Professional Documents
Culture Documents
Ultrasound Guided Drainage of Submasseteric Space Abscesses Gudi SS, Sarvadnya J, Hallur N, Sikkerimath B C - Ann Maxillofac Surg PDF
Uploaded by
Gabriel MiranceaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ultrasound Guided Drainage of Submasseteric Space Abscesses Gudi SS, Sarvadnya J, Hallur N, Sikkerimath B C - Ann Maxillofac Surg PDF
Uploaded by
Gabriel MiranceaCopyright:
Available Formats
22.04.
2013
Ultrasound guided drainage of submasseteric space abscesses Gudi SS, Sarvadnya J, Hallur N, Sikkerimath B C - Ann Maxillofac Surg
Home - About us - Editorial board - Search - Ahead of print - Current issue - Archives - Instructions - Subscribe - Contacts - Advertise - Login
Users Online: 15
Journal is indexed with PubMed
Search
Share Share Share Share Share Share More
Similar in PUBMED ORIGINAL ARTICLE - PROSPECTIVE STUDY Year : 2013 | Volume : 3 | Issue : 1 | Page : 31-34 Ultrasound guided drainage of submasseteric space abscesses Santosh S Gudi1, Jagadish Sarvadnya2, Neelakamal Hallur3, BC Sikkerimath1 1 Department of Oral and Maxillofacial Surgery, P.M.N.M Dental College and Hospital, Bagalkot, Karnataka, India 2 Fellow in Department of Oral Oncology, Kidwai Memorial Institute of Oncology, Bengaluru, Karnataka, India 3 HOD of Oral and Maxillofacial Surgery, Al-Badar Dental College and Hospital, Gulbarga, Karnataka, India Date of Web Publication 4-Apr-2013 Search Pubmed for Gudi SS Sarvadnya J Hallur N Sikkerimath B C
GO
Search in Google Scholar for Gudi SS Sarvadnya J Hallur N Sikkerimath B C Related articles Submasseteric space transducer ultrasonography Access Statistics Email Alert * Add to My List * * Registration required (free)
Correspondence Address : Santosh S Gudi Department of Oral and Maxillofacial Surgery, P.M.N.M Dental College and Hospital, Bagalkot, Karnataka India
DOI: 10.4103/2231-0746.110074
Abstract Background and Objectives: The objective of this study was to evaluate the usefulness of ultrasound guided surgical drainage in submasseteric space abscess of odontogenic origin without incision. Materials and Methods : Eleven patients (4 males and 7 females) aged 18 to 36 years were included in this study. Each patient had clinically and radiologically diagnosed submasseteric space abscesses of odontogenic origin. All the patients underwent ultrasound guided drainage by using 5.7 MHz B-mode, gray scale, ultrasound scanner. The aspirated pus was sent for microbiological culture and sensitivity tests. All the patients were given a prescription of antibiotics like Amoxicillin with Clavulanate in a dose of 625 mg 8 hourly daily, Metronidazole 400 mg 8 h daily and analgesic Diclofenac potassium in a dose of 50 mg 8 h daily. Infection was considered resolving when the following criteria were met like ceased or minimal drainage. Results: There was successful resolution of abscess in 10 cases, 1 case underwent incision and drainage because of spread of infection to other spaces. Conclusion: This study on 11 cases supported ultrasonography as an intraoperative aid in the assessment of the abscess cavity and its real-time imaging facility will help in the location and drainage of the abscess cavity effectively. It avoids large, unsightly, postoperative facial scars and often eliminates the need of general anesthesia and hospitalization. Keywords: Submasseteric space, transducer, ultrasonography Article Access Statistics Viewed 53 Printed 2 Emailed 0 PDF Downloaded 9 Comments [Add]
Total downloads in last 2 months
In this article Abstract Introduction Materials and Me... Results Discussion Conclusion References Article Figures Article Tables
How to cite this article: Gudi SS, Sarvadnya J, Hallur N, Sikkerimath B C. Ultrasound guided drainage of submasseteric space abscesses. Ann Maxillofac Surg 2013;3:31-4 How to cite this URL: Gudi SS, Sarvadnya J, Hallur N, Sikkerimath B C. Ultrasound guided drainage of submasseteric space abscesses. Ann Maxillofac Surg [serial online] 2013 [cited 2013 Apr 22];3:31-4. Available from: http://www.amsjournal.com/text.asp?
www.amsjournal.com/article.asp?issn=2231-0746;year=2013;volume=3;issue=1;spage=31;epage=34;aulast=Gudi
1/5
22.04.2013
Maxillofac Surg [serial online] 2013 [cited 2013 Apr 22];3:31-4. Available from: http://www.amsjournal.com/text.asp? 2013/3/1/31/110074
Ultrasound guided drainage of submasseteric space abscesses Gudi SS, Sarvadnya J, Hallur N, Sikkerimath B C - Ann Maxillofac Surg
Apr 2013 64
Introduction
Acute fascial space infections are common emergencies presenting to the maxillofacial surgeons. The dilemma often is to differentiate an abscess from cellulitis and determine whether antibiotic coverage is enough or the incision and drainage is needed and whether patency of the incision is to be maintained. The anatomic location of the abscesses in patients with odontogenic infection is commonly determined by the physical examination, but the abscesses of the deep subcutaneous layer can be difficult to locate. In these cases blind surgical drainage procedure can result in inadequate drainage tissue trauma, unnecessarily extensive incisions, excess time, pain, and failure to locate and evacuate the abscess cavity. [1] Submasseteric space (SMS) abscess usually presents as a painful, firm swelling over the posterior part of the ramus of the mandible [Figure 1]a and b. Severe trismus reflects involvement of the overlying masseter muscle. This leads to the severe restriction in the mastication and swallowing and patient usually presents with dehydration and fever. [2] Figure 1: Preoperative view: a) Frontal, b) Lateral Click here to view
Translate
Select Language
Gadgets powered by Google
Diagnostic ultrasonography (USG) is widely used to identify the presence of fluid collections preoperatively in head and neck region. It is an effective diagnostic tool to confirm abscess formation in the superficial spaces and is highly predictable in determining the stage of infection. [3] Presurgical assessment or evaluation of SMS using CT/MRI has yielded good results but not without cost factor. It seems the role of USG in diagnosis of SMS is effective but its role in treatment of SMS is not clear due to very few number of studies. The objective of this study is to evaluate the usefulness of USG guided surgical drainage in SMS abscesses of odontogenic origin without incision and drainage.
Materials and Methods
This study included a total of 11 patients (4 men and 7 women, from 2008 to 2010) age ranging between 18-36 years; average age being 26 years, with confirmed diagnosis of unilateral SMS abscess of odontogenic origin were subjected to thorough detailed clinical examination and radiographic examination (OPG). Preoperative routine blood investigations were performed and specific blood investigation in required cases (few) done to rule out the presence of underlying medical element like uncontrolled diabetes. Surgical procedure Patient was explained the surgical procedure and informed, written and verbal consent was taken. Under aseptic measures, a high resolution ultrasound scan was performed using a 5.7 linear array probe in direct contact with skin surface using sterile ultrasound gel as the coupling agent [Figure 2]. Patient was in supine position with the head tilted towards the unaffected side. After visualizing the abscess cavity under the guidance of the ultrasound, the probe position was adjusted so that the intended puncture point of the abscess was aligned with the imaginary midline of the probe and distance from skin surface to the required depth of the needle insertion was measured accurately [Figure 3]. A sixteen gauge intravenous catheter with the trocar needle mounted on sterile 10 ml disposable plastic syringe was inserted freehand at an angle perpendicular to the scanning plane [Figure 4]. During the procedure the patient was instructed to open his/her mouth maximally and not to move, breathe deeply, or swallow during the needle insertion to avoid the shifting of the image. The collected pus was sent for microbiological culture sensitivity tests. The needle was withdrawn leaving catheter in the site. The catheter was carefully taped to the skin and covered with the dressing, till complete cessation of pus. All the patients were prescribed a standard dose of empirical therapy of oral antibiotics covering both aerobic, as well as anaerobic microorganisms (Tab. Augmentin 625 mg 8 hourly and Tab. Metronidazole 400 mg 8 h) along with analgesic Tab. Diclofenac potassium in a dose of 50 mg 8 hourly daily for 5 days. All patients were treated on out patient basis and extraction of offending tooth was done after satisfactory opening of mouth. All patients were advised good home care, maintenance of oral hygiene and to perform mouth opening exercise. Patients were evaluated for 2 to 3 days postoperatively and if required second follow-up was done on 5 th postoperative day. This was done till complete resolution of all the sign and symptoms of space infection was attained [Figure 5]a and b. Figure 2: Examination of swelling using Ultrasound transducer
www.amsjournal.com/article.asp?issn=2231-0746;year=2013;volume=3;issue=1;spage=31;epage=34;aulast=Gudi
Click here to view
2/5
22.04.2013
Ultrasound guided drainage of submasseteric space abscesses Gudi SS, Sarvadnya J, Hallur N, Sikkerimath B C - Ann Maxillofac Surg
Click here to view
Figure 3: Submasseteric space abscess Click here to view
Figure 4: Drainage of abscess Click here to view Figure 5: Postoperative view: a) Frontal, b)Lateral Click here to view
Results
In all the 11 patients, USG confirmed the clinical diagnosis of SMS abscess, of which 10 patient were treated successfully using USG guided drainage and one case went for incision and drainage due to involvement of adjacent spaces. Ninety percent of cases treated by USG guided drainage showed clear edge definition, homogenous pattern with hypoechoic intensity on USG while 10 percent (1 case) showed ill defined edge with homogenous and hypoechoic pattern [Table 1]. Out of 11 cases only 1 case which showed heterogenous pattern with hypoechoic intensity was treated by incision and drainage due to involvement of adjacent spaces. The average predetermined depth of all the cases before insertion of the needle into the abscess cavity on the ultrasound screen was 9.21 mm and mean actual depth of insertion was 9.5 mm. [Table 2] shows the amount of pus individually collected for each case and cessation of drainage in all 11 cases. The average individual case pus collected after ultrasound guided needle aspiration was 2.1 ml and table also shows the period of minimal drainage and cessation of pus. The average minimal drainage period was 1-2 days and average cessation period was 2 days (mode value). All the patients followed the routine postoperative visits and all the patients followed the instructions as given to them. Table 1: Details of submasseteric space abscess in 11 patients Click here to view Table 2: Amount of pus collected and cessation of pus drainage Click here to view
Discussion
Ultrasound is a recognized diagnostic tool in various medical fields and has recently been used in the oral and maxillofacial region. It offers potential advantage because it can be performed non-invasively, repeatedly, easily and even at the bedside. [4] Since USG is a non-ionizing device it offers advantages of multiple exposure. [5] There is no need for administration of any radiological contrast which is used in certain radiological techniques like CT scans, and angiography that may be possibly harmful to the patients with impaired organ function (e.g. renal failure or liver failure). The major feature that is unique to USG is the ability to recognize and verify deep body organs and lesions having similar density on conventional radiographic studies. The information gained through ultrasound, like other imaging modalities is optimal when coupled with the patients clinical findings. [6] The relatively blind surgical incision and drainage of abscess based on the diagnosis by physical examination may result in excessive tissue trauma, unnecessarily extensive incisions, excessive time, pain, and failure to locate and evacuate the abscess cavity completely. [7] Ultrasound pinpoints the relation of the abscess to the overlying skin, the accurate dimensions of the abscess cavity, and its precise depth below the skin surface. [3],[7] With the aid of high resolution transducer, USG shows the internal muscle structures more clearly than CT. [7] Sonographic reduction of echo intensity is interpreted as an echo free or hypoechoic region which is indicative of an abscess. [4] Although it is sometimes difficult to confirm the existence of an abscess without open
www.amsjournal.com/article.asp?issn=2231-0746;year=2013;volume=3;issue=1;spage=31;epage=34;aulast=Gudi 3/5
22.04.2013
region which is indicative of an abscess. [4] Although it is sometimes difficult to confirm the existence of an abscess without open surgery. It would be more appropriate to use USG aspiration, for verification of an area felt to correspond to an abscess. Change of pattern of hypoechoic area is known to result from pre-examination surgical treatment. The heterogeneous appearance may be a sign of healing process and can be important in follow-up examinations. [7] The needle tip was guided accurately into all the abscesses, through skin, masseter muscle, without misdirected and repetitive punctures, or injury to the vessels. The technique presented here reduces the needle insertion distance by inserting it perpendicular to the scanning plane at the midline of the probe. Although it is difficult to visualize the whole needle by this method, the location of the tip of the needle relative to the abscess is always visible on the display. In addition, this decreases risk of vessel injury and facilitates the introduction of a drain.
Ultrasound guided drainage of submasseteric space abscesses Gudi SS, Sarvadnya J, Hallur N, Sikkerimath B C - Ann Maxillofac Surg
Fouad A. Al-Belasy (2005) et al., opined that USG guided drainage can be effectively employed in treatment of SMS abscess. [4] Similar views are also held by Pandey, et al., although they used USG mainly for diagnosis of only five SMS abscesses. [8] The very high success rate (91%) of present study also support the findings of previous authors. Once the SMS abscess develops, therapeutic management requires early incision and drainage. However, in a patient presenting with marked trismus, incision and drainage would require a general anesthesia necessitating an intubation while awake, which adds to morbidity. To address this situation, needle or catheter aspiration with ultrasound guidance has been used as the initial method of treatment. As suggested by Fouad A. Al-Belasy a 16-gauge intravenous catheter can be used and left inside the abscess cavity to serve as drain and to allow the constant painless access to the infection. [4] Easy maneuvering probe into the correct position to obtain dependent part of the abscess, and absence or bearable pain during procedure makes it feasible. [9] The presence of even meager amount of pus (less than 1 ml), has been detected by USG probe, as evident in 40% cases of our study. This highlights the advantage of USG in detection of even minimum amount of fluid or pus. Another advantage of USG is the portable feature which can be used in real time during surgery. [5] When used intraoperatively in real time, the continuous imaging capability is far more useful to the surgeon than static images as represented by other modalities. [10],[11] Interestingly the visualization of in situ positioning and movement of the needle or other instrument on the ultrasound screen facilitates guidance to the surgeon. This study further illustrates the reliability of USG in imaging and adequacy in drainage of SMS abscess at the time of operation. Although USG is considered to be safe to use repeatedly, there are few reported cases of heating effect of diagnostic ultrasound, which can be overcome by simple B-mode scanner which is used in oral and maxillofacial surgery that has no risk of adverse heating. So B-mode ultrasound scanning procedures that use scanned beams was also employed in our study. [12] Additionally it is not possible with USG to evaluate soft tissue swelling medial to the vertical ramus of the mandible because of total reflection of USG, as the bony surface shields the deep tissues. [9]
Conclusion
This study recommends the use of USG not only for diagnosis of SMS abscess but also for real time intraoperative USG guided drainage of SMS abscess. Further the study may be of great value in diagnosis of maxillofacial space infections containing meager amount of pus or fluid.
References 1. Yusa H, Yoshida H, Ueno E, Onizawa K, Yanagawa T. Ultrasound-guided surgical drainage of face and neck abscesses. Int J Oral Maxilofac Surg 2002;31:328-29. Hupp JR, Ellis E III, Tucker MR. Contemprorary Oral and Maxillofacial Surgery. 5 th ed. Mosby; 2008. p. 324. Baurmash HD. Ultrasonography in the diagnosis and treatment of facial abscesses. J Oral Maxillofac Surg 1999;57:6356. Al-Belasy FA. Ultrasound-Guided Drainage of Submasseteric Space Abscesses. J Oral Maxillofac Surg 2005;63:36-41. Thiruchelvam JK, Songra AK, Ng SY. Intraoperative ultrasound imaging to aid abscess drainage-a technical note. Int J Oral Maxillofac Surg 2002;31:442-3. Wilson IR, Crocker EF, McKellar G, Rengaswamy V. An evaluation of the clinical applications of diagnostic Ultrasonography in oral surgery. Oral Surg Oral Med Oral Pathol 1989;67:242-8. Peleg M, Heyman Z, Ardekian L, Taicher S. The use of Ultrasonography as a diagnostic tool for superficial fascial space infection. J Oral Maxilofac Surg 1998;56:1129-31. Pandey PK, Umarani M, Kotrashetti S, Baliga S. Evaluation of Ultrasonography as a Diagnostic Tool in Maxillofacial Space Infections. J Oral Maxillofac Res 2011;2:e4.
2. 3.
4. 5.
6.
7.
8.
www.amsjournal.com/article.asp?issn=2231-0746;year=2013;volume=3;issue=1;spage=31;epage=34;aulast=Gudi
4/5
22.04.2013
Ultrasound guided drainage of submasseteric space abscesses Gudi SS, Sarvadnya J, Hallur N, Sikkerimath B C - Ann Maxillofac Surg
Space Infections. J Oral Maxillofac Res 2011;2:e4. 9. Siegert R. Ultrasonography of inflammatory soft tissue swellings of head and neck. J Oral Maxillofac Surg 1987;45:8426. McMinn RM. Last's anatomy Regional and applied. 8 th ed. Sydney: McGraw Hill; 1990. p. 455. Ng SY, Songra AK, Bradley PF. A new approach using intraoperative ultrasound imaging for the localization and removal of multiple foreign bodies in the neck. Int J Oral Maxillofac Surg 2003;32:433-6. Barnett SB. Key issue in the analysis of safety of diagnostic ultrasound. Asum Ultrasound Bulletin 2003;6. p. 41-43.
10. 11.
12.
Figures [Figure 1], [Figure 2], [Figure 3], [Figure 4], [Figure 5]
Tables [Table 1], [Table 2]
Sitemap | What's New | Feedback | Disclaimer Annals of Maxillofacial Surgery | Published by Medknow Online since 15 November, 2010
ISSN : P rint -2231-0746, Online - 2249-3816
www.amsjournal.com/article.asp?issn=2231-0746;year=2013;volume=3;issue=1;spage=31;epage=34;aulast=Gudi
5/5
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Home Brewing Log Sheet PDFDocument2 pagesHome Brewing Log Sheet PDFStefanita0% (1)
- Troubleshooting Hydraulic Circuits: Fluid PowerDocument32 pagesTroubleshooting Hydraulic Circuits: Fluid PowerMi LuanaNo ratings yet
- Lesson Plan: Lesson: Projectiles Without Air ResistanceDocument4 pagesLesson Plan: Lesson: Projectiles Without Air ResistanceeltytanNo ratings yet
- Aircraft Design Project 2Document80 pagesAircraft Design Project 2Technology Informer90% (21)
- Metal Framing SystemDocument56 pagesMetal Framing SystemNal MénNo ratings yet
- Analysis and Calculations of The Ground Plane Inductance Associated With A Printed Circuit BoardDocument46 pagesAnalysis and Calculations of The Ground Plane Inductance Associated With A Printed Circuit BoardAbdel-Rahman SaifedinNo ratings yet
- VivsayamDocument87 pagesVivsayamvalarumsakthi100% (2)
- Lec9-Rock Cutting ToolsDocument35 pagesLec9-Rock Cutting ToolsAmraha NoorNo ratings yet
- PDFViewer - JSP 3Document46 pagesPDFViewer - JSP 3Kartik ChaudharyNo ratings yet
- SOR 8th Ed 2013Document467 pagesSOR 8th Ed 2013Durgesh Govil100% (3)
- Diia Specification: Dali Part 252 - Energy ReportingDocument15 pagesDiia Specification: Dali Part 252 - Energy Reportingtufta tuftaNo ratings yet
- IEQ CompleteDocument19 pagesIEQ Completeharshal patilNo ratings yet
- Ancient MesopotamiaDocument69 pagesAncient MesopotamiaAlma CayapNo ratings yet
- Soil LiquefactionDocument12 pagesSoil LiquefactionKikin Kikin PelukaNo ratings yet
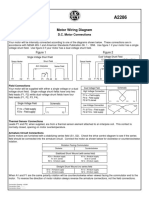
- Motor Wiring Diagram: D.C. Motor ConnectionsDocument1 pageMotor Wiring Diagram: D.C. Motor Connectionsczds6594No ratings yet
- Canon imageFORMULA DR-X10CDocument208 pagesCanon imageFORMULA DR-X10CYury KobzarNo ratings yet
- ProtectionDocument160 pagesProtectionSuthep NgamlertleeNo ratings yet
- Certificate Testing ResultsDocument1 pageCertificate Testing ResultsNisarg PandyaNo ratings yet
- AI Model Sentiment AnalysisDocument6 pagesAI Model Sentiment AnalysisNeeraja RanjithNo ratings yet
- Project On Stones & TilesDocument41 pagesProject On Stones & TilesMegha GolaNo ratings yet
- Product ListDocument4 pagesProduct ListyuvashreeNo ratings yet
- SECTION 303-06 Starting SystemDocument8 pagesSECTION 303-06 Starting SystemTuan TranNo ratings yet
- Garlic Benefits - Can Garlic Lower Your Cholesterol?Document4 pagesGarlic Benefits - Can Garlic Lower Your Cholesterol?Jipson VargheseNo ratings yet
- LKC CS Assignment2Document18 pagesLKC CS Assignment2Jackie LeongNo ratings yet
- Elements of ClimateDocument18 pagesElements of Climateእኔ እስጥፍNo ratings yet
- CAE The Most Comprehensive and Easy-To-Use Ultrasound SimulatorDocument2 pagesCAE The Most Comprehensive and Easy-To-Use Ultrasound Simulatorjfrías_2No ratings yet
- Design of Fixed Column Base JointsDocument23 pagesDesign of Fixed Column Base JointsLanfranco CorniaNo ratings yet
- Is.4162.1.1985 Graduated PipettesDocument23 pagesIs.4162.1.1985 Graduated PipettesBala MuruNo ratings yet
- Reflective Essay 4Document1 pageReflective Essay 4Thirdy AngelesNo ratings yet
- Life of A Landfill PumpDocument50 pagesLife of A Landfill PumpumidNo ratings yet