Professional Documents
Culture Documents
Oral Candidiasis Treatment - Phytotherapy Research
Uploaded by
SJ IraaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Oral Candidiasis Treatment - Phytotherapy Research
Uploaded by
SJ IraaCopyright:
Available Formats
652
PHYTOTHERAPY RESEARCH Phytother. Res. 19, 652654 (2005) Published online in Wiley InterScience (www.interscience.wiley.com). DOI: 10.1002/ptr.1715 V. R. SANTOS ET AL.
SHORT COMMUNICATION
Oral Candidiasis Treatment with Brazilian Ethanol Propolis Extract
V. R. Santos*, F. J. G. S. Pimenta, M. C. F. Aguiar, M. A. V. do Carmo, M. D. Naves and R. A. Mesquita
Department of Clinical Pathology and Surgery, Laboratory of Microbiology, Dentistry School, Minas Gerais Federal University, Avenida Antnio Carlos 6627, Campus da Pampulha, Belo Horizonte, Minas Gerais, Brazil, CEP 31.270-901
The Brazilian commercial ethanol propolis extract, also formulated to ensure physical and chemical stability, was found to inhibit oral candidiasis in 12 denture-bearing patients with prosthesis stomatitis candidiasis association. Copyright 2005 John Wiley & Sons, Ltd.
Keywords: Brazilian green propolis extract; oral candidiasis; antifungal activity.
INTRODUCTION Propolis has been used as a therapeutic agent by the world population since the time of Hippocrates. It is known that the ethanol extract of propolis (EEP) exhibits some pharmacological activities, such as antibacterial, antiviral, antifungal, antiinammatory, anesthesic and cytostatic properties (Marcucci, 1995; Kujumgiev et al., 1999; Pereira et al., 2002; Cicala et al., 2003). Propolis from the honey bee is used in folk medicine in the countries of Eastern Europe as an antiseptic and antiinammatory agent, for healing wounds and burns (Bankova et al., 1992; Valcic et al., 1999). Polyphenolic compounds, e.g. avonoid aglycones, pinocembrin, phenolic acids and their esters, phenolic aldehydes, have been mainly identied in propolis collected by bees in different regions (Bonhevi et al., 1994). Some avonoids are considered antimicrobial, such as pinocembrin, galangin, sakuranetin, kaempferol and pinobanksin (Aga et al., 1994; Drago et al., 2000). Other compounds are aromatic alcohols, aldehydes, acids and esters; aliphatic acids and esters; hydrocarbons; terpenoids, diterpenoids, amino acids, sugars, prenylated benzophenones, lignans, kaurenoic acid, triterpenes (lanosterol, cycloarterol, -amyrine), ferulic acid, phenolic compounds (3-phenyl-4-hydroxycinnamic acid (PHCA), 2,2-dimethyl-6-carboxyethyl-2h-1benzopyran (DCBE), 3-5-diprenyl-4-hhydroxycinnamic acid (DHCA), 6-propenoic-2-2,dimethyl-8-prenyl-2h1-benzopyran acid (DPB) (Velikova et al., 2000);
* Correspondence to: Professor Dr Vagner Rodrigues Santos, Department of Clinical Pathology and Surgery, Laboratory of Microbiology, Dentistry School, Minas Gerais Federal University, Avenida Antnio Carlos 6627, Campus da Pampulha, Belo Horizonte, Minas Gerais, Brazil, CEP 31.270-901. E-mail: vegneer2003@yahoo.com.br Contract/grant sponsor: Fundao de Amparo Pesquisa do Estado de Minas Gerais (FAPEMIG). Contract/grant sponsor: BIOBRS Laboratory (Montes Claros- Brazil). Contract/grant sponsor: CECON (So Paulo- Brazil). Contract/grant sponsor: Conselho Nacional de Desenvolvimento Cientico e Tecnolgico (CNPq). Contract/grant sponsor: PharmaNctar (Belo Horizonte- Brazil). Copyright 2005 John Wiley & Sons, Ltd. Copyright 2005 John Wiley & Sons, Ltd.
triterpenes (lanosterol, cycloarterol, -ampyrine); ferulic acid (Marcucci et al., 2001). The aim of this work was to verify the topical therapeutic effect of Brazilian green propolis extract on oral candidiasis and compare it with the positive control Nystatin.
MATERIAL AND METHODS Propolis. Green propolis was collected from the honey bee Apis mellifera in Minas Gerais State, Southeast Brazil. The 20% ethanol propolis extract used in this study was extracted by Pharma Nctar, Belo Horizonte, Brazil. Crude propolis samples collected by Apis mellifera were further dehydrated with a low-vacuum pump, and the extracts of the dried propolis were prepared as described by Koo and Park (1997). The dried propolis samples were ground into ne powder, and 2.0 g of propolis was mixed with 25 mL of 80% aqueous ethanol in a test tube and shaken at 70 C for 30 min. After extraction, the mixture was centrifuged at 8000 g to obtain the supernatants, which were named EPE. The original EPE was applied topically in candidiasis oral mucosa lesions with a swab. Patients. Details of patients are reported in Table 1. This research was approved by the UFMG Ethics Committee under number 020-97. Eighteen patients were selected from the UFMG Dentistry School Semiology Clinic. All the patients accepted the assigned treatment after being informed about the goals of the research, they had to sign a responsibility term and 12 received two bottles of the 20% EPE. After the habitual cleaning of the prothesis and the oral cavity, the patient had to dry the infected area using a swab, and then, applied topically the EPE four times a day, for 7 days. The patients mucosa was reevaluated, morphologically through a periodic acid Schiff (PAS) and biochemistry (Candifast, International Microbio, France) before and after the next treatment. Six patients, two men and four women were the control positive group using a solution of Micostatin/Nystatin (100 000 UI/mL,
24 March 2003 Phytother. Received Res. 19, 652654 (2005) Accepted 24 May 2005
ORAL CANDIDIASIS TREATMENT
653
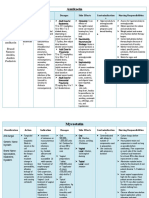
Table 1. Clinical aspects of patients with oral candidiasis from Clinic of Semiology and Pathology of Dentistry School UFMG participating in this study
Patient ISS SVCL AFF GMR MIC AFS EGSM TMS LMC HL SFS MCTS MJNM RCFR HBS JJAF GRA NMBA Age (years) 29 34 36 37 39 71 29 31 33 38 39 43 46 46 48 50 56 63 Race B W W W B B W B W W W W W B B W W W Gender F F M M F F F F M M F M F F M F F F Prosthesis TRDP TRDP TRDP TRDP TRDP TRDP TRDP TRDP TRDP TRDP/PRDP TRDP TRDP/PRDP TRDP TRDP TRDP TRDP TRDP TRDP Hard Hard Hard Hard Hard Hard Hard Hard Hard Hard Hard Hard Hard Hard Hard Hard Hard Hard Local lesions palate/soft palate palate palate palate/soft palate palate palate palate/soft palate palate palate palate/alveolar mucosa palate/soft palate palate/alveolar mucosa palate palate palate palate palate palate
F, female; M, male; TRDP, total removable dental prosthesis; PRDP, partial removable dental prosthesis; B, black; W, white.
Bristol-Myers Squibb, Brasil) in the same way as used for the propolis extract. Nystatin is the antifungal of choice for candidiasis treatment. The signicance of the results lies in the effect of EPE, when compared with Nystatin, on the presence or absence of lesions after treatment.
Table 2. Results of in vivo patients treatment of oral candidiasis with 20% Brazilian green ethanol propolis extract (EPE) and Nystatin (Nys). Use posology: 4 time/day for 7 days, topic application in local lesion and prosthesis surface
Patient ISS SVCL AFF GMR MIC AFS EGSM TMS LMC HL SFS MCTS MJNM RCFR HBS JJAF GRA NMBA Antifungal agent Nys Nys Nys Nys Nys Nys EPE EPE EPE EPE EPE EPE EPE EPE EPE EPE EPE EPE Result + + + ++ + ++ + ++ + + ++ + ++ + + + ++ ++
RESULTS In all patients treated with EPE and Nystatin the oral candidiasis lesion was in remission (Table 2).
CONCLUSIONS Candida albicans is susceptible in vitro to EPE (Martins et al., 2002; Kartal et al., 2003). Various antifungals are used in oral candidiasis, however, nystatin is the treatment of choice (Korting, 2003). In this study, all the patients treated with the commercial ethanol propolis extract showed a lesion regression similar to that observed in those patients treated with nystatin. It means that the 20% EPE used, in the therapeutic method assigned in this research is effective in the treatment of the oral candidiasis associated with stomatitis by using prothesis. However, after the treatment using propolis, the patient should change the prothesis to prevent trauma from its bad adjustment and imperfection. The efcacy of EPE in oral candidiasis treatment is of great interest for public health in Brazil. Propolis is cheap and is accessible to the population. Further studies with more signicant patient numbers are necessary for the statistical conrmation of these results.
+, total lesion remission after 7 days; ++, total lesion remission after 15 days.
Acknowledgements
Thanks to Fundao de Amparo Pesquisa do Estado de Minas Gerais (FAPEMIG), BIOBRS Laboratory (Montes Claros, Brazil), CECON (So Paulo, Brazil), Conselho Nacional de Desenvolvimento Cientico e Tecnolgico (CNPq) and PharmaNctar (Belo Horizonte- Brazil). Special thanks to Carlos Antonio da Rocha (technical laboratory work).
Copyright 2005 John Wiley & Sons, Ltd.
Phytother. Res. 19, 652654 (2005)
654
V. R. SANTOS ET AL.
REFERENCES
Aga H, Shibuya T, Sugimoto T, Kurimoto M, Nakajima S. 1994. Isolation and identication of antimicrobial compounds in Brazilian prpolis. Biosci Biotechnol Biochem 58: 945946. Bonhevi JS, Coll FV, Jord RE. 1994. The composition, active components and bacteriostatic activity of propolis in dietetics. J Am Oil Chem Soc 71: 529532. Cicala C, Morelle S, Iorio C, Capasso R, Borelli C, Mascolo N. 2003. Vascular effects of caffeic acid phenethyl ester (CAPE) on isolated rat thoracic aorta. Life Sci 73: 8084. Drago L, Mombelli B, De Vecchi E, Fassina MC, Tocalli L, Gismondo MR. 2000. In vitro antimicrobial activity of propolis dry extract. J Chemother 12: 390395. Kartal M, Yildiz S, Kaya S, Kurucu S, Topcu G. 2003. Antimicrobial activity of propolis samples from to different regions of Anatolia. J Ethnopharmacol 86: 6973. Korting HC. 2003. Fungi overall! Skin and mucosal mycoses and their treatment. Pharm Unserer Zeit 32: 130137. Kujumgiev A, Tsvetkova I, Serkedjieva Yu, Bankova V, Christov R, Popov S. 1999. Antibacterial, antifungal and antiviral activity of propolis of different geographic origin. J Ethnopharmacol 64: 235240. Marcucci MC. 1995. Propolis: Chemical composition, biological properties and therapeutic activity. Apidologie 26: 7681. Marcucci MC, Custodio AR, Ferreira MM, Bankova VS, GarciaViguera C, Bretz WA. 2000. Evaluation of phenolic compounds in Brazilian propolis from different geographic regions. Z Naturforsch [C] 55: 7681. Marcucci MC, Ferreres F, Garcia-Viguera C et al. 2001. Phenolic compounds from Brazilian propolis with pharmacological activities. J Ethnopharmacol 74: 105112. Martins RS, Pereira ESJ, Senna MIB, Mesquita RA, Santos VR. 2002. Effect of commercial ethanol propolis extract on the in vitro growth of Candida albicans collected from HIV-seropositive and HIV-seronegative Br patients with oral candidiasis. J Oral Sci 44: 4148. Valcic S, Montenegro G, Mujica AM et al. 1999. Phytochemical, morphological, and biological investigations of propolis from Central Chile. Z Naturforsch [C] 52: 13451350. Velikova M, Bankova V, Marcucci MC, Tsvetkova I, Kujumgiev A. 2000. Chemical composition and biological activity of propolis from Brazil. Z Naturforsch [C] 55: 785 789.
Copyright 2005 John Wiley & Sons, Ltd.
Phytother. Res. 19, 652654 (2005)
You might also like
- Observasional Studies. Jepsen Et AlDocument5 pagesObservasional Studies. Jepsen Et AlSJ IraaNo ratings yet
- Anti FungiDocument11 pagesAnti FungiSJ IraaNo ratings yet
- 03 Journal 2010 V9-2Document8 pages03 Journal 2010 V9-2SJ IraaNo ratings yet
- Identification of Malassezia SpeciesDocument3 pagesIdentification of Malassezia SpeciesSJ IraaNo ratings yet
- MfLIP1 Gene Encodes Extracellular Lipase in Lipid-Dependent Fungus Malassezia furfurDocument8 pagesMfLIP1 Gene Encodes Extracellular Lipase in Lipid-Dependent Fungus Malassezia furfurSJ IraaNo ratings yet
- Tambahan Skenario4Document1 pageTambahan Skenario4SJ IraaNo ratings yet
- DAPUSDocument4 pagesDAPUSSJ IraaNo ratings yet
- Optimum Extraction Process of Polyphenols From The Bark of Phyllanthus Emblica L. Based On The Response Surface MethodologyDocument8 pagesOptimum Extraction Process of Polyphenols From The Bark of Phyllanthus Emblica L. Based On The Response Surface MethodologySJ IraaNo ratings yet
- P OvaleDocument30 pagesP OvaleSJ IraaNo ratings yet
- Optimum Extraction Process of Polyphenols From The Bark of Phyllanthus Emblica L. Based On The Response Surface MethodologyDocument8 pagesOptimum Extraction Process of Polyphenols From The Bark of Phyllanthus Emblica L. Based On The Response Surface MethodologySJ IraaNo ratings yet
- Synergistic growth inhibitory effects of Phyllanthus emblica and Terminalia bellerica extracts with conventional cytotoxic agents: Doxorubicin and cisplatin against human hepatocellular carcinoma and lung cancer cellsDocument7 pagesSynergistic growth inhibitory effects of Phyllanthus emblica and Terminalia bellerica extracts with conventional cytotoxic agents: Doxorubicin and cisplatin against human hepatocellular carcinoma and lung cancer cellsSJ IraaNo ratings yet
- Abstraksi InggrisDocument1 pageAbstraksi InggrisSJ IraaNo ratings yet
- Antenatal Fetal AssessmentDocument7 pagesAntenatal Fetal AssessmentFitriana Nur RahmawatiNo ratings yet
- 03 Journal 2010 V9-2Document8 pages03 Journal 2010 V9-2SJ IraaNo ratings yet
- 1966 145 859535782 29.mello PDFDocument7 pages1966 145 859535782 29.mello PDFSJ IraaNo ratings yet
- F - 3067 OED Review of Azithromycin Ophthalmic 1 Solution AzaSite For The Trea - PDF - 4148 PDFDocument14 pagesF - 3067 OED Review of Azithromycin Ophthalmic 1 Solution AzaSite For The Trea - PDF - 4148 PDFSJ IraaNo ratings yet
- Antifungal Activity of Commercial Ethanolic and Aqueous Extracts of Brazilian Propolis Against Candida Spp.Document5 pagesAntifungal Activity of Commercial Ethanolic and Aqueous Extracts of Brazilian Propolis Against Candida Spp.SJ IraaNo ratings yet
- Amla Protects Rats from Lead ToxicityDocument1 pageAmla Protects Rats from Lead ToxicitySJ IraaNo ratings yet
- Characteristic Locations of InguinalRegion and Anterior Abdominal Wall Hernias: SonographicAppearances and Identification of Clinical PitfallsDocument9 pagesCharacteristic Locations of InguinalRegion and Anterior Abdominal Wall Hernias: SonographicAppearances and Identification of Clinical PitfallsSJ IraaNo ratings yet
- Screening For Gestational Diabetes MellitusDocument10 pagesScreening For Gestational Diabetes MellitusSJ IraaNo ratings yet
- Characteristic Locations of InguinalRegion and Anterior Abdominal Wall Hernias: SonographicAppearances and Identification of Clinical PitfallsDocument9 pagesCharacteristic Locations of InguinalRegion and Anterior Abdominal Wall Hernias: SonographicAppearances and Identification of Clinical PitfallsSJ IraaNo ratings yet
- Tympanostomy Tubes and Developmental Outcomes at 9 To 11 Years of AgeDocument14 pagesTympanostomy Tubes and Developmental Outcomes at 9 To 11 Years of AgeSJ IraaNo ratings yet
- Potential Effects of Bee Honey and Propolis Against The Toxicity of Ochratoxin A in RatsDocument8 pagesPotential Effects of Bee Honey and Propolis Against The Toxicity of Ochratoxin A in RatsSJ IraaNo ratings yet
- F 3160 OED Clinical Options For The Reduction of Elevated Intraocular Pressure - PDF 4280Document22 pagesF 3160 OED Clinical Options For The Reduction of Elevated Intraocular Pressure - PDF 4280SJ IraaNo ratings yet
- Propolis tincture for mouth ulcersDocument8 pagesPropolis tincture for mouth ulcersSJ IraaNo ratings yet
- Chest Wall Thickness and Needle Thoracocentesis 08Document4 pagesChest Wall Thickness and Needle Thoracocentesis 08SJ IraaNo ratings yet
- Muscular Dystrophy Overview: Genetics and DiagnosisDocument22 pagesMuscular Dystrophy Overview: Genetics and DiagnosisSJ IraaNo ratings yet
- Identification of Phenolics in The Fruit ofDocument7 pagesIdentification of Phenolics in The Fruit ofSJ IraaNo ratings yet
- Antimicrobial PropertiesDocument13 pagesAntimicrobial PropertiesSJ IraaNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- AmikacinDocument4 pagesAmikacinkristineK100% (1)
- Antimicrobial DrugsDocument64 pagesAntimicrobial Drugsdr. khushboo singh100% (1)
- Antifungal PharamcotherapyDocument29 pagesAntifungal Pharamcotherapyrijay2001No ratings yet
- Case Study AscariasisDocument60 pagesCase Study AscariasisRijane Tabonoc OmlangNo ratings yet
- Interactions of Yeasts, MouldsDocument183 pagesInteractions of Yeasts, MouldsAnca NegreanuNo ratings yet
- PHARMACOLOGY Anti Microbial DrugsDocument17 pagesPHARMACOLOGY Anti Microbial DrugsLeilani Sablan100% (2)
- Antifungal AgentsDocument91 pagesAntifungal AgentsSartika NapitupuluNo ratings yet
- Journal Buah Ketapang (Ficus Lyrata)Document5 pagesJournal Buah Ketapang (Ficus Lyrata)MuhammadRifqiAbdurrahmanNo ratings yet
- (500 MG Metronidazole and 100,000 IU Nystatin) Vaginal OvulesDocument22 pages(500 MG Metronidazole and 100,000 IU Nystatin) Vaginal OvulesAngel CoNo ratings yet
- Drug Study Batch 3 - Kristele Marie Joy CuaDocument26 pagesDrug Study Batch 3 - Kristele Marie Joy CuaKristele Marie Joy CuaNo ratings yet
- Clinical Significance of Cyniclomyces Guttulatus in DogsDocument7 pagesClinical Significance of Cyniclomyces Guttulatus in DogsNarvarte Hospital Veterinario de EspecialidadesNo ratings yet
- Review of Topical Antifungals for Otomycosis TreatmentDocument7 pagesReview of Topical Antifungals for Otomycosis TreatmentmedicamedicaNo ratings yet
- Macrorhabdus (Megabacteria) 10 Nov 2013 (2.0)Document10 pagesMacrorhabdus (Megabacteria) 10 Nov 2013 (2.0)Cristina Maria CampeanNo ratings yet
- Balanitis UpdatesDocument22 pagesBalanitis UpdatesUshal VeeriahNo ratings yet
- Efficacy of Nystatin For The Treatment of OralDocument11 pagesEfficacy of Nystatin For The Treatment of OralRegita AyuNo ratings yet
- Fluconazole Versus Nystatin in The Prevention of CandidaDocument25 pagesFluconazole Versus Nystatin in The Prevention of CandidaMutia SesunanNo ratings yet
- Antituberculars, Antifungals, and AntiviralsDocument44 pagesAntituberculars, Antifungals, and Antiviralsmam2017No ratings yet
- Dental Treatment Considerations in The Chemotherapy PatientDocument12 pagesDental Treatment Considerations in The Chemotherapy PatientAdeel TahirNo ratings yet
- Antifungal AgentsDocument37 pagesAntifungal AgentsChandrashekhar UnakalNo ratings yet
- Candidiasis A Fungal Infection Current Challenges and ProgressDocument11 pagesCandidiasis A Fungal Infection Current Challenges and ProgressLau's WorldNo ratings yet
- Nystatin Drug CardDocument1 pageNystatin Drug CardSheri490100% (1)
- FlagystatinDocument18 pagesFlagystatineherlinNo ratings yet
- Hospital Antibiotic Policy: ST Helens and Knowsley Hospitals TrustDocument72 pagesHospital Antibiotic Policy: ST Helens and Knowsley Hospitals TrustDimas RfNo ratings yet
- ANTIJAMURDocument3 pagesANTIJAMURCharlesMahonoNo ratings yet
- Dosage: Route:: Mycobacterium TuberculosisDocument21 pagesDosage: Route:: Mycobacterium TuberculosisLyn ConsingNo ratings yet
- Anti-Fungal Drugs - KatzungDocument2 pagesAnti-Fungal Drugs - Katzungsarguss14100% (2)
- Antifungal Agent PPT PresentationDocument38 pagesAntifungal Agent PPT Presentationdinberu tadesseNo ratings yet
- BREX Pharmacy Review Module 1Document9 pagesBREX Pharmacy Review Module 1Kenneth DayritNo ratings yet
- DecombDocument3 pagesDecombDr.2020No ratings yet
- F8DB F089:Fungal InfectionsDocument6 pagesF8DB F089:Fungal InfectionsPharmacist Ehab HammadNo ratings yet