Professional Documents
Culture Documents
Amblyopia - Diagnosis and Treatment: Pamela J. Kutschke, BS, Co
Uploaded by
Khushbu DedhiaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Amblyopia - Diagnosis and Treatment: Pamela J. Kutschke, BS, Co
Uploaded by
Khushbu DedhiaCopyright:
Available Formats
AmblyopiaDiagnosis and Treatment
Pamela J. Kutschke, bs, co
The term amblyopia is derived from the Greek, meaning dull vision.
Many parents or patients will refer to it as lazy eye. As a patient examiner, you will want to investigate the meaning of this term carefully, as many patients also use lazy eye to describe strabismus. Amblyopia occurs in approximately 25% of the general population. The visual system develops between birth and approximately age 7 to 9. The earlier the onset of the abnormal visual stimulation, the greater the visual deficit will be. Early detection is vital. Visual acuity increase secondary to treatment can occur only until around age 9. If treatment does not occur during this time, vision and binocularity are permanently lost. pamela J. kutschke, BS, CO Chief Orthoptist University of Iowa Hospitals and Clinics Pediatric Ocular Services Department of Ophthalmology & Visual Sciences 200 Hawkins Drive Iowa City, IA 52242 319.356.2859 Pamela-Kutschke@uiowa.edu The general term amblyopia refers to a decrease in vision due to abnormal visual stimulation of either one or both eyes. Both eyes must see the image simultaneously and in focus to work together. If, for some reason, one image is blurry and the other clear (refractive) or the eyes do not see the same object simultaneously (strabismic), amblyopia can develop. The three most common causes of amblyopia are: Strabismus Refraction Deprivation Combination of the above Strabismic amblyopia This type of amblyopia is often noted early due to a misalignment of the eyes, or strabismus. During strabismus, one eye is straight and being used for vision. The other eye is most often seen as turning in (esotropia) or turning out (exotropia), although the misalignment can be vertical as well. The deviation of the eyes creates two images of one object, one where each eye is focusing. When this occurs in children, the brain automatically turns off the second image (suppression) because two images cannot be focused at the same time. When strabismus occurs in older patients whose brain is no longer adaptable, two images will be seen at the same time but in two different places, resulting in diplopia. Many young patients freely alternate between the two eyes to fixate and develop equal vision. If they strongly favor one eye over the other and do not alternate fixation, amblyopia results. Strabismic amblyopia is always unilateral and occurs more frequently in esotropes than exotropes.
Refractive Amblyopia
This type of amblyopia is often noted much later in a childs development. There are no outward clues to forewarn parents of a visual problem. Many children are first noted to have decreased vision at school screenings. However, they will often cheat in a desire to give the correct answer. Screeners cannot always catch children who may be peeking with the better-seeing eye. Unlike strabismic amblyopia, refractive amblyopia can be unilateral or bilateral. The clearer image is always the preferred image. Bilaterally, amblyopia occurs with high myopia or hypermetropia as ammetropic amblyopia. A clear image is not seen by either eye. Uncorrected high myopia may be too high to create a clear image at any distance. Moderate myopia may create an image
20
I n s I g h t The Journal of the American Society of Ophthalmic Registered Nurses, Inc. |
AprilJune 2009
| Vol. XXXIV, No. 2
Continuing Nursing Education (CNE) Article
seen at near that may be clearer but not clear enough. However, uncorrected moderate or high hypermetropia will cause a great need to accommodate to produce a clear image. The image at near will actually require more accommodation to be seen. Most young children just wont make the effort to accommodate the amount necessary. In these cases, a clear image never reaches either eye and proper visual development cannot occur. Uncorrected high astigmatism will also create a blurred image. This type of amblyopia, where the image is blurred along one axis, is called meridional amblyopia. Depending on the uncorrected refractive error, ammetropic amblyopia may be mixed with meridional amblyopia. A significant refractive difference between the two eyes will cause anisometropic amblyopia. Anisohypermetropic amblyopia is more common than anisomyopic amblyopia. In anisohypermetropia, the least hypermetropic eye is the preferred eye, as less accommodation is needed to focus on an object. With anisomyopia, the more myopic eye is used for near and the other is used for distance. Although guidelines vary, it has been said that as little as one diopter of anisohypermetropia, 1.5D of astigmatism, or 3D of myopia can cause anisometropic amblyopia. It is important to remember that when correcting amblyopia, the image from the two eyes must be clear and the same. Spectacles to correct high refractive errors may be expensive, difficult to fit, and difficult to obtain. Anisometropic spectacles may cause aniseikonia, a difference in the retinal image size, providing another obstacle for amblyopia treatment. All types of optical correction should be considered. The progress of contact lens availability for children has provided an excellent treatment option. Contact lenses offer parents many advantages. They do not create aniseikonia, they cannot be broken, and they can be dispensed with a greater fit.
necessary to create as clear an image as possible. Parents should be aware that they will be making frequent visits, as contact lens power will need to be changed frequently, amblyopia treatment will be necessary, and further surgery may be necessary to correct secondary glaucoma or an opacified lens capsule.
Diagnosis
Amblyopia is diagnosed during normal visual acuity testing. As usual, the test must reflect the patients ability. Picture tests, such as Allen or LEA, can usually be used about age 3, either naming or matching. The next sets of more difficult tests are the preliterate E test or the HOTV. Once the child knows all of the letters, Snellen letters can be tested. The tests correlate in reliability with the difficulty. The last test is equal to adult testing, as long as effort is good. A difference of two lines of visual acuity is diagnostic of amblyopia. The vision in the amblyopic eye should be tested first. Studies have proven that a child with amblyopia will exhibit an improved visual acuity when shown isolated letters. This is called the crowding phenomenon since isolated letter visual acuity will be better than linear letter acuity. An inaccurate visual acuity measurement may miss identification of a child with amblyopia. Also, an examiner may be misled into believing better vision has been achieved in a patient who has been patched for amblyopia if a linear test is used on the first visit and isolated symbols on the second. Visual acuity should always be measured with an entire line of characters to limit the crowding phenomenon. With children too young for these quantitative tests, there are still ways to diagnose amblyopia. The least complicated test is to observe whether the child prefers to fixate with one eye over the other. This is determined by occluding one eye and observing the childs response. If the child cannot see well with one eye, they will push the occluder away or try to look around it. A more complicated test also observes fixation, but more formally. With strabismic patients, the practitioner observes which eye the child is fixating with. Obviously, this eye sees well. Then the examiner should cover the fixing eye and observe whether the child will fixate as well with the other eye. If there is a definite preference for one eye over the other, amblyopia is present. What if the child does not have strabismus? Can an examiner still assess fixation? Yes, but a strabismus must be created. A 16 prism is placed either base down or base in over one eye to create a second image. If the child picks up fixation through the prism, the patient can see well with this eye. Often the examiner will have to occlude the eye without the prism to force the eye to pick up fixation. The same procedure is performed with the prism covering the other eye. Amblyopia is present if one eye shows a preference over the other. The fixation tests are based on the premise that if vision is equal, the child will not care which eye he/she uses to see.
Visual Deprivation Amblyopia
To provide for a clear retinal image for both eyes, the visual pathway must be clear of obstacles. Conditions such as acquired or congenital cataracts, ptosis, or corneal opacities may cause unilateral or bilateral amblyopia. Many of these conditions involve the ocular refracting surfaces and may cause additional amblyopia due to anisometropia. With ptosis, for example, the eyelid may sit directly on the cornea, often causing astigmatism. Refractive errors should be corrected before amblyopia treatment takes place. Congenital cataracts create a much greater problem. These patients should be seen the same day as it is first detected, if possible. Treatment is performed early to create as clear an image as possible. With binocular cataracts, neither eye is seeing clearly and therefore there is no preference. With monocular cataract, it is important to remove the cataract as quickly as possible to create a clear image with each eye. Once the cataract(s) is (are) removed, refractive correction in the form of contact lenses is
21
I n s I g h t The Journal of the American Society of Ophthalmic Registered Nurses, Inc. |
AprilJune 2009
| Vol. XXXIV, No. 2
Continuing Nursing Education (CNE) Article
AMBLYOPIADIAGNOSIS AND TRE ATMENT
Continued from page 21
A more complicated test is the forced preferential looking test, commonly known as the Teller Cards. This test was experimental for a long time. Currently, many clinics are using it as a routine screening test in newborns and very young babies. The test consists of a series of cards with a homogeneous gray background and a pattern stimulus on one end. (See Figure 1.) The cards are held at a given distance from the subject and the examiner (who cannot see which side of the card is the patterned side) observes the direction the baby looks and records this. A young baby will look toward a pattern stimulus rather than a homogenous gray stimulus if they can see it. The line pattern stimuli are presented in decreasing thickness until there is no longer any preference for pattern vs. gray. At this stage, it is assumed that the baby can no longer perceive the patterned stimulus, and the level can be converted to a measurement of visual acuity. When a child begins to become distracted by background objects, noises, etc., they are really becoming too old to perform the test. There are some problems with this test. Although there is a chart to correlate Teller acuity to Snellen acuity, the tests cannot truly be compared, as they are different types of tests. A difference of two cards between the eyes is considered diagnostic of amblyopia. Studies have shown, however, that this test does not test well for amblyopia because it relies on resolution, not recognition.
example of a teller Card
Figur E 1
If the child will not wear the adhesive patch, many things can be tried. Convincing the parents by stressing the importance of occlusion therapy often is enough. Bribery works too. A special toy or additional video time may work with older children. Decorating the patch with stickers or having a stuffed animal wear the patch too often works with younger children. Another option for occlusion is a specially developed cloth patch that is worn over the patients glasses. Pirate patches are not recommended due to the difficulty of keeping the patch in the correct place. Arm restraints can be worn for short periods as a behavior modification technique. As a last resort, occlusion contact lenses have been prescribed. The cost is usually prohibitive, however. Occlusion can take various forms, often dependent on the practitioners preference. Full-time occlusion refers to 24 hours or all waking hours of occlusion. Part-time occlusion refers to any occlusion less than full time. Factors determining the duration of treatment include the age of the child, the density of amblyopia, the cooperation of the child and parents with patching and follow-up. The rule for follow-up with full-time occlusion is 1 week per year age of the child, up to four weeks. Anyone over the age of four is followed after 4 weeks. Full-time occlusion versus parttime occlusion has been investigated in great detail lately with a series of studies done by the Pediatric Eye Disease Investigation Group. Although the results appear equal with full-time and part-time occlusion, it is agreed that full-time occlusion shows positive results more rapidly, thus decreasing treatment time. Some have argued that they get better compliance with parttime occlusion, others with full-time occlusion. One of the difficulties with full-time occlusion is the possible development of occlusion amblyopia, where the patient prefers the previously amblyopic eye. Studies have shown this to be easily reversible in almost all cases. Although its occurrence is
Treatment
Occlusion therapy to treat amblyopia has been successfully used since 1743. Whatever t \he cause(s), the treatment of amblyopia is based on the same principle: make the amblyopic eye work and vision will increase. The goal is to acquire the best vision that can be obtained. The ultimate goal is to acquire equal vision in the two eyes. Prior to occlusion therapy, the patient needs to be wearing their full optical correction. Total occlusion obscures both light and form vision. Parents should be counseled about all complications prior to beginning any therapy. To occlude, an adhesive patch, similar to a Band-Aid, is worn directly over the preferred eye. Although latex free, patches may cause irritation to the skin, especially when removed. Prior to occlusion, a small notch can be cut in the patch so that it does not stick to the irritated area. Another trick is to apply milk of magnesia over the area where the adhesive will be. Once it dries, apply the patch. This provides a barrier between the skin and the patch that should help with removal. Other removal techniques include using a warm, wet cloth or using Vaseline or baby oil over the adhesive portions of the patch to decrease the stickiness.
22
I n s I g h t The Journal of the American Society of Ophthalmic Registered Nurses, Inc. |
AprilJune 2009
| Vol. XXXIV, No. 2
Continuing Nursing Education (CNE) Article
disturbing to the parents, it is better if they are informed of the possibility before starting occlusion. To practitioners, occlusion amblyopia can be a good sign, as it indicates good results with occlusion therapy. To treat occlusion amblyopia may require only a cessation of all patching or brief occlusion of the previously amblyopic eye. Another risk of occlusion therapy is the appearance of an esodeviation where no deviation had been seen prior to patching. The deviation does not always correct itself and strabismus surgery may be required to correct the deviation. Part-time occlusion has its advantages as well. Follow-up visits are needed less frequently and can take place over a longer interval. There is also less risk of occlusion amblyopia. Parttime occlusion is much more flexible to the patients lifestyle. Occlusion can take place at a time of day of the parents choosing, for example, after school or on weekends. Some parents prefer daycare or school time, as children sometimes listen to others better than they do to their parents. Occlusion can also be split between the two eyes, such as 3 days to one eye and 1 day to the other. Penalization is a form of amblyopia treatment that does not require occlusion. There are three forms: optical, pharmacological, or a combination of the two. Optical penalization involves the placement of fogging material or changing the spectacle correction over the non-amblyopic eye. Types of fogging materials include clear nail polish or frosted tape. Changing the spectacle or contact lens correction to create a blurred image is accomplished by overplussing the patient until the vision of the preferred eye is blurred below the level of the amblyopic eye. This will create a blurred image at distance but the patient may still prefer the non-amblyopic eye at near. Pharmacological penalization uses instillation of atropine 1% into the fornix of the preferred eye to prevent accommodation. This will blur the preferred eye for near work. Atropine will only limit the vision in the preferred eye to 20/80, however. If the vision of the amblyopic eye is worse than this, the patient will continue to fix with the non-amblyopic eye. Atropine has several side effects that parents should know about prior to starting penalization. Atropine is very toxic. An ordinary ophthalmic bottle contains enough medication to kill several children. Parents should be advised to keep the bottle out of reach. If the drop is mistakenly taken orally, poison control must be contacted immediately. Other side effects include increased intraocular pressure, reduced tear secretion, conjunctival hyperemia, dryness of the mouth, irritability, tachycardia, flushing of the face, and photophobia.
The cycloplegic effects of atropine may last up to 48 hours. The dilatory effects may last up to two weeks. Parents should be advised that if both eyes are dilated, theyve accidentally put the drop into both eyes. Also, just because the pupil is dilated, the desired effect of the drug, blurred vision of the preferred eye, may not be occurring. The scheduled use of atropine can vary from once daily to once weekly, at the discretion of the practitioner. To penalize the patient at near and distance, optical and pharmacological penalization must be used simultaneously. Total penalization involves atropinization and underplussing (or using minus lenses if not hyperopic) of the preferred eye. The effect will be the inability to accommodate and a blurred image for distance at near and distance. The amblyopic eye should be fully optically corrected. As this type of penalization involves obtaining a new pair of spectacles, it is usually reserved for dense amblyopia. The advantages of penalization over occlusion are that there is almost no chance of occlusion amblyopia, secondary esotropia may be better tolerated, and there is no aggravation of latent nystagmus. All types of amblyopia require full refractive correction prior to amblyopia treatment. Anisometropic patients should have a trial of wearing their optical correction first to determine if occlusion therapy will be needed. Deprivation amblyopia may need correction of the ocular defect prior to undergoing amblyopia therapy. It is a complicated decision based on each particular case. All strabismic patients will require some sort of amblyopia treatment. It is common for more than one causative factor for amblyopia to be present. Every patient is different. No matter what type of amblyopia therapy, it should have an endpoint. The ultimate endpoint is equal vision. If that is not obtainable, three months of occlusion with no improvement should be considered the endpoint. Amblyopia can be easily diagnosed with existing early screening methods. It just needs to be done. The medical cost of diagnosis and treatment is miniscule for the benefit produced. Vision is one of the primary senses. Loss of vision results in a permanent disability recognized not only by eye professionals but by all government agencies as well. Diagnosis and treatment of amblyopia should be everyones goal. Once lost, it is too quickly too late to get it back.
Bibliography
Amblyopia. In: Core Curriculum for Ophthalmic Nursing, Chapter 20: 620623. Ledford, J. K. (Ed.) 2001. Handbook of clinical ophthalmology for the eye care professional. Thorofare, NJ: SLACK Inc.
23
I n s I g h t The Journal of the American Society of Ophthalmic Registered Nurses, Inc. |
AprilJune 2009
| Vol. XXXIV, No. 2
Continuing Nursing Education (CNE) Test
Please note! In anticipation of updating to an online education system before the end of 2009, please note that this will be the final test to be included in an issue of Insight. Future tests will be accessed online and more information will be available in coming months. Until further notice, please continue to submit tests as requested below.
This activity is provided by ASORN, which is accredited as a provider of continuing nursing education by the American Nurses Credentialing Centers Commission on Accreditation. ASORN is a provider approved by the California Board of Registered Nursing, provider number 11901. This activity has been submitted to JCAHPO for consideration of CE Credit. JCAHPO CECs, if and when approved, will be posted on the ASORN Web site in the online education section.* For this activity, read the article, submit the completed post-test and general evaluation form by June 30, 2010, and achieve a passing rate of 80% or higher on the post-test. Non-members, send your post-test with payment of $20 (free for members/ affiliates through June 30, 2010). This post-test expires on June 30, 2010.
asOrn Dept 34095 PO Box 39000 San Francisco, CA 94139 Fax: 415.561.8531
AmblyopiaDiagnosis and Treatment
Objectives
CNE TE S T
After completing this independent study activity, the participant should be able to: Define amblyopia Describe testing utilized in diagnosing amblyopia Discuss treatment strategies used to reverse the condition please allow a minimum of three weeks from date of receipt of post-test to receive your attendance verification certificate. requests for certificate less than three weeks from date of receipt should be accompanied by an additional $10 fee.
Registration Information and Evaluation Response Form
Name Address City Work Phone RN# I request: Payment: 1.0 Nursing contact hour Check Visa JCAHPO CEC* Mastercard CC# Exp State Home Phone State of Licensure Zip Fax Exp. Date
Test response: Circle the most appropriate response matching test question number and response number. 1. A 2. A B B C C D D 3. A 4. A B B C C D D 5. A 6. A B B C C D D 7. A 8. A B B C C D D 9. A 10. A B B C C D D
General Evaluation: Please use the scale below to evaluate this educational activity and objectives. Circle your response. As a result of completing this offering, I am able to:
Very well moderately well Fairly well not at all
1. 2. 3. 4. 5. 6. 7.
Define amblyopia. Describe testing utilized in diagnosing amblyopia. Discuss treatment strategies used to reverse the condition. the content matches the objectives. Independent study was an effective teaching method. this course helped me achieve personal objectives. the time required to complete this offering (in minutes) and take the test was:
4 4 4 4 4 4 60
3 3 3 3 3 3 75
2 2 2 2 2 2 90
1 1 1 1 1 1 >90
24
I n s I g h t The Journal of the American Society of Ophthalmic Registered Nurses, Inc. |
AprilJune 2009
| Vol. XXXIV, No. 2
Continuing Nursing Education (CNE) Test
AmblyopiaDiagnosis and Treatment
1. Amblyopia occurs in approximately what percent of the general population? A. 1015% B. 25% C. 510% D. 12% 2. Common causes of amblyopia include all of the following except A. Strabismus B. Deprivation C. Refraction D. Injury 3. Amblyopia due to high, uncorrected astigmatism is called A. Meridional B. Against the rule C. Axis D. Oblique 4. Which of the following conditions may cause amblyopia? A. Cataracts B. Ptosis C. Corneal opacities D. All of the above 5. The definitive therapy in treating amblyopia is called A. Seclusion B. Reduction C. Occlusion D. None of the above 6. Occlusion therapy for amblyopia has been successfully used since A. 1743 B. 1847 C. 1950 D. 1929 7. Total occlusion obscures A. Light B. Form vision C. Light and form vision D. Light and acuity below 20/200 8. The rule for follow-up when using full-time occlusion is A. 1 week per year age of the child up to 4 weeks B. 2 weeks per year age of the child up to 8 weeks C. 1 week per year age of the child up to 6 weeks D. Every 2 weeks regardless of age 9. Side effects of atropine penalization include all except A. Reduced intraocular pressure B. Dry mouth C. Photophobia D. Tachycardia 10. Visual acuity in children should always be tested with an entire line of letters to avoid what? A. Myopic shift B. Crowding phenomenon C. Confusion D. Distortion
CNE P O S T-TE S T
25
You might also like
- Clinical Orthoptics - Fiona Rowe - 146Document6 pagesClinical Orthoptics - Fiona Rowe - 146Danielle SangalangNo ratings yet
- Wills Eye ManualDocument2 pagesWills Eye ManualKeyko Lampita33% (3)
- Dry EyeDocument126 pagesDry EyeAnonymous PYgnwOWK100% (4)
- Vision Loss (Blindness), A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandVision Loss (Blindness), A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Far-Sightedness, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandFar-Sightedness, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Restless Legs Syndrome Clinical Features, Diagnosis and A Practical Approach To Management BMJ 2017Document10 pagesRestless Legs Syndrome Clinical Features, Diagnosis and A Practical Approach To Management BMJ 2017Alex Del PieroNo ratings yet
- Color Atlas of Forensic Pathology Ebook Een PDFDocument2 pagesColor Atlas of Forensic Pathology Ebook Een PDFJavierNo ratings yet
- Neurofibromatosis 1, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandNeurofibromatosis 1, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Simplifying Strabismus: A Practical Approach to Diagnosis and ManagementFrom EverandSimplifying Strabismus: A Practical Approach to Diagnosis and ManagementNo ratings yet
- Optometric Vision Therapy Fact Sheets and Reimbursement GuideDocument30 pagesOptometric Vision Therapy Fact Sheets and Reimbursement Guidebiotech_vidhyaNo ratings yet
- Child Abuse and Neglect Advancements in the 21st CenturyDocument122 pagesChild Abuse and Neglect Advancements in the 21st CenturyDina HottestwopiemNo ratings yet
- Retinitis Pigmentosa, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandRetinitis Pigmentosa, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Care of The Patient With Accommodative and Vergence DisfunctionDocument6 pagesCare of The Patient With Accommodative and Vergence DisfunctionJosepMolinsReixachNo ratings yet
- 2008 - Irregular - Astigmatism - Diagnosis - (Ming - Wang - MD) - PDFDocument606 pages2008 - Irregular - Astigmatism - Diagnosis - (Ming - Wang - MD) - PDFRuslan IshalNo ratings yet
- Fragile X Syndrome and Premutation Disorders: New Developments and TreatmentsFrom EverandFragile X Syndrome and Premutation Disorders: New Developments and TreatmentsRandi J HagermanNo ratings yet
- Refractive Surgery (HJ) UpdatedDocument47 pagesRefractive Surgery (HJ) UpdatedSayoki ghosg100% (1)
- Coma, (Unconsciousness) A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandComa, (Unconsciousness) A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- Mom’s Losing Her Memory I’m Losing My Mind!: Taking Care of Mom and Dad with Memory DeclineFrom EverandMom’s Losing Her Memory I’m Losing My Mind!: Taking Care of Mom and Dad with Memory DeclineNo ratings yet
- Skin Infections, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandSkin Infections, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Cafe-Au-Lait Spots, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandCafe-Au-Lait Spots, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Child Sexual Exploitation Quick Reference: For Healthcare, Social Service, and Law Enforcement ProfessionalsFrom EverandChild Sexual Exploitation Quick Reference: For Healthcare, Social Service, and Law Enforcement ProfessionalsNo ratings yet
- Memoirs of a Surgeon's Wife: I’m Throwing Your Damn Pager Into the OceanFrom EverandMemoirs of a Surgeon's Wife: I’m Throwing Your Damn Pager Into the OceanNo ratings yet
- Tracing Your Prisoner Ancestors: A Guide for Family HistoriansFrom EverandTracing Your Prisoner Ancestors: A Guide for Family HistoriansNo ratings yet
- The Slim Book of Health Pearls: Symptoms Never to IgnoreFrom EverandThe Slim Book of Health Pearls: Symptoms Never to IgnoreNo ratings yet
- NVLD BrochureDocument2 pagesNVLD Brochureapi-543728028No ratings yet
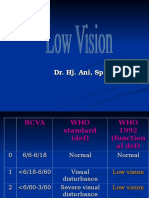
- Low VisionDocument36 pagesLow VisionIqbal HabibieNo ratings yet
- Cell Biology of the EyeFrom EverandCell Biology of the EyeDavid McdevittNo ratings yet
- External Disease and CorneaDocument105 pagesExternal Disease and CorneaNova CiNg CiNgNo ratings yet
- Measurement of Angle KappaDocument5 pagesMeasurement of Angle Kappapason1988100% (1)
- The Neural Basis of Romantic LoveDocument6 pagesThe Neural Basis of Romantic LoveBooster CNo ratings yet
- Glaucoma 2019Document130 pagesGlaucoma 2019Jennifer Conrad100% (1)
- Classification and Causes of Age-related CataractDocument16 pagesClassification and Causes of Age-related CataracttataNo ratings yet
- Child Maltreatment Assessment-Volume 1: Physical Signs of AbuseFrom EverandChild Maltreatment Assessment-Volume 1: Physical Signs of AbuseNo ratings yet
- Congenital Strabismus: S. Vanitha, B.optom, 3 YearDocument23 pagesCongenital Strabismus: S. Vanitha, B.optom, 3 YearDivya Priya Dharmalingam100% (1)
- The Retinal Muller Cell PDFDocument293 pagesThe Retinal Muller Cell PDFkemalasari8818No ratings yet
- Clinical Study On Scleral Lenses by Dr. Elise KramerDocument8 pagesClinical Study On Scleral Lenses by Dr. Elise KramerMiami Contact Lens InstituteNo ratings yet
- Angle Closure Glaucoma PDFDocument289 pagesAngle Closure Glaucoma PDFsisil muntheNo ratings yet
- The Wonderful World of Trivia: Ghosts,Vampires and Monsters TriviaFrom EverandThe Wonderful World of Trivia: Ghosts,Vampires and Monsters TriviaNo ratings yet
- Boomerang Nation: How to Survive Living with Your Parents...the Second Time AroundFrom EverandBoomerang Nation: How to Survive Living with Your Parents...the Second Time AroundNo ratings yet
- Pupil-Tutorial-1 09 14Document41 pagesPupil-Tutorial-1 09 14Jehangir Khan100% (1)
- Binocular Eye Movements GuideDocument36 pagesBinocular Eye Movements Guideblack00swanNo ratings yet
- Notes: GlaucomaDocument175 pagesNotes: GlaucomasasaNo ratings yet
- Binocular Eye MovementsDocument3 pagesBinocular Eye Movementsblack00swanNo ratings yet
- How To Go Blind and Not Lose Your Mind: Physical and Emotional Challenges of Sight LossFrom EverandHow To Go Blind and Not Lose Your Mind: Physical and Emotional Challenges of Sight LossNo ratings yet
- The Retina A Model for Cell Biology Studies Part_1From EverandThe Retina A Model for Cell Biology Studies Part_1Ruben AdlerNo ratings yet
- 1st-Ocular Pharmacology and Toxicology - M.sc1styrDocument58 pages1st-Ocular Pharmacology and Toxicology - M.sc1styrKhushbu DedhiaNo ratings yet
- PaperDocument7 pagesPaperKhushbu DedhiaNo ratings yet
- CorneaDocument73 pagesCorneaKhushbu DedhiaNo ratings yet
- KerasoftDocument8 pagesKerasoftKhushbu DedhiaNo ratings yet
- 2.4.2.a Visualperception 4Document5 pages2.4.2.a Visualperception 4Andy LinNo ratings yet
- Color Blindness, OR Color Vision DeficienciesDocument11 pagesColor Blindness, OR Color Vision DeficienciesSalih AliNo ratings yet
- Melanocytoma of The Optic Nerve Head: Clinical Case - Photo EssayDocument5 pagesMelanocytoma of The Optic Nerve Head: Clinical Case - Photo EssayKaran KumarswamyNo ratings yet
- Call Center Zocalo Listas de Precios Primavera - Verano 22 01jun22Document6 pagesCall Center Zocalo Listas de Precios Primavera - Verano 22 01jun22RUTH ROJASNo ratings yet
- Lesson Plan For Science 3Document6 pagesLesson Plan For Science 3Dinah DimagibaNo ratings yet
- Kohler 1962Document12 pagesKohler 1962LauraSanchezNo ratings yet
- Neuro Optha Mariano 6Document6 pagesNeuro Optha Mariano 6Dey SibalNo ratings yet
- Ophthalmology - AnatomyDocument5 pagesOphthalmology - AnatomyOscar Daniel MendezNo ratings yet
- Northern Medical Colleges Cataract CaseDocument4 pagesNorthern Medical Colleges Cataract CaseSIJINo ratings yet
- Smartphone-based screening for diabetic retinopathy in IndiaDocument10 pagesSmartphone-based screening for diabetic retinopathy in IndiaVivi DeviyanaNo ratings yet
- OT - Grandjean - Ergonomics in Computerized Offices PDFDocument238 pagesOT - Grandjean - Ergonomics in Computerized Offices PDFAubrey Vale SagunNo ratings yet
- Acute Angle-Closure Glaucoma (AACG) Treatment & Management - Approach Considerations, Medical Care, Surgical CareDocument3 pagesAcute Angle-Closure Glaucoma (AACG) Treatment & Management - Approach Considerations, Medical Care, Surgical CarePuddingNo ratings yet
- HPE Color Palette Asset Overview 050415Document1 pageHPE Color Palette Asset Overview 050415Henderson and SantosNo ratings yet
- Visual System ReportDocument7 pagesVisual System ReportAndre DueñasNo ratings yet
- With the rule' astigmatism correction and causesDocument23 pagesWith the rule' astigmatism correction and causesAmr AbdulradiNo ratings yet
- 5.1 Detecting Environmental Conditions AnsDocument3 pages5.1 Detecting Environmental Conditions AnsBelladonna LeeNo ratings yet
- Seemarollno 141219034210 Conversion Gate01Document16 pagesSeemarollno 141219034210 Conversion Gate01jessajoy deslateNo ratings yet
- Common Refractive Errors and Their TreatmentDocument60 pagesCommon Refractive Errors and Their TreatmentSneha PrakashNo ratings yet
- 10th SCERT KeralaDocument72 pages10th SCERT KeralaArun KNo ratings yet
- IaDocument415 pagesIaDiego DiazNo ratings yet
- Physio Lab PBLDocument4 pagesPhysio Lab PBLtheodore_estradaNo ratings yet
- Full Text 02Document31 pagesFull Text 02ANIENo ratings yet
- HAFFMANDocument29 pagesHAFFMANRahul SoniNo ratings yet
- Conclusions Background: Vision Development & RehabilitationDocument13 pagesConclusions Background: Vision Development & RehabilitationDanielle SangalangNo ratings yet
- 1980 - Buchsbaum. A Spatial Processor Model For Object Colour PerceptionDocument26 pages1980 - Buchsbaum. A Spatial Processor Model For Object Colour PerceptionYann FleatwoodNo ratings yet
- Oct.27 B Science q1 Week 1Document14 pagesOct.27 B Science q1 Week 1hpmadkitaibNo ratings yet
- Igcse AccommodationDocument3 pagesIgcse AccommodationChr1zFX4No ratings yet
- Senile Cataract Clinical Presentation and CausesDocument4 pagesSenile Cataract Clinical Presentation and CausesAhmad FahroziNo ratings yet
- Selective Perimetry in Glaucoma Diagnosis: Lisandro M. Sakata, Julio Deleo N-Ortega and Christopher A. GirkinDocument7 pagesSelective Perimetry in Glaucoma Diagnosis: Lisandro M. Sakata, Julio Deleo N-Ortega and Christopher A. GirkinMacarena AlvarezNo ratings yet
- Chapter 22Document17 pagesChapter 22Jeferson Alexander Pabon RodriguezNo ratings yet