat her urinary tract infection but
expresses concern that her baby will be born with an infection. Which response should the nurse make to help ease these
fears?
. Urinary infections during pregnancy are common. Your baby will be fine.
A. Your developing baby cannot acquire an infection from you during pregnancy.
B. You shouldn't worry about this, because you had early prenatal care and are taking your prenatal
vitamins.
C. Now that you have taken the medication as prescribed, well keep monitoring you closely and repeat the
urine culture before you leave today. Correct
Rationale: Symptomatic bacteriuria has been associated with an increased risk of neonatal sepsis after delivery.
Appropriate antenatal care of a client with a urinary tract infection includes antibiotic treatment and follow-up with repeat
urine cultures. The correct option is the only therapeutic response and is the response that presents accurate information.
Test-Taking Strategy: Use the process of elimination and your knowledge of therapeutic communication techniques. This
will direct you to the correct option. Review therapeutic communication techniques if you had difficulty with this question.
79. A nurse is changing the diaper of a 1-day-old full-term female newborn. The nurse notes that the labia are edematous and
darker than the surrounding skin and that a white mucous vaginal discharge is present. On the basis of these findings, the
nurse determines that the appropriate action is:
. Notifying the physician
A. Documenting the findings Correct
B. Obtaining a specimen of the discharge for culture
C. Reviewing the mothers record to determine whether she has a history of gonorrhea
Rationale: The labia of a newborn female may be darker in color than the surrounding skin; this is a normal finding, a
result of exposure to the mothers hormones before birth. Edema of the labia and a white mucous vaginal discharge are
also normal. Therefore the nurse would document the findings. The other options are unnecessary.
Test-Taking Strategy: Use the process of elimination and focus on the data in the question. Recalling normal newborn
findings and remembering that the findings noted in the question are normal will direct you to the correct option. If you had
difficulty with this question, review normal newborn findings.
80. A client in the third trimester of pregnancy is complaining of urinary frequency, and the nurse instructs the client in
measures to alleviate the discomfort. Which statement by the client indicates an understanding of these self-care
measures?
. I need to drink at least 2000 mL of fluid a day. Correct
A. I should cut back on my fluid intake in the evening.
B. I need to avoid emptying my bladder so frequently.
C. I should avoid drinking large amounts of fluids during the day.
Rationale: Urinary frequency is present in the first trimester and late in the third trimester because of the pressure exerted
on the bladder by the enlarging uterus. Self-care measures for urinary frequency include frequent emptying of the bladder
(every 2 hours) and drinking at least 2000 mL of fluid a day. Restricting fluid intake at any time is incorrect; it could lead to
urinary stasis and fluid-volume deficit
Test-Taking Strategy: Use the process of elimination. Eliminate first the options that are comparable or alike (i.e.,
restricting fluid intake and avoiding large amounts of fluid). Realizing that it does not make sense to avoid emptying the
bladder frequently, which could lead to urinary stasis and cause discomfort, will assist you in eliminating this option.
Review measures for relieving the discomfort of urinary frequency if you had difficulty with this question.
81. A nurse is monitoring a pregnant client with placental abruption. Which pattern on the fetal monitor indicates to the nurse
that fetal tissue perfusion is adequate?
.
A.
B. Correct
C.
Rationale: Accelerations, shown in the correct answer, are brief temporary increases in the fetal heart rate of at least 15
beats/min from baseline and lasting at least 15 seconds. They are an indication of fetal well-being and an oxygenated
fetal central nervous system. Variable decelerations do not have the uniform appearance of early or late decelerations.
Early decelerations are decreases in the fetal heart rate to below baseline; late decelerations look similar to early
decelerations but begin well after the contraction begins and return to baseline after the contraction ends.
Test-Taking Strategy: Use the process of elimination and your knowledge of the indications of fetal well-being. To answer
this question correctly it is necessary to be able to interpret fetal heart rate patterns and identify those that indicate fetal
well-being. If you had difficulty with this question, review fetal heart rate patterns.
82. A nurse performing an assessment of a pregnant client prepares to auscultate the fetal heart sounds, using a Doppler
ultrasound stethoscope. By which week of gestation are fetal heart sounds audible with the use of this device?
. 4 weeks
A. 6 weeks
B. 8 weeks
C. 12 weeks Correct
Rationale: Fetal heart sounds can be heard with the use of a Doppler ultrasound stethoscope by 12 weeks of gestation
and can be heard with a fetoscope by 18 to 20 weeks of gestation. The gestational times of 4, 6, and 8 weeks are
incorrect because the fetal heart sounds cannot be heard with a Doppler ultrasound stethoscope this early in pregnancy.
Test-Taking Strategy: Knowledge regarding the auscultation of fetal heart sounds and when they are audible during
pregnancy is required to answer this question. Noting the strategic words Doppler ultrasound stethoscope in the
question direct you to the correct option. If you are unfamiliar with the assessment of and auscultation of fetal heart
sounds, review this procedure.
83. A hepatitis B screen is performed on a pregnant client, and the results indicate the presence of antigens in the maternal
blood. The nurse tells the client that:
. She must be retested in 1 week
A. Liver function tests will be prescribed
B. A repeat hepatitis screen will be performed during the pregnancy
C. The infant should receive both the vaccine and hepatitis immune globulin soon after birth Correct
Rationale: A hepatitis B screen is performed to detect the presence of antigens in maternal blood. If antigens are present,
the infant should receive hepatitis immune globulin and a vaccine soon after birth. Repeating the screen and prescribing
liver function tests are incorrect measures and are unnecessary.
Test-Taking Strategy: Use the process of elimination. Eliminate the options that are comparable or alike in that they
involve repeating the test. To select from the remaining options, recall that the concern is the effect on the fetus, which will
direct you to the correct option. Review the purpose and significance of the hepatitis B screen if you had difficulty with this
question.
84. A nurse performing an assessment of a pregnant client is preparing to take the clients blood pressure. The nurse
positions the client:
. Supine, on the left side
A. Supine, on the right side
B. Lying down with the arm in a horizontal position at heart level
C. In a sitting position with the arm in a horizontal position at heart level Correct
Rationale: Because position affects blood pressure in the pregnant woman, the method for obtaining blood pressure
should be standardized as much as possible. Blood pressure should be obtained with the client sitting position and the
arm supported in a horizontal position at heart level. Supine on the right or left side and lying down with the arm in a
horizontal position at heart level are both incorrect and could cause physiological stress that would affect the blood
pressure.
Test-Taking Strategy: Use the process of elimination. Eliminate the options that are comparable or alike in that they
involve indicate positioning the client lying down or supine. If you are unfamiliar with the procedure of taking a pregnant
clients blood pressure, review this procedure.
85. A pregnant client is positive for HIV. The client asks the nurse whether her newborn will contract the virus. The
appropriate response is:
. Yes, the newborn will also have the virus.
A. HIV can only be transmitted through sexual contact.
B. The newborn does have a risk of contracting the infection. Correct
C. The newborn will have signs of HIV at birth if the virus has been transmitted.
Rationale: An infant born to an HIV-positive mother is at risk for contracting the infection. The modes of transmission are
sexual, parenteral, and perinatal. Characteristically the newborn is asymptomatic at birth, but signs and symptoms in an
infected child usually become obvious during the first year of life. Therefore the remaining options are incorrect.
Test-Taking Strategy: Use the process of elimination. Simply knowing that the infant born to an HIV-positive mother is at
risk for contracting the infection will direct you to the correct option. Review the risks associated with pregnancy in an HIV-
positive woman if you had difficulty with this question.
86. A nurse working in a prenatal clinic is reviewing the records of several clients scheduled for prenatal visits today. Which
client does the nurse identify as being at risk for abruptio placentae?Select all that apply.
. A primipara
A. A 36- year-old
B. A hypertensive client Correct
C. A pack-a-day smoker Correct
D. A client who exercises regularly
Rationale: The cause of abruptio placentae is unknown, but several risk factors have been identified. Maternal use of
cocaine, which causes vasoconstriction of the endometrial arteries, is a leading cause. Other risk factors include
hypertension, cigarette smoking, abdominal trauma, and a history of previous premature separation of the placenta.
Test-Taking Strategy: Note the strategic words at risk and focus on the subject, abruptio placentae. The correct options
identify situations that could be harmful. Review the risk factors for abruptio placentae if you had difficulty with this
question.
87. A nurse is providing instructions to a mother of an infant with seborrheic dermatitis (cradle cap) about treatment of the
condition. The nurse tells the mother to:
. Avoid the use of shampoo on the infants scalp
A. Apply oil to the affected area on the infants scalp Correct
B. Wash the infants scalp daily, using only tepid water
C. Shampoo the infants scalp, avoiding the anterior fontanel area
Rationale: Seborrheic dermatitis, a chronic inflammation of the scalp or other areas of the skin, is characterized by yellow,
scaly, oily lesions. It sometimes results when parents do not wash over the anterior fontanel carefully for fear that they will
hurt the infant. Treatment includes the application of oil (e.g., mineral oil) to the area to help soften the lesions followed by
gentle removal of the scaly lesions with a comb before the head is shampooed. The nurse should teach the mother how to
shampoo the scalp and explain that she will not damage the fontanel with normal gentle shampooing. The scalp should be
rinsed well to remove all soap, which could cause irritation.
Test-Taking Strategy: Use the process of elimination. Eliminate the option containing the closed-ended word only. To
select from the remaining options, recall that this condition is characterized by the presence of scaly lesions; this will direct
you to the correct option. Review the treatment for seborrheic dermatitis (cradle cap) if you had difficulty with this
question.
88. A nurse is assessing a newborn with a diagnosis of congenital diaphragmatic hernia (CDH). Which assessment finding
would the nurse specifically expect to note in the newborn?
. Excessive oral secretions
A. Bowel sounds heard over the chest Correct
B. Hiccupping and spitting up after a meal
C. Coughing, wheezing, and short periods of apnea
Rationale: Clinical manifestations associated with CDH include diminished or an absence of breath sounds on the
affected side, bowel sounds heard over the chest, cardiac sounds heard on the right side of the chest, and respiratory
distress, including dyspnea, cyanosis, nasal flaring, tachypnea, retractions, and a scaphoid abdomen, that develops soon
after birth. The presence of excessive oral secretions is a clinical manifestation of esophageal atresia and
tracheoesophageal fistula. Hiccups and spitting up after meals are clinical manifestations of gastroesophageal reflux. A
hiatal hernia may be evidenced by coughing, wheezing, and short periods of apnea.
Test-Taking Strategy: Specific knowledge of the pathophysiology associated with CDH and knowledge that CDH is a
neonatal emergency will direct you to the correct option. If you had difficulty with this question, review the characteristics
of congenital diaphragmatic hernia.
89. A nurse is reviewing the medical record of a pregnant client with sickle cell anemia. To which of the following information
related by the client would the nurse give the highest priority?
. Poor appetite
A. Drinking less than 4 glasses of fluid daily Correct
B. Concern about her inability to care for her baby
C. Occasional slight dizziness when standing up
Rationale: Dehydration will precipitate sickling of the red blood cells in the person with sickle cell disease. Sickling can
lead to life-threatening consequences, such as an interruption of blood flow to the respiratory system and placenta, for the
pregnant woman and fetus. Therefore a low fluid intake is the priority. Although the clients complaints of poor appetite
and occasional dizziness on standing require attention, they are not the priority in this situation. The clients concerns
about being able to care for her baby may be a priority after delivery, depending on the specific client situation at the time.
Test-Taking Strategy: Use Maslow's Hierarchy of Needs theory to prioritize, remembering that physiological needs come
first. Using this principle, eliminate the option involving the clients concern about her inability to care for her baby. To
select from the remaining options, use your knowledge of sickle cell anemia to select the correct option. In this case, the
potential outcome, sickling, means that the clients deficient fluid volume is the priority. Review sickle cell anemia if you
had difficulty with this question.
90. A nurse is performing an assessment of a female client with suspected mittelschmerz. Which question does the nurse ask
the client to elicit data specific to this disorder?
. Do you have continuous heavy vaginal bleeding?
A. Do you have pain at the beginning of your period?
B. Do you have pain every time you have intercourse?
C. Do you have sharp pain on the right or left side of your pelvis? Correct
Rationale: Mittelschmerz ("middle pain") refers to pelvic pain that occurs midway between menstrual periods or at the time
of ovulation. The pain is due to growth of the dominant follicle within the ovary or to rupture of a follicle and subsequent
spillage of follicular fluid and blood into the peritoneal space. The pain, which is fairly sharp, is felt on the right or left side
of the pelvis. It generally lasts a few hours to 2 days, and slight (not profuse) vaginal bleeding may accompany the
discomfort. The pain is not associated with intercourse.
Test-Taking Strategy: Use the process of elimination. Recalling that mittelschmerz is middle pain, that this condition
occurs as a result of growth or rupture of the follicle, and that it generally lasts a few hours to 2 days will assist you in
answering correctly. If you are unfamiliar with this condition, review this content.
91. A nurse teaching a pregnant client about the expectations and complications of pregnancy is describing Braxton Hicks
contractions. The nurse tells the client these contractions:
. Indicate that labor has started
A. Must be reported to the physician
B. Are a common occurrence of pregnancy Correct
C. Necessitate bed rest for the remainder of the pregnancy
Rationale: Braxton Hicks contractions are irregular, painless contractions that occur throughout pregnancy, although many
expectant mothers do not notice them until the third trimester. Because Braxton Hicks contractions are a normal finding
experienced by many pregnant women during pregnancy, the other options represent inaccurate assumptions and an
unnecessary intervention.
Test-Taking Strategy: Use the process of elimination. Eliminate the options that are comparable or alike (i.e., labor has
started and the physician must be contacted). To select from the remaining options, recall that Braxton Hicks contractions
may occur throughout pregnancy; this will direct you to the correct option. If you had difficulty with this question, review
the physiology of Braxton Hicks contractions.
92. A woman in labor suddenly experiences chest pain and dyspnea, and the nurse suspects the presence of amniotic fluid
embolism (AFE). The nurse immediately:
. Notifies the family
A. Prepares the client for intubation
B. Administers oxygen to the woman Correct
C. Attaches a cardiac monitor to the woman
Rationale: Supportive interventions are instituted immediately to maintain cardiac and respiratory function, and oxygen is
a necessary supportive therapy. The woman is intubated, and positive end expiratory pressure (PEEP) may be
prescribed. The family should be notified; however, the nurse would first administer the oxygen, then prepare for
intubation. A cardiac monitor may be needed, but this is not the initial action.
Test-Taking Strategy: Use your knowledge of the ABCs airway, breathing, and circulation to answer the question.
This will easily direct you to the correct option. If you are unfamiliar with the care of a woman in labor with amniotic fluid
embolism (AFE), review this content.
93. A nurse is told that a newborn with myelomeningocele will be admitted to the newborn nursery. In which position does the
nurse plan to place the infant?
. Prone Correct
A. Supine
B. On the back, in semi-Fowler
C. On the back, in Trendelenburg
Rationale: A myelomeningocele is a neural tube defect caused by failure of the posterior neural tube to close. The
meninges are exposed through the surface of the skin in a herniated sac that may be either healed or leaking. One major
preoperative intervention is protection of the sac from injury to prevent its rupture and resultant risk of central nervous
system infection. The infant should be positioned in a side-lying or prone position to prevent pressure on the sac until
surgical repair can be performed. Supine positioning would increase pressure on the sac, thereby increasing the risk for
sac rupture.
Test-Taking Strategy: Focus on the newborns diagnosis and use the process of elimination. Eliminate the positions that
are comparable or alike in that they involve placing the newborn on the back. If you had difficulty with this question, review
care of a newborn with myelomeningocele.
94. A nurse is monitoring a fetal heart rate (FHR). The nurse documents a reassuring FHR pattern in the record on noting:
. Late decelerations
A. Variability of 6 to 25 beats/min Correct
B. No change in FHR as a result of fetal activity
C. An average baseline rate ranging between 80 and 100 beats/min
Rationale: Variability of 6 to 25 beats/min is a reassuring pattern. The FHR should accelerate with fetal activity. The
baseline range for the FHR is 110 to 160 beats/min. Late decelerations are a result of decreased uteroplacental perfusion
that causes a decrease in fetal oxygenation. Late decelerations are not a reassuring pattern.
Test-Taking Strategy: Use the process of elimination. Focus on the subject, a reassuring FHR pattern. Knowing that late
decelerations indicate a perfusion problem will assist you in eliminating this option. Eliminate the option in which the fetal
heart rate does not increase with activity, because this finding indicates a problem. Next recall that 80 to 100 beats/min is
too low for a FHR. If you had difficulty with this question, review the characteristics of normal and abnormal FHRs.
95. A nurse teaches a new mother how to perform umbilical cord care and how to recognize the signs of a cord infection.
Which of the following findings does the nurse tell the mother is an indicator of infection?
. A darkened, drying cord
A. Edema at the base of the cord Correct
B. A brownish-black cord with pinkness around the base
C. A brownish-black cord with some moistness at the base
Rationale: Symptoms of a cord infection include purulent drainage or redness or edema at the base of the cord. If
symptoms of infection occur, the mother should be instructed to notify the healthcare provider, because antibiotics are
necessary. The cord begins to dry shortly after birth. It turns a brownish black within 2 to 3 days and falls off within 10 to
14 days.
Test-Taking Strategy: Use the process of elimination and focus on the clinical manifestations associated with infection.
Noting the word edema will direct you to the correct option. Also, note that the incorrect options are comparable or alike
in that they all involve a darkened cord. Review the signs of an infected umbilical cord if you had difficulty with this
question.
96. A nurse is performing an assessment of a pregnant woman to determine whether labor has begun. For which sign of true
labor does the nurse assess the client?
. A lack of cervical changes
A. A soft uterus with indentable contractions
B. Contractions that are irregular in rhythm and duration
C. Contractions that begin in the lower abdomen and back and radiate over the entire abdomen Correct
Rationale: Discomfort and pain associated with true labor contractions typically begin in the lower abdomen and back,
then radiate over the entire abdomen. Mild, irregular contractions and a lack of changes in the cervix are findings
associated with false labor. A firm uterus is present when contractions occur.
Test-Taking Strategy: Note the subject, a sign associated with true labor. Eliminate a lack of cervical changes first,
because cervical changes are expected in true labor. In true labor, contractions are regular, so contractions that are
irregular in rhythm and duration are not a sign. A firm uterus (not soft) is present when contractions occur, so eliminate
this option. If you had difficulty with this question, review the characteristics of true and false labor.
97. A 1-hour oral glucose tolerance test is performed on a pregnant client, with a result of 155 mg/dL. The nurse tells the
client that:
. Daily NPH insulin will be needed
A. Her glucose level is within normal limits
B. A daily oral hypoglycemic agent will be prescribed
C. A 3-hour glucose tolerance test will likely be performed to confirm gestational diabetes Correct
Rationale: A maternal 1-hour blood glucose test may be prescribed as a screen for gestational diabetes. If it is increased
(140 mg/dL or greater), a 3-hour glucose-tolerance test may be recommended to confirm the presence of gestational
diabetes. Oral hypoglycemics and insulin would not be prescribed solely on the basis of an increased maternal 1-hour
glucose level. Additionally, oral hypoglycemic agents are contraindicated during pregnancy. A result of less than 140
mg/dL indicates no need for further glucose testing and continued routine prenatal care.
Test-Taking Strategy: Use the steps of the nursing process and an understanding of the results and purpose of a 1-hour
oral glucose tolerance test to address this question. Eliminate the daily oral hypoglycemic agent and daily NPH insulin
options because they are comparable or alike in that they represent the administration of medication to treat the increased
blood glucose. The correct option is the only one that identifies further assessment of the client because of an increased
result on 1-hour glucose testing. Review measures to evaluate and treat increased blood glucose in a pregnant client if
you had difficulty with this question.
98. A postpartum nurse instructs a new mother in how to bathe her newborn. Which statement by the mother indicates a need
for further instruction?
. I should bathe him after a feeding. Correct
A. I need to sponge-bathe him until the cord falls off.
B. I should check the temperature of the water before using it to bathe him.
C. I need to keep him covered as much as possible while Im giving him a bath.
Rationale: It is not advisable to bathe a newborn infant after a feeding, because handling the infant may cause
regurgitation. Controlling heat loss during the bath to help conserve the infants energy and prevent cold stress is a
priority, and the baby should be covered as much as possible during bathing. The baby should be given sponge bath until
the cord falls off. Additionally, the mother should check the temperature of the water before using it to bathe the infant as
a means of preventing burns.
Test-Taking Strategy: Note the strategic words need for further instruction, which indicate a negative event query and
the need to select the incorrect statements. Recalling that handling the infant could cause regurgitation will assist in
directing you to the correct option. Review teaching points for bathing of a newborn if you had difficulty with this question.
99. A nurse is assessing a woman in labor and notes the presence of accelerations on the fetal monitor tracing. Which of the
following actions should the nurse perform in response to this observation?
. Calling the physician
A. Documenting the finding Correct
B. Repositioning the mother
C. Taking the mothers vital signs
Rationale: Accelerations are transient increases in the fetal heart rate, normally caused by fetal movement or
accompanying contractions. Accelerations are a sign of fetal well-being and adequate oxygen reserve. No intervention
besides documentation is necessary in this situation.
Test-Taking Strategy: Use the process of elimination. Recalling that the presence of accelerations indicates fetal well-
being will direct you to the correct option. Review the description of accelerations if you are unfamiliar with this content.
100. A nurse caring for a hospitalized client with a diagnosis of abruptio placentae and develops a nursing care plan
incorporating interventions to be implemented in the event of shock. If signs of shock develop, to promote tissue
oxygenation, the nurse would immediately:
. Limit maternal activity
A. Turn the client on her side Correct
B. Monitor maternal vital signs
C. Provide emotional support to reduce anxiety
Rationale: With a client in shock, the goal is to increase perfusion to the placenta. The immediate nursing action would be
to turn the client on her side. This would increase blood flow to the placenta by relieving pressure from the gravid uterus
on the great vessels. The remaining options are also interventions that would be implemented, but only after this
immediate action had been taken. Additionally, oxygen at 8 to 10 L/min by way of face mask would be administered.
Test-Taking Strategy: Note the strategic word immediately. Use your knowledge of the ABCs (airway, breathing, and
circulation). Remember that the goal is to increase perfusion to the placenta. This will direct you to the correct option.
Review initial interventions for shock if you had difficulty with this question.
You might also like
- NCLEX-RN Prep Plus: 2 Practice Tests + Proven Strategies + Online + VideoFrom EverandNCLEX-RN Prep Plus: 2 Practice Tests + Proven Strategies + Online + VideoRating: 3 out of 5 stars3/5 (4)
- Ball & Bindler Pediatric Nursing - Caring For ChildrenDocument105 pagesBall & Bindler Pediatric Nursing - Caring For Childrenfriendofnurse50% (4)
- RN ATI Fundamentals Proctored Exam 2021Document7 pagesRN ATI Fundamentals Proctored Exam 2021Andrew Kang'ethe67% (3)
- Antenatal Glucocorticoid Therapy and Fetal Lung MaturationDocument32 pagesAntenatal Glucocorticoid Therapy and Fetal Lung Maturationcclaire197% (37)
- Maternal-Newborn Nursing DeMYSTiFieD: A Self-Teaching GuideFrom EverandMaternal-Newborn Nursing DeMYSTiFieD: A Self-Teaching GuideNo ratings yet
- Chicago Review Press NCLEX-PN Practice Test and ReviewFrom EverandChicago Review Press NCLEX-PN Practice Test and ReviewRating: 4 out of 5 stars4/5 (4)
- NCLEX: Pharmacology for Nurses: 100 Practice Questions with Rationales to help you Pass the NCLEX!From EverandNCLEX: Pharmacology for Nurses: 100 Practice Questions with Rationales to help you Pass the NCLEX!Rating: 5 out of 5 stars5/5 (4)
- Hesi Hints MaternityDocument4 pagesHesi Hints MaternityThomas Stewart91% (11)
- Test Bank For Maternity Nursing 8th Edition, LowdermilkDocument26 pagesTest Bank For Maternity Nursing 8th Edition, LowdermilkILL101100% (2)
- Introduction Maternity Pediatric Nursing 8th Leifer Test BankDocument11 pagesIntroduction Maternity Pediatric Nursing 8th Leifer Test Banksonyaaaq100% (4)
- Maternity Nclex RN ReviewDocument11 pagesMaternity Nclex RN ReviewKwai Browne100% (7)
- Final Exam MaternityDocument137 pagesFinal Exam MaternityJohanna Erazo Padilla100% (7)
- Family-Centered Nursing Care AssessmentDocument32 pagesFamily-Centered Nursing Care AssessmentMorgan100% (41)
- Maternity Exam 181920Document99 pagesMaternity Exam 181920Johanna Erazo Padilla100% (3)
- ATI OB Study GuideDocument26 pagesATI OB Study GuideThelma Jerome100% (1)
- HESI Test - Free Most Up To Date SampleDocument13 pagesHESI Test - Free Most Up To Date Sample22oct201481% (32)
- Maternity Nursing ReviewDocument8 pagesMaternity Nursing ReviewJulienne Sanchez-Salazar100% (2)
- ATI Maternal Newborn Chapter 1-ContraceptionDocument23 pagesATI Maternal Newborn Chapter 1-ContraceptionVin Lorenzo Campbell100% (4)
- Med-Surg Hesi CompilationDocument71 pagesMed-Surg Hesi CompilationJbl2328100% (4)
- Ati Nclex Review Ob Y6k2c6Document62 pagesAti Nclex Review Ob Y6k2c6Sunny100% (1)
- CH 13 Fluid and Electrolytes Balance and DisturbanceDocument20 pagesCH 13 Fluid and Electrolytes Balance and DisturbanceMicoJimenez80% (10)
- NCLEX Review of Maternal NursingDocument34 pagesNCLEX Review of Maternal NursingAlain Chery100% (2)
- DDocument56 pagesDDarren Balbas100% (1)
- New Text DocumentDocument3 pagesNew Text DocumentTro Wact100% (1)
- Peds ATI TakeawaysDocument4 pagesPeds ATI TakeawaysNiki95% (19)
- Ob Maternity NotesDocument46 pagesOb Maternity Notesr79cb5480100% (4)
- NCLEXstudyguidevmDocument31 pagesNCLEXstudyguidevmAnonymous vqG0paWG100% (1)
- Test Bank For Olds Maternal Newborn Nursing and Womens Health Across The Lifespan 8th Edition DavidsonDocument5 pagesTest Bank For Olds Maternal Newborn Nursing and Womens Health Across The Lifespan 8th Edition DavidsonJohnny Shields100% (25)
- Obstetric Questions: Please State Whether The Following Statements Are TRUE or FALSEDocument8 pagesObstetric Questions: Please State Whether The Following Statements Are TRUE or FALSEjulialeo90% (10)
- Child Evolve ExamDocument37 pagesChild Evolve Examfriendofnurse100% (14)
- Child Evolve ExamDocument37 pagesChild Evolve Examfriendofnurse100% (14)
- Hesi Practice Test ADocument15 pagesHesi Practice Test Avicnmar78% (9)
- Maternal-Newborn Care ATIDocument29 pagesMaternal-Newborn Care ATIAn Nguyen90% (20)
- Maternity QuestionsDocument49 pagesMaternity Questionsdeb100% (17)
- HESI PsyDocument16 pagesHESI PsyKrista Howe100% (13)
- Maternity Ati Key PointsDocument28 pagesMaternity Ati Key PointsVin Lorenzo Campbell100% (2)
- Ob HesiDocument1 pageOb HesiJoyzoey93% (27)
- Antidote: Calcium Gluconate or Calcium Chloride: Excessively Frequent Uterine Contractions During PregnancyDocument3 pagesAntidote: Calcium Gluconate or Calcium Chloride: Excessively Frequent Uterine Contractions During PregnancyCohort Six100% (1)
- Acid Base Self Study With Practice QuestionsDocument13 pagesAcid Base Self Study With Practice QuestionsfriendofnurseNo ratings yet
- Nursing Management of CAD and ACSDocument9 pagesNursing Management of CAD and ACSfriendofnurse100% (4)
- NATIONAL COUNCIL LICENSURE EXAMINATION FOR REGISTERED NURSES (NCLEX-RN): Passbooks Study GuideFrom EverandNATIONAL COUNCIL LICENSURE EXAMINATION FOR REGISTERED NURSES (NCLEX-RN): Passbooks Study GuideNo ratings yet
- Hesi MaternityDocument20 pagesHesi Maternityracquela_367% (3)
- 93.3% Level 3 On RN Maternal Newborn 2016, TipsDocument2 pages93.3% Level 3 On RN Maternal Newborn 2016, TipsOSAKA THOMAS100% (2)
- This Study Resource Was: ATI Maternal Newborn Proctored Exam Study Set 1Document4 pagesThis Study Resource Was: ATI Maternal Newborn Proctored Exam Study Set 1Gina Giammalvo100% (5)
- Ob Ati StudyDocument22 pagesOb Ati Studylpirman0580% (5)
- Maternity Study GuideDocument43 pagesMaternity Study Guidepgmanski100% (23)
- NLE PreBoard QuestionsDocument73 pagesNLE PreBoard QuestionsAaron Johnson Fantastico JarrellNo ratings yet
- Gi NclexDocument14 pagesGi NclexYoke W Khoo100% (3)
- NCM 107a Care of The Pregnant WomanDocument43 pagesNCM 107a Care of The Pregnant WomanMelchizedek Tagarino Torio100% (1)
- Neonatal Infections - Pathophysiology, Diagnosis, and Management 2018 PDFDocument254 pagesNeonatal Infections - Pathophysiology, Diagnosis, and Management 2018 PDFBao NguyenNo ratings yet
- Cardiomyopathy Nursing Concept MapDocument2 pagesCardiomyopathy Nursing Concept Mapfriendofnurse100% (1)
- Introduction Maternity Pediatric Nursing 7th Leifer Test BankDocument12 pagesIntroduction Maternity Pediatric Nursing 7th Leifer Test Banksonyaaaq0% (1)
- NCLEX Questions - OB MATERNITY QUESTIONS PDFDocument17 pagesNCLEX Questions - OB MATERNITY QUESTIONS PDFAnneRaquelTalentoNo ratings yet
- ATI PN Maternal Newborn NotesDocument13 pagesATI PN Maternal Newborn NotesDiamond Blackwell100% (6)
- Medsurg ATIDocument7 pagesMedsurg ATIloveoverpride12% (17)
- Pediatric RemediationDocument5 pagesPediatric RemediationAlvin L. Rozier67% (3)
- Maternity Ati RemediationDocument2 pagesMaternity Ati Remediationcse100% (1)
- ATI Maternal Newborn Proctored Study Guide (2018)Document8 pagesATI Maternal Newborn Proctored Study Guide (2018)Emma Lilly100% (6)
- Test Bank For Maternal Child Nursing Care 6th Edition by PerryDocument36 pagesTest Bank For Maternal Child Nursing Care 6th Edition by Perrygoodgeonneogaeanjlf6y100% (38)
- Maternity Nursing An Introductory Text 11th Edition Leifer Test BankDocument9 pagesMaternity Nursing An Introductory Text 11th Edition Leifer Test BankSerenaNo ratings yet
- 440 - Med Surg HESI 2Document8 pages440 - Med Surg HESI 2Chalcey Polson87% (15)
- Ob Final Exam Review Summary Maternity NursingDocument40 pagesOb Final Exam Review Summary Maternity NursingVin Lorenzo CampbellNo ratings yet
- Maternity Practice TestDocument12 pagesMaternity Practice TestJoslyn Gross87% (15)
- FHC AaaaAAADocument5 pagesFHC AaaaAAAJUANJOSEFOXNo ratings yet
- Nursingnotes - Info Maternal and Child NursingDocument54 pagesNursingnotes - Info Maternal and Child Nursinggrey26100% (1)
- Intrapartum Fetal MonitoringDocument15 pagesIntrapartum Fetal MonitoringAnuradha Maurya100% (1)
- Mcqforneonatology 120612005106 Phpapp02Document7 pagesMcqforneonatology 120612005106 Phpapp02DoctorSajid BuzdarNo ratings yet
- Chapter 25 26 27 28 29 30Document9 pagesChapter 25 26 27 28 29 30Laneshia Mason86% (7)
- 2009 HESI Practice - FundamentalsDocument14 pages2009 HESI Practice - FundamentalsQueennita100% (1)
- Maternal and Newborn-Labour and Delivery NotesDocument2 pagesMaternal and Newborn-Labour and Delivery NotesSavanna Chambers100% (2)
- Renal Medications WorksheetDocument11 pagesRenal Medications Worksheetfriendofnurse100% (1)
- Lecture Outline - Fluids and ElectrolytesDocument19 pagesLecture Outline - Fluids and Electrolytesfriendofnurse100% (1)
- CD4 count determines AIDS diagnosis and disease progressionDocument2 pagesCD4 count determines AIDS diagnosis and disease progressionfriendofnurseNo ratings yet
- Fundamentals of Nursing Chapter 12Document7 pagesFundamentals of Nursing Chapter 12friendofnurseNo ratings yet
- Prophylactic Antibiotics in LaborDocument17 pagesProphylactic Antibiotics in LaborAlejandra BuNo ratings yet
- 1 s2.0 S0266613823000384 MainDocument7 pages1 s2.0 S0266613823000384 MainMayte Muñoz RejaNo ratings yet
- Committee Opinion No 712 Intrapartum Management.57 PDFDocument7 pagesCommittee Opinion No 712 Intrapartum Management.57 PDFernestosandNo ratings yet
- Light, Zimbrunes, & Gomez-Lobo, 2017Document7 pagesLight, Zimbrunes, & Gomez-Lobo, 2017Anonymous 75M6uB3OwNo ratings yet
- Contraction Ring & Uterine Rupture GuideDocument4 pagesContraction Ring & Uterine Rupture GuideJessica Carmela CasugaNo ratings yet
- Oligohydramnios 11Document32 pagesOligohydramnios 11Otchi Pudtrie WijayaNo ratings yet
- PSYCHOLOGICAL CHANGES OF PREGNANCYDocument15 pagesPSYCHOLOGICAL CHANGES OF PREGNANCYPasay Trisha Faye Y.No ratings yet
- High Risk PregnancyDocument2 pagesHigh Risk PregnancyDianeNo ratings yet
- Active Management of The Third Stage of LabourDocument15 pagesActive Management of The Third Stage of LabourtyasNo ratings yet
- Endalews CV CredentialsDocument18 pagesEndalews CV CredentialsAmoure TubeeNo ratings yet
- Rh-Pregnancy 202240 184928Document2 pagesRh-Pregnancy 202240 184928siddharthNo ratings yet
- Case Analysis - Pregnant With AsthmaDocument1 pageCase Analysis - Pregnant With AsthmaJanine mae MacaraigNo ratings yet
- R.A. No. 11210: 105-Day Expanded Maternity Leave Law (EMLL)Document36 pagesR.A. No. 11210: 105-Day Expanded Maternity Leave Law (EMLL)Ritchelle Quijote DelgadoNo ratings yet
- Nursing Care for a Woman in LaborDocument7 pagesNursing Care for a Woman in LaborNicole cuencosNo ratings yet
- Hubungan Dukungan Keluarga Dengan Tingkat Kecemasna Ibu Hamil Menghadapi Proses PersalinanDocument7 pagesHubungan Dukungan Keluarga Dengan Tingkat Kecemasna Ibu Hamil Menghadapi Proses PersalinanAsryanty AmelindaNo ratings yet
- Ellis, Wojnar, & Pettinato, 2015Document8 pagesEllis, Wojnar, & Pettinato, 2015Anonymous 75M6uB3OwNo ratings yet
- Severe Tear Patient HandoutDocument12 pagesSevere Tear Patient HandoutIzz ShuhaimiNo ratings yet
- Bovine Cesarean Field Surgery TechniquesDocument21 pagesBovine Cesarean Field Surgery TechniquesAndres Luna MendezNo ratings yet
- Water Birth: Benefits and SafetyDocument21 pagesWater Birth: Benefits and SafetyudupisonyNo ratings yet
- Printable Pregnancy CalendarDocument10 pagesPrintable Pregnancy CalendarRodica Buga100% (1)
- Star Comprehensive Policy ClauseDocument16 pagesStar Comprehensive Policy ClauseGopinath PuralachettyNo ratings yet
- ANC Checkups Ensure Healthy PregnancyDocument18 pagesANC Checkups Ensure Healthy PregnancyHemamaliniNo ratings yet