Professional Documents
Culture Documents
Microsoft CHH S
Uploaded by
Joe CuraOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Microsoft CHH S
Uploaded by
Joe CuraCopyright:
Available Formats
MICROSOFT CONNECTED HEALTH AND HUMAN SERVICES FRAMEWORK
TRANSFORMING THE MANAGEMENT AND DELIVERY OF HEALTH AND HUMAN SERVICES
MICROSOFT PUBLIC SECTOR WHITE PAPER JUNE 2012
TRANSFORMING THE MANAGEMENT AND DELIVERY OF HEALTH AND HUMAN SERVICES
Contents
Executive summary ................................................................................................................................................................................ 1 Welcome to Connected HHS ............................................................................................................................................................. 3 Why service mattersfor IT .......................................................................................................................................................... 4 A new model for the business and technology of Connected HHS.................................................................................. 5 Looking at Connected HHS for care coordination ....................................................................................................................... 6 Ideas for care coordination ............................................................................................................................................................ 7 Modernizing systems for the HIX era ............................................................................................................................................... 8 Ideas for modernizing ...................................................................................................................................................................10 Shared services: an overview of Medicaid today ........................................................................................................................11 Ideas for Medicaid systems ..........................................................................................................................................................12 The architecture of coordination .....................................................................................................................................................13 Core infrastructure ..........................................................................................................................................................................13 Connected HHS enterprise service bus ....................................................................................................................................14 Shared services layer .....................................................................................................................................................................15 Agency applications layer.............................................................................................................................................................15 Always-on services in the cloud .................................................................................................................................................15 Getting started: your roadmap forward ........................................................................................................................................16 A roadmap for shared services...................................................................................................................................................16 Manage change: the new governance.....................................................................................................................................17 Microsoft and HHS ...............................................................................................................................................................................18 Connected HHS technology from Microsoft ..........................................................................................................................19
List of tables
Table 1. SOA at a glance: benefits of a Connected HHS environment ..................................................................................................... 4 Table 2. Phased implementation of a Connected HHS environment........................................................................................................ 5 Table 3. Ways to use CRM in a Connected HHS environment ................................................................................................................... 6 Table 4. High-level HIX architecture based on a Connected HHS environment .................................................................................... 9 Table 5. Microsoft products and solutions ................................................................................................................................................... 19
2012 Microsoft Corporation. All rights reserved. This document is provided "as-is." Information and views expressed in this document, including URL and other Internet website references, may change without notice. You bear the risk of using it. This document does not provide you with any legal rights to any intellectual property in any Microsoft product. You may copy and use this document for your internal, reference purposes.
ii
TRANSFORMING THE MANAGEMENT AND DELIVERY OF HEALTH AND HUMAN SERVICES
EXECUTIVE SUMMARY
From Medicaid to children's services to public safety, state and local agencies provide vital health and human services (HHS), typically each with its own information technology (IT) systems. With changes in policy and funding models, your organization has the opportunity to modernize systems so you can coordinate care and connect services across programs in ways that produce better outcomesfor the people you serve and for your agency.
Government, nongovernment, and nonprofit HHS organizations and their partners strive to work together and to deliver exceptional services, despite the fact that many operate in relative isolation, without the ability to easily share information and to coordinate services. State and local agencies and partners often rely on legacy IT systems that arose in isolation over time in response to program-specific needs, independent funding vehicles, and different policy drivers. Citizens are now served by multiple agencies spanning functions such as behavioral health, family services, employment programs, courts, and education. Given lean budgets and legacy IT investments, how can your organization move toward the promise of a simpler, connected future? The past decade of increasingly connected systems of care points the way to innovation, while changing requirements, such as health insurance exchanges (HIXs), are driving rapid change. New models of improved access, quality, and efficiency support the proactive strategies you need to innovate in HHS deliveryfor example, the rising use of electronic records, relatively inexpensive data warehousing options, and the ability to bridge diverse operating environments. Together, these changes can help you devise more coordinated, interconnected, and cost-effective systems of care that enhance outcomes. Innovators such as The Childrens Trust, Health Choice Network, MiamiDade County Public Schools, and Ready Schools Miami demonstrate the leading edge of change. Their information exchange may revolutionize the delivery of health, education, and social services for children from birth through entry into the workforce. Called Childrens Health Education and Economic Resource (CHEER), the exchange will enable programs to coordinate the delivery of services and benefits to children and measure their impact.
ii i
TRANSFORMING THE MANAGEMENT AND DELIVERY OF HEALTH AND HUMAN SERVICES
CHEER is just one example of something we at Microsoft call Connected Health and Human Services, a vision and a technology framework for making the most of IT in the service of people. Rather than an all-or-nothing approach to IT, organizations are using the Connected HHS Framework to evolve over time. Without embarking on a costly rip-andreplace project, your agency can make improvements incrementally and can share business and IT services across groupsand start benefitting from new avenues of funding. Through the Connected HHS Framework and platform, your agency or program can begin sharing services and information with others in a beneficial exchange that helps support coordinated care models, deliver cost savings, respond to a changing regulatory environment, and can ultimately improve health and services.
TRANSFORMING THE MANAGEMENT AND DELIVERY OF HEALTH AND HUMAN SERVICES
WELCOME TO CONNECTED HHS
New coordinated care models ask HHS agencies to work together and help connect people to services more efficiently. Yet many agencies find themselves mired in workflows that sprang from last-generation software. With Connected HHS technologies and practices, you can begin to bridge the gaps and move on.
In the past, federal and state categorical funding requirements effectively dictated separate infrastructures and organizations. For many years, IT systems supported only limited, if any, coordination across programs. Dating back to the 1980s, agencies were tethered to a legacy of large, disconnected transfer systems that took years to build, were outdated at implementation, and could not interoperate with one another. In the past several years, as technology has rapidly evolved, policymakers have begun to endorse the operating models that support a vision of shared services. These architectural guidelines recognize the value of a serviceoriented approach to IT, in which technology components can be reused across organizations and programs that have similar business processes. By sharing services, agencies can reduce the cost and complexity of both acquiring and supporting business applications. Connected HHS is the model and the technology that enable you to shift from the disconnected systems of care of the past to the coordinated systems of care needed today and in the future. With this approach, your organization can begin to: Connect information. When you bring systems, processes, and people together across public health and social services organizations, partners, and citizens, you can free the data that is locked in existing systems. Promote collaboration. When people can work together easilywhether through better program or case management, coordinated workflows, or information accesseveryone wins. Support decisions. The right information in the right hands at the right time unlocks insights. Business intelligence (BI) helps leaders act decisively on critical issues.
3 steps to Connected HHS
On the road to Connected HHS, you can start with the systems you already have. Then, you need a vision of where you want to go and a list of the partners to connect to. The journey takes three steps: 1. Connect. Get systems talking to one another. For that, you need to connect disparate systems and integration services that enable databases to exchange records freely. That way, you have all the relevant information you need about a clientfor example, Samand you know you have the right Sam. 2. Analyze. Find the details you need based on queries of accurate data. For example, you can find at-risk populations or see all the services Sam is receiving. 3. Coordinate care. Collaborate with caregivers, case workers, care recipients, and other stakeholders. With a click, you can be connected through email, instant messaging (IM), the phone, a website, or a common workflow.
TRANSFORMING THE MANAGEMENT AND DELIVERY OF HEALTH AND HUMAN SERVICES
Why service mattersfor IT
Connected HHS is a technology and a roadmap for transforming HHS delivery using a service-oriented architecture (SOA) designed to work whenever possible with familiar Microsoft technologies that many agencies already have. Your organization has the choice to build, deploy, and manage solutions in the way that works beston your premises, in the cloud, or in a hybrid approachusing SOA and industry standards. A Connected HHS approach based on SOA works. For example, in 2004, the Medicaid Information Technology Architecture (MITA) framework from the Centers for Medicare and Medicaid Services (CMS) advocated a business and technology architecture in which modular components can be reused efficiently across HHS agencies, and it provided a path for agencies to modernize their IT systems. The Enterprise Architecture Committee of the National Association of State Chief Information Officers (NASCIO) endorses MITA-like IT concepts and principles for connecting systems, as does the Federal Enterprise Architecture (FEA) project sponsored by the Federal Office of Management and Budget (OMB). Furthermore, to share information among systems, the National Information Exchange Model (NIEM) was created. Also endorsed by NASCIO, NIEM provides a common vocabulary for information-sharing across government lines of business. Taken together, these guidelines make it clear why SOA matters and how a Connected HHS platform benefits service organizations. You could say that SOA gives power to the people by giving them access to information that helps them make decisions about care and services. (See Table 1.) Table 1. SOA at a glance: benefits of a Connected HHS environment
Who Case workers Decisionmakers Benefits Workflow solutions give case workers relief from the burden of redundant administrative reporting processes and repetitive intake processes that get in the way of service delivery. BI solutions help managers focus on problem-solving based on accurate metrics and enhanced analysis. Results can be seen quicklyeven within an executives tenure. Solutions for coordination bring agencies and programs together so they can focus on common business processes and target services to at-risk populations, such as children or the elderly. The right services get delivered at the right time to the right people, helping to reduce administrative overhead and risk. Through web-based solutions and self-help tools, clients become more independent. For example, people can log on to web-based information kiosks or portals and then determine eligibility requirements or review their case status.
iii
Agencies
Citizens
TRANSFORMING THE MANAGEMENT AND DELIVERY OF HEALTH AND HUMAN SERVICES
A new model for the business and technology of Connected HHS
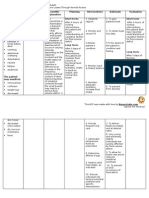
How do you get started? Think sharing. Shared service initiatives drive for improvements through specific tactics, such as care coordination, case management, better business analytics, streamlined communications, data integration, and relationship management. Connected HHS technology can help you meet the needs of these new care models, but you must also consider how shared services affect your business processes. The Connected HHS architecture is designed for incremental deployment, enabling your agency to take a three-phased approach to implementation. (See Table 2.) Whether you implement all three phases together or over time, the goal is to deliver early successes that galvanize future efforts. Table 2. Phased implementation of a Connected HHS environment
Phase Goal Description Select and deploy foundation technologies that use SOA, because they support the standard protocols and interfaces needed for cross-agency collaboration, information access, and process orchestration. Connect disparate systems and information silos. The Connected HHS enterprise service bus is the key to providing people-centric views of data and to supporting performance management across agencies. Develop HHS-specific applications for common functions, such as intake, financial payments, or eligibility.
A solution for service delivery
Nonprofit Aspiranet delivers services to more than 10,000 California children and families a year. It is imperative for them to carefully coordinate service delivery and to keep meticulous records to remain compliant with regulations. They deployed a solution based on Microsoft SharePoint technologies to help meet their need for case worker collaboration and enhanced compliance. The solution helped them streamline business processes so that they could enhance the services they deliver to communities.iv
Affordable email for HHS
Since consolidating its HHS agencies, Texas needed a long-term solution for also consolidating their communications. The Texas Health and Human Services Commission (HHSC) was finally able to link five HHS agencies, representing 55,000 state employees, with a single email system. They chose Microsoft Office 365, a cloud-hosted service. Office 365 includes around-the-clock support and disaster recovery services, two features HHSC required in a new email platform.v
Build the foundation.
Connect the silos.
Use shared services.
TRANSFORMING THE MANAGEMENT AND DELIVERY OF HEALTH AND HUMAN SERVICES
LOOKING AT CONNECTED HHS FOR CARE COORDINATION
What do coordination of care models, e-health initiatives, child welfare services, and behavioral health programs have in common? People. Coordinated care models ask HHS organizations to share common data, information, and processes. Connected HHS helps you bring people, processes, and systems together.
Organizations are using the new care coordination models to reveal areas where shared services can help them to streamline and cut costs. The main point of intersection for many agencies, departments, and programs is people: the citizens, clients, or patients they serve. When health and social services are fragmented, the experience can seem like a tangle of complex, impersonal, and inefficient interactions between caregivers and recipients. The new coordinated care models cross traditional organizational boundaries and help caregivers establish ongoing relationships with colleagues, clients, partners, and patients. For this reason, many are turning to citizen relationship management (CRM) as the foundation of their Connected HHS environment. Whether you work in a clinical setting or in a social services organization, CRM is a strategyand technologythat can help you achieve efficient workflows and improved outcomes of coordinated care. As part of a Connected HHS platform, CRM gives your organization a way to manage relationships based on the needs of the people you serve. For example, a social worker can use CRM tools to view all the services being delivered to an individual or family no matter who provided those services or when they provided them. From there, it can be much easier to coordinate benefits, avoid duplication of effort, and get better results. (See Table 3.) Table 3. Ways to use CRM in a Connected HHS environment
Area Benefits Coordinate care across the continuum of serviceswhether primary care, lab services, vision, dental, or behavioral health counselingto help improve outcomes. Manage and schedule ongoing communications for proactive, long-term care and patient follow-up. Analyze and improve processes so you can track complex workflows, become more efficient, and help boost patient satisfaction. Coordinate benefits for a family, and track all the services they receive from different programs. Get up-to-date client information in combination with rich demographic data from multiple sourcesall in one view. Manage more tasks across functions, such as intake, eligibility, and enrollment, to maximize your relationships with other departments, agencies, and partners.
HEALTH
HUMAN SERVICES
TRANSFORMING THE MANAGEMENT AND DELIVERY OF HEALTH AND HUMAN SERVICES
Ideas for care coordination
Connected HHS architectures support care coordination solutions, which might look like a mobile application that a case worker can use while out of the office, an automated process that replaces tedious manual procedures, or something else. Consider these ideas for enhancing care coordination: Streamline administration. Take key tasks, such as provider management or benefits management, or joint workflows, such as tracking, alerting, and e-forms, and look for ways to implement a common interface across the groups that use similar processes. Or integrate common administrative functions, such as scheduling, payments, or claims. For example, to provide benefits for community college students, Single Stop USA created the Benefits Enrollment Network (BEN) using Connected HHS technologies. Existing IT silos were connected, enabling information-sharing across multiple systems with identity security. Thanks to BEN, workers can coordinate benefits and provide critical tax preparation assistance; benefit screening and eligibility for federal, state, and local programs; and even legal assistance. Preliminary data from select sites indicates an improvement in semester-to-semester retention rates of students who received Single Stop services.
vi
Ease case management. Look for ways to improve forms and records management so case workers can spend less time on data entry and manual reporting and more time helping clients. Help boost workflow, too, by offering workers smartphone applications or automated workflow tools. For example, employees gain mobility when they can record data in the field using everyday software, such as Microsoft Outlook. Enhance communications and public safety. Extend care coordination models to systems for public safety. For example, the Wisconsin Health Information Exchange (WHIE) aggregates real-time data across more than 142 hospitals and 120 clinics, plus claims information from the state, primarily for use by participating emergency departments. However, by depersonalizing the records, they can make that information available to public health organizations, which use it to help support their public health surveillance activities.
vii
TRANSFORMING THE MANAGEMENT AND DELIVERY OF HEALTH AND HUMAN SERVICES
MODERNIZING SYSTEMS FOR THE HIX ERA
HIX requirements are driving IT modernization efforts for many state officials. The right solution must help you integrate multiple aspects of health insurance deliveryincluding plan enrollment, privacy, consumer portals, eligibility determinations, financial services, and program administration.
Although a HIX is often compared to an online travel site, with its onetime purchasing transactions, the comparison is inadequate. States must now assume significantly more complex, ongoing administrative workflowsall while managing numerous regulatory changes throughout the year. To do that, your agency needs flexible IT components that support interoperable exchanges in addition to applications that enable enrollment, assess eligibility, deliver business intelligence, and support case coordination. An end-to-end HIX solution based on the Connected HHS Framework can help you achieve compliance and keep costs down while adapting to changing regulations and technology approaches. For example, one large, private Medicare insurance exchange is using Connected HHS technologies to extend its services in support of HIX requirements. They plan to provide plan-comparison tools and to add enrollment and call center functionality.
viii
HIX in Utah
Utah Health Exchange was one of the first operational state health insurance exchanges in the country. To meet the requirements of their states health system reform legislation, the state Office of Consumer Health Services created an Internet portal, the Utah Health Exchange. It connects consumers to the information they need to make informed health care choices and, in the case of health insurance, to execute that choice electronically.ix The Utah Health Exchange is administered by Microsoft partner bswift, which provides enrollment and administrative services through Connected HHS technologies, including Microsoft SQL Server and the Microsoft .NET Framework. Through this flexible, familiar platform, state administrators are freed to focus on helping Utahs citizens make the best choice in a health plan.x
With its infrastructure based on SOA components, the Connected HHS Framework delivers a consistent architecture that connects internal and external systems so that you can: Accommodate the many aspects of health insurance delivery. Get the most out of your existing IT systems. Connect existing systems to new technology and data from other agencies and the private sector. Combine all of the components into an integrated, end-to-end solution. Expand into health areas not traditionally administered by state agencies, such as comparing health plans or collecting premiums.
TRANSFORMING THE MANAGEMENT AND DELIVERY OF HEALTH AND HUMAN SERVICES
With the Connected HHS approach to HIX, state agencies can assess a single offering and a well-known set of interoperable technology productsa simpler task than evaluating numerous solutions from various firms to find something that works well with government policies and existing IT infrastructures. In this architecture, back-end systems help states to handle eligibility and enrollment, while front-end portals provide access to resources for consumers. In addition, integration with cloud services enables insurers to handle fluctuating volumes of queries, payment deductions, and processing. (See Table 4.) Table 4. High-level HIX architecture based on a Connected HHS environment CONSUMER PORTAL
Plan tools: Presentation Comparison Enrollment
Eligibility determination User interfaces
Financial services Subsidies Premium pooling
Customer care Call center
EXCHANGE ADMINISTRATION, OPERATIONS, COMPLIANCE, AND TRANSPARENCY MICROSOFT CONNECTED HHS FRAMEWORK AND PLATFORM
Another benefit of the Connected HHS approach to HIX is the ease with which business intelligence can be provided to decision-makers and key stakeholders. By providing healthcare payers with analytics tools to measure health outcomes, the HIX solution can help reduce costs. For example, state administrators can use the analytics capabilities to search demographic data so they can research plans for children, senior citizens, or other groups.
TRANSFORMING THE MANAGEMENT AND DELIVERY OF HEALTH AND HUMAN SERVICES
Ideas for modernizing
Connected HHS solutions support IT modernization initiatives and help bring organizations together with up-to-date capabilities, such as access to real-time information and collaboration tools. Consider the following possibilities for your organization. Get digital. If electronic case files are not part of your institutions vocabulary yet, they should be. By digitizing health and human services data, your organization can begin exchanging electronic records easily and in a highly secure manner across organizational boundaries. Your agency can also create business intelligence solutions that give employees access to accurate, up-to-date information. Build a bus. Bridge disparate legacy systems with a Connected HHS enterprise service bus, which enables you to connect fragmented parts of your services ecosystem. For example, Arizona Department of Health Services adopted the Partner Healthcare Electronic Data Exchange (PHEDEX) to meet the federal requirement for state health departments to support interoperable information exchange between public health partners. PHEDEX organizes exchanges among diverse applications and data types while ensuring that transactions are audited and backed up.
xi
Put business intelligence to work. Empower decision-makers with analytics tools that provide big picture data. Web dashboards can turn raw data into visually appealing charts and graphs. For example, analysts can monitor claims data more effectively to prevent fraud, administrators gain insight from financial data that can help achieve cost savings, and managers can visualize demographic and mapping information that helps them serve key populations better. Automate compliance and reporting. Help reduce report-processing time with an automated solution based on your business intelligence. For example, Boulder County, Colorado, had no way to understand the impact of its services on the 294,000 individuals it served, and reporting requirements were burdensome and inconsistent across the more than 100 local agencies and organizations involved. To enhance program efficiency and to improve cross-agency coordination, the county worked with Microsoft Gold Certified Partner Social Solutions to deploy Efforts to Outcomes (ETO) software, a community-based, collaborative social services solution. ETO not only helped the county dramatically reduce wait times for participants but also enabled it to measure services overlap to help improve efficiency, protect against abuses of the system, measure the impact of its various agencies, and track participant progress toward self-sufficiency on a benchmarked spectrum.
xii
10
TRANSFORMING THE MANAGEMENT AND DELIVERY OF HEALTH AND HUMAN SERVICES
SHARED SERVICES: AN OVERVIEW OF MEDICAID TODAY
The ripple effect of federal policy reform opens new doors for state Medicaid programs. Flexible Connected HHS solutions can help you meet the latest mandates for program modernization and interoperable systems of care.
Health reform is in the spotlight, thanks to the Affordable Care Act and the Health Information Technology for Economic and Clinical Health Act (HITECH Act). Nearly $25 billion dollars is at stake from various federal grants, stimulus funds, and incentive payments from the CMS, Health Resources Services Administration (HRSA), and the Office of the National Coordinator for Health Information Technology (ONC). Now its up to state Medicaid programs to try to keep up with increasing healthcare costs and expanding populations. Fortunately, technology has become more flexible and mature since the days of the Medicaid Management Information Systems (MMIS). The current legacy of Medicaid policies and MMIS are based on the fee-forservice model, which has been the norm for decades and which was designed simply to pay claims. Yet as states shift to managed carein which commercial payers become accountable care organizations for the Medicaid populationsstates will benefit from pay-forperformance models, in which providers are held accountable for improved patient outcomes. For this shift to occur, the payers who manage the care of their Medicaid members must have robust information systems capable of integration with health information exchanges (HIEs). Only then can organizations gain seamless access to members medical records. To fulfill the promise of health reform goalsimproved outcomes plus more efficient, cost-effective service deliveryhealth information must flow freely. An MMIS solution based on the Connected HHS Framework makes that possible for payers and providers alike by providing the rich technologies and business services they need to meet the challenges of modern health IT.
Connected HHS benefits for Medicaid
Make use of existing infrastructure. Simplify and speed administrative
processes.
Preserve the organizational
integrity of caregivers and agencies.
Help enhance service outcomes. Provide security-enhanced, role-
based access to information.
Deliver improvements in access
and efficiencies.
Provide better analytics.
11
TRANSFORMING THE MANAGEMENT AND DELIVERY OF HEALTH AND HUMAN SERVICES
Ideas for Medicaid systems
MMIS solutions based on Connected HHS components can help you comply with MITA standards by integrating your existing, agencyshared services with new services. Consider the following possibilities: Expedite access to services. Eliminate complex, redundant intake and eligibility systems, which can discourage individuals and families from seeking care or finding necessary resources. Portals with webbased forms offer a simple solution for easing access and reducing duplication. Assess where data can be shared. Start streamlining eligibility determination across programs by using a solution that passes client information from one system to anothersuch as Temporary Assistance for Needy Families (TANF) to Supplemental Nutrition Assistance Program (SNAP). Manage identities. Improve data quality while resolving and correlating common data, such as names and places, as information is aggregated from across different data systems. You may be familiar with identity management by another name: Master Data Management (MDM), Enterprise Master Patient Index (EMPI), or Common Client ID (CCID). By any name, identity management is essential for shared services and enables the correct matching of information drawn from disparate systems. For example, the Alabama Medicaid Agency adopted a solution for identity synchronization and autoprovisioning, which helped saved IT staff valuable hours. The solution also helped the state enhance the security of its data and its compliance with privacy regulations, such as those detailed in the Health Insurance Portability and Accountability Act of 1996 (HIPAA).
xiii
12
TRANSFORMING THE MANAGEMENT AND DELIVERY OF HEALTH AND HUMAN SERVICES
THE ARCHITECTURE OF COORDINATION
Today we have the technology to build more holistic, connected, people-centered HHS systems. Your IT legacy need not become an impediment. The Connected HHS Framework demonstrates how interoperability and services can be deployed in an IT architecture.
By adhering to the tenets of service orientation, federated data, federated security, and trustworthiness, the Connected HHS Framework can help you: Create a security-enhanced, connected infrastructure. How can you make information accessible when and where people need it? It starts with a core infrastructure designed for integration and interoperability. Connect operational silos. How can government agencies, nongovernment service providers, nonprofit agencies, commercial partners, and relevant stakeholders work together unless they can share information easily? An enterprise service bus connects the dots. Modernize information and systems. Do you want to enhance and extend existing applications or to develop new solutions that work with your existing IT investments? To coordinate care, you need an architectural framework based on shared services. Connect people. At the applications layer, the Connected HHS architecture exemplifies the meaningful use of technologyto promote coordination and information sharing across programs, departments, and communities of careand, ultimately, to improve your ability to deliver services.
Success with SOA
Technical solutions based on SOA achieve limited success when they are driven from the bottom up without attention to an organization's larger mission. And top-down, mega-projects often take so long to implement that they are obsolete before they are complete. How is the Connected HHS Framework and vision different? Its the:
People. A people-first approach to
SOA means implementing technologies that are mapped to processes and desired outcomes according to your roadmap and business processes.
Incremental approach. Technologies
are implemented as incremental, iterative projects governed by your strategic vision.
Rapid return. Unlike systems of the
past that took years of planning and implementation, an architecture based on Connected HHS principles enables you to build solutions that deliver results fastwithin the tenure of the executives backing the rollout.
Core infrastructure
The core infrastructure of a Connected HHS technology platform includes enterprise-level communications, collaboration, and other services that provide the stable building blocks for an agile applications environment. (See Figure 1.)
13
TRANSFORMING THE MANAGEMENT AND DELIVERY OF HEALTH AND HUMAN SERVICES
Figure 1. Architectural layers of the Connected HHS Framework rely on a common set of technologies.
Connected HHS enterprise service bus
To join up silos of operations, you need solutions that help you handle diverse systems, platforms, technologies, access and delivery channels, applications, languages, and credentials. The Connected HHS architecture is designed to help you support interoperability amidst diversity. To do this, the architecture uses an enterprise service bus that performs multiple functions. It: Enables interoperability across programs and systems through web services. Provides the data services used for business performance management tools. Offers a unified view of clients and resources across departments.
14
TRANSFORMING THE MANAGEMENT AND DELIVERY OF HEALTH AND HUMAN SERVICES
Shared services layer
In a Connected HHS architecture, new applications and functionality can be introduced through the shared services layer. In this context, shared services refer to extensible applications and loosely coupled web services reusable components that you can deploy across agencies to target common areas, such as intake, pre-eligibility, referrals, business rules engine, case coordination, security, and privacy. These types of shared services help you implement process, program, or legislative changes fast and flexibly. At this layer, a security and compliance strategy must be built in with appropriate controls. You must protect confidential citizen information and support compliance with relevant policies yet retain the flexibility to share data and application functions across boundaries. The Connected HHS Framework is designed with multiple layers of security. You can also provide a single, consistent identity credential for many applications, including authentication and authorization of different kinds of users.
Agency applications layer
With a clear view of common service components needed in your environment, you can then choose the most suitable application technologies. The agency applications layer of a Connected HHS architecture makes available to users the information that would have been stored away in legacy systems. Even within single departments, workers can get more from your existing systems. Business solutions can provide improved access to data and analytics, offer simplified user interfaces for workflows, or deliver flexible, web-enabled interfacesthus liberating data and creating a platform for business transformation. Mobile applications, in particular, can help free workers to spend more time with clients. With a smartphone, tablet PC, or other mobile device, employees have access to the information they need to stay productivevirtually anytime and anywhere they have an Internet connection.
Always-on services in the cloud
The freeing power of cloud computing is allowing public and private sector professionals to stay connected to vital work resources while on the road, with a combination of smart devices, Internet connectivity, and powerful apps. As a Connected HHS option, cloud computing unlocks access to programs using Internet protocols while also significantly reducing the high material costs of ITservers, software, and operations by in-house IT staff. Instead, cloud data centers do the work for you so your IT staff can focus on business solutions for your organizations users. For example, the nonprofit Czech Red Cross worked with a partner to create a hosted private cloud infrastructure built on Windows Hyper-V technology. The solution replaced the inefficient, paper-based communication processes that volunteers had been using and sped the transmission of information during emergencies. In addition, the new IT infrastructure can be easily managed by its volunteer staff.
xiv
With a platform based on Connected HHS and shared services, you don't have to choose between cloud services or on-premises solutions. You can configure a hybrid combination that fits your requirements now and in the future.
15
TRANSFORMING THE MANAGEMENT AND DELIVERY OF HEALTH AND HUMAN SERVICES
GETTING STARTED: YOUR ROADMAP FORWARD
Out with the stove pipes and silos, in with the shared services. But how do you get there? Your agency needs a new approach to its business processes to take full advantage of Connected HHS technology. Its time to draft your strategy.
The Connected HHS vision encompasses a new approach to business processes and technology infrastructure. A project-specific roadmap guides your teams toward the shared services goal by analyzing business needs, identifying gaps, and then aligning technology initiatives with business goals. For example, when the State of Alabama began planning its Connected HHS deployment, key agencies convened, from the Department of Human Resources to the Medicaid Agency to the Department of Finance. Commissioners and key staff worked together to review processes, systems, plans, and performance results alongside the Information Services Division. Planning paid off in design specifications tailored for the critical initial components of the states deployment.
xv
Updating your business model
With the new service models, your agency needs to develop an architecture for its business as much as it needs one for its IT infrastructure. A business architecture is your roadmap of enterprise processes and performance objectives. With the goal of sharing and connecting services, your business architecture aligns with your technical strategy so that you can drive program and technology departments in the same direction. A roadmap guides the process. As you begin to define your business requirements, you can use the Connected HHS approach for the delivery of shared services. You start with two key pieces of information:
Common practices. By identifying the
common business processes used across multiple programs, you begin to see where organizations can share services.
Points of intersection. Where do
A roadmap for shared services
Your roadmap should define the approach, timing, and steps that will take your organization to a shared services environment: Establish a baseline. Know what you have so you know what success
programs and departments cross paths? Your architecture must address these points of information access.
looks like. Start by listing existing business and technology assets, and then set targets, establish metrics, and measure progress against your baseline so you can track the return on investment (ROI). Get strategic. Articulate a front-to-back business strategy, and align it with a comprehensive technology strategy. Start with your model for delivering collaborative services. Determine the types of data-sharing that are useful. Weigh the choices. Which cases need cross-agency collaboration? How will the agencies and programs work together? Review relevant experiences, and evaluate approaches that have been successful elsewhere.
16
TRANSFORMING THE MANAGEMENT AND DELIVERY OF HEALTH AND HUMAN SERVICES
Get funding. Ask how cost will be allocated. Where is the funding coming from? Design for governance. Establish clear parameters for sharing information. From a user perspective, clarify accountability. Who gets to decide the optimal, cross-agency case plan? Who can see what about whom, when, and where? From a systems perspective, determine where the integrated system runsand who makes repairs when necessary. Invest over time. Don't wait to define perfection on paper before moving forward. Instead, plan for incremental changes in alignment with your roadmaps vision. Grow capabilities over time, build upon each success, and expectand design forchange. Prioritize. Let policy set precedence, whether that means providing emergency relief, expanding access to care, becoming more accountable, improving reporting, or mitigating risk. Set milestones. Recognize that aspects of the roadmap will probably shift with time and experience. Adopt regular checkpoints for roadmap reassessment.
Mind the gap as you go
Your roadmap should include a detailed gap analysis, which serves as the blueprint for implementing a Connected HHS solution. Microsoft Services can help you assess how closely the Connected HHS Framework aligns with your requirements and can help determine how to tailor the solution to your needs. Our analysis helps fulfill your due diligence requirements by:
Identifying gaps before you deploy,
which helps reduce risk.
Providing a quick, but thorough,
analysis for your decision.
Building confidence that your
solution will meet expectations.
Reducing the time and effort
required for implementation.
Contact us for details at:
Manage change: the new governance
How agile are you? Youre about to find out. Shared services require a new approach to governance and change management, and your roadmap needs to consider this idea. Governance is the operational framework you use to determine how existing services are monitored, defined, and authorizedtasks that often become more complex in shared services workflows where the number of stakeholders expands.
www.microsoft.com/services
Therefore, the transition to a more agile and connected business and technology environment requires organizations to rethink governance. Whether your organization chooses to set up a centralized, distributed, or outsourced model or to use a hybrid approach, successful governance requires a strong vision and shared goals across agencies, departments, and programs.
17
TRANSFORMING THE MANAGEMENT AND DELIVERY OF HEALTH AND HUMAN SERVICES
MICROSOFT AND HHS
The health of our nations HHS systems depends on a service-oriented business and technology architecture. Shared services are at the heart of the Connected HHS Framework and the Microsoft vision for a holistic, incremental approach to innovation. Our goal is to help improve access, outcomes, and efficiency through connected systems of care.
Connected systems of care center on the individual and the family. Microsoft delivers comprehensive, proven, security-enhanced technology and services platform for HHS agencies, departments, and programs. Through CRM, business intelligence, unified communications, and other Connected HHS technologies, your agency can speed response time and deliver greater value to citizens, other organizations, and the communities you serve. With more than $10 billion invested annually in research and development, plus the largest partner ecosystem in the industry, Microsoft offers wide-ranging choices to public sector organizations considering business and technology modernization initiatives. Together with our certified partners, we can help you apply Microsoft technologies in innovative ways that unite government and IT for greater impact.
LEARN MORE
Microsoft has a long-term commitment toand extensive experience inthe public health and social services sectors. As a technology leader, we understand the importance of compliance with standards and we routinely operate within open-standard and industrystandard environments to support your agencys technology needs. Contact your Microsoft Account Manager or partner to learn more about how Microsoft solutions and Connected HHS technology can help your organization.
CONTACT US health@microsoft.com www.microsoft.com/hhs
18
TRANSFORMING THE MANAGEMENT AND DELIVERY OF HEALTH AND HUMAN SERVICES
Connected HHS technology from Microsoft
Much of the technology and resources needed on the road to Connected HHS may already exist in your data centers and on your computers. Microsoft can show you how other government agencies have embraced the Connected HHS philosophy by leveraging existing IT tools and integrating new technologies. To learn more, contact health@microsoft.com or take a look at some of our products and solutions, listed below. Table 5. Microsoft products and solutions
Technology Business intelligence Description Derive the most value from information with the enterprise-ready data analysis tools in Microsoft SQL Server 2012. Boost satisfaction for citizens with the latest unified communications technologies which, together with CRM applications, can help you manage citizen requests and connect callers to the channels they preferincluding live service representatives or web-enabled self-service portals. Give case workers access to up-to-date demographic information, progress notes, and other information critical to individual or family care. Microsoft Dynamics CRM 2011 delivers connected case coordination capabilities. Gain more value from your server infrastructure by turning to the cloud. A cloud-optimized data center can help you deploy agency solutions and data to community-based organizations and nonprofit agencies that do not have dedicated IT staff or data centers. Extend the use of existing Microsoft Office products for communication and collaboration. Microsoft SharePoint 2010 gives teams many ways to share information. For more information, download the white paper, Improving health and human services with enterprise content management.
Call centers
Case management
Cloud services
Collaboration
Desktop efficiency
Get a streamlined user interface and new features that make everyday tasks easier with Windows 7.
Medicaid management
Get help complying with MITA standards. Microsoft solutions for Medical management information systems, based on the Connected HHS Framework, can help you to reduce administrative costs, enhance delivery of essential services, and implement improved security, privacy, and control. Connect disparate systems with the integration server solution, Microsoft BizTalk Server 2010, the hub of your Connected HHS architecture. Provide flexible access to servicesfrom mobile service centers to self-help portalsfrom a variety of devices, including PCs, smartphones, and other mobile devices. Web solutions can also provide a central workspace where cross-agency teams can log on and share information.
Systems integration
Web services
19
TRANSFORMING THE MANAGEMENT AND DELIVERY OF HEALTH AND HUMAN SERVICES
Endnotes
i
Hersey, Jack. Miami-Dade County makes a connection. Microsoft in Health blog. October 19, 2011. blogs.msdn.com/b/microsoft_in_health/archive/2011/10/19/miami-dade-county-makes-a-connection.aspx
ii iii
Ibid.
A call to action: Information exchange strategies for effective state government. April 2011. www.nascio.org/publications/ Cooper, Lane F. Aspiranet leverages collaboration platform to deliver better and more accountabl e services to California children and families. Aspiranet case study. 2009. biztechreports.com/yahoo_site_admin/assets/docs/AspiranetCaseStudy.360202244.pdf v Thomas-Flynn, Gail. Office 365 and the cloud make HIPAA easy. Microsoft Government: Bright Side of Government blog. January 20, 2012. www.microsoft.com/industry/government/state/brightside/detailBlog.aspx?title=Office_365_and_the_Cloud_Make_HIPAA_Easy vi OLeary, William, and Elizabeth Mason. Improving health, human services, and education outcomes and reducing poverty: Microsoft and Single Stop USA case study. 2011. www.singlestopusa.com/MicrosoftSingleStopUSA.pdf vii The Wisconsin Health Information Exchange Emergency Department Linking Project. March 2011. Microsoft case study. download.microsoft.com/download/5/3/F/53F61716-24A3-4EA4-936E38F865D546DE/AmalgaWisconsinHealthInformationExchangeCaseStudy.pdf viii Horowitz, Brian T. Microsoft launches state health insurance exchange platform. eWeek. February 9, 2011. www.eweek.com/c/a/Health-Care-IT/Microsoft-Launches-State-Health-Insurance-Exchange-Platform-403447/ ix Utah Health Exchange website. www.exchange.utah.gov/about-the-exchange/overview x bswift, Microsoft join forces to provide health insurance exchange solutions. bswift case study. October 25, 2011. www.bswift.com/index.php?/press-releases/bswift-microsoft-join-forces-to-provide-health-insurance-exchange-solu/ xi Arizona health agency ups quality and security with interoperable exchange solution. Microsoft case study. August 2009. www.microsoft.com/casestudies/Case_Study_Detail.aspx?casestudyid=4000005113 xii Boulder County deploys collaborative social services tool, wait times drop from weeks to hours. Microsoft case study. August 16, 2010. www.microsoft.com/casestudies/Case_Study_Detail.aspx?CaseStudyID=4000008098 xiii Alabama Medicaid Agency to cut time spent on identity management by 75 percent. Microsoft case study. February 2010. www.microsoft.com/canada/casestudies/Case_Study_Detail.aspx?casestudyid=4000006514 xiv Humanitarian group offers timely emergency relief with scalable, hosted private cloud. November 21, 2011. Microsoft case study. www.microsoft.com/casestudies/Windows-Server-2008-R2/Czech-Red-Cross/Humanitarian-Group-Offers-TimelyEmergency-Relief-with-Scalable-Hosted-Private-Cloud/4000011451 xv Day, Alan, Lynn Davenport, David Meyers, and William OLeary. "Camellia Project: A Connected Health and Human Services Framework for Alabama." May 2007. www.camellia.alabama.gov
iv
20
You might also like
- Arrastre Operator's Liability Limited to P5,000 Per Package Despite Late ClaimDocument21 pagesArrastre Operator's Liability Limited to P5,000 Per Package Despite Late ClaimJoe CuraNo ratings yet
- First Division G.R. No. 135645, March 08, 2002: Supreme Court of The PhilippinesDocument10 pagesFirst Division G.R. No. 135645, March 08, 2002: Supreme Court of The PhilippinesJoe CuraNo ratings yet
- First Division G.R. No. L-31379, August 29, 1988: Supreme Court of The PhilippinesDocument9 pagesFirst Division G.R. No. L-31379, August 29, 1988: Supreme Court of The PhilippinesJoe CuraNo ratings yet
- Cudia v. CA PDFDocument4 pagesCudia v. CA PDFJoe CuraNo ratings yet
- Heirs of Felicidad Canque v. CADocument1 pageHeirs of Felicidad Canque v. CAJoe Cura100% (1)
- First Division G.R. No. 172682, July 27, 2016: Supreme Court of The PhilippinesDocument19 pagesFirst Division G.R. No. 172682, July 27, 2016: Supreme Court of The PhilippinesJoe CuraNo ratings yet
- Unitrans v. Insurance Company of North America GR. 203865Document10 pagesUnitrans v. Insurance Company of North America GR. 203865Joe CuraNo ratings yet
- Esmena v. PogoyDocument2 pagesEsmena v. PogoyJoe CuraNo ratings yet
- PBCom V Basic Polyprinters and Packaging Corp.Document9 pagesPBCom V Basic Polyprinters and Packaging Corp.Judy Ann MurilloNo ratings yet
- Lexber Inc. V Sps. Dalman G.R. No. 183587, April 20, 2015Document14 pagesLexber Inc. V Sps. Dalman G.R. No. 183587, April 20, 2015Joe CuraNo ratings yet
- NPC v. IbrahimDocument5 pagesNPC v. IbrahimJoe CuraNo ratings yet
- Cudia v. CA PDFDocument4 pagesCudia v. CA PDFJoe CuraNo ratings yet
- Habana v. RoblesDocument1 pageHabana v. RoblesJoe CuraNo ratings yet
- Beegan v. BorjaDocument1 pageBeegan v. BorjaBenBulacNo ratings yet
- People v. BaringDocument1 pagePeople v. BaringJoe CuraNo ratings yet
- NYK Int'l Knitwear Corp. Philippines v. NLRCDocument1 pageNYK Int'l Knitwear Corp. Philippines v. NLRCJoe CuraNo ratings yet
- Go Chi Gun v. Co ChoDocument1 pageGo Chi Gun v. Co ChoBenBulacNo ratings yet
- NYK Int'l Knitwear Corp. Philippines v. NLRCDocument1 pageNYK Int'l Knitwear Corp. Philippines v. NLRCJoe CuraNo ratings yet
- Chavez v. PCGGDocument1 pageChavez v. PCGGJoe Cura100% (2)
- Credtrans Compiled Digests May 12Document17 pagesCredtrans Compiled Digests May 12Joe CuraNo ratings yet
- Filipino Society of Composer v. Benjamin TanDocument1 pageFilipino Society of Composer v. Benjamin TanJoe CuraNo ratings yet
- Tax Base RatesDocument8 pagesTax Base RatesJoe CuraNo ratings yet
- Harper & Row v. Nation EnterprisesDocument1 pageHarper & Row v. Nation EnterprisesJoe Cura100% (1)
- Go Chi Gun v. Co ChoDocument1 pageGo Chi Gun v. Co ChoBenBulacNo ratings yet
- Etepha v. Director of PatentsDocument1 pageEtepha v. Director of PatentsJoe CuraNo ratings yet
- Conrad v. CA (Trademark InfringementDocument1 pageConrad v. CA (Trademark InfringementJoe CuraNo ratings yet
- Asia Brewery v. CADocument1 pageAsia Brewery v. CAJoe CuraNo ratings yet
- Etepha v. Director of PatentsDocument1 pageEtepha v. Director of PatentsJoe CuraNo ratings yet
- Fruit of The Loom v. CADocument1 pageFruit of The Loom v. CAJoe CuraNo ratings yet
- Campbell v. Acuff-Rose MusicDocument3 pagesCampbell v. Acuff-Rose MusicJoe CuraNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5784)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Balanced Diet ChartDocument2 pagesBalanced Diet ChartjosephNo ratings yet
- Posterior Stabilization of Wedge Compression Fractures with Pedicle Screw FixationDocument7 pagesPosterior Stabilization of Wedge Compression Fractures with Pedicle Screw FixationAlla Yeswanth Dilip KumarNo ratings yet
- Bipolar Disorder Symptoms, Causes and TreatmentDocument108 pagesBipolar Disorder Symptoms, Causes and TreatmentMaica LectanaNo ratings yet
- ACF Community Nutrition GuideDocument170 pagesACF Community Nutrition GuideAction Against Hunger USA100% (1)
- List of Chyawanprash Manufacturers in IndiaDocument3 pagesList of Chyawanprash Manufacturers in Indiaplacementducat63No ratings yet
- Deficient Fluid Volume (AGEDocument2 pagesDeficient Fluid Volume (AGENursesLabs.com83% (6)
- SolutionDocument7 pagesSolutionapi-269290275No ratings yet
- The same questions apply as aboveDocument29 pagesThe same questions apply as aboveمحمد عزيز حسن ماضيNo ratings yet
- WPH VMO Directory1Document56 pagesWPH VMO Directory1Ragupathi MNo ratings yet
- Significance of Rural Development: Dr. Radhika KapurDocument16 pagesSignificance of Rural Development: Dr. Radhika KapurRay chijiokeNo ratings yet
- Patient Examination: History: by Professor of Internal MedicineDocument47 pagesPatient Examination: History: by Professor of Internal MedicineMonqith YousifNo ratings yet
- YL Camping Consent and Health FormDocument4 pagesYL Camping Consent and Health Formmcronin1970No ratings yet
- Hyponatremia: Causes, Evaluation & TreatmentDocument20 pagesHyponatremia: Causes, Evaluation & TreatmentmanjaruNo ratings yet
- Trauma and Stressor-Related DisordersDocument32 pagesTrauma and Stressor-Related DisordersRay Anne Labra-PepitoNo ratings yet
- Research FinalDocument31 pagesResearch FinalLiezl mm100% (1)
- Peter Lin, MD Biography: Medical TopicsDocument4 pagesPeter Lin, MD Biography: Medical TopicsBeo ThaiNo ratings yet
- Progressive Balbar Palsy: Dr. Mohamed Ali 3 Year MD IM ResidentDocument15 pagesProgressive Balbar Palsy: Dr. Mohamed Ali 3 Year MD IM ResidentMohamed AliNo ratings yet
- 26 Sri Rahayu OktavianiDocument123 pages26 Sri Rahayu OktavianiFebrianti FebriantiNo ratings yet
- How To Gain Muscle Workout and Diet Tips PDFDocument1 pageHow To Gain Muscle Workout and Diet Tips PDFSebastian ZuniniNo ratings yet
- Standards For Sanitation: What, Why and How?: Kate Hurley, DVM, MPVMDocument26 pagesStandards For Sanitation: What, Why and How?: Kate Hurley, DVM, MPVMKaren SalcedoNo ratings yet
- NHS Patient Safety SyllabusDocument22 pagesNHS Patient Safety SyllabusMubeenRahmanNo ratings yet
- Ampicillin drug profileDocument2 pagesAmpicillin drug profileRenz Ivan FuntilonNo ratings yet
- Industrial Safety: University of Kirkuk College of Engineering Mechanical DepartmentDocument4 pagesIndustrial Safety: University of Kirkuk College of Engineering Mechanical DepartmentAbdullah HusseinNo ratings yet
- MDRTB Case StudyDocument35 pagesMDRTB Case StudyFejlean Angelica AntineoNo ratings yet
- Crossm: George R. Thompson, III, Phoebe Lewis, Stuart Mudge, Thomas F. Patterson, Bruce P. BurnettDocument11 pagesCrossm: George R. Thompson, III, Phoebe Lewis, Stuart Mudge, Thomas F. Patterson, Bruce P. BurnettarchikaNo ratings yet
- The Importance of Using ContraceptivesDocument14 pagesThe Importance of Using ContraceptivesYsabelle De GuzmanNo ratings yet
- Peace Corps Mefloquine Policy March 2015 Letter To DirectorDocument7 pagesPeace Corps Mefloquine Policy March 2015 Letter To DirectorAccessible Journal Media: Peace Corps DocumentsNo ratings yet
- E-Learning PHARM 131 - Chapter2Document10 pagesE-Learning PHARM 131 - Chapter2Ryan Charles Uminga GalizaNo ratings yet
- Government of NCT of Delhi Delhi Subordinate Services Selection Board Fc-18, Institutional Area, Karkardooma, DelhiDocument3 pagesGovernment of NCT of Delhi Delhi Subordinate Services Selection Board Fc-18, Institutional Area, Karkardooma, DelhiVivekRawalNo ratings yet
- Human BecomingDocument3 pagesHuman BecomingCharles DaveNo ratings yet