Professional Documents
Culture Documents
Effect of Menopause On Lipid Profile and Apolipoproteins
Uploaded by
Sabrina Indri WardaniOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Effect of Menopause On Lipid Profile and Apolipoproteins
Uploaded by
Sabrina Indri WardaniCopyright:
Available Formats
AJ M S
(A US National Library of Medicine enlisted journal)
Al Ameen J Med Sci (2011)4(3):221-228
ISSN 0974-1143 CODEN: AAJMBG
ORIGINAL ARTICLE
Effect of Menopause on Lipid Profile and Apolipoproteins
R.K. Swapnali1*, Ravikiran Kisan2 and D.S. Jayaprakash Murthy3
Department of Biochemistry SSIMS, Davangere, Karnataka India, 2Department of Physiology, SSIMS, Davangere, Karnataka, India and 3Department of Biochemistry, JJMMC Davangere, Karnataka, India.
Abstract: Menopause is an estrogen deficient state. Natural menopause confers a threefold increase in Coronary Artery Disease (CAD) risk. This study was conducted to assess the effect of menopause on serum lipid profile and apolipoproteins. About 123 healthy subjects were studied (62 premenopausal and 61 postmenopausal women). Total Cholesterol (TC), Triglycerides (TG) and High Density Lipoprotein (HDL) were estimated by enzymatic method and Apo A-I and Apo B were estimated by immunoturbidimetric method by semi-autoanalyzer. TC, TG, Very Low Density Lipoprotein (VLDL), Low Density Lipoprotein (LDL), Apo B, TC/HDL and Apo B/Apo A-I were increased, whereas HDL and Apo A-I were decreased in postmenopausal women when compared to premenopausal women and were statistically significant (p < 0.001). Apo A-I and HDL cholesterol are antiatherogenic whereas Apo B and LDL cholesterol are atherogenic. The cholesterol content of HDL and LDL as an indicator for risk of CAD may be misleading because the cholesterol content varies with a variety of physiological and pathological conditions but not their protein content. Hence estimation of Apo A-I and Apo B, the protein part of HDL and LDL respectively serves as a more reliable tool in predicting the risk of CAD in postmenopausal women. Key Words: Premenopausal women; Postmenopausal women; Apolipoproteins.
1
Introduction Menopause is the permanent amenorrhea, which lasts atleast for a period of one year due to the cessation of ovarian function [1]. In young women, where estrogen production is high, serum lipids are normal but after menopause, lipid levels are increased and also the increased incidence of Coronary Artery Disease (CAD). This shows the possible relationship among estrogen, normal lipid profile and the relative immunity to CAD [2]. Hence after menopause, risk of atherosclerosis and CAD are more frequent [3]. Natural menopause confers a threefold increase in CAD risk [4]. Currently postmenopausal women account for more than 30% of the female population at risk for CAD in India [5]. Apolipoprotein A-I (Apo A-I) and Apolipoprotein B (Apo B) are protein constituents of HDL and LDL respectively. Apo A-I and HDL are antiatherogenic whereas Apo B and LDL are atherogenic [6]. The present study was conducted to assess the effect of menopause on lipids, lipoproteins and apolipoproteins concentration. It is estimated that, at the turn of this century, more than one third of the female population will be in their postreproductive years compared to about 10% at present and the impact of CAD on womens health management will increase.
2011. Al Ameen Charitable Fund Trust, Bangalore
221
Al Ameen J Med Sci; Volume 4, No.3, 2011
Swapnali RK et al
Although certain forms of CAD can be treated medically or surgically, the most effective means to decrease the impact of CAD on womens health is by modifying the contribution of specific factors that increase the risk of the disease [7]. Material and Methods A total number of 123 subjects were selected from the out-patient department of Bapuji Hospital and Chigateri District General Hospital, Davangere, of which 61 were the healthy postmenopausal women of age 42-75 years with a history of natural menopause (that is, cessation of menstrual period atleast for a period of one year) without any disease and 62 were healthy premenopausal women aged 26-50 years with regular menstruation without any disease. Subjects with cardiovascular disease, diabetes mellitus, hypertension, familial hypertriglyceridemia, history of hysterectomy, oophorectomy, those on exogenous hormone or hormone replacement therapy, intake of lipid lowering drugs or any surgery were excluded from the study. After an overnight fasting of 12-14 hours, about 5 ml of venous blood was drawn under aseptic precaution in a sterile bulb from selected subjects after the informed written consent. Serum was immediately separated by centrifugation and was used for analysis. The serum total cholesterol was estimated by Enzymatic Cholesterol Oxidase (CHOD) / Phenol Aminoantipyrine (PAP) Method, triglyceride by Enzymatic Glycerol Phosphate Oxidase / Phenol Amino Antipyrine, HDL by Enzymatic Cholesterol Oxidase / Phenol Amino Antipyrine (CHOD / PAP) method and serum LDL and VLDL were calculated by Friedewald formula [8]. The serum Apo A-I [9] and Apo B [10] were estimated by Immunoturbidimetric method. Descriptive data were presented as mean SD values. Students unpaired t test was used for comparing the means of two groups. Relationship between variables was measured by Pearsons correlation coefficient. Results According to table-1 the mean values of TC, TG, VLDL and LDL were increased except HDL cholesterol which was decreased in postmenopausal women when compared to premenopausal women and were statistically highly significant (p < 0.001). Apo A-I values were lower and Apo B values were higher in postmenopausal women than in premenopausal women and were statistically significant (p < 0.001). The ratios of TC/HDL and Apo B/Apo A-I were decreased in premenopausal women, compared to postmenopausal women and were statistically significant (p < 0.001).
2011. Al Ameen Charitable Fund Trust, Bangalore
222
Al Ameen J Med Sci; Volume 4, No.3, 2011
Swapnali RK et al
Table-1: Comparison of TC, TG, HDL, VLDL, LDL, APO A-I, B and their ratios in pre and post menopausal women. Subjects Preme nopausal women (n=62) Postmeno pausal women (n=61) Preme nopausal women Vs postmeno pausal women APO-B/ APO-A-I 0.53 0.12 1.49 0.32 19.5 <0.001 223 APO A-I mg/dL APO B mg/dL 68.6 8.6 108.1 13.3 16.1 <0.001 Apo B p- level < 0.01 < 0.01 < 0.01 < 0.01 < 0.01 < 0.01 r- value* + 0.88 + 0.87 - 0.90 + 0.87 + 0.88 + 0.88 p-level < 0.01 < 0.01 < 0.01 < 0.01 < 0.01 < 0.01 TC mg/dL TG mg/dL HDL mg/dL VLDL mg/dL LDL mg/dL TC/ HDL 3.95 1.1 6.9 2.07 10.8 <0.001
Mean SD
152.3 21.6
86.6 19.8
39.7 4.8
16.8 4.0
95.8 22.3
131.3 11.8
Mean SD
207.2 34.0 10.7 <0.001
112.8 21.2 7.1 <0.001
30.9 3.7 11.4 <0.001
22.6 4.2 7.8 <0.001
153.8 33.6 11.3 <0.001
74.1 7.1 32.6 <0.001
It is evident from the table-2 that there was a positive correlation between TC, TG, VLDL, TC / HDL ratio and Apo B and the correlation was statistically significant but there was a negative correlation between HDL and Apo B. Also there was a positive correlation between HDL and Apo A-I. Both the variables were dependent on each other. As the concentration of HDL increases there was simultaneous increase in Apo A-I level and this correlation was statistically significant (p < 0.01).
Table 2: Relationship of Apo A- I and Apo B with other lipid profiles in postmenopausal women Apo A- I r-value* TC TG HDL VLDL LDL TC / HDL - 0.96 - 0.95 + 0.96 - 0.95 - 0.95 - 0.94
*r Pearson Correlation Coefficient
t*
2011. Al Ameen Charitable Fund Trust, Bangalore
Al Ameen J Med Sci; Volume 4, No.3, 2011
Swapnali RK et al
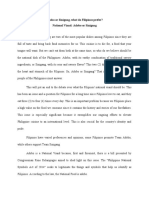
Figure: Lipid profile in premenopausal & post menopausal women
*** p<0.001
Discussion Coronary Artery Disease is the leading cause of death among the postmenopausal women. Indeed postmenopausal women are four to eight times more likely to die of CAD than of any other disease [4]. Blood lipids are an important metabolic feature of the atherosclerotic process in women [11]. The mean age in the postmenopausal women is 56.6 8.0 years and in the premenopausal women is 32.2 5.8 years. The mean age in postmenopausal group is greater than that of premenopausal women. Unavoidably, there is difference in age between both groups of women because it is difficult to design studies that can separate the effects of the normal ageing process from natural menopause [3]. Menopause normally occurs between 45 to 50 years of age [1]. In our study it is evident that the total cholesterol is increased in postmenopausal women due to estrogen deficiency when compared to premenopausal women and is statistically significant (p<0.001) and these findings are in accordance with other studies [3,12-13]. 1% increase in TC is associated with atleast 2% increase in the incidence of CAD and they also showed that TC was 19% (1.0 mmol/L) higher in postmenopausal women compared to premenopausal women [7,14]. In our study when compared to premenopausal women, postmenopausal women are having high TG and was statistically significant (p<0.001). These findings are in accordance with other studies [4,15].
2011. Al Ameen Charitable Fund Trust, Bangalore
224
Al Ameen J Med Sci; Volume 4, No.3, 2011
Swapnali RK et al
In the postmenopausal women, the higher body weight is due to increased fat accumulation and there will be increased release of free fatty acids into the circulation and excessive free fatty acids provides substrate for hepatic triglyceride and triglyceride rich lipoprotein production [16]. According to the study done by Razay Y et al [14], in the postmenopausal women TG was higher by 31% (0.31mmol/L) when compared to premenopausal women. In our study the VLDL was increased in postmenopausal women when compared to premenopausal women and was statistically significant (p<0.001) and these findings are in accordance with other studies [4,13]. In postmenopausal women due to estrogen deficiency, there will be relative enrichment of small VLDL particles with CE which is unclear but could be either due to increased catabolism of VLDL with resulting increased number of VLDL remnant particles or increased activity of Cholesterol Ester Transfer Protein (CETP) or both [7]. These small VLDL particles contain more CE molecules per particle and are highly atherogenic [17]. The VLDL remnants have a high capacity for interacting with arterial smooth muscle cells [18]. In our study when compared to premenopausal women, postmenopausal women were having high levels of LDL and was statistically significant (p<0.001). These findings are in accordance with other studies [3, 19]. Circulating estrogen is a regulator of Lipoprotein Lipase (LPL). LPL catalyzes the hydrolysis of VLDL to form IDL and later LDL. After menopause due to estrogen deficiency, there will be increased plasma LPL and hepatic TG lipase activity causing plasma LDL accumulation and also leads to down-regulation of LDL receptors [12, 10]. The higher the small dense LDL proportion which characterizes the atherogenic shift, higher is the LDL oxidation [12] and these particles are associated with a threefold increase in CAD risk [4]. 1% increase in LDL cholesterol increases the risk of CAD by 2% [20]. In our study it was evident that premenopausal women were having high HDL than postmenopausal women and was statistically significant (p<0.001) and these findings are in accordance with other studies [11,13]. Due to estrogen deficiency, postmenopausal women will have highest activity of postheparin hepatic lipase and enhances the uptake of HDL and also increases the catabolism of HDL thus decreasing plasma HDL concentration [5]. Also in postmenopausal women there is increased LDL accumulation, so more and more HDL gets esterified for the metabolism of those accumulated LDL. Hence postmenopausal women were having lower HDL compared to premenopausal women. For every 10 mg/dL increase in HDL, there is a corresponding 50% decrease in CAD risk [11]. They also showed that, 1% decrease in HDL increases the risk of CAD by 2% - 4.7% [20]. In our study TC / HDL ratio was significantly increased in postmenopausal women when compared to premenopausal women (p<0.001). This result was in agreement with other studies [4, 5, 11, 14]. TC/HDL ratio increases steadily with age and the risk of CAD increases progressively in proportion to TC/HDL ratio. This explains the waning protection for women against CAD and other vascular diseases as the age advances [11]. TC/HDL ratio around 3.5 is optimal and above 5 is dangerous [11]. In our study the postmenopausal women were at higher risk for CAD because the ratio was above the dangerous level. Further they stated that one unit increase in TC / HDL ratio was associated with 49% increase in risk of CAD [5].
2011. Al Ameen Charitable Fund Trust, Bangalore
225
Al Ameen J Med Sci; Volume 4, No.3, 2011
Swapnali RK et al
Our study showed that the concentration of Apo A-I was significantly decreased in postmenopausal women when compared to premenopausal women (p<0.001) and these results are in agreement with other studies [12,18-19]. Apo-A-I is about 75% of the protein component (major protein) of HDL and activates the enzyme LCAT, which catalyses the esterification of cholesterol. Apo A-I interact with a putative HDL receptor and facilitate to remove cholesterol from the peripheral cells to transport it back to liver for excretion into bile as bile acids.[21] Estrogen increases HDL concentration by increasing the production of Apo A-I. Hence after menopause due to estrogen deficiency there will be decrease in plasma Apo A-I and HDL concentration [5]. A study stated that 1% reduction in Apo A-I increases the risk of CAD by 2% [21]. Our study showed that the concentration of Apo B was significantly increased in postmenopausal women when compared to premenopausal women (P<0.001). These results are in agreement with other studies [13,19]. Apolipoprotein B is required for the hepatic secretion of VLDL and Apo B remains associated with the particle during the triglyceride hydrolysis and lipid exchange cascade until its clearance from the circulation as IDL or LDL particle. By measuring Apo B in plasma is roughly equivalent to quantifying the number of Apo B containing lipoproteins secreted by the liver because only one Apo B molecule per particle is secreted and the cholesterol content of Apo B containing lipoproteins may be highly variable [17,22]. Apolipoprotein B is involved in the transportation of LDL cholesterol, which carries cholesterol to the peripheral tissues. In CAD subjects there is increased synthesis of Apo B which delivers the increased plasma cholesterol to macrophages of arterial wall resulting in the formation of atherosclerotic plaque. A study showed that, a 10% decrease in Apo B level was associated with 22% decreased risk of CAD [23]. In our study the Apo B/Apo A-I ratio was increased in postmenopausal women when compared to premenopausal women and was statistically significant (p<0.001). The increased concentration of Apo B and decreased concentration of Apo A-I in postmenopausal women results in increase in the ratio of Apo B/Apo A-I. The results are in agreement with other studies [5,12,19]. Apolipoproteins and their ratios were highly significant in all the age group patients of CAD and kept their discriminating power upto the oldest decade. But the diagnostic validity of lipids and lipoproteins decreases as the age advances [24]. The development of immunoassay techniques has allowed measurement of the protein as well as the lipid portions of lipoproteins. Apo B, the protein part of LDL particle predicts the development of CAD significantly better than the plasma levels of LDL cholesterol [25]. Each of the atherogenic particles in plasma (VLDL, IDL, LDL) contain one molecule of Apo B and therefore plasma Apo B measures the total number of atherogenic particles [6]. Our results indicate that the risk for CAD increases after natural menopause [5]. In comparison to premenopausal women, asymptomatic postmenopausal women showed an increase in atherogenic lipoprotein profile, inflammatory markers and circulating fibronectin coming from the subendothelial space [12]. The most investigated risk factor in postmenopausal women is estrogen deficiency and estrogen replacement therapy emerges as a single most significant factor that can decrease CAD risk in women [7].
2011. Al Ameen Charitable Fund Trust, Bangalore
226
Al Ameen J Med Sci; Volume 4, No.3, 2011
Swapnali RK et al
The estrogen replacement therapy reduces the serum LDL and increases serum HDL in a dose dependent manner [26]. Oral estrogen therapy (0.625 mg conjugated estrogen) decreased the LDL by 10 15% and increased the HDL by about 10 15%, overall it changed 25 50% of lipid profile. So estrogen treatment reduces the CAD risk by 35% [26]. So this implies that in order to modify risks of CAD in older women intervention with regard to lipid status should begin in perimenopausal state [7]. Indian postmenopausal women are at a greater risk of CAD due to genetically low HDL levels. The benefits of hormone replacement therapy may be greater in Indian postmenopausal women, who have substantially higher rates of CAD (three fold) and lower rates of breast cancer (half fold) compared with whites [5].
References 1. 2. Padubidri VG, Daftary SN. Howkins and Bourne Shaws textbook of gynaecology. 13th ed. New Delhi: Elsevier; 2004. p. 56-58. Sultan N, Nawaz M, Sultan A, Fayaz M, Baseer A. Effect of menopause on serum HDLcholesterol level. JAMC 2003; 15(13): (about 3 screens). Available from: http://www.ayubmed.edu.pk/JAMC/PAST/15-3/norin.htm Kalavathi L, Dhruvanarayan HR, Zachariah E. Plasma estradiol and lipid profile in perimenopausal women. Indian J Physiol Pharmacol 1991; 35(4): 260-262. Welty FK. Cardiovascular disease and dyslipidemia in women. Arch Intern Med 2001; 161: 514-522. Arora S, Jain A, Chitra R. Effects of short-term hormone replacement on a atherogenic indices in Indian postmenopausal women. Indian J Clin Biochem 2006; 21(1): 41-47. Miremad S, Sniderman A, Frohlich J. Can measurement of serum apolipoprotein B replace the lipid profile monitoring of patients with lipoprotein disorders? Clin Chem 2002; 48(3): 484-488. Gorodeski GI, Utian WH. Epidemiology and risk factors of cardiovascular disease in postmenopausal women. In: Lobo RA editor. Treatment of the postmenopausal women. 2nd ed. Philadelphia: Lippincott Williams and Wilkins; 1999. p. 331-359. Kannel WB. Metabolic risk factors for coronary heart disease in women: perspective from the Framingham study. Am Heart J 1987; 114(2): 413-419. Marconiva SM, Albers JJ, Henderson O, Hannon WH. International Federation of Clinical Chemistry standardization project for measurements of apolipoproteins A-I and B. Comparability of apolipoprotein A-I values by use of International reference material. Clin Chem 1993; 39(5): 773-781. Wakatsuki A, Sagara Y. Lipoprotein metabolism in postmenopausal and oophorectomized women. Obstet Gynecol 1995 ; 85(4): 523-528. Kannel WB. Metabolic risk factors for coronary heart disease in women: perspective from the Framingham study. Am Heart J 1987; 114(2): 413-419. Muzzio ML, Berg G, Zago V, Basilio F, Sanguinetti S, Lopez G, et al. Circulating small dense LDL, endothelial injuring factors and fibronectin in healthy postmenopausal women. Clin Chim Acta 2007; 381: 157-163. Matthews KA, Meilahn E, Kuller LH, Kelsey SF, Caggiula AW, Wing RR. Menopause and risk factors for coronary heart disease. N Eng J Med 1989; 321(10): 641-646. Razay G, Heaton KW, Bolton CH. Coronary heart disease risk factors in relation to the menopause. Quarterly J Med 1992 ; 85(307-8): 889-896. Hallberg L, Svanborg A. Cholesterol, phospholipids and triglycerides in plasma in 50 year-old women. Acta Med Scand 1967; 181(2): 185-194.
2011. Al Ameen Charitable Fund Trust, Bangalore
3. 4. 5. 6.
7.
8. 9.
10. 11. 12.
13. 14. 15.
227
Al Ameen J Med Sci; Volume 4, No.3, 2011
Swapnali RK et al
16. Tanko LB, Bagger YZ, Qin G, Alexandersen P, Larsen PJ, Christiansen C. Enlarged waist combined with elevated triglycerides is a strong predictor of accelerated atherogenesis and related cardiovascular mortality in postmenopausal women. Circulation 2005; 111: 1883-1890. 17. Tornvall P, Bavenholm P, Landou C, de Faire U, Hamsten A. Relation of plasma levels and composition of apolipoprotein B containing lipoproteins to angiographycially defined coronary artery disease in young patients with myocardial infarction. Circulation 1993; 88(5): 2180-2189. 18. Reardon MF, Nestel PJ, Craig IH, Harper RW. Lipoprotein predictors of the severity of coronary artery disease in men and women. Circulation 1985; 71(5): 881-888. 19. Kwiterovich PO, Coresh J, Smith HH, Bachorik PS, Derby CA, Pearson TA. Comparison of the plasma levels of apolipoproteins B and A-I and other risk factors in men and women with premature coronary artery disease. Am J Cardiol 1992; 69: 1015-1021. 20. Rifai N, Bachorik PS, Allbers JJ. Lipids, lipoproteins and apolipoproeins. In: Burtis CA, Ashwood ER, editors. Tietz fundamental of clinical chemistry. 5th ed. Philadelphia: Saunders Co; 2001. p. 463-493. 21. Sigurdsson G, Baldursdottir A, Sigvaldason H, Agnarsson U, Thorgeirsson G, Sigfusson N. Predictive value of apolipoproteins in a prospective survey of coronary artery disease in men. Am J Cardiol 1992; 69: 1251-1254. 22. Regnstrom J, Nilsson J, Tornvall P, Landou C, Hamsten A. Susceptibility to low-density lipoprotein oxidation and coronary atherosclerosis in man. Lancet 1992; 339:1183-1186. 23. Wald NJ, Law M, Watt HC, Wu T, Bailey A, Johnson AM, et al. Apolipoproteins and ischemic heart disease: implications for screening. Lancet 1994; 343: 75-79. 24. Avogard P, Bon GB, Cazzolato G, Quinci GB. Are apolipoproteins better discriminators than lipids for atherosclerosis? Lancet 1979; 901-903. 25. Sinderman AD, Wolfson C, Teng B, Franklin FA, Bachorik PS, Kwiterovich PO. Association of hyperapobetalipoproteinemia with endogenous hypertriglyceridemia and atherosclerosis. Ann Intern Med 1982; 97(6): 833-839. 26. Grady D, Rubin SM, Petitti DB, Fox CS, Black D, Ettinger B, et al. Hormone therapy to prevent disease and prolong life in postmenopausal women. Ann Intern Med 1992 15; 117(12): 1016-1037.
*All correspondences to: Dr. Swapnali R.K, Assistant Professor, Department of Biochemistry, SS Institute of Medical Sciences and Research Centre, NH-4 Bypass road, Davangere, Karnataka, India. Email: dr.swapnaliravikiran@gmail.com
2011. Al Ameen Charitable Fund Trust, Bangalore
228
You might also like
- Allaergic Conjunctivitis PathophysiologyDocument25 pagesAllaergic Conjunctivitis PathophysiologyRabiu Hassan MusaNo ratings yet
- DR Jacqui Newest Journal I1552-5783-56-13-7784-9Document10 pagesDR Jacqui Newest Journal I1552-5783-56-13-7784-9Sabrina Indri WardaniNo ratings yet
- Evaluate Clinical Prediction RuleDocument5 pagesEvaluate Clinical Prediction RuleTiaz DiniutamiNo ratings yet
- Calcium Flux-Independent NMDA Receptor Activity is Required for Aβ Oligomer-Induced Synaptic LossDocument9 pagesCalcium Flux-Independent NMDA Receptor Activity is Required for Aβ Oligomer-Induced Synaptic LossSabrina Indri WardaniNo ratings yet
- Improving Bioscience Research Reporting - The ARRIVE Guidelines For Reporting Animal Research PDFDocument5 pagesImproving Bioscience Research Reporting - The ARRIVE Guidelines For Reporting Animal Research PDFSabrina Indri WardaniNo ratings yet
- Focus On Cell Cycle and DNA DamageDocument1 pageFocus On Cell Cycle and DNA DamageSabrina Indri WardaniNo ratings yet
- The Mitotic Spindle Is Chiral Due To Torques Within Microtubule BundlesDocument10 pagesThe Mitotic Spindle Is Chiral Due To Torques Within Microtubule BundlesSabrina Indri WardaniNo ratings yet
- A Minimally Invasive Technique For Serial Intraosseous Perfusion Measurements Using Laser Doppler FlowmetryDocument6 pagesA Minimally Invasive Technique For Serial Intraosseous Perfusion Measurements Using Laser Doppler FlowmetrySabrina Indri WardaniNo ratings yet
- A Review of Molecular Mechanisms of The Anti-LeukemicDocument20 pagesA Review of Molecular Mechanisms of The Anti-LeukemicSabrina Indri WardaniNo ratings yet
- The Cell CycleDocument4 pagesThe Cell CycleSabrina Indri WardaniNo ratings yet
- A Detailed Phenotypic Description of Autosomal Dominant Cone Dystrophy Due To A de Novo Mutation in The GUCY2D GeneDocument7 pagesA Detailed Phenotypic Description of Autosomal Dominant Cone Dystrophy Due To A de Novo Mutation in The GUCY2D GeneSabrina Indri WardaniNo ratings yet
- A Mutation in (GUCA1A) in An AD Cone Dystrophy Pedigree Mapping To A New Locus On Chrom 6p21-1 PDFDocument5 pagesA Mutation in (GUCA1A) in An AD Cone Dystrophy Pedigree Mapping To A New Locus On Chrom 6p21-1 PDFSabrina Indri WardaniNo ratings yet
- Tumor of CNS and Peripheral Nerve (DR - Betty)Document22 pagesTumor of CNS and Peripheral Nerve (DR - Betty)Sabrina Indri WardaniNo ratings yet
- Cephalopod Neural NetworksDocument12 pagesCephalopod Neural NetworksSabrina Indri WardaniNo ratings yet
- Indonesia Beyond 2015 PDFDocument19 pagesIndonesia Beyond 2015 PDFSabrina Indri WardaniNo ratings yet
- Antimicrobial Guideline 2009 2010Document78 pagesAntimicrobial Guideline 2009 2010Lalalala Gabriella KristianiNo ratings yet
- Functional Roles of Bestrophins in Ocular EpitheliaDocument21 pagesFunctional Roles of Bestrophins in Ocular EpitheliaSabrina Indri WardaniNo ratings yet
- Public Acceptance and Willingness-To-Pay For A FutureDocument11 pagesPublic Acceptance and Willingness-To-Pay For A FutureRainer Danny Poluan MamahitNo ratings yet
- Jadwal Jaga IpdDocument4 pagesJadwal Jaga IpdSabrina Indri WardaniNo ratings yet
- Joint DislocationsDocument64 pagesJoint DislocationsSabrina Indri WardaniNo ratings yet
- Bone Tumors: Department of Pathology Anatomy Universitas PadjadjaranDocument28 pagesBone Tumors: Department of Pathology Anatomy Universitas PadjadjaranSabrina Indri WardaniNo ratings yet
- Leta Asdew Da Asdaw DadaDocument2 pagesLeta Asdew Da Asdaw DadaSabrina Indri WardaniNo ratings yet
- Confounding and Validity 2009Document32 pagesConfounding and Validity 2009Sabrina Indri WardaniNo ratings yet
- Jadwal Jaga IpdDocument4 pagesJadwal Jaga IpdSabrina Indri WardaniNo ratings yet
- CA CervixDocument43 pagesCA CervixSabrina Indri WardaniNo ratings yet
- Anaerobic Bacteria: Dept. of Microbiology Medical Faculty, Padjadjaran UniversityDocument52 pagesAnaerobic Bacteria: Dept. of Microbiology Medical Faculty, Padjadjaran UniversitySabrina Indri WardaniNo ratings yet
- Thyroid Disease AlgorithmsDocument29 pagesThyroid Disease AlgorithmsGoh Chong Aik100% (1)
- Mental Disorder and Related Key Symptoms (DR - Tuti W)Document45 pagesMental Disorder and Related Key Symptoms (DR - Tuti W)Sabrina Indri WardaniNo ratings yet
- Signal Direction DendritesDocument12 pagesSignal Direction DendritesSabrina Indri WardaniNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- 2020 2021 Suplementary Admission ListDocument165 pages2020 2021 Suplementary Admission ListBarry AllenNo ratings yet
- Module 13 PhatfitDocument5 pagesModule 13 PhatfitMark Anthony RabyNo ratings yet
- MPDFDocument38 pagesMPDFEmerlyn AtanacioNo ratings yet
- The High Fibre NutriBullet RecipeDocument223 pagesThe High Fibre NutriBullet RecipeAvram Lucia AlexandraNo ratings yet
- ATIP N-12 Final Information Transfer (1) - 1Document164 pagesATIP N-12 Final Information Transfer (1) - 1tessavanderhartNo ratings yet
- TEACHING PLAN DiarrheaDocument2 pagesTEACHING PLAN DiarrheashanilaNo ratings yet
- Adobo or SinigangDocument3 pagesAdobo or SinigangJosephine Anne Piguerra0% (1)
- Food Additives PPT 1416wfcfDocument15 pagesFood Additives PPT 1416wfcfRosita C.CayananNo ratings yet
- Global Nutrition Report 2016Document180 pagesGlobal Nutrition Report 2016IFPRINo ratings yet
- Best Restaurants in Copenhagen - Google SearchDocument1 pageBest Restaurants in Copenhagen - Google Searchlelo1420No ratings yet
- Indian Five Year Plans 1 - 11 (Agriculture Sector Only)Document179 pagesIndian Five Year Plans 1 - 11 (Agriculture Sector Only)Suman ChattopadhyayNo ratings yet
- Altered Nutrition Nursing DiagnosisDocument4 pagesAltered Nutrition Nursing DiagnosisAndrea BroccoliNo ratings yet
- Nutrition in DermatologyDocument46 pagesNutrition in DermatologyRahul KirkNo ratings yet
- Hors D' OeuvresDocument23 pagesHors D' OeuvresMariaChristina DabuNo ratings yet
- Final MNT Ostomy 1Document11 pagesFinal MNT Ostomy 1api-366154535100% (1)
- Product Knowledge PHDocument43 pagesProduct Knowledge PHapi-23450006275% (4)
- Is Heavy Cream The Same As Heavy Whipping Cream?Document7 pagesIs Heavy Cream The Same As Heavy Whipping Cream?Trâm NguyễnNo ratings yet
- I Cut My Body Fat Percentage in Half With a High-Protein DietDocument10 pagesI Cut My Body Fat Percentage in Half With a High-Protein Dietpang sai siong pang sai siongNo ratings yet
- Citron Jaune Cap FruitDocument2 pagesCitron Jaune Cap FruitfgilaNo ratings yet
- Phosphate and Calcium Metablolism, KMUD, 2012Document11 pagesPhosphate and Calcium Metablolism, KMUD, 2012wxcvbnnbvcxwNo ratings yet
- Healthy Food Guide - August 2016Document100 pagesHealthy Food Guide - August 2016YuliiaNo ratings yet
- Why Practitioners in Development Should Integrate Nutrition: United Nations System Standing Committee On NutritionDocument43 pagesWhy Practitioners in Development Should Integrate Nutrition: United Nations System Standing Committee On NutritionadindaNo ratings yet
- Nu Skin Anti-Aging Science Published Articles 2009-2016Document14 pagesNu Skin Anti-Aging Science Published Articles 2009-2016Uditia Alham SaktiNo ratings yet
- Lite N Easy Lunch FavouritesDocument1 pageLite N Easy Lunch FavouritesClare EdwardsNo ratings yet
- Liquid Flavour - Oil SolubleDocument1 pageLiquid Flavour - Oil SolubleAshwin LalaNo ratings yet
- Nutridiet-Enteral and Parenteral FeedingDocument3 pagesNutridiet-Enteral and Parenteral FeedingBSN 1-N CASTRO, RicciNo ratings yet
- Diagram and TablesDocument9 pagesDiagram and TablesPatricia Denise OrquiaNo ratings yet
- Integrated Metabolic Control of Food Intake: Mark I. Friedman, Michael G. Tordoff and Israel RamirezDocument5 pagesIntegrated Metabolic Control of Food Intake: Mark I. Friedman, Michael G. Tordoff and Israel RamirezsyliusNo ratings yet
- Room Service ClearingDocument4 pagesRoom Service Clearingoliver fabonNo ratings yet
- Magical Diet PlanDocument6 pagesMagical Diet PlanManish KumarNo ratings yet