Professional Documents
Culture Documents
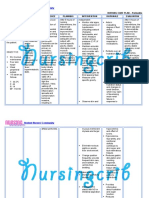
cASE STUDIES ANSWER
Uploaded by
Nur LiyanaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
cASE STUDIES ANSWER
Uploaded by
Nur LiyanaCopyright:
Available Formats
CLINICAL BIOCHEMISTRY
Answers to case studies
Chapter 1
Case study 1.1 (a) 0.027 (b) 0.999 (c) The assay has a very low false negative rate (NPV close to 1) and therefore will classify most women with the disease, correctly; however, it has a very high false positive rate giving a very low PPV and will misclassify many women who are disease free. This assay is not good enough to be used to screen for ovarian cancer. Case study 1.2 (a) By exchanging samples between the laboratories and comparing results. (b) Peripheral laboratories should be encouraged to use the same method as the specialist laboratory or send all requests to them. Case study 1.3 (a) The sample has not reached the laboratory quickly enough and intracellular contents have leaked into the plasma. Red cells have high potassium content and this explains the result. (b) Request a repeat sample to be taken and transported to the laboratory for urgent processing. Case study 1.4 (a) This is a systematic error (a constant shift in one direction). (b) The most likely cause of the shift is that the incorrect calibrator has been used. (c) Re-calibrate the assay using the correct calibrator and check the QC again. Case study 1.5 (a) The laboratory cannot produce evidence to conrm that the reagents have been stored at the recommended temperature and therefore cannot guarantee that the assay is working. (b) A procedure must be introduced to check refrigerator temperatures regularly. (c) Perform another horizontal audit at a later date. (b) AKI causes a rapid decline in calcium (due to failed vitamin D synthesis) and increase in serum phosphate concentration due to renal retention. It is also thought that calcium is sequestered by binding to damaged muscle bres, exacerbating the hypocalcaemia. Case study 3.2 (a) Cystinuria is an autosomal recessive condition due to a defect in proximal tubular cystine transport. Cystinuria should always be excluded as a cause of stone formation, but the index of suspicion is raised if stones occur (i) at a young age and/or (ii) there is a family history of renal stones. Once a cystinuric patient has been identied, it is important to screen all members of the family. (b) In the commonest form of cystinuria there is also excess excretion of these dibasic amino acids, which share the same tubular transporter as cystine. However, their presence in urine appears benign.
Chapter 4
Case study 4.1 (a) This is a classical presentation of gout, being of sudden onset, nocturnal occurrence, and symptoms in a single joint. (b) He should be treated initially with a non-steroidal anti-inammatory drug such as naproxen and the symptoms should subside rapidly. Given his family history, signs, and symptoms, three to four weeks later he should be prescribed allopurinol, a drug which inhibits xanthine oxidase, the enzyme that mediates the formation of urate, to prevent further attacks. Case study 4.2 (a) The patient has a high serum creatinine and a reduced EGFR consistent with chronic kidney disease. The high serum urea suggests a depletion of the intravascular volume probably caused by overmedication with diuretic therapy. There is severe hyperuricaemia, which is probably mainly caused by over treatment with diuretics, but also by the chronic kidney disease. (b) Acute gout and chronic tophaceous gout. (c) The diagnosis may be conrmed by microscopic examination of synovial uid taken from the knee joint to show the presence of crystals of monosodium urate.
Chapter 3
Case study 3.1 (a) Myoglobin, derived from muscular breakdown (rhabdomyolysis) imparts a red, muddy colour to urine. It is directly toxic to renal tubular cells, therefore precipitating AKI. Many laboratories offered a screening test for urinary myoglobin. However, the assay is poorly specic and sensitive and no quality assessment program existed for this measurement. Generally it is considered that serum creatine kinase activity is more closely related to the extent of injury and the renal prognosis.
Chapter 5
Case study 5.1 The plasma sodium is clearly very low, as is the osmolality, indicating a true hyponatraemia (i.e. not pseudo-hyponatraemia). Creatinine and urea are not raised, suggesting renal function is adequate. In health, the physiological response to such a low plasma osmolality should be to stop the production of ADH and for dilute urine of high volume to be produced. Further laboratory tests might
OXFORD UNIVER SIT Y PRESS 2011
ANSWERS TO CASE STUDIES
(b) The low HCO3 concentration would indicate a (metabolic) acidosis and is consistent with the low pH, the low PCO2 is not consistent with the acidaemia, but more indicative of the compensatory response (hyperventilation). As the pH has not returned to normal there is only partial compensation. This is a partially compensated metabolic acidosis.
include tests of endocrine function, including thyroid function tests and tests for cortisol, but the results are consistent with a diagnosis of SIADH. Case study 5.2 The plasma sodium is increased, as is the osmolality. These results indicate an appropriate degree of sodium excretion and the production of concentrated urine in response to dehydration. The hypernatraemia resolved within three days. Case study 5.3 The plasma potassium result is below the critical threshold for most laboratories and should be communicated rapidly to the requesting clinician. Hypokalaemia in this case was caused by treatment with a thiazide diuretic. Case study 5.4 (a) The electrolyte abnormality is hypokalaemia and this is consistent with Conns syndrome. (b) This could be conrmed by measurement of the plasma aldosterone concentration and the plasma renin activity. In Conns syndrome, the aldosterone will be increased and the renin activity low. The collection of the samples for the analysis of aldosterone and renin must be associated with avoidance of hypertensive medication as these can induce similar biochemical changes. Case study 5.5 The data set shows electrolyte results that are not compatible with normal physiology or, indeed, life. The specimen tube was inspected and found to be one containing sodium uoride and potassium oxalate, a preservative and anticoagulant additive used for specimens requiring glucose analysis. The patient had also had a request for glucose analysis and the two tubes had been inadvertently swapped. Re-analysis of the tests using the correct tubes was required. Case study 5.6 (a) The electrolyte abnormality is hyperkalaemia. (b) The sample is not haemolysed, nor has analysis been delayed; both of which might falsely elevate the potassium result. The calcium value is within the reference range, which would suggest the specimen has been collected into an appropriate specimen collection tube. The urea and creatinine concentrations are also increased, and together with the potassium value would suggest the patient has renal failure. The liver function tests are all within their reference ranges. (c) In most laboratories such a potassium result would be communicated to the clinicians managing the patient as soon as possible, usually by telephone as the increased potassium could lead to cardiac arrest. Case study 5.7 (a) This appears to be an example of hyponatraemia. However, the total protein value of 140 g/L is highly abnormal and will produce the effect of pseudohyponatraemia. (b) The difference in sodium values from the main automated analyser, which employs an indirect ion selective electrode (131 mmol/L) and the direct reading ion selective electrode (144 mmol/L) is due to the water displacement effect caused by the increased protein concentration in the sample. The clinically relevant result is that derived from the direct reading ion selective electrode and, as such, this patient does not have true hyponatraemia.
Case study 6.2
(a) The decreased pH indicates acidaemia. PCO2 and HCO3 are abnormal in the same direction (both low), therefore less likely to be a mixed acid-base disorder. (b) The low HCO3 concentration would indicate a (metabolic) acidosis and is consistent with the low pH, the low PCO2 is not consistent with the acidaemia, but more indicative of the compensatory response (hyperventilation). This is an uncompensated metabolic acidosis.
(c) The other laboratory tests indicate hyperkalaemia, due to the movement of potassium out of cells and there is a raised anion gap. This is consistent with the ingestion of ethylene glycol (antifreeze) that metabolizes into acidic (anionic) products which increases the unmeasured anion fraction in the blood. Case study 6.3 (a) The increased pH indicates alkalaemia. PCO2 is abnormal indicating a respiratory alkalosis.
(b) The HCO3 concentration is still within normal range indicating that the slower renal compensatory response had not yet begun. This is an uncompensated respiratory alkalosis.
Case study 6.4
(a) Low pH indicates acidaemia. PCO2 and HCO3 are abnormal in different directions, which indicates a possible mixed acid-base disorder.
(b) The results would indicate a respiratory acidosis and a metabolic acidosis. This is a mixed acid-base disorder: respiratory acidosis and metabolic acidosis. (c) Such results are consistent with a patient after cardiac arrest with impaired respiratory and circulatory functions. Case study 6.5
The raised pH indicates alkalaemia. PCO2 and HCO3 are abnormal in the same direction, which indicates a possible respiratory alka losis. The HCO3 results would appear to conrm this assumption. However, such low HCO3 levels are uncommon and not consistent with the relative decrease in PCO2 levels. This would indicate a respiratory alkalosis superimposed with a metabolic acidosis. This is a mixed acid-base disorder; respiratory alkalosis and metabolic acidosis. Also, the serum electrolyte measurements conrm a high anion gap associated with metabolic acidosis, due to the unmeasured anion metabolites. These results are consistent with a patient with salicylate overdose. Salicylate stimulates the respiratory centre to hyperventilate. Salicylate metabolites are acidic, resulting in the metabolic acidosis. Salicylate determination would be appropriate to conrm the diagnosis.
Chapter 7
Case study 7.1 (a) The ndings on the ECG indicate the chance that this man is having an MI is very high. (b) No. Given the chance this man is suffering a MI, treatment needs to be started as quickly as possible. The changes on the ECG are sufficient to commence treatment either by immediate cardiac catheterization or administration of a thrombolytic (clot busting) drug.
Chapter 6
Case study 6.1
(a) Low pH indicates acidaemia. PCO2 and HCO3 are abnormal in the same direction (both low), therefore less likely to be a mixed acid-base disorder.
ANSWERS TO CASE STUDIES
(c) The second troponin value conrms that he has had an AMI. He has chest pains, changes in his ECG and a rise in his troponin from undetectable to 1.5 g/L. This meets the diagnostic criteria for an AMI. Case study 7.2 (a) It is difficult to be sure whether this woman is having an MI although the previous history of heart surgery and the increased troponin on admission makes this likely. The working diagnosis for this patient is a suspected ACS and further tests are recommended. Although she has an elevated troponin she does not meet all the criteria for a diagnosis of MI. (b) Yes. This patient had NSTEMI, which was conrmed by the rise in troponin from the admission to six-hour values. She should be treated with anti-thrombotic (blood thinning) drugs and considered for cardiac catheterization at the next convenient opportunity. Case study 7.3 (a) This is very unlikely. This is a young man and there is evidence that he has been stabbed. Heart damage from the stabbing is more likely to be the cause of his collapse than an MI. (b) He has had damage to his heart from stabbing. This will damage heart muscle cells and cause the release of troponin. Because the troponin elevation is due to direct myocardial damage from trauma, this is a non-ischemic cardiac injury.
Case sudy 9.2 (a) Her very high TAGs are due to the presence of chlomicrons and other TRL particles. She had a genetic predisposition to hypertriglyceridaemia, which would be classied as Frederickson type I. This condition has been exacerbated by dietary indiscretion, excessive alcohol consumption, and poor diabetic control. Dietary advice was reinforced. She was treated with the triacylglycerol-lowering drug, brate, in addition to her statin treatment. (b) This case shows that the only present cure for chylomicronaemia is not to eat fat. The womans HDL remained low because of increased exchange of HDL cholesterol with TRL. Although the main clinical problem is pancreatitis, related to her high TAG concentrations, she requires statin medication to lower her LDL because of the cardiovascular risk associated with her diabetes. This pattern of dyslipidaemia is usually associated with the accumulation of atherogenic small dense LDL. Case study 9.3 (a) This woman had type 3 dyslipidaemia. Most people with the E2E2 genotype do not develop dyslipidaemia. Usually additional factors, such as high energy diet, obesity, and diabetes contribute to its development. The hypertriglyceridaemia is due to the accumulation of IDL particles, which are atherogenic. (b) Because of the increased cardiovascular risk secondary to her diabetes.
Chapter 8
Case study 8.1 The LFTs are indicative of cholestasis, with a low albumin and raised bilirubin suggestive of a chronic liver disorder. The rst line of investigation would be an abdominal X-ray and liver ultrasound to rule out gallstones and obstruction due to a tumour in the bile ducts or pancreas. She is of an age where autoimmune liver disease must be considered and autoantibodies measured. Her anti-mitochondrial antibody was positive, consistent with PBC. Case study 8.2 The AST and ALP results are within reference ranges and suggest no hepatocellular damage. The urine bilirubin is negative, suggesting that the increased serum bilirubin must be unconjugated in nature. The normal haemoglobin and reticulocyte count suggest that haemolysis cannot be responsible for this raised bilirubin. It is very likely that the mild jaundice is because the individual suffers from Gilberts syndrome. In Gilberts syndrome, there is reduced activity of UDP-glucuronosyl transferase and often reduced uptake of unconjugated bilirubin by hepatocytes. Case study 8.3 The recent travel to Africa and the hepatitic pattern of the LFTs strongly suggest an infective cause of his liver disease. Hepatitis A is endemic in many parts of the developing world and could cause these results and the clinical ndings. Hepatitis B and C are less likely as there is no evidence of at-risk behaviour, for example sexual activity or drug misuse. Other causes of infectious hepatitis such as Weils disease (leptospirosis) or malaria should also be on the list of possible diagnoses. In fact, he had hepatitis A.
Chapter 10
Case study 10.1 The patient suffers from hypercalcaemia as conrmed by the high serum calcium and supported by her clinical features. A possible explanation for this could be that she took too much of the vitamin D therapy resulting in hypercalcaemia. Case study 10.2 (a) 3.46 mmol/L. (b) She does not suffer from diabetes mellitus as her urine glucose is negative. She does have hypercalcaemia and this is supported by her clinical features. Common causes of hypercalcaemia in clinical practice are primary hyperparathyroidism or malignancy. (c) Measurements of serum PTH will be high if she suffers from primary hyperparathyroidism and low in malignancy. (d) The patient suffers from dehydration as she has a high serum sodium and urea, and this is likely to be due to the vomiting. Rehydration should be a priority before identifying and treating the cause of the hypercalcaemia. Case study 10.3 The results suggest hypocalcaemia but the values for serum calcium are too low and so this is likely to be artefactual. Such ndings are typical of blood being collected into EDTA tubes. The EDTA chelates the calcium ions, hence the low reading for calcium. Tubes containing EDTA as an anticoagulant are commonly used in haematology laboratories. Case study 10.4
Chapter 9
Case study 9.1 These results show that she has mild subclinical hypothyroidism and secondary hypercholesterolaemia. After treating her hypothyroidism with a small dose of thyroxine, her cholesterol was found to be 4.2 mmol/L. Given she was healthy and had no risk factors for heart disease, this cholesterol concentration is satisfactory and further treatment is unnecessary.
(a) This patient has hypocalcaemia with hyperphosphataemia, which is typical of reduced PTH secretion as in hypoparathyroidism. She had undergone thyroidectomy and this could have resulted in accidental removal of her parathyroid gland giving rise to hypoparathyroidism. (b) Cataracts occur frequently in patients with hypoparathyroidism and arise due to precipitation of calcium phosphate in the eye lens.
ANSWERS TO CASE STUDIES
Case study 10.5 (a) This patient has hypocalcaemia and the likely cause of this is the hypomagnesaemia. A low serum magnesium concentration can cause hypocalcaemia by reducing action of PTH and partly by inhibiting secretion of PTH from the parathyroid glands. (b) She should be placed on calcium and magnesium supplements.
Case study 12.3 (a) The patient has increased free T4 and free T3 with inappropriately high concentrations of TSH. The concentrations of testosterone, FSH, and LH are also high. (b) Imaging of the brain and pituitary which may reveal a pituitary tumour. (c) The patient has clinical and laboratory ndings consistent with hyperthyroidism. It is likely the individual has a pituitary tumour secreting TSH. Most of these tumours secrete TSH alone (72%), but some tumours can secrete other hormones. The high testosterone and FSH/LH are consistent with a TSH secreting tumour.
Chapter 11
Case study 11.1 The patient has a normal TSH and free T4 and is biochemically euthyroid, that is normal thyroid function. However, the cortisol is <550 nmol/L so it does not exclude adrenal or pituitary dysfunction. Note, however, that the sample was collected at 2 pm. Before proceeding with further investigations, the sample should be collected at 9 am for cortisol measurement. If the cortisol concentration in this sample is greater than 550 nmol/L then that would suggest normal pituitary and adrenal function. Case study 11.2 (a) The most likely explanation for a suppressed LH/FSH and increased prolactin in a woman of childbearing age is pregnancy. (b) Therefore human chorionic gonadotrophin (hCG) should be measured in this sample to exclude pregnancy. Case study 11.3 (a) This man presented with classical clinical signs of GH excess. The patients blood glucose is in the diabetic range and his random GH is detectable although within the normal range. The physician is therefore considering the diagnosis of acromegaly. (b) The detectable random GH does not exclude acromegaly even though it is within the normal range, and it is necessary to establish if GH can be suppressed following the OGTT. (c) During the OGTT, the concentration of serum GH does not decline, supporting the diagnosis of acromegaly. (d) For further investigation, measurement of serum IGF-1 would be useful, as would pituitary imaging to check for pituitary mass. Case study 11.4 (a) The results of the water deprivation test show an increasing plasma osmolality, with an inappropriately low urine osmolality. (b) The differential diagnosis is therefore between cranial and nephrogenic diabetes insipidus. (c) Following administration of DDAVP, the urine becomes concentrated and plasma osmolality returns to normal. (d) The diagnosis is therefore cranial diabetes insipidus.
Chapter 13
Case study 13.1 (a) This patient had adrenal insufficiency, hence the low serum cortisol concentration. Cortisol is an essential counter-regulatory hormone and glucocorticoid decient patients are at high risk of hypoglycaemia. In an acutely ill patient like this, cortisol levels are usually elevated so the low cortisol was an important pointer to the diagnosis of adrenal insufficiency. In this case, the adrenal insufciency was secondary and due to pituitary disease. However, the cortisol result was not returned to the ward until after the patient had died. The initial presentation was hypoglycaemic coma as conrmed by laboratory glucose measurements. Primary and secondary adrenal failure should always be considered as a cause for hypoglycaemia, especially in hypoglycaemic coma. If suspected, glucocorticoid treatment should be given. This case emphasizes that cortisol deciency is a life-threatening condition and unfortunately here had a fatal outcome. (b) The diagnosis is hypoglycaemia caused by adrenal failure secondary to pituitary failure. Case study 13.2 (a) He has developed type 2 diabetes and expresses all the clinical and biochemical features of the metabolic syndrome. (b) The results are related to his sedentary lifestyle and his developing obesity. He is insulin-resistant and his high triacylglycerols are due to the failure of insulin to regulate his lipoprotein metabolism as well as his glucose homeostasis. The inammatory component of the metabolic syndrome which is related to his adiposity is affecting his vascular endothelium, contributing to his high blood pressure. (c) He should be advised to take more exercise and lose weight. As he is obese, an insulin sensitizing drug such as metformin should be used. In addition, antihypertensive medication should be given and because of the increased cardiovascular risk he should be prescribed a statin drug to lower his cholesterol. Case study 13.3 (a) The diagnosis is severe diabetic ketoacidosis. (b) She has a low pH because of unregulated lipolysis due to severe insulin deciency, increasing the production of keto acids such as acetoacetate from triacylglycerol stores. Acetoacetate is an end product of fatty acid metabolism which spontaneously decarboxylates to acetone and can be detected in the urine and smelt on the breath. (c) The serum potassium is raised because the acidosis causes hydrogen ions to enter cells and displace potassium (the major intracellular cation) into the extracellular space. Additionally, insulin upregulates the cell membrane sodium/potassium exchange pump which keeps potassium inside and sodium outside cells.
Chapter 12
Case study 12.1 (a) The patient has a suppressed TSH, normal freeT4, and increased free T3. (b) T3-toxicosis. Case study 12.2 Plasma TSH is not a reliable measure of thyroid status in the early months of treating hyperthyroidism as the response lags behind the fall in free T4 and free T3 for several weeks. During this time free T4 and free T3 are the most reliable indicators. In this patient, the free T4 and free T3 results would support a reduction in the dose of carbimazole used.
ANSWERS TO CASE STUDIES
(d) She has thrush, which is a pathological yeast infection caused by Candida albicans, which thrives in sugar-rich urine. Patients with diabetes often have chronic candida infections. (e) She was thirsty because of her need to replace uid due to high glucose levels, which were producing an osmotic diuresis. (f) She had lost weight because in uncontrolled diabetes there is a large calorie loss in the urine as glucose. (g) She had a faint rapid pulse on admission because her plasma volume was reduced due to her uid loss in the urine. (h) She should be rehydrated with intravenous saline and soluble insulin. She will then require stablilizing on a long-term insulin regime. Case study 13.4 (a) He is pale and clammy due to the release of catecholamines in response to the hypoglycaemia. The rm rapid pulse is also a catecholamine mediated effect on the heart. (b) The laboratory results suggest inappropriate insulin secretion. The neurological episode followed by unconsciousness is due to the effects of the hypoglycaemia on the central nervous system. The cortisol result rules out adrenal insufficiency as a cause of hypoglycaemia and the negative drug screen makes ingestion of hypoglycaemic drugs unlikely. The high insulin, together with the low plasma glucose is referred to as inappropriate insulin secretion. It is called inappropriate because normally when glucose is low insulin is also low. The main causes of inappropriate insulin secretion are an insulinoma, that is, a pancreatic beta cell tumour producing insulin, exogenous insulin administration, or ingestion of sulphonylurea drugs. (c) C-peptide measurements would be useful and are low in exogenous insulin administration but high in an insulinoma. An abdominal CT scan would be useful and may reveal the presence of a tumour in the pancreas, consistent with an insulinoma.
(b) The plasma cortisol concentration will be suppressed in a low dose dexamethasone suppression test in all cases except for Cushings. A high ACTH excludes an adrenal tumour secreting cortisol. (c) Plasma cortisol concentration will be suppressed in a high dose dexamethasone suppression test in most cases of Cushings disease (pituitary tumour secreting ACTH), but not if the ACTH tumour is ectopic. Cushings disease is usually associated with weight gain around the waste. Ectopic ACTH secreting tumours are aggressive and not all features of cortisol excess are apparent in the time course of the disease, which is rapidly terminal. A tumour in the lung was found in this case. Case study 14.4 (a) These results were suggestive of primary aldosteronism. The fall in aldosterone concentration on ambulation, with continued low renin activity, favours an adenoma. If the patient has bilateral adrenal hyperplasia the plasma aldosterone increases after ambulation. (b) A catheterization study may be performed if imaging did not conrm a unilateral lesion. A dexamethasone suppression test with normal 18-hydroxycortisol concentrations would exclude glucocorticoid remediable aldosteronism.
Chapter 15
Case study 15.1 (a) As her prolactin had normalized and her periods remained regular this suggests that hyperprolactinaemia was not the cause of infertility. (b) A macroprolactin screen was indicated and this should be carried out at initial presentation in all new cases of hyperprolactinaemia. In the event the patient was shown to have macroprolactinaemia. Case study 15.2 (a) Nasreen has all the features of polycystic ovary syndrome. (b) In an obese patient with PCOS it is appropriate to perform a glucose tolerance test. Case study 15.3 (a) The high gonadotrophins suggest a premature menopause, which was conrmed by ovarian biopsy. (b) As she is now menopausal and her ovaries contain no viable follicles, Sharons principal option for a pregnancy is egg donation.
Chapter 14
Case study 14.1 (a) Salt-losing congenital adrenal hyperplasia due to 21-hydroxylase deciency is indicated. (b) If the 17-OHP had been measured in a direct assay, a repeat measurement in an assay after solvent extraction should be conducted to exclude interference from foetal zone steroids. (c) Plasma aldosterone would be below the reference range in CAH due to 21-hydroxylase deciency, adrenal hypoplasia, 3-hydroxysteroid dehydrogenase deciency, and aldosterone synthase deciency. These defects could be picked up with a urine steroid prole analysis. If aldosterone is above the reference range this would suggest salt loss due to renal disease, aldosterone resistance, or a sodium channel defect. Case study 14.2 (a) The symptoms, physical ndings with hyponatraemia, hyperkalaemia, and metabolic acidosis are typical of adrenal failure. Diabetes mellitus was excluded by the urine tests. (b) Plasma ACTH will be raised. A synacthen test can be performed. You will see low plasma cortisol concentrations basally and no response to the synacthen if the patient has adrenal failure. Case study 14.3 (a) High cortisol, with no diurnal rhythm is seen in Cushings disease and Cushings syndrome. However, hypercortisolism can also be seen in stress, depression, and alcoholism.
Chapter 16
Case study 16.1 (a) His albumin is signicantly low and his urea and creatinine are consistent with dehydration as a result of his poor oral intake. His serum sodium is borderline low. (b) C-reactive protein to conrm the degree of the acute phase response. The C-reactive protein level was 220 mg/L. Thus, the albumin level resulted from an ongoing acute phase response. (c) In addition to treatment for sepsis, he requires oral nutritional supplements until his appetite improves. Case study 16.2 (a) Serum magnesium. (b) In acute excess, alcohol acts as a diuretic, causing a rapid and large increase in urinary magnesium excretion. In chronic excess, alcohol depletes the bodys magnesium stores. In addition, alcohol abusers often have a poor diet and do not eat sufficient magnesium rich foods (legumes, nuts, green vegetables, and whole
ANSWERS TO CASE STUDIES
grains). Magnesium requirements are therefore increased in those who abuse alcohol. (c) Magnesium can cause hypocalcaemia by two mechanisms: (i) reducing the release of PTH and (ii) decreasing the action of PTH by a post-receptor mechanism. Such hypocalcaemia is resistant to calcium replacement but is usually responsive to magnesium replacement without calcium replacement. Case study 16.3 (a) Whilst technically possible, vitamin C analysis has very specialized pre-analytical requirements and the turnaround time would be several weeks. (b) Vitamin C deciency results in scurvy, where there is defective synthesis of collagen, including that within blood vessel walls. (c) This can manifest as bleeding from all mucous membranes, swollen and bleeding gums with loosened teeth; bleeding into joints, deep tissue, into the skin, or around hair follicles; corkscrew hair; slow wound-healing; and anaemia. (d) The consumption of fresh fruit and vegetables (especially citrus fruit) is the best way to avoid scurvy. Case study 16.4 (a) His BMI is 36.6 kg/m2 and thus he is obese. (b) Polyuria, nocturia, and polydipsia. (c) He has a low HDL-C, giving him a cholesterol:HDL-C ratio of 8.3 and mixed dyslipidaemia (raised cholesterol and raised fasting triacylglycerols). Such a lipid pattern is commonly seen in both obesity and diabetes mellitus; when the cholesterol:HDL-C ratio 6.0. The 2006 Joint British Societies recommendations on the prevention of cardiovascular disease include treatment of the dyslipidaemia. Case study 16.5 (a) Her age (nutritional deciencies are not uncommon at the age of 75; her pathology (malignant tumour) causing unintentional weight loss of more than 10% of her body weight; latterly she had not been eating anything substantial at all. (b) Signicantly low inorganic phosphate with renal impairment and minor decreases in sodium, potassium, and albumin. (c) Give intravenous phosphate, arrange a dietetics review, and reduce her caloric intake.
of 550 pmol/L (<30), with pancreatic polypeptide, gastrin, somatostatin, and neurotensin being normal. A combination of low serum potassium and watery diarrhoea is a pointer to secretory diarrhoea, which is conrmed by the low FOG result. Further testing excludes laxative abuse, which is a relatively common cause. Elevated VIP concentration indicates likelihood of a VIPoma (vaso active intestinal peptide tumour as in the Verner Morrison syndrome) and this was subsequently identied as a pancreatic islet cell tumour conrmed by a computed tomography scan and biopsy. Case study 17.3 (a) Previous surgery and reduced acid production may compromise vitamin B12 absorption and predispose to bacterial overgrowth of the small bowel, with malabsorption and diarrhoea. (b) The normal CRP would not exclude a gastrointestinal inammatory condition, but would indicate malabsorption as being the most likely cause of weight loss. Basic laboratory tests for small bowel malabsorption and pancreatic exocrine function were normal but vitamin B12 concentration was low. Because of previous gastric surgery, the patient could be predisposed to bacterial colonization. Increase in breath hydrogen was >20 ppm above baseline and conrmed probable bacterial colonization of the small bowel. The patients symptoms responded well to broad spectrum antibiotics. Case study 17.4 Faecal calprotectin, if normal, may help to exclude inammatory bowel disease in younger patients. A test for coeliac disease, which has a high incidence of <1 in 500 in the general population and is easily performed, could also be undertaken.
Chapter 18
Case study 18.1 (a) The low IgG would lead to susceptibility to bacterial infection. (b) The BCG method at the local hospital had overestimated the albumin concentration.
Chapter 19
Case study 19.1 (a) Urine sodium, serum cortisol, and thyroid function tests should be carried out. (b) If the patient had SIADH, the urine sodium would be <300 mmol/L, cortisol and thyroid function tests would be within normal limits, and the patient would be clinically euvolaemic. Case study 19.2 (a) The CA 125 was measured too soon after surgery and was raised due to release from damaged tissue. The CA 125 should not be measured within two weeks of treatment to avoid such misleading results. (b) The clinician should wait and ask for CA 125 measurement at least two weeks post-surgery to provide information about the effectiveness of the treatment. The CA 125 could also be used to monitor this patient for disease recurrence, although we are still awaiting data as to the usefulness of this.
Chapter 17
Case study 17.1 (a) Diabetes is conrmed by the fasting blood glucose. The low haemoglobin (hypochromic anaemia) and gastrointestinal symptoms would suggest iron malabsorption or blood loss, which could be conrmed by a test of body iron stores such as serum ferritin. A test for coeliac disease, a cause of malabsorption, should also be carried out because of the strong association between coeliac disease and type 1 diabetes. (b) The low haemoglobin combined with the low serum ferritin indicates low iron stores. Since there is a strong association between type 1 diabetes and coeliac disease, the latter is suspected and conrmed as a strong possibility by the raised serum TTGA. Coeliac disease was conrmed from a duodenal biopsy which indicated partial villous atrophy. Case study 17.2 (a) No response to fasting would indicate diarrhoea was unrelated to dietary constituents and so was most likely secretory. (b) A gut hormone screen should now be undertaken as an investigation of rare causes of watery diarrhoea. This revealed a VIP level
Chapter 20
Case study 20.1 (a) Classical phenylketonuria due to phenylalanine hydroxylase deciency. (b) Dietary treatment with a low phenylalanine diet.
ANSWERS TO CASE STUDIES
Case study 20.2 (a) Urea cycle disorders, organic acid disorders. (b) Quantitative plasma amino acids, acyl carnitines, and urine organic acids. Case study 20.3 (a) A non-reducing sugar, for example galactose, fructose, or lactose. (b) Classical galactosaemia (galactose-1-phosphate uridyl transferase deciency). (c) Assessment of galactose-1-phosphate uridyl transferase activity in red blood cells (ensure baby has not had a blood transfusion). Case study 20.4 (a) Hypoglycaemia requires urgent treatment to avoid brain damage. (b) Due to storage of excess glycogen in the liver. The infant had glycogen storage disease type 1a (glucose-6-phosphatase deciency). (c) Endocrine disorders. (d) Universal newborn screening for MCADD has been in place in England since April 2009. It is important to remember that some patients may have missed screening.
Case study 21.2 This case underlines the importance of collecting samples for TDM at the appropriate time after the last dose and ensuring clinicians and nursing staff are made fully aware of the importance. Wherever possible the laboratory should discuss these results with the ward pharmacist or senior clinician. For tacromilus, peak concentrations of 4050 g/L can be observed, with the corresponding trough level often in the range 28 g/L after an oral dose.
Chapter 22
Case study 22.1 The lead was coming from car exhaust fumes. As a result of these ndings laws were put in place to stop the use of lead tetraethyl as an additive to petrol. Case study 22.2 (a) The maximum amount ingested = number of tablets unaccounted for amount per tablet = (16 2 8) 300 mg = 1800 mg, which is equivalent to 90 mg/kg body weight. (b) No further investigations are required as the aspirin ingested is only 90 mg/kg of body weight. Case study 22.3 Yes. Standard tablets contain 500 mg of paracetamol so she appears to have taken 16 g. Doses of more than 12 g are likely to cause potentially fatal liver damage. The history is conrmed by the serum paracetamol concentration at 5.5 hours being above the line for treatment on the treatment nomogram. Case study 22.4 The clinical features suggest opiate toxicity from intravenous use. Plasma ethanol should also be measured in addition to a urine screen for drugs of abuse, as ethanol is a CNS depressant and enhances opiate toxicity. A panel of drugs of abuse tests is preferable to a single test for opiates as, more often than not, more than one drug will be used.
Chapter 21
Case study 21.1 (a) It is possible that the patient took the digoxin just before going to see his doctor. Digoxin is slowly absorbed and so blood samples for digoxin measurements should be taken at least six hours after the last dose. (b) Serum creatinine to assess renal function as the renal system is the major route of digoxin clearance in the body, therefore deteriorating renal function could account for the high serum concentration. Patients with hypokalaemia are susceptible to digoxin toxicity even when digoxin concentrations are within the reference range, hence the need to measure serum potassium.
You might also like
- Store Employee Safety Handbook: Dear Dollar General EmployeeDocument6 pagesStore Employee Safety Handbook: Dear Dollar General EmployeeLaura HugginsNo ratings yet
- Nasm Study Guide PDF 2016 Nasm CPTDocument54 pagesNasm Study Guide PDF 2016 Nasm CPTAlonzo Mark100% (7)
- Hypokalemia 180813073624Document26 pagesHypokalemia 180813073624korotkofNo ratings yet
- Parasite QuizDocument7 pagesParasite QuizNur Liyana100% (1)
- Plasma Enzyme Levels and Their Clinical SignificanceDocument18 pagesPlasma Enzyme Levels and Their Clinical SignificanceNur LiyanaNo ratings yet
- Palliative Care: Improving Quality of Life When Seriously IllDocument16 pagesPalliative Care: Improving Quality of Life When Seriously IllHashim Ahmad100% (1)
- Thalassemi ADocument23 pagesThalassemi Ainterna MANADO100% (1)
- Megaloblastic and Other Macrocytic Anaemia: Dr. Nilukshi Perera Consultant HaematologistDocument58 pagesMegaloblastic and Other Macrocytic Anaemia: Dr. Nilukshi Perera Consultant HaematologistThaveeshaLindsayWhiteNo ratings yet
- PhospholipidsDocument3 pagesPhospholipidsPatti LeeNo ratings yet
- Clinical Chemistry Case StudyDocument8 pagesClinical Chemistry Case StudyGlydenne Glaire Poncardas Gayam67% (3)
- Potassium Homeostasis and Causes of Hypo/HyperkalemiaDocument47 pagesPotassium Homeostasis and Causes of Hypo/HyperkalemiaMayuresh ChaudhariNo ratings yet
- COPPERDocument36 pagesCOPPERmonday125100% (1)
- BUN and CreatinineDocument4 pagesBUN and Creatininesarguss14100% (1)
- Blood Transfusion: DR Vishwabharathi TDocument28 pagesBlood Transfusion: DR Vishwabharathi TSuma0% (1)
- Understanding Thalassemia: Causes, Types, Symptoms and TreatmentDocument23 pagesUnderstanding Thalassemia: Causes, Types, Symptoms and Treatmentinterna MANADONo ratings yet
- Concentration of Urine: Maj DR Shavana R.L RanaDocument22 pagesConcentration of Urine: Maj DR Shavana R.L RanaChandan Sah100% (1)
- Hematologic DisordersDocument197 pagesHematologic DisordersDanica Mae BianitoNo ratings yet
- Abg PPT NewDocument69 pagesAbg PPT NewMalaka Atapattu100% (2)
- Diabetes InsipidusDocument39 pagesDiabetes Insipidusกรคุง ภิญโญพจนารถNo ratings yet
- Pedigree Analysis and Inheritance PatternsDocument13 pagesPedigree Analysis and Inheritance PatternsVi LamNo ratings yet
- Hyperosmolar Non Ketotic ComaDocument23 pagesHyperosmolar Non Ketotic Comaprakash gunaNo ratings yet
- Acid-Base BalanceDocument28 pagesAcid-Base Balanceps4only100% (1)
- Composition and regulation of gastric juiceDocument31 pagesComposition and regulation of gastric juicewanderer_1010100% (1)
- Electrolyte Imbalances: Understanding Sodium, Potassium, and the Anion GapDocument4 pagesElectrolyte Imbalances: Understanding Sodium, Potassium, and the Anion Gapjohnjoseph.ermitanoNo ratings yet
- Diabetes MellitusDocument15 pagesDiabetes Mellitusfayeniwa100% (1)
- Eclampsia From MedscapeDocument11 pagesEclampsia From Medscapevicky v. p. wardenaar100% (1)
- 2 Medicine HematologyDocument78 pages2 Medicine HematologyAmitNo ratings yet
- Wilson S DiseaseDocument28 pagesWilson S DiseasemichaelcylNo ratings yet
- MED - Finals 1.5 - Asthma PDFDocument12 pagesMED - Finals 1.5 - Asthma PDFYestin Reece Corpus ArcegaNo ratings yet
- ADRENALSDocument60 pagesADRENALSJyoti ChadhaNo ratings yet
- Pathophysiology 2Document92 pagesPathophysiology 2Princess AgarwalNo ratings yet
- AlcoholDocument20 pagesAlcoholrecklesspeshal2058100% (1)
- Hepatic Encephalopathy Is by DR Gireesh Kumar K PDocument16 pagesHepatic Encephalopathy Is by DR Gireesh Kumar K PAETCM Emergency medicineNo ratings yet
- Semmelweis Uni Entrance Exam List QuestionDocument6 pagesSemmelweis Uni Entrance Exam List QuestionNgô Minh KhuêNo ratings yet
- Dr. Niranjan Murthy H.L Assistant Professor Dept of Physiology SSMCDocument37 pagesDr. Niranjan Murthy H.L Assistant Professor Dept of Physiology SSMCnirilib100% (2)
- Serum ElectrolytesDocument2 pagesSerum ElectrolytesKervin CablaidaNo ratings yet
- Surgical Conditions of Pleura: Kibrom Gebreselassie, MD, FCS-ECSA Cardiovascular and Thoracic SurgeonDocument63 pagesSurgical Conditions of Pleura: Kibrom Gebreselassie, MD, FCS-ECSA Cardiovascular and Thoracic SurgeonVincent SerNo ratings yet
- SICKLE CELL DISEASE: A CASE OF VASO-OCCLUSIVE CRISISDocument44 pagesSICKLE CELL DISEASE: A CASE OF VASO-OCCLUSIVE CRISISNICHOLAS KAUMBA100% (1)
- Pathophysiology of Hemolytic AnemiaDocument2 pagesPathophysiology of Hemolytic AnemiaArvin CruzNo ratings yet
- Cme PresentationDocument56 pagesCme Presentationapi-439712011No ratings yet
- Celiac DiseaseDocument37 pagesCeliac DiseaseTaj lamajed100% (1)
- Hypocalcemia: Author: Christopher B Beach, MD, FACEP, FAAEM, Associate Professor and ViceDocument65 pagesHypocalcemia: Author: Christopher B Beach, MD, FACEP, FAAEM, Associate Professor and ViceronelnNo ratings yet
- Review Article: Sodium Bicarbonate Therapy in Patients With Metabolic AcidosisDocument14 pagesReview Article: Sodium Bicarbonate Therapy in Patients With Metabolic AcidosisMuhammad Arif Nur SyahidNo ratings yet
- Acid-Base Disorders NotesDocument10 pagesAcid-Base Disorders NotesLovely100% (1)
- Lab Report 1 (Hematology)Document8 pagesLab Report 1 (Hematology)Romanda GreeneNo ratings yet
- Arterial Blood Gas InterpretationDocument65 pagesArterial Blood Gas InterpretationDaniel AryanNo ratings yet
- Tubular Functions of KidneyDocument161 pagesTubular Functions of KidneyPhysiology by Dr RaghuveerNo ratings yet
- Complement: Kathleen Basa Kris Nicole de Guzman Jessica Mae Ong 3HmtDocument70 pagesComplement: Kathleen Basa Kris Nicole de Guzman Jessica Mae Ong 3HmtCherry Reyes-Principe100% (1)
- Aspirin OverdoseDocument3 pagesAspirin OverdoseSaputra BismaNo ratings yet
- NAFLD—Where We Stand TodayDocument32 pagesNAFLD—Where We Stand TodaySaad MotawéaNo ratings yet
- Understanding Metabolism of CarbohydratesDocument48 pagesUnderstanding Metabolism of CarbohydratesAbdullah TheNo ratings yet
- PHARM4515-16 (NSAIDs)Document45 pagesPHARM4515-16 (NSAIDs)kitsilcNo ratings yet
- Anemia in ChildrenDocument67 pagesAnemia in ChildrenDenny BimatamaNo ratings yet
- Hyperglycemia Crisis: Dr. Netty NurnaningtyasDocument34 pagesHyperglycemia Crisis: Dr. Netty Nurnaningtyasnetty nurnaningtyasNo ratings yet
- Acid Hydrolysis and Chemical Characterization of DNADocument28 pagesAcid Hydrolysis and Chemical Characterization of DNAai_ferminNo ratings yet
- UrinalysisDocument9 pagesUrinalysisSukma EffendyNo ratings yet
- Anti Diabetic DrugsDocument58 pagesAnti Diabetic DrugsDaniel WangNo ratings yet
- Assessment of Acid-Base DisordersDocument39 pagesAssessment of Acid-Base Disordersmonday125100% (1)
- Reverse Cholesterol TransportDocument29 pagesReverse Cholesterol TransportSolomon RotimiNo ratings yet
- Urinary Tract InfectionDocument30 pagesUrinary Tract InfectionMedita PrasetyoNo ratings yet
- Genetic Tongue RollingDocument18 pagesGenetic Tongue RollingMizaZainal100% (1)
- BloodDocument40 pagesBloodShaina Charmaine Quirol100% (1)
- Acute On Chronic Kidney DiseaseDocument6 pagesAcute On Chronic Kidney DiseaseElizabeth LieNo ratings yet
- Answers To Case StudiesDocument7 pagesAnswers To Case StudiesPhú NguyễnNo ratings yet
- Acid-Base and Electrolyte Handbook for Veterinary TechniciansFrom EverandAcid-Base and Electrolyte Handbook for Veterinary TechniciansAngela Randels-ThorpNo ratings yet
- Admission Hyperglycemia and The No - Reflow Phenomenon in Patients With Acute Myocardial InfarctionDocument10 pagesAdmission Hyperglycemia and The No - Reflow Phenomenon in Patients With Acute Myocardial InfarctionNur LiyanaNo ratings yet
- Taenia SagitaDocument3 pagesTaenia SagitaNur LiyanaNo ratings yet
- Basic Mechanisms of Diabetic Heart DiseaseDocument25 pagesBasic Mechanisms of Diabetic Heart DiseaseNur LiyanaNo ratings yet
- Acute Myocardial InfarctionDocument12 pagesAcute Myocardial InfarctionRoberto López Mata100% (1)
- Berberine Attenuates Cardiac Dysfunction in Hyperglycemic and Hypercholesterolemic RatsDocument7 pagesBerberine Attenuates Cardiac Dysfunction in Hyperglycemic and Hypercholesterolemic RatsNur LiyanaNo ratings yet
- Infarct Size Reduction in Acute Myocardial InfarctionDocument11 pagesInfarct Size Reduction in Acute Myocardial InfarctionNur LiyanaNo ratings yet
- Acute Hyperglycemia in Patients With Acute Myocardial InfarctionDocument9 pagesAcute Hyperglycemia in Patients With Acute Myocardial InfarctionNur LiyanaNo ratings yet
- Acute Hyperglycemia Abolishes Cardioprotection by Remote Ischemic PerconditioningDocument10 pagesAcute Hyperglycemia Abolishes Cardioprotection by Remote Ischemic PerconditioningNur LiyanaNo ratings yet
- Fin Nov 12 Sph2014Document11 pagesFin Nov 12 Sph2014Nur LiyanaNo ratings yet
- Thesis Guidelines Update180115Document53 pagesThesis Guidelines Update180115Nur LiyanaNo ratings yet
- 2-Introduction To ProtozoaDocument4 pages2-Introduction To ProtozoaNur LiyanaNo ratings yet
- Left Ventricular Diastolic Dysfunction in Diabetes.832Document1 pageLeft Ventricular Diastolic Dysfunction in Diabetes.832Nur LiyanaNo ratings yet
- Cardiac Dysfunction 2Document7 pagesCardiac Dysfunction 2Nur LiyanaNo ratings yet
- Sedative HypnoticsDocument6 pagesSedative HypnoticsNur LiyanaNo ratings yet
- Chapter 3 - EntomologyDocument11 pagesChapter 3 - EntomologyNur LiyanaNo ratings yet
- Cytokine Functions and Receptor FamiliesDocument6 pagesCytokine Functions and Receptor FamiliesNur LiyanaNo ratings yet
- Introduction To Systemic PathologyDocument11 pagesIntroduction To Systemic PathologyNur LiyanaNo ratings yet
- Chapter Seven: Immunity Response Induction: Granulocyte ExocytosisDocument4 pagesChapter Seven: Immunity Response Induction: Granulocyte ExocytosisNur LiyanaNo ratings yet
- Assessment Handout 2 SBD2013 201211Document1 pageAssessment Handout 2 SBD2013 201211Nur LiyanaNo ratings yet
- ENT156 Practice Midterm Exam QuestionsDocument3 pagesENT156 Practice Midterm Exam QuestionsRey Christian Cabreros91% (11)
- Introduction To HistopathologyDocument9 pagesIntroduction To HistopathologyNur LiyanaNo ratings yet
- Tutorial Related To Clinical BiochemistryDocument2 pagesTutorial Related To Clinical BiochemistryNur LiyanaNo ratings yet
- Typhoid FeverDocument5 pagesTyphoid FeverNur LiyanaNo ratings yet
- Basic PathologyDocument2 pagesBasic PathologyNur LiyanaNo ratings yet
- Introduction ImmunologyDocument8 pagesIntroduction ImmunologyNur LiyanaNo ratings yet
- Microbial DiseaseDocument3 pagesMicrobial DiseaseNur LiyanaNo ratings yet
- Introduction To Basic PathologyDocument30 pagesIntroduction To Basic PathologyNur LiyanaNo ratings yet
- Nejmcp 2108502Document9 pagesNejmcp 2108502Manuel GilNo ratings yet
- Salter 2018 - Changes in Temperature Management of Cardiac Arrest Patients Following Publication of The Target Temperature Management TrialDocument9 pagesSalter 2018 - Changes in Temperature Management of Cardiac Arrest Patients Following Publication of The Target Temperature Management TrialSteven BrownNo ratings yet
- 3B User-Manual BPAP-25A RESmart BMC V1.2 ENG PDFDocument38 pages3B User-Manual BPAP-25A RESmart BMC V1.2 ENG PDFBasheer AlmetwakelNo ratings yet
- DR Rashmi S R Consultant NephrologyDocument1 pageDR Rashmi S R Consultant Nephrologyanant chauhanNo ratings yet
- Don Mariano Marcos Memorial State University Campus Film Reveals Sugar's EffectsDocument3 pagesDon Mariano Marcos Memorial State University Campus Film Reveals Sugar's EffectsJinky FernandezNo ratings yet
- Comprehensive Development Plan 2021 RegulationsDocument308 pagesComprehensive Development Plan 2021 RegulationsRinoy R BhagoraNo ratings yet
- Perineal Care and CatheterizationDocument10 pagesPerineal Care and CatheterizationHarold DiasanaNo ratings yet
- Soal Bahasa Inggris TKJ SEMESTER GENAP 2020-2021: PoinDocument18 pagesSoal Bahasa Inggris TKJ SEMESTER GENAP 2020-2021: PoinRauf AthilaNo ratings yet
- Nursing Care Plan For Peritonitis NCPDocument2 pagesNursing Care Plan For Peritonitis NCPderic83% (6)
- Material: Safety Data SheetDocument3 pagesMaterial: Safety Data SheetMichael JoudalNo ratings yet
- Mise Ry by Stephen King: AnalysisDocument9 pagesMise Ry by Stephen King: AnalysisMartinaNo ratings yet
- 1 Assessment Data Form MS-1Document6 pages1 Assessment Data Form MS-1alharbimanar20No ratings yet
- The Role of The Government in Economics: Executive SummaryDocument10 pagesThe Role of The Government in Economics: Executive SummaryrojithvNo ratings yet
- REPUBLIC ACT NO. 10354 (The Responsible Parenthood and Reproductive Health Act of 2012) PDFDocument15 pagesREPUBLIC ACT NO. 10354 (The Responsible Parenthood and Reproductive Health Act of 2012) PDFYappi NaniNo ratings yet
- Utilidad de La Puntuación de Boey Y Portsmouth-Possum Fisiológico en Pacientes Con Úlcera Péptica PerforadaDocument8 pagesUtilidad de La Puntuación de Boey Y Portsmouth-Possum Fisiológico en Pacientes Con Úlcera Péptica PerforadaEdgarOrtaNo ratings yet
- Good Clinical Laboratory Practice (GCLP) : Quality Demanding From Clinical LaboratoriesDocument5 pagesGood Clinical Laboratory Practice (GCLP) : Quality Demanding From Clinical LaboratoriesJaneNo ratings yet
- Zircad: The Innovative Zirconium OxideDocument16 pagesZircad: The Innovative Zirconium OxideVladimirNo ratings yet
- Department of Education: Region Vi-Western Visayas Schools Division of SipalayDocument3 pagesDepartment of Education: Region Vi-Western Visayas Schools Division of SipalayRoseo BatillerNo ratings yet
- Building J Renovation-PlansDocument83 pagesBuilding J Renovation-PlansBala Hemanth KumarNo ratings yet
- Admission Criteria in A Pediat Ric Intensive Therapy Unit: Presentation of An Evaluation InstrumentDocument8 pagesAdmission Criteria in A Pediat Ric Intensive Therapy Unit: Presentation of An Evaluation InstrumentrupaliNo ratings yet
- ELIII - Vocabulary List Second TermDocument5 pagesELIII - Vocabulary List Second Termyacantomariana2No ratings yet
- Grade 7 Biology revision worksheetDocument3 pagesGrade 7 Biology revision worksheetRenee DisaNo ratings yet
- Miami-Dade County Response To Miami-Dade County Back Bay CSRM Feasibility StudyDocument6 pagesMiami-Dade County Response To Miami-Dade County Back Bay CSRM Feasibility StudyAmanda RojasNo ratings yet
- Corporate Ergonomics ProgramsDocument16 pagesCorporate Ergonomics ProgramsJharef Rupire DelgadoNo ratings yet
- Method Statement For Coring On Hollow Core Slab To Provide Holes For MEP Service Line OpeningsDocument6 pagesMethod Statement For Coring On Hollow Core Slab To Provide Holes For MEP Service Line Openingsmd_rehan_2No ratings yet
- Bivariate Probit and Logit Models ExampleDocument4 pagesBivariate Probit and Logit Models ExampleNchimunya Alik ChompololaNo ratings yet
- Malaya Integrated National High SchoolDocument28 pagesMalaya Integrated National High SchoolRea Maureen BansaleNo ratings yet