Professional Documents
Culture Documents
Cardiovascular Video Assessment: Greeting
Uploaded by
Brittany L.Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cardiovascular Video Assessment: Greeting
Uploaded by
Brittany L.Copyright:
Available Formats
Cardiovascular Video Assessment
1. Greeting
Hello, Mr./Mrs. ______. Im ____, your family nurse practitioner student. Its
nice to meet you.
Tell me what brings you into the clinic today.
2. Health History:
History of Present Illness:
o When did it begin? Was it sudden or gradual?
o Where is it?
o How long are the episodes? Has it been constant or intermittent?
o Describe a typical attack. What does it feel like? How severe is it from
0-10?
o Does anything make it worse?
o Does anything make it better? What have you done to treat it? Have
you taken any medications for it?
o Do you have any associated symptoms?
Past Medical History: Now we are going to review your past medical
history.
o Have you ever had cardiac surgery?
o Have you ever been hospitalized for a cardiac disorder?
o Do you have a history of congenital heart disease? A rhythm
disorder? Acute rheumatic fever? Kawasaki disease?
o Have you ever been diagnosed with any chronic illnesses such as:
- Hypertension? Bleeding disorders? Clotting disorders?
Hyperlipidemia? Diabetes? Thyroid dysfunction? Coronary
Artery Disease? Obesity? Anemia?
o Have you ever had an MI or heart attack?
Family History:
o Has anyone in your family been diagnosed with:
- Long QT syndrome? Marfan syndrome? Diabetes? Heart
disease? Dyslipidemia? Hypertension? Obesity? Congenital
heart disease?
o Have there been any sudden cardiac deaths in your family?
Personal/Social History:
o What type of job do you do? Is it physically demanding? Are you
exposed to environmental hazards?
o Do you smoke or use tobacco?
o Do you drink alcohol?
o Do you use any illicit drugs such as cocaine or injection drugs?
o Do you exercise? How often? For how long?
3. Review of Systems: Identify the presence or absence of health-related
issues in the pertinent body system(s).
General:
o Have you had any fever? Chills? Malaise? Fatigue? Night sweats?
Weight changes?
Cardiac: Have you had any.
o Chest pain/distress? (causes, duration, timing, relieving factors)
o Palpitations?
o Dyspnea?
o Orthopnea? How many pillows do you sleep on?
o Edema?
o Exercise intolerance?
o Cyanosis?
o Cough?
o Loss of consciousness?
Vascular:
o Do you have any pain in your legs when walking? (frequency,
severity)
o Do you have a tendency to bruise/bleed?
4. General Survey:
Alertness & Orientation/Mental Status: Based on our interaction and his
responses thus far, the patient is alert and oriented x 4. He also follows
commands and answers questions appropriately.
Appearance: Patient appears calm, well-groomed and in no apparent
distress.
Heart Rate: palpate radial pulse for 30 sec & multiply by 2
o Regular rhythm with HR of __ beats per minute.
Respirations: count number of breaths for 30 sec & multiply by 2
immediately after counting pulse
o Respirations are regular and even with a rate of __ breaths per
minute.
Pain:
o Are you having any pain now? OLDCARTS
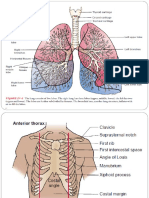
5. Estimation of Jugular Venous Pressure: I am now going to assess your jugular
venous pressure. Would you mind lying down for me?
Have patient supine at 30
Find point of pulsation in right jugular vein
Extend index card at right angle from meniscus point of pulsation to the
ruler, which should be placed vertically on the sternal angle (AKA Angle of
Louis; continuous with 2nd rib)
Read where card crosses the ruler & round to nearest centimeters of water
(should be < 9 cm)
6. Assessment of Carotid Pulses: I am now going to assess your carotid pulses.
I am inspecting your right and left carotid arteries and comparing sides.
I am now palpating each side to feel for thrills.
o Place index & middle finger on carotid artery in lower 3rd of neck &
press just inside the medial border of a well-relaxed
sternocleidomastoid muscle.
o Increase pressure until you feel a maximal pulsation.
o Decrease pressure to detect arterial wave & contour.
o Assess amplitude of pulse.
I am now auscultating your carotid arteries to listen for bruits. Can you hold
your breath for just a moment?
o Use diaphragm
7. Inspection of Chest: I am now inspecting your chest for lifts or heaves. Normally,
I would inspect a bare chest.
Rate, Rhythm, Depth, & Effort of Breathing
o Rate of respirations determined earlier. Regular rhythm and depth.
No increased effort of breathing. No lifts or heaves noted.
8. Palpation of Chest: I am now palpating your chest for heaves, lifts, & thrills.
Normally, I would palpate a bare chest.
Heaves, Lifts, Thrills
o Use finger pads to palpate for heaves & lifts at right & left 2nd
intercostal spaces, along the left sternal border, & in the apical area.
o Use ball of hand to palpate for thrills in the same locations.
Apical Impulse
o Palpate with finger pads & describe location, diameter, & amplitude.
o If cant feel it, ask pt to roll into left lateral decubitus position.
9. Auscultation of Chest: I am going to listen to your heart over various areas of
your chest. Normally, I would place my stethoscope on a bare chest.
Heart Rate/Rhythm in Key Locations:
o Listen for S1 & S2 at all 6 sites:
- Aortic area: Right 2nd intercostal space; sternal border
Use
- Pulmonic area: Left 2nd intercostal space; sternal border
diaphragm
- Erbs Point: Left 3rd intercostal space; sternal border
- Tricuspid Area: Left 4th & 5th intercostal spaces; sternal border
Use bell
- Mitral/Apex Area: Left 5th intercostal space; midclavicular line
o Will you please roll on your left side while I listen to your apical
impulse?
- Use bell to listen at apical impulse area
Lung Sounds: Will you please sit up so that I may listen to your lungs?
o Use diaphragm; have patient breathe slowly & deeply through the
mouth
o Comparing sides, start at top and work down
- 8 sites on front
- 10 sites on back
You might also like
- Nursing Mnemonics: The Ultimate Tips and Notes For NursesFrom EverandNursing Mnemonics: The Ultimate Tips and Notes For NursesRating: 5 out of 5 stars5/5 (1)
- APA Citations For Nursing TextbooksDocument1 pageAPA Citations For Nursing Textbooksbbianca199075% (4)
- Ebstein Anomaly, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandEbstein Anomaly, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Abdominal Assessment VideoDocument4 pagesAbdominal Assessment VideoAmber Nicole HubbardNo ratings yet
- SBAR Doris BowmanDocument2 pagesSBAR Doris BowmanM.I Dia Izibelle F. AMENAMENNo ratings yet
- Abdominal AssessmentDocument59 pagesAbdominal AssessmentSIR ONE100% (1)
- Assessing Newborns EffectivelyDocument35 pagesAssessing Newborns EffectivelyBaldwin Hamzcorp Hamoonga100% (1)
- Oxygen InhalationDocument47 pagesOxygen InhalationKomalNo ratings yet
- Respiratory Assessment FindingsDocument197 pagesRespiratory Assessment Findingsannatw100% (2)
- Cardiovascular AssessmentDocument21 pagesCardiovascular AssessmentRhitzle AnnNo ratings yet
- Nasogastric Tube GuideDocument7 pagesNasogastric Tube GuideAltrOi AgtangNo ratings yet
- Head to Toe Physical AssessmentDocument11 pagesHead to Toe Physical Assessmentالأغا محمد زكارنةNo ratings yet
- Critical Care Note PDFDocument10 pagesCritical Care Note PDFlml100% (1)
- Postural DrainageDocument6 pagesPostural DrainageKit Alizon Barredo0% (1)
- PT 2 Nurse NotesDocument1 pagePT 2 Nurse NotesAmy67% (3)
- Thorax and Lungs: Chapter EighteenDocument12 pagesThorax and Lungs: Chapter Eighteengrool29r67% (3)
- Physical Assessment of Cardiovascular SystemDocument31 pagesPhysical Assessment of Cardiovascular SystemaagNo ratings yet
- Nursing ProcessDocument19 pagesNursing Processmsncabanatuan100% (1)
- Wound CareDocument17 pagesWound Caredlneisha6183% (6)
- Glasgow Coma ScaleDocument2 pagesGlasgow Coma Scalejean thereseNo ratings yet
- Respiratory AssessmentDocument38 pagesRespiratory AssessmentNisha MwlzNo ratings yet
- Cardiovascular Assessment ChecklistDocument2 pagesCardiovascular Assessment Checklistvishnu100% (3)
- Assessment and Management of Patients With Hearing and Balance Disorders WebDocument36 pagesAssessment and Management of Patients With Hearing and Balance Disorders WebStephKirstin Velasco Malapit100% (2)
- Case Study HypertensionDocument7 pagesCase Study Hypertensionsanthyakunjumon67% (3)
- Surgical Pediatric Prenatal Care Psychiatric Patient CareDocument17 pagesSurgical Pediatric Prenatal Care Psychiatric Patient CareJireh Mae Cordero67% (3)
- Cardiac ComplicationDocument12 pagesCardiac ComplicationResa ShotsNo ratings yet
- GI Health AssessmentDocument45 pagesGI Health Assessmentفاتن أشتيويNo ratings yet
- Physical AssessmentDocument3 pagesPhysical AssessmentHyacinth ExmundoNo ratings yet
- Benner's Stages of Nursing: WHO IS Patricia Benner? Major ConceptDocument2 pagesBenner's Stages of Nursing: WHO IS Patricia Benner? Major ConceptRhuaine ReyesNo ratings yet
- Nursing Management of Congestive Heart FailureDocument37 pagesNursing Management of Congestive Heart FailurePierre Aseron ManuelNo ratings yet
- Focus ChartingDocument5 pagesFocus ChartingJeselo Ouano GormeNo ratings yet
- CARDIAC ASSESSMENT CHECKLISTDocument7 pagesCARDIAC ASSESSMENT CHECKLISTElle ChasenNo ratings yet
- 2) Vital SignsDocument7 pages2) Vital SignsJudy JalbunaNo ratings yet
- Medical Surgical Nursing - RespiratoryDocument15 pagesMedical Surgical Nursing - RespiratoryChristian Esteves75% (4)
- PneumoniaDocument71 pagesPneumoniafrancis00090100% (1)
- Ortho Nursing NotesDocument6 pagesOrtho Nursing NotesRAYANA UBASNo ratings yet
- COPD - Chronic Obstructive Pulmonary DiseaseDocument30 pagesCOPD - Chronic Obstructive Pulmonary DiseaseAmila SirisingheNo ratings yet
- PericarditisDocument45 pagesPericarditisBrenda WardshoneNo ratings yet
- Cesarean Section PDFDocument9 pagesCesarean Section PDFIeien MuthmainnahNo ratings yet
- Congenital Heart Disease NursingDocument21 pagesCongenital Heart Disease NursingAshiqAhleBaytNo ratings yet
- Nursing DiagnosisDocument86 pagesNursing DiagnosisMarianne Gonzales100% (5)
- Assessing the Abdomen DemoDocument6 pagesAssessing the Abdomen DemoMay Chelle ErazoNo ratings yet
- Nursing Care Plan WordDocument115 pagesNursing Care Plan WordKi C PungitNo ratings yet
- Concept MapDocument1 pageConcept MapSheryl Ann Barit PedinesNo ratings yet
- Taking Blood Pressure CorrectlyDocument7 pagesTaking Blood Pressure CorrectlySamue100% (1)
- Rheumatic Heart DiseaseDocument22 pagesRheumatic Heart DiseasemajdNo ratings yet
- Respiratory Exam GuideDocument18 pagesRespiratory Exam GuideIbi Yulia Setyani100% (1)
- Nursing Process: A Critical Thinking ToolDocument15 pagesNursing Process: A Critical Thinking Toolsushma shresthaNo ratings yet
- Carla Hernandez Clinical WorksheetDocument2 pagesCarla Hernandez Clinical WorksheetJasmyn RoseNo ratings yet
- Procedure ON Bladder Irrigation: SUBMITTED TO: Mr. EKE Lama TamangDocument17 pagesProcedure ON Bladder Irrigation: SUBMITTED TO: Mr. EKE Lama TamangRajaNo ratings yet
- Proper Nursing Documentation WillDocument4 pagesProper Nursing Documentation Willbel_dawn019No ratings yet
- Complete Physical Examination Eyes, Ears, Nose, ThroatDocument103 pagesComplete Physical Examination Eyes, Ears, Nose, Throatjennylyn guadalupe100% (3)
- Nursing Care Plans CVADocument14 pagesNursing Care Plans CVAJaye DangoNo ratings yet
- Nursing DiagnosisDocument14 pagesNursing Diagnosissunny kent100% (1)
- Nursing Case Study Ch46 Med SurgDocument1 pageNursing Case Study Ch46 Med SurgPriyal ParikhNo ratings yet
- Assessment of The Peripheral Vascular SystemDocument17 pagesAssessment of The Peripheral Vascular SystemgrailbadNo ratings yet
- Health Assessment: Nursing ProcessDocument7 pagesHealth Assessment: Nursing ProcessAngelrica TumbadoNo ratings yet
- Lessonplan FinDocument14 pagesLessonplan Finx483xDNo ratings yet
- Asthma Care PlanDocument2 pagesAsthma Care Planwongfany100% (2)
- Assessment of The Peripheral Vascular SystemDocument11 pagesAssessment of The Peripheral Vascular SystemGVHHNo ratings yet
- Appendix C: Tables, Conversions and AbbreviationsDocument2 pagesAppendix C: Tables, Conversions and AbbreviationsBrian FoongNo ratings yet
- Acute Otitis MediaDocument16 pagesAcute Otitis Mediaadrianne18sNo ratings yet
- MEDUMAT Standard 2 83700-ENDocument16 pagesMEDUMAT Standard 2 83700-ENJagath PrasangaNo ratings yet
- DrugStudyFormatDocument2 pagesDrugStudyFormatSheryl Ann Barit PedinesNo ratings yet
- Endocrine Society Hypercalcemia MalignancyDocument22 pagesEndocrine Society Hypercalcemia MalignancyJoão Pedro RibasNo ratings yet
- COE WorksheetDocument16 pagesCOE WorksheetiloveraynaNo ratings yet
- BaytexDocument7 pagesBaytexArvind AkkNo ratings yet
- Dim Mak and Acupuncture: Understanding the Medical Reasons Behind this Martial ArtDocument6 pagesDim Mak and Acupuncture: Understanding the Medical Reasons Behind this Martial ArtIoan NeacsuNo ratings yet
- Oxidative Stress in Aging HairDocument9 pagesOxidative Stress in Aging HairRoxana GuillénNo ratings yet
- Practice Guidelines For The Diagnosis and Management of Aspergilosis 2016 Update by AmericaDocument60 pagesPractice Guidelines For The Diagnosis and Management of Aspergilosis 2016 Update by AmericaNur Prasetyo Nugroho100% (1)
- Konversi Kode Prosedure INACBGs Ke Kode ICD 9-CMDocument349 pagesKonversi Kode Prosedure INACBGs Ke Kode ICD 9-CMTri Muhammad HaniNo ratings yet
- 04.retrievable Metal Ceramic Implant-Supported Fixed ProsthesesDocument9 pages04.retrievable Metal Ceramic Implant-Supported Fixed Prostheses친절No ratings yet
- Leptin HormoneDocument21 pagesLeptin Hormonemarah almahameed100% (2)
- Susan M. Pollak, Thomas Pedulla, Ronald D. Siegel - Sitting Together - Essential Skills For Mindfulness-Based Psychotherapy-The Guilford Press (2014)Document258 pagesSusan M. Pollak, Thomas Pedulla, Ronald D. Siegel - Sitting Together - Essential Skills For Mindfulness-Based Psychotherapy-The Guilford Press (2014)duasherazi55No ratings yet
- Baby Massage Consultation Form - November 2017Document1 pageBaby Massage Consultation Form - November 2017api-257327106No ratings yet
- PracticeWise Blue Menu of Evidence-Based InterventionsDocument5 pagesPracticeWise Blue Menu of Evidence-Based InterventionsLem BoneteNo ratings yet
- Emily Morgan - ResumeDocument2 pagesEmily Morgan - Resumeapi-283578734No ratings yet
- Hicks ITC Goa Monthly Report Highlights ABC Surgeries, Rabies ResponseDocument16 pagesHicks ITC Goa Monthly Report Highlights ABC Surgeries, Rabies ResponseAkshay JainNo ratings yet
- AutocoidsDocument26 pagesAutocoidsA.R. ChowdhuryNo ratings yet
- Wound AssessmentDocument19 pagesWound Assessmentdrsonuchawla100% (1)
- Presented By: Bhawna Joshi Msc. Nursing 1 YearDocument52 pagesPresented By: Bhawna Joshi Msc. Nursing 1 YearBhawna JoshiNo ratings yet
- Medium Opening Activator: (Removable Functional Appliance)Document22 pagesMedium Opening Activator: (Removable Functional Appliance)Abiha AliNo ratings yet
- Nurs 205 Concept MapDocument1 pageNurs 205 Concept MapJami SpearsNo ratings yet
- 13 Implant Supported Fixed ProsthesesDocument52 pages13 Implant Supported Fixed ProsthesesJúliaJulieNo ratings yet
- Zurita (2020) The ACT Workbook For Teens With OCDDocument274 pagesZurita (2020) The ACT Workbook For Teens With OCDCecilia Romero100% (2)
- Dr. RKM ProfileDocument1 pageDr. RKM Profilevmeharia123No ratings yet
- Rotator CuffDocument46 pagesRotator Cuffeuan00No ratings yet
- Current Status of NTD PhilippinesDocument28 pagesCurrent Status of NTD PhilippinesMelody PardilloNo ratings yet
- Gram08 28Document21 pagesGram08 28Hendra Wana Nur'aminNo ratings yet
- Gout and Hyperuricemia: PathophysiologyDocument1 pageGout and Hyperuricemia: Pathophysiologyسمرة طايبNo ratings yet
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (13)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 3.5 out of 5 stars3.5/5 (2)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (402)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (78)
- Techniques Exercises And Tricks For Memory ImprovementFrom EverandTechniques Exercises And Tricks For Memory ImprovementRating: 4.5 out of 5 stars4.5/5 (40)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 5 out of 5 stars5/5 (4)
- Chakras and Yoga: Finding Inner Harmony Through Practice, Awaken the Energy Centers for Optimal Physical and Spiritual Health.From EverandChakras and Yoga: Finding Inner Harmony Through Practice, Awaken the Energy Centers for Optimal Physical and Spiritual Health.Rating: 4 out of 5 stars4/5 (2)
- The Ultimate Guide To Memory Improvement TechniquesFrom EverandThe Ultimate Guide To Memory Improvement TechniquesRating: 5 out of 5 stars5/5 (34)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (41)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (327)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 5 out of 5 stars5/5 (4)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Seeing What Others Don't: The Remarkable Ways We Gain InsightsFrom EverandSeeing What Others Don't: The Remarkable Ways We Gain InsightsRating: 4 out of 5 stars4/5 (288)
- The Happiness Trap: How to Stop Struggling and Start LivingFrom EverandThe Happiness Trap: How to Stop Struggling and Start LivingRating: 4 out of 5 stars4/5 (1)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsFrom EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsNo ratings yet
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 3.5 out of 5 stars3.5/5 (33)
- Troubled: A Memoir of Foster Care, Family, and Social ClassFrom EverandTroubled: A Memoir of Foster Care, Family, and Social ClassRating: 4.5 out of 5 stars4.5/5 (23)