Professional Documents
Culture Documents
Alzheimer Disease PDF
Uploaded by
karpanaiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Alzheimer Disease PDF
Uploaded by
karpanaiCopyright:
Available Formats
Alzheimer Disease: Genetic and Environmental Influences
Chandra A Reynolds, University of California, California, USA
Based in part on the previous version of this eLS article Alzheimer Disease (2005) by Chandra A Reynolds and Michael Crowe.
Advanced article
Article Contents
. Introduction . Inheritance and Population Genetics . Aetiological Heterogeneity . Environmental Factors . Conclusions
Online posting date: 15th January 2013
Alzheimer disease (AD) is a complex, progressive neurodegenerative disease. Prevalence of AD is expected to grow substantially, although predictions may shift given future treatment interventions or higher levels of engagement in lifestyle delaying factors that may reduce risk. Several mutations have been characterised and susceptibility genes implicated as playing a role in the disorder. The apolipoprotein E (APOE) e4 allele remains the best-established susceptibility gene for late-onset AD. Although a substantial proportion of the liability for AD may be accounted for by genetic factors, heterogeneity or differences in aetiology are important to consider. Environmental factors probably play a significant role, such as education, head injury and nonsteroidal anti-inflammatory drugs (NSAIDs) use, as well as obesity, diabetes, physical activity and cognitively engaging leisure activities. The extent to which susceptibility genes interact with environmental factors may provide further clues to aetiology. Lastly, a developmental longitudinal perspective on the salience of particular risk and protective factors across the life course may illuminate etiologies and potential points of intervention.
genes as well as multiple environmental factors are involved in the development of AD. These genetic and environmental factors may act independently or synergistically. Thus, current genetic research is aimed not only at nding new genes and gene pathways related to AD but also at examining genegene and geneenvironment interactions.
General characteristics
AD is a devastating disease and is also a tremendous public health concern. It is the number one cause of dementia in older adults (Alzheimers Association, 2012). Typically, the initial and primary observable characteristic of AD is a progressive and irreversible decline in memory. This decline in memory is accompanied by deterioration in at least one or the other area of intellectual functioning, such as language, visualspatial skills and judgment and reasoning (McKhann et al., 2011). Emotional and personality changes are also common (McKhann et al., 2011). Recent diagnostic criteria and guidelines disseminated by the Alzheimers Association and the National Institute on Aging in 2011 revise and expand the criteria used over the past three decades (Sperling et al., 2011). The new diagnostic criteria recognise three stages of AD: (1) dementia due to Alzheimers, (2) mild cognitive impairment (MCI) and (3) preclinical Alzheimers, whereby biological changes emerge over time, up to decades ahead of any clinical signs. To diagnose probable AD dementia, the cognitive decits must represent a gradual decline from previous functioning levels, unexplained by other major psychiatric disorders or delirium, and must be severe enough to interfere with social and occupational functioning (McKhann et al., 2011). MCI includes relative declines in cognitive functioning with impairments in one or more areas of intellectual functioning, but individuals maintain independence in daily activities of living (Albert et al., 2011). Onset of AD symptoms is often dicult to pinpoint because deterioration is gradual. People in close contact with someone beginning to develop AD may not notice changes for some time. Memory impairment, especially impairment of the ability to retain new information, is
1
Introduction
As knowledge of human genetics has progressed substantially since the 1990s, and indeed rapidly in the last 5 years, knowledge regarding the genetics of Alzheimer disease (AD) has also accumulated rapidly. One major conclusion drawn from this line of research is that the aetiology of AD is complex. It is now widely believed that multiple
eLS subject area: Neuroscience How to cite: Reynolds, Chandra A (January 2013) Alzheimer Disease: Genetic and Environmental Influences. In: eLS. John Wiley & Sons, Ltd: Chichester. DOI: 10.1002/9780470015902.a0005243.pub2
eLS & 2013, John Wiley & Sons, Ltd. www.els.net
Alzheimer Disease: Genetic and Environmental Influences
usually the rst symptom to be noticed in persons with AD (McKhann et al., 2011). After diagnosis, AD patients may live an average of 48 years (Alzheimers Association, 2012). As the disease progresses, there is a gradual loss of abilities that eventually includes the inability to perform many basic activities of daily life, such as taking a bath or dressing (Alzheimers Association, 2012). Death is often due to other ailments that result from a greater susceptibility to illness or due to AD-related complications such as the inability to swallow (Alzheimers Association, 2012). Although AD primarily aects those over the age of 65, it can also occur in younger people. A distinction is commonly made between early-onset, or onset before age 60, and late-onset cases of AD. Early-onset patients are more likely than late-onset patients to have a rst-degree relative, such as a parent or a sibling, who also has the disease (Silverman et al., 2005). This nding may point to a possibly greater contribution of genetic inuences for earlyversus late-onset AD. In further support for the distinction between early and late onset is the nding that the disease may progress more rapidly in those with early-onset AD (Reitz et al., 2011).
Prevalence
Prevalence of AD (number of current cases) increases dramatically after age 60. Indeed, the prevalence appears to double every 56 years between the ages of 60 and 90 years (Brookmeyer et al., 2011). The prevalence of AD is approximately .9% in those aged 6569 years and more than 26% in those aged 90 years and older (Colantuoni et al., 2010). The overall prevalence in those aged 60 years or older is approximately 67% in North America (Colantuoni et al., 2010), and worldwide the prevalence is approximately 4.5% (Colantuoni et al., 2010). Successive generations of people are now living longer, and this increase in longevity suggests that the prevalence of AD will continue to rise over this century, quadrupling by 2050 (Brookmeyer et al., 2011). Of the entire population, those of 85 years of age and older are both the fastest-growing group of people and most at risk for developing AD. However, future prevalence is dicult to estimate. Factors that may plausibly contribute to risk of AD, such as low education may be less frequent in successive cohorts. There may also be research advances in treatment or prevention that would counter otherwise increasing rates of disorder (Brookmeyer et al., 2011). Thus, prevalence may not increase to the extent that many projections have estimated despite the expected growth in the elderly population.
Neuropathology
In addition to clinical symptoms, there are pathological changes that are consistently found in the brains of people with AD. Alois Alzheimer rst described the primary signs of AD brain tissue pathology in 1907 (see Perl, 2010). He observed clusters of proteins in the brain that are now considered to be pathological hallmarks of AD. He also
2
noticed brain atrophy, or shrinking of the brain due to neuronal death, another hallmark sign of AD. Neuronal cell loss, amyloid plaques and neurobrillary tangles are the three predominant neuropathological characteristics of the AD brain (Perl, 2010). Neuronal cell loss is most pronounced in the hippocampus and cerebral cortex (Mattson, 2004). The hippocampus is an area of the brain that is involved in memory, whereas the cortex is thought to be involved in judgment, reasoning, memory, language and other higher-order thought processes. The question of what causes these cells to die is central to understanding AD. Formation of plaques and tangles is believed to be responsible for much of this neuronal loss, but the proposed explanations for this process remain controversial (Nelson et al., 2012). Amyloid plaques, which are sometimes also referred by subtypes as diuse or neuritic plaques, form between neurons in the synapses (Nelson et al., 2012; Perl, 2010). Synapses are the spaces between neurons into which neurotransmitters (chemicals used for communication between neurons) are released. The plaques consist of accumulations of degenerative nerve endings and other materials, with a core of beta-amyloid (Ab; Perl, 2010). Ab peptide fragments are cleaved from a much larger amyloid precursor protein (APP) that is thought to be involved in nerve growth and repair. However, it is a toxic version of the Ab peptide that has been detected in plaques (Mattson, 2004; Perl, 2010). Compared with diuse plaques, neuritic plaques contain deteriorating or distended neuritic structures (axons and dendrites) and accumulations of abnormal tau protein products (Nelson et al., 2012). Amyloid plaques may interfere with communication between neurons, due to damaged neurites and synapses, as well as cause cell death (Mattson, 2004). Some studies have suggested that Ab deposits may disturb calcium levels, whereas others suggest that Ab plaques may be related to the generation of free radicals that damage cells (Mattson, 2004). Amyloid plaques are accompanied by an inammatory response, that is, activation of astrocytes, microglial cells and expression of cytokines, which may provoke neuronal damage (Nelson et al., 2012). Another possibility is that APP malfunctioning leads to neuronal damage and cell loss (Nelson et al., 2012). If this is true, the amyloid deposits may be a result of cell loss rather than a primary cause. Neurobrillary tangles are also made up of protein clusters; however, unlike the amyloid plaques, they are found within the nerve cell body. The protein that makes up these tangles is called tau; alterations in tau may lead to decient axonal transport and defective microtubule structure (Mattson, 2004). It is believed that the neurobrillary tangles impede energy metabolism, movement of nutrients and communication within and between nerve cells by disturbing the aected cells microtubule structure (Mattson, 2004). Feasible hypotheses regarding the associations among plaques, tangles, neuronal death and AD have been put forth, most notably the amyloid cascade hypothesis and
eLS & 2013, John Wiley & Sons, Ltd. www.els.net
Alzheimer Disease: Genetic and Environmental Influences
Hypothetical model of AD pathophysiological cascade
Age Genetics
Cerebrovascular risk factors Other age-related brain diseases
Amyloid- accumulation
Synaptic dysfunction Glial activation Tangle formation Neuronal death
Cognitive decline
Brain and cognitive reserve ? environmental factors
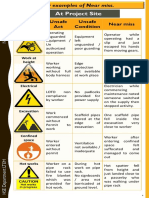
Figure 1 Hypothetical model of the Alzheimers disease (AD) pathophysiological sequence leading to cognitive impairment. This model postulates that amyloid beta (Ab) accumulation is an upstream event in the cascade that is associated with downstream synaptic dysfunction, neurodegeneration and eventual neuronal loss. Note that although recent work from animal models suggests that specific forms of Ab may cause both functional and morphological synaptic changes, it remains unknown whether Ab is sufficient or not to incite the neurodegenerative process in sporadic late-onset AD. Age and genetics as well as other specific host factors such as brain and cognitive reserve or other brain diseases may influence the response to Ab and/or the pace of progression towards the clinical manifestations of AD. Reproduced from Sperling et al. (2011), p. 283, with permission from Elsevier.
newer hypothetical models termed the AD pathophysiological cascade (Sperling et al., 2011; Figure 1), but much additional research is needed to fully understand AD aetiology. Although there is a strong correlation between neurobrillary tangle density and AD severity, there appears to be a negligible correlation between the amount of amyloid in the brain and AD severity (Nelson et al., 2012). That said, the amount of neuritic plaques appear to correlate more with measures of cognitive dysfunction than diuse plaques (Nelson et al., 2012). In fact, a number of people show no clinical symptoms of dementia before death despite the presence of plaques and tangles found on autopsy (Nelson et al., 2012). These observations in part have led to the revised diagnostic criteria and guidelines briey described above (Sperling et al., 2011).
Inheritance and Population Genetics
Genetic risk and heritability
An important question for AD researchers is: to what degree can the disease be attributed to genetic inuences? The lifetime risk of developing AD is 1012% (Goldman et al., 2011). Being genetically related to someone with AD raises ones own risk for the disorder. People who have a rst-degree relative with AD have a lifetime risk of developing dementia that is 24 times higher than those who do not have a family history of dementia (Goldman
et al., 2011). In terms of population-based statistics, the relative contribution of genes and the environment to the risk of AD can also be calculated. Heritability and environmentality are estimates of how much genetic and environmental factors, respectively, contribute to the underlying liability for a disease (van Dongen et al., 2012). An assumption is that there is some theoretical threshold of risk. It is only when this threshold is exceeded that the disorder will appear. It is possible that the cumulative (and possibly interactive) eects of genetic and environmental risk factors may push a person over the AD threshold, leading to onset of the disease. Twin studies are valuable for studying heritability for behavioural traits including AD. In twin studies, three components are typically estimated on the basis of the similarity (e.g. concordance rates) of monozygotic (MZ) and dizygotic (DZ) twin pairs (van Dongen et al., 2012): heritability; shared environmental inuences or experiences shared by twin pairs; and unique or nonshared environmental inuences. These components can be estimated using twins because MZ twins are genetically identical and DZ twins share half of their segregating genes on average (van Dongen et al., 2012). Given that one twin has AD, the extent to which MZ and DZ pairs dier in the probability that the twins partner also has AD is an indication of genetic eects. Relatively few studies have examined the heritability of AD by using twin samples that are representative of the general population. Since the rst registry-based twin study
3
eLS & 2013, John Wiley & Sons, Ltd. www.els.net
Alzheimer Disease: Genetic and Environmental Influences
by Kallman (1956), on senile dementia, researchers using four dierent twin registries have published ndings on the aetiology of dementia, including AD: the National Academy of SciencesNational Research Council registry (Breitner et al., 1995); the Finnish Twin Registry (Raiha et al., 1996); the Norwegian Twin Registry (Bergem et al., 1997) and the Swedish Twin Registry (Gatz et al., 2006b). Results from every twin study demonstrate that identical (MZ) twins have higher concordance rates for AD than concordance rates for fraternal (DZ) twins. In other words, if one twin has AD, it is more likely that his or her twin sibling will also have AD if they are identical twins. This consistent nding points to the importance of genetics in AD. Overall, the evidence from the largest study to date of 11 884 twin pairs (Gatz et al., 2006b) suggests that the heritability of AD is between .58 and .79. This means that 5879% of the liability of developing AD is due to genetic inuences. The range of estimates from the other studies is .28 to .60 (Bergem et al., 1997; Breitner et al., 1995; Raiha et al., 1996). Environmentality estimates (the estimated inuence of the environment on the development of AD) range from .21 to .42 (Gatz et al., 2006b), with shared environmental factors playing some role in the liability for AD (up to .19). This suggests that some of the inuence of the environment may represent exposure to similar environmental risk factors by both members of a pair during childhood or later in adulthood. There may be dierent inuences for age of onset of AD than for overall lifetime risk of developing the disease. For example, reports from the Swedish Twin Registry suggest that there is a high probability of unaected twin siblings remaining cognitively intact for at least 3 years following their cotwins AD diagnosis (Gatz et al., 1997). The unaected twin sibling may even remain intact for a decade. However, the probability of remaining intact drops signicantly 15 years after diagnosis of AD in their twin sibling. Findings showed that the younger the proband, the longer the time the initially unaected twin remained cognitively intact. MZ partners were signicantly more likely than DZ partners to become demented during the period from 4 to 12 years after their cotwins diagnosis. These results suggest that dierent genetic factors may inuence age of onset of AD to liability of manifesting AD. Two important conclusions are apparent from twin studies: First, although genetic eects are important, environmental factors also play a role in the development of AD. Second, there is a wide range of estimates of the inuence of genes relative to the environment. This lack of consistency may be attributable to at least four major sources: sample size; age and gender of those in the study sample; and ascertainment bias (bias resulting from how AD cases are identied) (Gatz et al., 2006b).
mutations assure that one will eventually get the disease, this is not true of susceptibility genes. Susceptibility genes raise the likelihood, or the risk, that one will get the disease.
Mutations
Mutations on three chromosomes have been linked to early-onset familial AD: chromosomes 21, 14 and 1 (Schellenberg and Montine, 2012). The pattern of familial transmission is consistent with a completely penetrant, autosomal dominant model, assuring that those carrying one of the mutations will develop AD if they live long enough. However, there is a great degree of variability for age of onset and clinical presentation associated with the mutations, suggesting that other environmental or genetic factors modify both the timing and the symptom prole of the disease presentation. Three specic gene loci have been identied as carrying multiple mutations: amyloid beta (A4) precursor protein (protease nexin-II, AD) (APP) on chromosome 21; presenilin 1 (AD 3) (PSEN1) on chromosome 14; and presenilin 2 (AD 4) (PSEN2) on chromosome 1 (Schellenberg and Montine, 2012). Down syndrome has also been associated with early-onset AD. Those with Down syndrome have three copies of chromosome 21 and thereby three alleles for the APP gene. The consequence of the presenilin and APP gene mutations appears to be an overproduction or faulty processing of APP, leading to amplied Ab protein deposition (Schellenberg and Montine, 2012). Mutations of the presenilin-1 gene are the most common. Nevertheless, the presenilin and APP gene mutations occur infrequently and account for only 15% of AD cases (Galimberti and Scarpini, 2012). Although most of the people with these mutations have early-onset familial AD, a vast majority of those with AD have the later-onset variety, which is not attributable to these genetic mutations.
Susceptibility genes Apolipoprotein E (APOE)
The apolipoprotein E gene (APOE; the protein is APOE), found on chromosome 19, is the susceptibility gene with the most support for late-onset AD (Schellenberg and Montine, 2012). Genetic linkage analysis and numerous casecontrol association studies have conrmed APOE as an important risk factor for AD (Schellenberg and Montine, 2012). APOE, a cholesterol transporter, has been implicated in repair of injury to the central nervous system (Dardiotis et al., 2012; Verghese et al., 2011). Two single nucleotide polymorphisms (SNPs) make up the primary APOE haplotypes which are combinations of alleles from rs7412 and rs429358. Of three haplotype variants that code for this protein, denoted e2, e3 and e4, the e3 allele is the most common (Egert et al., 2012), constituting 7488% of the APOE alleles in European and predominately white North American populations. The e4 allele frequency by comparison ranges from 6.5% to 17%. Allele frequencies for e4 vary widely worldwide (510% in Mediterranean
Gene mutations and susceptibility genes related to Alzheimer disease
Several specic genetic abnormalities, or mutations, have been found to cause AD. Although certain genetic
4
eLS & 2013, John Wiley & Sons, Ltd. www.els.net
Alzheimer Disease: Genetic and Environmental Influences
and Asian populations to nearly 41% in Central African populations; Egert et al., 2012). Moreover, a strong positive correlation exists between increasing northern latitude and e4 allele frequency in Europe (r=.80; Egert et al., 2012). The APOEe4 allele is linked with an increased risk for AD where e4 frequencies in AD cases are typically double or even triple that of unaected individuals (Genin et al., 2011; Schellenberg and Montine, 2012). The presumed mechanism is that the e4 variant may lead to greater deposition of Ab (Schellenberg and Montine, 2012). Most evidence suggests that the risk of AD increases with the number of e4 alleles, suggesting a dosage eect. A lower risk for AD is associated with the APOEe2 allele (Genin et al., 2011; Schellenberg and Montine, 2012). This indicates that the APOEe2 allele may be protective, though the evidence is weaker than for e4. The relationship between APOEe4 and AD may be age dependant, with a heightened risk between the ages of 65 and 75 years (Blacker et al., 1997). APOE genotype may explain 2030% of AD liability or more (Reitz et al., 2011). Thus, other factors must contribute to AD liability than APOE status. The association between APOE and AD is well documented; yet, inheriting either one or two APOEe4 alleles does not make it certain that an individual will get AD. Lifetime risk of AD by age 85 is estimated to be as high as 5152% and 6068% for males and females, respectively, that carry two e4 alleles (Genin et al., 2011); thus, many having at least one e4 allele will not develop AD. However, not having any APOEe4 alleles provides no assurance that an individual will never have AD (Genin et al., 2011). Genetic testing for APOEe4 to diagnose or prospectively predict AD is currently not recommended (Goldman et al., 2011). Although APOEe4 is strongly associated with AD, studies have found that APOE genotype alone does not provide sucient specicity as the e4 allele is also associated with other forms of dementia. Furthermore, the e4 allele is not present in many late-onset AD patients (Genin et al., 2011; Mayeux and Stern, 2012), suggesting the inuences of other genetic or environmental causes. Finally, APOE genotyping is not considered to be a useful predictive genetic test. A majority of people with one and a third to a half with two APOEe4 alleles do not develop AD (Genin et al., 2011). Thus, test results may cause unnecessary apprehension.
Emerging genes
APOEe4 is the best-established risk factor for AD (Schellenberg and Montine, 2012); however, other genes are involved. A variety of potential AD neuropathways led researchers to examine plausible candidates. As technology rapidly increased and ndings from candidate gene association approaches did not generally result in well-replicated ndings as anticipated, agnostic genome-wide association studies (GWAS) became the prominent strategy in which thousands of common genetic variants spread across the genome (typically SNP markers) were evaluated
for association with AD (Schellenberg and Montine, 2012). Although APOE and SORL1 were identied as plausible candidates given the potential role in Ab protein deposition, new genes identied via GWAS appear to be associated with increased risk of AD after accounting for APOE (Schellenberg and Montine, 2012). Indeed, several additional susceptibility genes appear to be important to the risk of AD, conrming and extending previous estimates that at least four to seven additional susceptibility genes may make a signicant contribution to late-onset AD (Daw et al., 2000). Altogether 10 conrmed susceptibility genes, with nine discovered in the past 5 years via GWAS, are: ABCA7, BIN1, CD33, CD2AP, CLU, CR1, EPHA1, MS4A4E/MS4A6A, PICALM and SORL1 (Schellenberg and Montine, 2012). Additional possible candidates have recently emerged from analytical approaches that take a gene-wide approach to evaluating association with the risk of AD rather than single SNP markers (e.g. FRMD6, Hong et al., 2012). The pathways that some of the newly identied susceptibility genes implicate are briey highlighted. The genes APOE, SORL1, CLU and ABCA7 play a role in the lipid metabolism pathway (Schellenberg and Montine, 2012). As summarised above the apoE protein encoded by APOE, the most well-established susceptibility gene for late-onset AD, is the major cholesterol transporter in the brain, although it is expressed elsewhere (that is, in the periphery); the e4 allele is associated with greater Ab protein deposition (Schellenberg and Montine, 2012). The SORL1 gene encodes sortilin receptor 1 (SorL1), which assists in the transport of the APP protein, a precursor of Ab, and also binds to lipoproteins (Schellenberg and Montine, 2012). Multiple SORL1 SNP variants and haplotypes, both common and rare, have been associated with increased risk of AD (Reitz et al., 2011; Schellenberg and Montine, 2012). The CLU gene, also known as APOJ, codes for apolipoprotein J (APOJ) and like APOE serves as a cholesterol transporter in the brain and periphery; ApoJ is proposed to inuence Ab protein deposition (Schellenberg and Montine, 2012). The ABCA7 gene encodes the adenosine triphosphate (ATP)-binding cassette (ABC) A7 transporter and may aect the outow (eux) of phospholipids and cholesterol from cells, mediate the formation of high density lipoprotein (HDL, often referred to as the good cholesterol) and may be implicated in cell injury response processes (Schellenberg and Montine, 2012; Tanaka et al., 2011). Other new susceptibility genes appear to be involved in immune response, including MS4A4E/MS4A6A as well as CR1 and CD33, both of which encode for cell surface receptors. For example, CR1 appears to be involved in the clearance of immune complexes, which are bound antibodyantigen formations, and possibly in the clearance of the Ab protein (Schellenberg and Montine, 2012). Other candidates appear to be involved in endocytosis (e.g. BIN1, PICALM and CD2AP), a process by which cells absorb or move extracellular protein molecules into the cytoplasm, or cell adhesion (EPHA1) (Schellenberg and Montine, 2012). Other newly emergent susceptibility
5
eLS & 2013, John Wiley & Sons, Ltd. www.els.net
Alzheimer Disease: Genetic and Environmental Influences
candidates, implicated using whole-gene methods, may be involved in pathways such as glycosylation or cell growth (e.g. FRMD6, Hong et al., 2012). For these and the other recently identied GWAS susceptibility genes, further research is necessary to identify and establish their specic functional roles that lead to an increased AD risk (Schellenberg and Montine, 2012).
Summary
The APOE and SORL1 gene candidates have been conrmed as increasing-AD risk after having been selected due to a hypothesised role in AD pathogenesis; these genes have amassed a relatively greater or lesser body of evidence, respectively, that implicates their involvement in Ab protein deposition. The extent and manner in which the newly identied susceptibility genes alter the risk of AD or moderate age of onset is yet unclear (ABCA7, BIN1, CD33, CD2AP, CLU, CR1, EPHA1, MS4A4E/MS4A6A, PICALM, FRMD4A) however, these candidates suggest a role for pathways such as lipid metabolism, immune response and cellular processes important to absorption of proteins. Moreover, in comparison with APOE, the balance of ndings for these 10 additional genes, although conrmed, suggests that they contribute to a lesser degree to AD risk. The functional roles of these new susceptibility genes remain to be evaluated in future work.
2011), where the relative impacts of acute versus chronic illness may vary in contributing to mortality. The prevalence of AD appears to dier among some groups with the same ethnic origins but living in dierent countries (Manly and Mayeux, 2004). For example, although the prevalence of AD appears higher in Japanese American men in Hawaii compared with Japanese men in Japan (c.f., White et al., 1996), it does not dier for Japanese immigrants to Brazil who arrived before the second World War (Ishii et al., 1999 as cited in Manly and Mayeux, 2004). This nding suggests that environmental factors, in addition to genetic factors, may play a part in the development of the disease. Dierential risk associated with APOEe4 according to ethnicity has been observed. Specically, APOEe4 appears to pose a signicant risk to those of European or Japanese origins, but the e4 association may be attenuated among African Americans and Hispanics (Manly and Mayeux, 2004); conversely, the risk of AD for none4 carriers may be greater among African Americans and Hispanics (Manly and Mayeux, 2004). A higher risk of AD among African Americans and Hispanics compared with whites, regardless of APOE status, has been reported (Manly and Mayeux, 2004). This suggests that other genetic or environmental inuences may play a role in the risk of AD in these ethnic groups.
Environmental Factors Aetiological Heterogeneity
Gender
Studies of prevalence of AD in dierent groups are important because true dierences between populations can contribute to understanding of the underlying aetiology and risk factors. A higher prevalence of AD among women than men has generally been found across epidemiological studies, 1417% versus 911% in overall lifetime risk estimates (Genin et al., 2011). Similarly, incidence data (number of new cases of AD) suggest a higher risk of AD among women than men. In addition to survival dierences between men and women, the gender dierence in part may reect dierential gene action conferred in women compared with men. For example, APOEe4 has been found to elevate risk of AD for women more so than for men (Genin et al., 2011). Age, family history of dementia and APOEe 4 are the bestestablished risk factors for late-onset AD (Alzheimers Association, 2012; Reitz et al., 2011). It is apparent that none of the best-established risk factors are reversible or preventable. However, it is also true that none of these risk factors assure that one will get AD. In addition, it is known from twin studies that environmental risk factors must also be involved in the aetiology of AD. As for the genetic risk factors for late-onset AD, it is important to remain mindful that although some of the described environmental risk factors may be associated with an increase risk of AD, observing an association or correlation does not establish causality.
Education
Currently, the best-established environmental risk factor for AD is low education (Sharp and Gatz, 2011). The education eect extends to dementia risk on the whole, albeit AD is the most common form of dementia (Sharp and Gatz, 2011). Determining the nature of the association between education and AD has proved to be dicult. Education may serve as a surrogate for other factors that could be related to the risk of AD, such as intelligence, socioeconomic status or lifestyle and health habits (Gatz et al., 2006a). It is not easy to separate education level from these confounding variables. However, education is a stronger predictor of AD or dementia risk where access to education is more available, and therefore more likely to be
Ethnicity
In general, cross-national comparisons suggest variations in the prevalence of AD (Brookmeyer et al., 2011; Reitz et al., 2011). Studies from Asia tend to report lower prevalence rates for AD, whereas higher rates are reported in Western Europe and North America (Brookmeyer et al., 2011; Reitz et al., 2011). However, incidence (new cases) of AD is relatively similar before age of 75, but diers at older ages likely due to dierences in survival rates (Reitz et al.,
6
eLS & 2013, John Wiley & Sons, Ltd. www.els.net
Alzheimer Disease: Genetic and Environmental Influences
reective of cognitive capacity and less likely to be confounded with socioeconomic status (Sharp and Gatz, 2011). Also, the association between education and AD may be partially due to diagnostic bias. Education level may aect scores on tests used for screening and dementia assessment variables (Sharp and Gatz, 2011). Some studies have found that those with less education have lower scores on neuropsychological tests but not greater functional decits or that lower education predicts incident dementia risk but not subsequent autopsy-dened neuropathology (see Sharp and Gatz, 2011). The cognitive reserve model has been used to explain the association between education and AD (see Sharp and Gatz, 2011; Stern, 2009). This idea is related to the threshold model of dementia. Within this model, the amount of cognitive reserve is associated with the threshold for meeting dementia criteria. The amount of brain reserve due to innate factors, prenatal development and early brain development during childhood may be reduced by damage to the brain that occurs over the life span. These processes may determine whether and when the critical threshold of viable brain tissue is reached and which dementia is apparent. Less cognitive reserve would mean that fewer changes would be necessary to reach this threshold compared with those with greater cognitive reserve. Low educational attainment may reect less cognitive reserve (Sharp and Gatz, 2011). Alternatively, higher education may reect engagement in more intellectually stimulating activities over the life span (Gatz et al., 2006a), which would hypothetically increase cognitive reserve.
deposition after head injury (Verghese et al., 2011). However, the relatively few available epidemiological studies have provided inconsistent ndings regarding the interaction between APOEe4 allele status and history of head injury on AD risk, although some characterise the evidence of moderation of risk across neurological disorders on the whole as strong (Verghese et al., 2011). It has been proposed that the association between head injury and AD may be explained by reduced cognitive reserve due to the head injury (Stern, 2009). The results for head injury hearken back to the threshold theory described earlier in this article that cumulative and perhaps interactive eects of genetic and environmental risk factors may tip ones risk of AD over a threshold, leading to or hastening the onset of the disease. Nonetheless, an increased risk due to environmental or genetic susceptibility factors does not ensure a diagnosis.
Physical activity and Obesity
Low physical activity and high body mass index (BMI) are each associated with higher risks of chronic illnesses that are in turn associated with poorer cognitive health in late life, such as cerebrovascular disease and diabetes (Reitz et al., 2011). Moreover, higher midlife BMI and lower physical activity, respectfully, predict a higher risk of AD (Reitz et al., 2011). However, a higher BMI in late life may be related to a reduced risk of AD (Reitz et al., 2011). Such results suggest that midlife weight may be particularly salient to later AD risk. Indeed, higher midlife BMI and declines in BMI between mid and late life may be predictive of worse cognitive performance across domains, and in particular may potentiate decline in speed of processing (Dahl et al., 2012), altogether leading to a higher risk of poor cognitive health in late life. Exercise, particularly aerobic exercise, shows an overall benet to cognition in old age and may be related to increased brain volume or levels of amyloid which may aect brain and cognitive reserve (Erickson et al., 2012; Hertzog et al., 2009). Whether physical activity mitigates AD risk irrespective of APOE genotype or is particularly benecial to those carrying one or more e4 alleles is not clear (Erickson et al., 2012; Miller et al., 2012). However, self-reported physical exercise engagement appears to be correlated with amyloid plaque deposition in nondemented adults aged 45 to 88 years (Head et al., 2012), and sedentariness was particularly negative in terms of increased amyloid plaque deposition in APOE e4 carriers (Head et al., 2012). Measurement of physical activity and related health behaviours (objective versus self-report), follow-up time, and sample selectivity are important to evaluate in future work (Miller et al., 2012). Moreover, a life course perspective on multiple health behaviours including physical activity and BMI may prove illuminative as to whether and when cognitive benets depend in part on e4 status or whether the benets of physical activity or exercise may apply equally (c.f., Obisesan et al., 2012).
7
Head injury
History of head injury is commonly listed as a probable risk factor for AD. A metaanalysis of 15 case-control studies conducted up to 2001 suggested that the risk of AD is increased 1.5 times given a history of head injury but with eects more prominent for men at more than two-fold the risk compared with women which showed no signicant elevation in risk (Fleminger et al., 2003). Prospective studies of head injury avoid recall biases, though ndings are not clear as to the nature of the increased risk. A study of American male veterans of the Second World War avoided the problem of inaccurate recall by looking at head injuries that were documented by military hospital records (Plassman et al., 2000), nding that head injury in early adulthood was associated with AD in later life. A population-based study suggested that head injury may hasten the onset of AD but did not increase the risk per se (Nemetz et al., 1999). APOEe4 allele status may moderate the relationship between head injury and AD risk, where recovery from neurotrauma appears to be less optimal or extended for e4 carriers (Dardiotis et al., 2012) and increased Ab deposition after head injury has been reported for some individuals (Dardiotis et al., 2012). Indeed, a higher APOEe4 allele frequency has been noted among those with Ab deposition after head injury versus those without Ab
eLS & 2013, John Wiley & Sons, Ltd. www.els.net
Alzheimer Disease: Genetic and Environmental Influences
Leisure activities
Engagement in a variety of leisure activities has become a focus of research in the last decade and ndings have promoted notions of use it or lose it. Above, the ndings on physical activity are discussed and thus cognitive and socially oriented activities are focused on here. Engagement in cognitive activities such as reading, puzzles, card games or playing a musical instrument may be benecial to reducing the risk of AD according to prospective cohort studies (Hertzog et al., 2009; Reitz et al., 2011). This eect appears to hold even when controlling for other types of activities (e.g. Wilson et al., 2007). Similar to the physical activity literature, the evidence is less certain as to the benets of short-term cognitive exercise versus cognitive engagement patterns developed and maintained over the life course. For example, levels of engagement in cognitively oriented leisure activities are related to educational attainment achieved in earlier adulthood (Gatz et al., 2006a). Moreover, short-term cognitive-training benets appear to be specic to the type of cognitive task that individuals are trained on rather than showing global benets (e.g. training on speed of processing tasks benet speed of processing abilities but does not enhance shortterm memory, see Hertzog et al., 2009; Reitz et al., 2011). Participation in socially oriented activities may be benecial to the maintenance of cognitive functioning and a reduced risk of AD (Hertzog et al., 2009), although more conclusive evidence is needed. Change in cognitive health may aect level of participation in leisure activities (Fratiglioni et al., 2004). Thus, when social activities are assessed during the life course may be important to evaluating the directionality of the associations with AD risk. Moreover, the quality or perceptions of social relationships are not always included in studies of social networks, which may aect ndings (Fratiglioni et al., 2004; Hertzog et al., 2009). Some of the compelling evidence to date includes ndings such as: the size of social networks is associated with higher cognitive performance, particularly for memory tasks, and reduced AD-like neuropathology at autopsy (amyloid plaque load and density of neurobillary tangles) (Bennett et al., 2006), suggesting that social interactions may support cognitive reserve. Overall, the direction of eect of the associations among leisure activities is not entirely clear; for example, does engagement in social, cognitive or even physical activities mitigate AD risk by bolstering cognitive or brain reserve or do they act as a signal of an individuals state of health or capacity? (cf., Bennett et al., 2006). Moreover, the unique benets of leisure activity types are not clear; for example, to what extent does physical activity directly promote cognitive health versus indirectly through social interaction components that may be inherent to some physical activities? (Miller et al., 2012).
protective factor against AD (McGeer and McGeer, 2007). Activation of factors associated with inammatory processes in the brains of AD patients, such as microglial activation and the presence of inammatory cytokines, suggests that the possibly protective eect of NSAIDs may not be spurious. Indeed, an analysis of American twins discordant for AD reported that the unaected twin was more likely to use anti-inammatory drugs than the aected twin (Breitner et al., 1994). However, a recent evaluation of 14 randomised-controlled trials suggests that NSAIDs are not an eective treatment for already diagnosed AD patients (Jaturapatporn et al., 2012). More work is required to understand the role of inammatory processes on AD risk and the (lack of) eectiveness of NSAIDs as a putative treatment of AD.
Summary
The described risk factors and protective factors have triggered the formulation of interesting hypotheses relating to the aetiology of AD. Other proposed risk factors, which vary in terms of empirical support, include history of depression, smoking, diabetes, dietary factors (e.g. possible reduced risk with adherence to a Mediterranean-style diet) and serum lipid levels (Reitz et al., 2011). Overall, methodological issues and complexity in the aetiology of AD may hinder more denitive conclusions regarding environmental risk and protective factors for AD. Methodological problems include: biased recall of risk factors; reliance on single reporters (self-report or proxy informants) without other validation sources; participant dropout in longitudinal studies; and poor matching of AD cases to control subjects. To some extent, prospective studies have added greater weight to some of the putative factors. However, randomised-controlled trials are needed to evaluate many of the possible treatments or interventions (Reitz et al., 2011). Lastly, researchers need to consider the multifactorial bases of the risk factors themselves (van Dongen et al., 2012) in order to understand more clearly their relationship to AD risk. Twin designs represent an especially useful and informative way to progress in understanding about interactions between environmental and genetic risk factors (van Dongen et al., 2012), whereby analysis of genotypic background or environmental exposure can be fully controlled. Overcoming these and other methodological problems will further our knowledge of risk factor mechanisms and will lead to greater understanding of AD aetiology.
Conclusions
Although a substantial portion of the liability of AD may be accounted for by genetic factors, a signicant role for environmental factors is likely. Twin studies provide heritability estimates that suggest that the relative genetic contribution to the liability for AD may be as high as 79%, though not 100%, implying that environmental inuences
Nonsteroidal anti-inflammatory drugs
Several studies have suggested that the long-term use of nonsteroidal anti-inammatory drugs (NSAIDs) may be a
8
eLS & 2013, John Wiley & Sons, Ltd. www.els.net
Alzheimer Disease: Genetic and Environmental Influences
are also important. The APOEe4 allele, the best documented of possible genetic risk factors for late-onset AD, probably accounts for less than one quarter of all AD cases. New evidence for the inuence of other genes has emerged, though further research is necessary to evaluate the small fraction of the genetic risk for the disease that they explain. Notably, other risk factors and protective factors appear to play a role in AD risk, such as education, head injury and NSAIDs use. Among the more interesting directions in research are geneenvironment interactions. The interaction of environmental factors with genetic risk may provide further clues about underlying mechanisms. Studies combining molecular genetics and behavioural genetics will be helpful in uncovering the complexities of geneenvironment interactions and the roles of specic genes and risk factors contributing to liability for AD. Moreover, the gap between the small amount of variation contributed by common susceptibility genes and the substantial heritability observed in twin and family studies may be further claried. Altogether, a developmental longitudinal perspective on the salience of (and interaction among) particular risk and protective factors over the life course may increase an understanding of AD etiologies and illuminate potential points of intervention. See also: Alzheimer Disease, Genetics of; Genetics of Dementia
References
Albert MS, DeKosky ST, Dickson D et al. (2011) The diagnosis of mild cognitive impairment due to Alzheimers disease: recommendations from the National Institute on Aging-Alzheimers Association workgroups on diagnostic guidelines for Alzheimers disease. Alzheimers and Dementia 7(3): 270279. doi: 10.1016/j.jalz.2011.03.008. Alzheimers Association (2012) Alzheimers disease facts and gures. Alzheimers and Dementia 8(2): 131168. doi: 10.1016/ j.jalz.2012.02.001. Bennett DA, Schneider JA, Tang Y, Arnold SE and Wilson RS (2006) The eect of social networks on the relation between Alzheimers disease pathology and level of cognitive function in old people: a longitudinal cohort study. Lancet Neurology 5(5): 406412. doi: S1474-4422(06)70417-3 [pii] 10.1016/S14744422(06)70417-3. Bergem AL, Engedal K and Kringlen E (1997) The role of heredity in late-onset Alzheimer disease and vascular dementia. A twin study. Archives of General Psychiatry 54(3): 264270. Blacker D, Haines JL, Rodes L et al. (1997) ApoE-4 and age at onset of Alzheimers disease: the NIMH genetics initiative. Neurology 48(1): 139147. Breitner JC, Gau BA, Welsh KA et al. (1994) Inverse association of anti-inammatory treatments and Alzheimers disease: initial results of a co-twin control study. Neurology 44(2): 227232. Breitner JC, Welsh KA, Gau BA et al. (1995) Alzheimers disease in the National Academy of SciencesNational Research Council Registry of Aging Twin Veterans. III. Detection of cases, longitudinal results, and observations on twin concordance. Archives of Neurology 52(8): 763771.
Brookmeyer R, Evans DA, Hebert L et al. (2011) National estimates of the prevalence of Alzheimers disease in the United States. Alzheimers and Dementia 7(1): 6173. doi: 10.1016/ j.jalz.2010.11.007. Colantuoni E, Surplus G, Hackman A, Arrighi HM and Brookmeyer R (2010) Web-based application to project the burden of Alzheimers disease. Alzheimers and Dementia 6(5): 425428. doi: 10.1016/j.jalz.2010.01.014. Dahl AK, Hassing LB, Fransson EI et al. (2012) Body mass index across midlife and cognitive change in late life. International Journal of Obesity. doi: 10.1038/ijo.2012.37. Dardiotis E, Grigoriadis S and Hadjigeorgiou GM (2012) Genetic factors inuencing outcome from neurotrauma. Current Opinion in Psychiatry 25(3): 231238. doi: 10.1097/YCO. 0b013e3283523c0e. Daw EW, Payami H, Nemens EJ et al. (2000) The number of trait loci in late-onset Alzheimer disease. American Journal of Human Genetics 66(1): 196204. doi: 10.1086/302710. van Dongen J, Slagboom PE, Draisma HH, Martin NG and Boomsma DI (2012) The continuing value of twin studies in the omics era. Nature Reviews Genetics 13(9): 640653. doi: 10. 1038/nrg3243. Egert S, Rimbach G and Huebbe P (2012) ApoE genotype: from geographic distribution to function and responsiveness to dietary factors. Proceedings of the Nutrition Society 71(3): 115. doi: S0029665112000249 [pii] 10.1017/ S0029665112000249. Erickson KI, Miller DL, Weinstein AM, Akl SL and Banducci S (2012) Physical activity and brain plasticity in late adulthood: a conceptual and comprehensive review. Ageing Research 3: 34 47. Fleminger S, Oliver DL, Lovestone S, Rabe-Hesketh S and Giora A (2003) Head injury as a risk factor for Alzheimers disease: the evidence 10 years on; a partial replication. Journal of Neurology, Neurosurgery, and Psychiatry 74(7): 857862. Fratiglioni L, Paillard-Borg S and Winblad B (2004) An active and socially integrated lifestyle in late life might protect against dementia. Lancet Neurology 3(6): 343353. doi: 10.1016/S14744422(04)00767-7. Galimberti D and Scarpini E (2012) Progress in Alzheimers disease. Journal of Neurology 259(2): 201211. doi: 10.1007/ s00415-011-6145-3. Gatz M, Pedersen NL, Berg S et al. (1997) Heritability for Alzheimers disease: the study of dementia in Swedish twins. Journal of Gerontology. Series A, Biological Sciences and Medical Sciences 52(2): M117M125. Gatz M, Prescott CA and Pedersen NL (2006a) Lifestyle risk and delaying factors. Alzheimer Disease and Associated Disorders 20(3 Suppl. 2): S84S88. Gatz M, Reynolds CA, Fratiglioni L et al. (2006b) Role of genes and environments for explaining Alzheimer disease. Archives of General Psychiatry 63(2): 168174. Genin E, Hannequin D, Wallon D et al. (2011) APOE and Alzheimer disease: a major gene with semi-dominant inheritance. Molecular Psychiatry 16(9): 903907. doi: 10.1038/mp.2011.52. Goldman JS, Hahn SE, Catania JW et al. (2011) Genetic counseling and testing for Alzheimer disease: joint practice guidelines of the American College of Medical Genetics and the National Society of Genetic Counselors. Genetics in Medicine 13(6): 597605. doi: 10.1097/GIM.0b013e31821d69b8.
eLS & 2013, John Wiley & Sons, Ltd. www.els.net
Alzheimer Disease: Genetic and Environmental Influences
Head D, Bugg JM, Goate AM et al. (2012) Exercise engagement as a moderator of the eects of APOE genotype on amyloid deposition. Archives of Neurology. doi: 10.1001/archneurol.2011.845. Hertzog C, Kramer AF, Wilson RS and Lindenberger U (2009) Enrichment eects on adult cognitive development. Psychological Science in the Public Interest 9(1): 165. doi: 10.1111/ j.1539-6053.2009.01034.x. Hong MG, Reynolds CA, Feldman AL et al. (2012) Genome-wide and gene-based association implicates FRMD6 in Alzheimer disease. Human Mutation 33(3): 521529. doi: 10.1002/ humu.22009. Ishii H, Meguro K, Ishizaki J et al. (1999) Prevalence of senile dementia in a rural community in Japan: the Tajiri project. Archives of Gerontology and Geriatrics 29(3): 249265. Jaturapatporn D, Isaac MG, McCleery J and Tabet N (2012) Aspirin, steroidal and non-steroidal anti-inammatory drugs for the treatment of Alzheimers disease. Cochrane Database of Systematic Reviews 2: CD006378. doi: 10.1002/14651858. CD006378.pub2. Kallman F (1956) Genetic aspects of mental disorders in later life. In: Kaplan O (ed.) Mental Disorders in Later Life, 2nd edn, pp. 2646. Stanford, CA: Stanford University Press. Manly JJ and Mayeux R (2004) 4. Ethnic Dierences in Dementia and Alzheimers Disease. In: Anderson NB, Bulatao RA and Cohen B (eds) Critical Perspectives on Racial and Ethnic Differences in Health in Late Life, pp. 95141. Washington (DC): National Academies Press. Mattson MP (2004) Pathways towards and away from Alzheimers disease. Nature 430(7000): 631639. doi: 10.1038/ nature02621. Mayeux R and Stern Y (2012) Epidemiology of Alzheimer disease. Cold Spring Harbor Perspectives in Medicine 2(8): 118. doi: 10.1101/cshperspect.a006239. McGeer PL and McGeer EG (2007) NSAIDs and Alzheimer disease: epidemiological, animal model and clinical studies. Neurobiology of Aging 28(5): 639647. doi: 10.1016/ j.neurobiolaging.2006.03.013. McKhann GM, Knopman DS, Chertkow H et al. (2011) The diagnosis of dementia due to Alzheimers disease: recommendations from the National Institute on Aging-Alzheimers Association workgroups on diagnostic guidelines for Alzheimers disease. Alzheimers and Dementia 7(3): 263269. doi: 10.1016/j.jalz.2011.03.005. Miller DI, Taler V, Davidson PS and Messier C (2012) Measuring the impact of exercise on cognitive aging: methodological issues. Neurobiology of Aging 33(3): 622, e629-643. doi: 10.1016/ j.neurobiolaging.2011.02.020. Nelson PT, Alafuzo I, Bigio EH et al. (2012) Correlation of Alzheimer disease neuropathologic changes with cognitive status: a review of the literature. Journal of Neuropathology and Experimental Neurology 71(5): 362381. doi: 10.1097/NEN. 0b013e31825018f7. Nemetz PN, Leibson C, Naessens JM et al. (1999) Traumatic brain injury and time to onset of Alzheimers disease: a population-based study. American Journal of Epidemiology 149(1): 3240. Obisesan TO, Umar N, Paluvoi N and Gillum RF (2012) Association of leisure-time physical activity with cognition by apolipoprotein-E genotype in persons aged 60 years and over: the
National Health and Nutrition Examination Survey (NHANES-III). Clinical Interventions in Aging 7: 3543. doi: 10.2147/CIA.S26794. Perl DP (2010) Neuropathology of Alzheimers disease. Mount Sinai Journal of Medicine 77(1): 3242. doi: 10.1002/ msj.20157. Plassman BL, Havlik RJ, Steens DC et al. (2000) Documented head injury in early adulthood and risk of Alzheimers disease and other dementias. Neurology 55(8): 11581166. Raiha I, Kaprio J, Koskenvuo M, Rajala T and Sourander L (1996) Alzheimers disease in Finnish twins. Lancet 347(9001): 573578. Reitz C, Brayne C and Mayeux R (2011) Epidemiology of Alzheimer disease. Nature Reviews. Neurology 7(3): 137152. doi: 10.1038/nrneurol.2011.2. Schellenberg GD and Montine TJ (2012) The genetics and neuropathology of Alzheimers disease. Acta Neuropathologica. doi: 10.1007/s00401-012-0996-2. Sharp ES and Gatz M (2011) Relationship between education and dementia: an updated systematic review. Alzheimer Disease and Associated Disorders 25(4): 289304. doi: 10.1097/WAD. 0b013e318211c83c. Silverman JM, Ciresi G, Smith C J, Marin D B and SchnaiderBeeri M (2005) Variability of familial risk of Alzheimer disease across the late life span. Archives of General Psychiatry 62(5): 565573. doi: 10.1001/archpsyc.62.5.565. Sperling RA, Aisen PS, Beckett LA et al. (2011) Toward dening the preclinical stages of Alzheimers disease: recommendations from the National Institute on Aging-Alzheimers Association workgroups on diagnostic guidelines for Alzheimers disease. Alzheimers and Dementia 7(3): 280292. doi: 10.1016/ j.jalz.2011.03.003. Stern Y (2009) Cognitive reserve. Neuropsychologia 47(10): 2015 2028. doi: 10.1016/j.neuropsychologia.2009.03.004. Tanaka N, Abe-Dohmae S, Iwamoto N and Yokoyama S (2011) Roles of ATP-binding cassette transporter A7 in cholesterol homeostasis and host defense system. Journal of Atherosclerosis and Thrombosis 18(4): 274281. Verghese PB, Castellano JM and Holtzman DM (2011) Apolipoprotein E in Alzheimers disease and other neurological disorders. Lancet Neurology 10(3): 241252. doi: 10.1016/S14744422(10)70325-2. White L, Petrovitch H, Ross GW et al. (1996) Prevalence of dementia in older Japanese-American men in Hawaii: the Honolulu-Asia Aging Study. Journal of the American Medical Association 276(12): 955960. Wilson RS, Scherr PA, Schneider JA, Tang Y and Bennett DA (2007) Relation of cognitive activity to risk of developing Alzheimer disease. Neurology 69(20): 19111920. doi: 10.1212/ 01.wnl.0000271087.67782.cb.
Further Reading
Esiri MM and Chance SA (2012) Cognitive reserve, cortical plasticity and resistance to Alzheimers disease. Alzheimers Research and Therapy 4(2): 7. doi: 10.1186/alzrt105. Jagust WJ and Mormino EC (2011) Lifespan brain activity, bamyloid, and Alzheimers disease. Trends in Cognitive Sciences 15(11): 520526.
10
eLS & 2013, John Wiley & Sons, Ltd. www.els.net
Alzheimer Disease: Genetic and Environmental Influences
Williams JW, Plassman BL, Burke J and Benjamin S (2010) Preventing Alzheimers disease and cognitive decline [Review]. Evidence Report/Technology Assessment193: 1727.
Web Links
Alzheimers Association: alz.org [Accessed 9 September 2012].
Bertram L, McQueen M, Mullin K, Blacker D and Tanzi R. The AlzGene Database. Alzheimer Research Forum. Available at: http://www.alzgene.org. [Accessed 9 September 2012]. Internet-based Forecasting of the Burden of Alzheimers Disease: iFBAD http://www.biostat.jhsph.edu/project/globalAD/ indexpage2.htm [Accessed 9 September 2012].
eLS & 2013, John Wiley & Sons, Ltd. www.els.net
11
You might also like
- Fire Watcher Duties (7) - 6Document1 pageFire Watcher Duties (7) - 6karpanaiNo ratings yet
- NFPA Codes & Standards - 3Document1 pageNFPA Codes & Standards - 3karpanai100% (1)
- NFPA Codes & Standards - 2Document1 pageNFPA Codes & Standards - 2karpanai100% (2)
- Responsibilit Denfition PDFDocument1 pageResponsibilit Denfition PDFkarpanaiNo ratings yet
- Chemical Engineering Science: Yanchang Wang, Fazhi Zhang, Sailong Xu, Lan Yang, Dianqing Li, David G. Evans, Xue DuanDocument7 pagesChemical Engineering Science: Yanchang Wang, Fazhi Zhang, Sailong Xu, Lan Yang, Dianqing Li, David G. Evans, Xue DuankarpanaiNo ratings yet
- NFPA Codes & Standards - 1Document1 pageNFPA Codes & Standards - 1karpanaiNo ratings yet
- Near Miss - Identification Made Simple en & HI - PDF-1 - 4Document1 pageNear Miss - Identification Made Simple en & HI - PDF-1 - 4karpanaiNo ratings yet
- Permits To Work - Scotland PDFDocument14 pagesPermits To Work - Scotland PDFFOZCANNo ratings yet
- Report near misses to improve workplace safetyDocument1 pageReport near misses to improve workplace safetykarpanaiNo ratings yet
- Near Miss - Identification Made Simple en & HI - PDF-1 - 8Document1 pageNear Miss - Identification Made Simple en & HI - PDF-1 - 8karpanaiNo ratings yet
- Occupational exposure limits for chemical substancesDocument1 pageOccupational exposure limits for chemical substanceskarpanaiNo ratings yet
- SOP Fire Blankets PDFDocument4 pagesSOP Fire Blankets PDFkarpanaiNo ratings yet
- Application of CFD Technique To Simulate Enhanced Oil RecoveryDocument23 pagesApplication of CFD Technique To Simulate Enhanced Oil RecoverykarpanaiNo ratings yet
- Form of Application For Approval of Safety Equipment For Use in MinesDocument5 pagesForm of Application For Approval of Safety Equipment For Use in MineskarpanaiNo ratings yet
- Chemical Engineering Science Parametric Effects Taguchi ApproachDocument11 pagesChemical Engineering Science Parametric Effects Taguchi ApproachkarpanaiNo ratings yet
- Organises An: Intellectual Property Rights Awareness ProgrammeDocument1 pageOrganises An: Intellectual Property Rights Awareness ProgrammekarpanaiNo ratings yet
- Form For Field Trial Report of Equipment-MaterialDocument22 pagesForm For Field Trial Report of Equipment-MaterialkarpanaiNo ratings yet
- Forms For Permission Under OMR 1984Document5 pagesForms For Permission Under OMR 1984karpanaiNo ratings yet
- J Jclepro 2020 120777Document56 pagesJ Jclepro 2020 120777karpanaiNo ratings yet
- Regulations & Syllabus 2016-2017Document98 pagesRegulations & Syllabus 2016-2017kannanNo ratings yet
- Fenton-Biostimulation Sequential Treatment of A Petroleum-Contaminated Soil Amended With Oil Palm Bagasse (Elaeis Guineensis)Document17 pagesFenton-Biostimulation Sequential Treatment of A Petroleum-Contaminated Soil Amended With Oil Palm Bagasse (Elaeis Guineensis)karpanaiNo ratings yet
- No Injury-No Incident?: "Near Misses"Document15 pagesNo Injury-No Incident?: "Near Misses"Theresa West100% (1)
- Tube Coating - ArticleDocument5 pagesTube Coating - ArticlekarpanaiNo ratings yet
- Isolation, Screening, and Crude Oil Degradation BacteriaDocument13 pagesIsolation, Screening, and Crude Oil Degradation BacteriakarpanaiNo ratings yet
- A Novel Sophorolipid-Producing Candida Keroseneae GBME-IAUF-2 As A Potential Agent in Microbial Enhanced Oil Recovery (MEOR)Document8 pagesA Novel Sophorolipid-Producing Candida Keroseneae GBME-IAUF-2 As A Potential Agent in Microbial Enhanced Oil Recovery (MEOR)karpanaiNo ratings yet
- Discussion Points MAH Barriers: Date of Event: 23Document1 pageDiscussion Points MAH Barriers: Date of Event: 23karpanaiNo ratings yet
- Fmicb 11 569019Document13 pagesFmicb 11 569019karpanaiNo ratings yet
- Adsorption Kinetics of Arsenic (V) On Nanoscale Zero-Valent Iron Supported by Activated CarbonDocument12 pagesAdsorption Kinetics of Arsenic (V) On Nanoscale Zero-Valent Iron Supported by Activated CarbonkarpanaiNo ratings yet
- Discussion Points MAH Barriers: Date of Event: 6Document1 pageDiscussion Points MAH Barriers: Date of Event: 6karpanaiNo ratings yet
- SFO A ParticipantsHandbookDocument336 pagesSFO A ParticipantsHandbookkarpanaiNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5784)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- A Critical Appraisal of Amyloid-β-targeting Therapies for Alzheimer Disease 2019 ReviewDocument16 pagesA Critical Appraisal of Amyloid-β-targeting Therapies for Alzheimer Disease 2019 Review畏No ratings yet
- EA Lancet 2021Document14 pagesEA Lancet 2021Felipe SennNo ratings yet
- CSH Perspectives Rev - Apolipoprotein E and Apolipoprotein E Receptors - Normal Biology and Roles in ADDocument23 pagesCSH Perspectives Rev - Apolipoprotein E and Apolipoprotein E Receptors - Normal Biology and Roles in ADGeneziz DiazNo ratings yet
- Dementia and Cognitive Impairment Epidemiology, Diagnosis, and TreatmentDocument24 pagesDementia and Cognitive Impairment Epidemiology, Diagnosis, and TreatmentPutri YunandaNo ratings yet
- Alzheimer Disease.4Document28 pagesAlzheimer Disease.4Nicki Pinzon NariñoNo ratings yet
- 1file NaotherDocument3 pages1file NaotherzeeshanNo ratings yet
- Schizophrenia PPT For EditDocument75 pagesSchizophrenia PPT For EditCharline A. Radislao100% (1)
- Alzheimer Disease Including Focal Presentations PDFDocument14 pagesAlzheimer Disease Including Focal Presentations PDFpiedrahitasaNo ratings yet
- Randox - Immunoturbidimetric ProteinsDocument32 pagesRandox - Immunoturbidimetric ProteinsCoțovanu IulianNo ratings yet
- Best Diets For Cognitive Fitness: HarvardDocument7 pagesBest Diets For Cognitive Fitness: HarvardAdin100% (1)
- Review HMG-CoA ReductaseDocument10 pagesReview HMG-CoA ReductaseFrancisco TapiaNo ratings yet
- Egg Consumption and Risk of Incident Type 2 Diabetes in Men: The Kuopio Ischaemic Heart Disease Risk Factor StudyDocument9 pagesEgg Consumption and Risk of Incident Type 2 Diabetes in Men: The Kuopio Ischaemic Heart Disease Risk Factor StudyMatías RamírezNo ratings yet
- 304 Stanbul Yabanc 305 Lar 304 231 in T 252 RK 231 e 199 Al 305 351 Ma Kitab 305 A2Document33 pages304 Stanbul Yabanc 305 Lar 304 231 in T 252 RK 231 e 199 Al 305 351 Ma Kitab 305 A2Eleni KartsonakiNo ratings yet
- NEET PG 2019 Question Paper With SolutionsDocument364 pagesNEET PG 2019 Question Paper With SolutionsmedpoxNo ratings yet
- International Experts Reach Consensus on Mild Cognitive Impairment DefinitionDocument7 pagesInternational Experts Reach Consensus on Mild Cognitive Impairment DefinitionRoxana SanduNo ratings yet
- Alzheimer's Disease Research PaperDocument24 pagesAlzheimer's Disease Research Papershayne86% (22)
- Mini Project Report FinalDocument40 pagesMini Project Report Final【BEING MYSTIC】 (teen rider)No ratings yet
- Apoe4 AdDocument23 pagesApoe4 AdHelena QuintNo ratings yet
- Osteoporosis: Pathophysiology and Clinical ManagementDocument628 pagesOsteoporosis: Pathophysiology and Clinical ManagementKartika AnggakusumaNo ratings yet
- Session 5Document28 pagesSession 5IndhumathiNo ratings yet
- Introduction To Lipids and LipoproteinsDocument24 pagesIntroduction To Lipids and LipoproteinsYoungFanjiensNo ratings yet
- Cognitive Performance After Postoperative Pituitary Radiotherapy: A Dosimetric Study of The Hippocampus and The Prefrontal CortexDocument9 pagesCognitive Performance After Postoperative Pituitary Radiotherapy: A Dosimetric Study of The Hippocampus and The Prefrontal CortexManishKondapuramNo ratings yet
- PCR Tests and Vaccines DiscussedDocument74 pagesPCR Tests and Vaccines DiscussedConstantin RaduNo ratings yet
- Lipids Lipoproteins ApolipoproteinsDocument26 pagesLipids Lipoproteins ApolipoproteinssakuraleeshaoranNo ratings yet
- Genetics of Sex Differences in Brain & BehaviorDocument20 pagesGenetics of Sex Differences in Brain & BehaviorAlice Andrews100% (1)
- Clinical Features of Alzheimer's DiseaseDocument100 pagesClinical Features of Alzheimer's Diseasedrkadiyala2No ratings yet
- (2009) Study Guide To GeriatricPsychiatry - QsDocument41 pages(2009) Study Guide To GeriatricPsychiatry - QsPepe Garcia Estebez100% (1)
- Severe Mini-Mental State Examination PDFDocument1 pageSevere Mini-Mental State Examination PDFKelly YoungNo ratings yet
- Alzheimer's DiseaseDocument31 pagesAlzheimer's DiseasePAULA ITZEL AVALOS POLANCONo ratings yet
- Nutrigenomics and Cardiovascular DiseaseDocument19 pagesNutrigenomics and Cardiovascular DiseaseAssignmentLab.comNo ratings yet