Professional Documents
Culture Documents
DPW Fact Sheet On Medicaid Expansion
Uploaded by
Nathan BenefieldOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
DPW Fact Sheet On Medicaid Expansion
Uploaded by
Nathan BenefieldCopyright:
Available Formats
FACT SHEET: Medicaid Expansion and Pennsylvania
Background: The Pennsylvania Medicaid program, often referred to as the Medical Assistance program, provides a comprehensive array of health and long-term care services to over 2.2 million Pennsylvanians. These benefits are provided to persons of all ages including adults, children, pregnant women, low-income families, people with disabilities and seniors. Currently 1 out of every 6 citizens in Pennsylvania receives Medicaid benefits. Spending on Medicaid programs accounts for 75 percent of the Department of Public Welfares (DPW) $27.6 billion budget (including state, federal and other funds). DPWs budget constitutes 39 percent of the states annual budget with Medicaid being the number one cost driver at 30 percent of Pennsylvanias General Fund. In addition to Medicaid, Pennsylvania also provides an additional layer of benefits as part of the safety net not found in many other states, namely state-only funded General Assistance medical benefits for adults who do not qualify for Medicaid. All of these programs represent important and vital services to some of Pennsylvanias most vulnerable citizens; however, funding for these programs represents a substantial amount of state and federal spending that continues to grow every year. Cost Growth of Current Program: The costs of the current Medicaid program in Pennsylvania continue to grow. Maintaining that cost growth is requiring substantial new state revenue. The costs to fund DPW are projected to grow by nearly $400 million in fiscal year 2013-2014. These costs do not include additional costs that the state may incur as a result of the Affordable Care Act (ACA). While Medicaid is a very important program, the continued annual cost growth is placing an increased strain and burden on Pennsylvanias budget and is making it more difficult for the state to invest in other important programs. Medicaid Expansion: The expansion of the Medicaid program, as proposed in the ACA, would make all adults between the ages of 19-64 with incomes at or below 133% of the federal poverty level (FPL) eligible for the program. This expansion would cover vulnerable persons as well as healthy, able-bodied individuals. However, as a result of the United States Supreme Courts ruling, states have the option to decide whether expansion of the Medicaid program is the best approach to improving access to affordable health care coverage for their citizens. After review, initial estimates on the costs and impact of expanding Pennsylvanias Medicaid program, as proposed in the ACA, are as follows: In total, expansion under the ACA would add over 800,000 new enrollees into the program resulting in approximately 1 in 4 Pennsylvanians being enrolled in Medicaid. The expansion would add more than 643,000 new adults above and beyond the current 2.2 million Pennsylvanians already enrolled. In addition to these new adults, the ACA mandates that an additional 161,306 children be covered through Medicaid. The number of children required to be covered by Medicaid increases by another 75,352 if Pennsylvania is required to transfer into Medicaid all the children under 133% FPL who are currently enrolled in the Childrens Health Insurance Program (CHIP) -- bringing the potential total number of children covered by Medicaid as a result of its expansion under the ACA to 236,658.
The expansion numbers above include individuals currently eligible who have not enrolled (woodwork) and individuals who are currently insured but could enter the program as a result of their employer dropping their insurance or a personal choice to drop coverage (droppers) because they would eligible to enroll in benefits fully paid for by the taxpayers. The premise that the federal government is picking up 100 percent of the costs of expansion is simply inaccurate. The additional federal funding does not apply to: o (1) current Medicaid recipients o (2) woodwork (new enrollees who were eligible under Pennsylvanias current program rules) o (3) droppers category noted above. In addition, the Commonwealth has to absorb increased costs associated with additional staffing, administrative and IT changes that are not paid for at the higher federal funding level. Even with initial federal support for some categories, under the ACA, federal funds will decline by 10 percent over the next 6 years -- thereby shifting a staggering burden onto the states. In addition, through the years states have seen Washington reduce or change funding for programs, such as Medicaid, as new policies are enacted or budget cuts threaten federal government spending. Any additional reductions in federal funding in the future would only compound the states burden further. Thousands of individuals with intellectual and physical disabilities have been on waiting lists for home and community based services for years. The ACA expansion does nothing to assist those people reach the critical services they need. There is no additional federal funding for these programs, and every state dollar put toward expanding Medicaid, takes away funding that could be used to help these individuals get off of waiting lists and into programs and services. A recent study by the Government Accountability Office (GAO) raised numerous concerns with the management of the current Medicaid program nationally. In particular, the GAO raised various inconsistencies in the administration of the program by the Center for Medicare & Medicaid Services and the overall financial integrity of what they have dubbed a high-risk program. In fact the GAO found that in 2009, $43 billion could not be traced directly back to Medicaid beneficiaries. Initial estimates show that expanding Medicaid, as proposed in the ACA, would cost Pennsylvania almost $1 billion of new state taxpayer dollars through FY 2015-2016; rising to a total of over $4.1 billion of new state taxpayer dollars by the end of FY 2020-2021. Conclusion: Pennsylvania is striving to maintain a health safety net for its citizens, while maintaining fiscal stability for our taxpayers. However, with continued large annual cost increases of the current Medicaid program, serious questions exist as to the sustainability of an expansion of Medicaid without significant reform of the program. DPW is examining reforms and program changes designed to meet the unique needs and diversity of Pennsylvanias citizens and to make the program work more effectively for beneficiaries and the state. It may be possible for Pennsylvania to provide affordable health care coverage to more of its citizens, but only if DPW is allowed to pursue meaningful reforms and program flexibility.
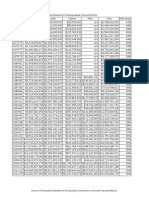
ACA Impact: Breakout of Costs to Pennsylvania
$1,400.000
$1,200.000
$1,000.000
$800.000
$600.000
$400.000
$200.000
State Savings State Cost Net
Millions of Dollars
SFY 14/15 Newly eligible SFY 15/16 SFY 16/17 Woodwork SFY 17/18 Savings SFY 18/19 Other Mandates SFY 14/15 ($288.939) $666.444 $377.505 SFY 15/16 ($352.329) $716.294 $363.965 SFY 16/17 ($408.526) $821.455 $412.929 SFY 17/18 ($421.360) $949.900 $528.540 SFY 18/19 ($414.536) $1,018.521 $603.985 SFY 19/20 ($369.872) $1,129.115 $759.242
$0.000
($200.000)
($400.000)
($600.000) SFY 19/20 SFY 20/21
SFY 13/14
SFY 13/14 ($144.799) $366.547 $221.748
SFY 20/21 ($346.864) $1,229.430 $882.566
TOTAL ($2,747.225) $6,897.705 $4,150.480
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- ESDocument139 pagesESRaviNo ratings yet
- IncytepdfDocument14 pagesIncytepdfnate_raymondNo ratings yet
- Community Nursing Practice QuizDocument60 pagesCommunity Nursing Practice QuizJason Cillo90% (10)
- PSEA Mailer For Tom WolfDocument2 pagesPSEA Mailer For Tom WolfNathan BenefieldNo ratings yet
- Benefield Testimony AttachmentsDocument18 pagesBenefield Testimony AttachmentsNathan BenefieldNo ratings yet
- Testimony To PA Funding Reform CommissionDocument8 pagesTestimony To PA Funding Reform CommissionNathan BenefieldNo ratings yet
- Gov. Wolf's Tax ProposalsDocument7 pagesGov. Wolf's Tax ProposalsNathan BenefieldNo ratings yet
- Benefield Testimony AttachmentsDocument18 pagesBenefield Testimony AttachmentsNathan BenefieldNo ratings yet
- Trans $ by State 2010Document1 pageTrans $ by State 2010Nathan BenefieldNo ratings yet
- PSEA Political MailerDocument2 pagesPSEA Political MailerNathan BenefieldNo ratings yet
- Charter Testimony (Benefield)Document5 pagesCharter Testimony (Benefield)Nathan BenefieldNo ratings yet
- Bleeding GreenDocument1 pageBleeding GreenNathan BenefieldNo ratings yet
- More Taxpayer Funded Lobbying Against School ChoiceDocument2 pagesMore Taxpayer Funded Lobbying Against School ChoiceNathan BenefieldNo ratings yet
- PSEA Campaign Mailer 2012 PrimaryDocument2 pagesPSEA Campaign Mailer 2012 PrimaryNathan BenefieldNo ratings yet
- Fireproofing Pennsylvania'S Economy:: P L Isttbdt2012 Pennsylvania State Budget 2012Document25 pagesFireproofing Pennsylvania'S Economy:: P L Isttbdt2012 Pennsylvania State Budget 2012Nathan BenefieldNo ratings yet
- Constitutionality of School Choice in PennsylvaniaDocument2 pagesConstitutionality of School Choice in PennsylvaniaNathan BenefieldNo ratings yet
- Pennsylvania Government Structural ReformsDocument5 pagesPennsylvania Government Structural ReformsNathan BenefieldNo ratings yet
- 2011-12 PA Budget Deal SpreadsheetDocument17 pages2011-12 PA Budget Deal SpreadsheetNathan BenefieldNo ratings yet
- PLCB Wine Kiosk Cover UpDocument7 pagesPLCB Wine Kiosk Cover UpNathan BenefieldNo ratings yet
- Shippensburg Prevailing Wage ResolutionDocument1 pageShippensburg Prevailing Wage ResolutionNathan BenefieldNo ratings yet
- PA Transportation SpendingDocument1 pagePA Transportation SpendingNathan BenefieldNo ratings yet
- Letter To Pitt FamilyDocument2 pagesLetter To Pitt FamilyNathan BenefieldNo ratings yet
- 2010 School Choice Poll - PADocument5 pages2010 School Choice Poll - PANathan BenefieldNo ratings yet
- PA Pension Reform PresentationDocument21 pagesPA Pension Reform PresentationNathan BenefieldNo ratings yet
- Pennsylvania State Union ContractsDocument2 pagesPennsylvania State Union ContractsNathan BenefieldNo ratings yet
- Toomey Vs Sestak On JobsDocument1 pageToomey Vs Sestak On JobsNathan BenefieldNo ratings yet
- Pennsylvania State Spending & Fiscal Crunch: What Now: by Nathan Benefield Commonwealth FoundationDocument22 pagesPennsylvania State Spending & Fiscal Crunch: What Now: by Nathan Benefield Commonwealth FoundationNathan BenefieldNo ratings yet
- Pennsylvania State Budget PresentationDocument20 pagesPennsylvania State Budget PresentationNathan BenefieldNo ratings yet
- Cabot Oil and Gas Letter Sent To DEPDocument6 pagesCabot Oil and Gas Letter Sent To DEPNathan BenefieldNo ratings yet
- Comparing States Severance TaxDocument1 pageComparing States Severance TaxNathan BenefieldNo ratings yet
- Gasland DebunkedDocument2 pagesGasland DebunkedNathan BenefieldNo ratings yet
- Memo On AEPS ReportDocument1 pageMemo On AEPS ReportNathan BenefieldNo ratings yet
- HPE Eligibility GuideDocument2 pagesHPE Eligibility GuideNephNo ratings yet
- Drug Utilization ReviewDocument7 pagesDrug Utilization ReviewFaizaNadeemNo ratings yet
- Health 101 Research PaperDocument14 pagesHealth 101 Research Paperapi-302787939No ratings yet
- Appendix 1 Eliminating Rural-DisparitiesDocument1 pageAppendix 1 Eliminating Rural-Disparitiesapi-104972596No ratings yet
- Accenture Medicaid Waiver Proposal REDACTED With CostDocument141 pagesAccenture Medicaid Waiver Proposal REDACTED With CostTech NiqoNo ratings yet
- Pennsylvania Medicaid Fraud Control UnitDocument2 pagesPennsylvania Medicaid Fraud Control UnitBeverly TranNo ratings yet
- BAGLY V Azar Amended Complaint PDFDocument107 pagesBAGLY V Azar Amended Complaint PDFRicca PrasadNo ratings yet
- Research Outline - Universal HealthcareDocument8 pagesResearch Outline - Universal HealthcarenemellistxNo ratings yet
- Ethics Discussion Otter AiDocument6 pagesEthics Discussion Otter AiGrigori ChulakiNo ratings yet
- Grandfamilies MaineDocument10 pagesGrandfamilies MaineNEWS CENTER MaineNo ratings yet
- INBDEBooster Patient Management NotesDocument19 pagesINBDEBooster Patient Management NotessuryathatiNo ratings yet
- 2008 Health Care Fraud ReportDocument44 pages2008 Health Care Fraud ReportMike DeWineNo ratings yet
- CB Insights Amazon in Healthcare BriefingDocument83 pagesCB Insights Amazon in Healthcare BriefingmedtechyNo ratings yet
- Complaint - Heritage and Evergreen v. NY DOHDocument86 pagesComplaint - Heritage and Evergreen v. NY DOHLuke ParsnowNo ratings yet
- OakPoint Carlton Ambulance StudyDocument2 pagesOakPoint Carlton Ambulance StudyDuluth News TribuneNo ratings yet
- 2022 California Childrens Report Card CompressedDocument104 pages2022 California Childrens Report Card CompressedRoxanne ReevesNo ratings yet
- SARCOA Senior Resource Directory 2009Document100 pagesSARCOA Senior Resource Directory 2009WISEGUY1943100% (2)
- Economics 6th Edition Hubbard Solutions ManualDocument26 pagesEconomics 6th Edition Hubbard Solutions ManualPeterHolmesfdns100% (54)
- 2022 State of The State BookDocument237 pages2022 State of The State BookCity & State NYNo ratings yet
- Family-Related Medicaid Programs Fact Sheet: January 2014Document10 pagesFamily-Related Medicaid Programs Fact Sheet: January 2014Patrick PerezNo ratings yet
- Fy 19 Enac FPDocument440 pagesFy 19 Enac FPThe Capitol PressroomNo ratings yet
- cms1500 FormDocument2 pagescms1500 FormpalashNo ratings yet
- Pap - Katrina Hpa432Document16 pagesPap - Katrina Hpa432api-324671865No ratings yet
- Finding Low-Cost Dental Care: National Institute of Dental and Craniofacial Research (NIDCR)Document2 pagesFinding Low-Cost Dental Care: National Institute of Dental and Craniofacial Research (NIDCR)P D SpencerNo ratings yet
- PWC Report On Medicaid ExpansionDocument6 pagesPWC Report On Medicaid ExpansionHLMeditNo ratings yet
- DHH S Acronym ListDocument15 pagesDHH S Acronym Listagostoanthony085No ratings yet
- Siemens Group Medical Insurance Guideline 2015-16Document34 pagesSiemens Group Medical Insurance Guideline 2015-16Vani ShriNo ratings yet