Professional Documents
Culture Documents
Untitled
Uploaded by
api-241264935Original Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Untitled
Uploaded by
api-241264935Copyright:
Available Formats
AAOS Appropriate Use Criteria Summary
Treatment of Distal Radius Fractures
Abstract
Jayson Murray, MA Leeaht Gross, MPH
From the American Academy of Orthopaedic Surgeons, Rosemont, IL. Neither of the following authors nor any immediate family member has received anything of value from or has stock or stock options held in a commercial company or institution related directly or indirectly to the subject of this article: Mr. Murray and Ms. Gross. These appropriate use criteria were approved by the American Academy of Orthopaedic Surgeons on March 18, 2013. The complete Appropriate Use Criteria for Treatment of Distal Radius Fractures includes all tables, gures, and appendices, and is available at http://www.aaos.org/ research/Appropriate_Use/ DRF_AUC.pdf. J Am Acad Orthop Surg 2013;21: 502-505 http://dx.doi.org/10.5435/ JAAOS-21-08-502 Copyright 2013 by the American Academy of Orthopaedic Surgeons.
The American Academy of Orthopaedic Surgeons has developed Appropriate Use Criteria (AUC) for treating distal radius fractures (DRF). Evidence-based information, in conjunction with the clinical expertise of physicians, was used to develop the criteria to improve patient care and obtain best outcomes while considering the subtleties and distinctions necessary in making clinical decisions. The DRF AUC clinical patient scenarios were derived from patient indications that generally accompany a DRF, as well as from current evidence-based clinical practice guidelines and supporting literature. The 216 indications and 10 treatments were developed by the Writing Panel, a group of clinicians who are specialists in this AUC topic. Next, the Review Panel, a separate group of volunteer physicians, independently reviewed these materials to ensure that they were representative of patient scenarios that clinicians are likely to encounter in daily practice. Finally, the multidisciplinary Voting Panel (made up of specialists and nonspecialists) rated the appropriateness of treatment of each patient scenario using a 9-point scale to designate a treatment as Appropriate (median rating, 7 to 9), May Be Appropriate (median rating, 4 to 6), or Rarely Appropriate (median rating, 1 to 3).
Overview and Rationale
This Appropriate Use Criteria (AUC) was approved by the American Academy of Orthopaedic Surgeons (AAOS) Board of Directors on March 18, 2013. The purpose of the AUC is to help determine the appropriateness of treatments of the heterogeneous patient population routinely seen in practice. The best available scientific evidence is synthesized with collective expert opinion on topics for which gold standard, randomized clinical trials are not available or are inadequately detailed for identifying distinct patient types. AAOS staff convened three independent volunteer physician panels that developed this AUC.
Musculoskeletal care is provided in many settings by different providers. The AAOS created this AUC as an educational tool to guide qualified physicians through a series of treatment decisions in an effort to improve the quality and efficiency of care. These criteria should not be construed as including all indications or excluding indications reasonably directed to obtaining the same results. The criteria are intended to address the most common clinical scenarios facing all appropriately trained surgeons and all qualified physicians managing patients under consideration for treatment of distal radius fractures (DRF). The ultimate judgment regarding any specific criteria should address all circum-
502
Journal of the American Academy of Orthopaedic Surgeons
Jayson Murray, MA, and Leeaht Gross, MPH
stances presented by the patient and the needs and resources particular to the locality or institution. The Appropriate Use Criteria for Treatment of Distal Radius Fractures developed appropriateness treatment ratings for 216 patient scenarios.
Potential Harms and Contraindications
The aim of treatment is pain relief and maintenance of the patients functional status. Most treatments are associated with some known risks, especially invasive and surgical management. In addition, contraindications vary widely based on the treatment administered. Therefore, discussion of available treatments and procedures applicable to the individual patient rely on mutual communication between the patient and physician, weighing the potential risks and benefits for that patient.
materials and provide any suggestions for improvement; and (3) constructing a multidisciplinary voting panel who uses a review of the most current and relevant literature, along with their expert clinical judgment, to rate the appropriateness of treatment of various patient scenarios. General assumptions were developed by the DRF AUC panel members to clarify the interpretation of the patient scenarios and provide standardization for the parameters used to rate the appropriateness of treatment. This AUC was approved by the Appropriate Use Criteria Section, the Council on Research and Quality, and the AAOS Board of Directors. All tables, figures, and appendices, as well as the details of the methods used to prepare this AUC, are detailed in the full AUC, which is available at http://www.aaos.org/research/ Appropriate_Use/DRF_AUC.pdf.
due to trauma, such as a fall from higher-than-standing height, a motor vehicle accident, or an industrial accident in which velocity at impact results in high compression forces, resulting in significant displacement and comminution. A Low-energy mechanism of injury classification was defined as injury due to chronic conditions that weaken the strength of the bone. Low velocity at impact results in bending forces, resulting in minimal comminution and displacement.
Functional Demands
A Homebound classification refers to a patient who cannot leave his or her place of residence without considerable taxing efforts. An Independent classification refers to a patient who routinely completes activities of daily living with assistance of ambulation devices (eg, canes, walkers). A Normal classification refers to a patient who completes activities of daily living without assistance. A High Function Demand classification refers to a patient who experiences substantial stress/strain on his or her wrist on a regular basis (eg, highlevel athletics, heavy labor jobs).
Methods
The AAOS uses the RAND/UCLA Appropriateness Method to develop AUC.1 The process includes the following steps: (1) constructing a writing panel, consisting of 6 to 10 clinicians who are experts in the topic under study, to create a list of patient indications, assumptions, and treatments based on an evidence-based systematic review of the literature conducted by AAOS staff research analysts; (2) constructing a review panel consisting of 10 to 30 clinicians to review the writing panels
Indications and Classications
Figure 1 shows the AO/OTA classification of fractures of the distal radius. Table 1 provides the list of patient indications and classifications developed by the DRF AUC Writing Panel.
Denition of Patient Indications Mechanism of Injury
A High-energy mechanism of injury classification was defined as injury
American Society of Anesthesiologists Status (Comorbidities)
The American Society of Anesthesiologists (ASA) 1 status refers to a normal, healthy patient; the ASA 2 status refers to a patient with mild systemic disease; the ASA 3 status re-
Treatment of Distal Radius Fracture Appropriate Use Criteria Writing Panel: Julie E. Adams, MD, MS, Brett D. Crist, MD, FAAOS, FACS, Charles A. Goldfarb, MD, John J. McGraw, MD, Miguel Pirela-Cruz, MD, FACS, David C. Ring, MD, PhD, Jaiyoung Ryu, MD, and Paul Tornetta III, MD. Review Panel: Jeffrey E. Budoff, MD, Peter J. Evans, MD, PhD, Daren Forward, MD, FRCS, Jeffrey B. Friedrich, MD, FACS, M. Felix Freshwater, MD, Kenneth Koval, MD, Donald H. Lee, MD, Jose J. Monsivais, MD, FACS, Jay Pomerance, MD, J. Andrew Trenholm, MD, FRCSC, Boris A. Zelle, MD, and Dan A. Zlotolow, MD. Voting Panel: Alan M. Adelman, MD, MS, Henry Backe, MD, George W. Balfour, MD, Warren C. Hammert, MD, Robert Charles Kramer, MD, David Dirk Leu, MD, Peter Stern, MD, Steven Strode, MD, MPH, Med, and Walter H. Truong, MD. Moderators: William C. Watters III, MD, and James O. Sanders, MD. Staff of the American Academy of Orthopaedic Surgeons: William R. Martin III, MD, Deborah S. Cummins, PhD, Jayson Murray, MA, Nilay Patel, MA, Ann Woznica, MLS, Leeaht Gross, MPH, and Yasseline Martinez.
August 2013, Vol 21, No 8
503
Treatment of Distal Radius Fractures
Figure 1
Figure 2
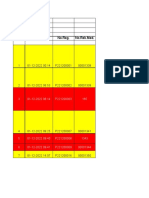
Summary of appropriateness ratings of the distal radius fracture AUC mobile application.
fers to a patient with severe systemic disease; and the ASA 4 status refers to a patient with severe systemic disease that is a constant threat to life.
Associated Injuries
The No Associated Injuries classification refers to isolated DRF. An Open Fracture refers to a wound caused by penetration or puncture of the skin (eg, foreign objects, fractured bones) of the same arm as the DRF. Open fractures are defined using the following two Gustilo classifications: (a) grade I or II open fracture, (b) grade III open fracture. A Median Nerve Injury classification refers to damage/dysfunction of the median nerve on the same arm as the DRF, as determined by physical examination or electrodiagnostic testing. Other Ipsilateral Injury refers to injuries to ligaments, bones, or soft tissue of the same arm/hand as the DRF.
AO/OTA fracture classication of the distal radius. (Reproduced with permission from Xavier C, Molin D, Marins dos Santos R, Torre dos Santos R, Neto J: Surgical treatment of distal radius fractures with a volar locked plate: Correlation of clinical and radiographic results. Rev Bras Ortop 2011;46[5]:505-513.)
Table 1 Indications and Classications Indication AO/OTA fracture type Classication A: Extra-articular fracture B: Partial articular fracture C: Complete articular fracture High energy Low energy Homebound Independent Normal High ASA 13 ASA 4 No associated injuries Grade I or II open fracture Grade III open fracture Median nerve injury Other ipsilateral injury
Mechanism of injury Functional demands
ASA status (comorbidities)a Associated injuries
Results of Appropriateness Ratings
Of 2,160 total voting items (216 patient scenarios, 10 treatments), 440 voting items (20%) were rated as Rarely Appropriate, 953 voting items (44%) were rated as May Be Appropriate, and 767 voting items (36%) were rated as Appropriate
ASA = American Society of Anesthesiologists a ASA 1 = normal, healthy patient; ASA 2 = patient with mild systemic disease; ASA 3 = patient with severe systemic disease; ASA 4 = patient with severe systemic disease that is a constant threat to life
504
Journal of the American Academy of Orthopaedic Surgeons
Jayson Murray, MA, and Leeaht Gross, MPH
(Figure 2). Additionally, the voting panel members were in agreement on 730 voting items (34%) and were in disagreement on 10 voting items (0.5%). The final appropriateness ratings assigned by the nine-member voting panel can be accessed online via the AAOS DRF AUC web-based mobile application at www.aaos.org/ aucapp. As part of the dissemination efforts for the DRF AUC, this web-based mobile application was developed to provide physicians with immediate access to information to assist them
with providing evidence-based patient care. The mobile application includes the list of patient indications and treatment recommendations. Once the clinician enters a patient indication profile specifying the AO/ OTA Fracture Type, Mechanism of Injury, Activity Level of Patient, Patient Health, and Other Injuries, a list of treatment recommendations is provided. For the selected patient profile, green circled checkmarks reflect appropriate treatments, yellow caution symbols reflect treatments that may be appropriate, and red cir-
cled Xs reflect treatments that are rarely appropriate. The application also includes a demonstration (ie, tour), definitions, fracture illustrations, background information, assumptions, a literature review, and a list of contributors.
Reference
1. Fitch K, Bernstein SJ, Aguilar MD, et al: The RAND/UCLA Appropriateness Method Users Manual. Santa Monica, CA, RAND Corporation, 2001.
August 2013, Vol 21, No 8
505
You might also like
- Hip Disarticulation - The Evolution of A Surgical Technique: Sonia J. Wakelin, Christopher W. Oliver, Matthew H. KaufmanDocument10 pagesHip Disarticulation - The Evolution of A Surgical Technique: Sonia J. Wakelin, Christopher W. Oliver, Matthew H. Kaufmanapi-241264935No ratings yet
- UntitledDocument7 pagesUntitledapi-241264935No ratings yet
- Foot & Ankle International: Minimal Incision Surgery For Tibiotalocalcaneal ArthrodesisDocument14 pagesFoot & Ankle International: Minimal Incision Surgery For Tibiotalocalcaneal Arthrodesisapi-241264935No ratings yet
- Open Reduction and Plate Fixation Versus Nonoperative Treatment For Displaced Midshaft Clavicular FracturesDocument9 pagesOpen Reduction and Plate Fixation Versus Nonoperative Treatment For Displaced Midshaft Clavicular Fracturesapi-241264935No ratings yet
- Complications of Arthroscopic Femoroacetabular Impingement TreatmentDocument9 pagesComplications of Arthroscopic Femoroacetabular Impingement Treatmentapi-241264935No ratings yet
- UntitledDocument7 pagesUntitledapi-241264935No ratings yet
- UntitledDocument11 pagesUntitledapi-241264935No ratings yet
- Peripheral Nerve Repair and Reconstruction: Current Concepts ReviewDocument8 pagesPeripheral Nerve Repair and Reconstruction: Current Concepts Reviewapi-241264935No ratings yet
- 2013 Comparative Effectiveness of Exercise and Drug Interventions On Mortality Outcomes Metaepidemiological StudyDocument14 pages2013 Comparative Effectiveness of Exercise and Drug Interventions On Mortality Outcomes Metaepidemiological StudyJohnDoe92No ratings yet
- Evidence-Supported Rehabilitation of Patellar TendinopathyDocument13 pagesEvidence-Supported Rehabilitation of Patellar TendinopathyfilorpgNo ratings yet
- UntitledDocument12 pagesUntitledapi-241264935No ratings yet
- Instructional Course Lectures: SelectedDocument10 pagesInstructional Course Lectures: Selectedapi-241264935No ratings yet
- Osteochondrallesionsofthe Talus:: Size, Age, and Predictors of OutcomesDocument22 pagesOsteochondrallesionsofthe Talus:: Size, Age, and Predictors of Outcomesapi-241264935No ratings yet
- 8 Ankle SprainDocument11 pages8 Ankle Sprainapi-241264935No ratings yet
- 66 Total Ankle Replacement (TAR) : 66.1 Indications and Contraindications For TARDocument42 pages66 Total Ankle Replacement (TAR) : 66.1 Indications and Contraindications For TARapi-241264935No ratings yet
- UntitledDocument11 pagesUntitledapi-241264935No ratings yet
- 65 Tibial Plafond FracturesDocument3 pages65 Tibial Plafond Fracturesapi-241264935No ratings yet
- Foot & Ankle International: Comparison of Gait After Total Ankle Arthroplasty and Ankle ArthrodesisDocument10 pagesFoot & Ankle International: Comparison of Gait After Total Ankle Arthroplasty and Ankle Arthrodesisapi-241264935No ratings yet
- UntitledDocument10 pagesUntitledapi-241264935No ratings yet
- UntitledDocument27 pagesUntitledapi-241264935No ratings yet
- Preface Osteochondrallesionsofthe Talus: Current Issues in Treatment of Osteochondral DefectsDocument1 pagePreface Osteochondrallesionsofthe Talus: Current Issues in Treatment of Osteochondral Defectsapi-241264935No ratings yet
- UntitledDocument12 pagesUntitledapi-241264935No ratings yet
- Stressfracturesofthetibiaand MedialmalleolusDocument17 pagesStressfracturesofthetibiaand Medialmalleolusapi-241264935No ratings yet
- UntitledDocument12 pagesUntitledapi-241264935100% (1)
- Adult Traumatic Brachial Plexus InjuriesDocument15 pagesAdult Traumatic Brachial Plexus Injuriesapi-241264935No ratings yet
- Clinical Diagnosis of Femoroacetabular Impingement: HistoryDocument4 pagesClinical Diagnosis of Femoroacetabular Impingement: Historyapi-241264935No ratings yet
- UntitledDocument10 pagesUntitledapi-241264935No ratings yet
- UntitledDocument10 pagesUntitledapi-241264935No ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5784)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- JSS20-48 Single Time Control Digital Display Time Relay: Page 1 / 2Document2 pagesJSS20-48 Single Time Control Digital Display Time Relay: Page 1 / 2FranciscoNo ratings yet
- Do We Still Need Formocresol in Pediatric DentistryDocument3 pagesDo We Still Need Formocresol in Pediatric DentistryAlexanderDetorakisNo ratings yet
- Higuey, Dom Rep Mdpc/Puj: .Eff.23.MayDocument5 pagesHiguey, Dom Rep Mdpc/Puj: .Eff.23.MayVanessa Yumayusa0% (1)
- Egyptian GlyphsDocument35 pagesEgyptian GlyphsDrMoor0% (1)
- 2008 Annual Debt StatementDocument12 pages2008 Annual Debt StatementEwing Township, NJNo ratings yet
- AZIZ Ur RehmanDocument3 pagesAZIZ Ur Rehmantop writerNo ratings yet
- Brand Mgt. StarbucksDocument3 pagesBrand Mgt. StarbucksPrashansa SumanNo ratings yet
- Lecture 4 Part 1 PDFDocument11 pagesLecture 4 Part 1 PDFBashar AntriNo ratings yet
- 700 - 900 Error Codes PDFDocument1 page700 - 900 Error Codes PDFIsai Lara OsoriaNo ratings yet
- Electrical ManualDocument145 pagesElectrical ManualAbhishek KushwahaNo ratings yet
- Unit 23 The Interior LandscapeDocument21 pagesUnit 23 The Interior LandscapesNo ratings yet
- STRATEGIC MANAGEMENT FRAMEWORKDocument19 pagesSTRATEGIC MANAGEMENT FRAMEWORKCharles CagaananNo ratings yet
- Msae Msae2018-Arwm012 Full Dronespraying 2Document4 pagesMsae Msae2018-Arwm012 Full Dronespraying 2Muhammad Huzaifah Mohd RoslimNo ratings yet
- Al Khanif 2Document31 pagesAl Khanif 2Muhammad DahlanNo ratings yet
- The Dukan Diet by Dr. Pierre Dukan - ExcerptDocument8 pagesThe Dukan Diet by Dr. Pierre Dukan - ExcerptCrown Publishing Group15% (20)
- SKC EPAM-5000 Instruction Manual PDFDocument90 pagesSKC EPAM-5000 Instruction Manual PDFmegacobNo ratings yet
- CX-5 BX-10 No. 1 & 1.5 Fluid Cylinder PartsDocument5 pagesCX-5 BX-10 No. 1 & 1.5 Fluid Cylinder PartsPierreNo ratings yet
- Quartz Textures in Epithermal VeinsDocument16 pagesQuartz Textures in Epithermal VeinsAlvaro MadridNo ratings yet
- Postnatal Care, Complaints & AbnormalitiesDocument38 pagesPostnatal Care, Complaints & AbnormalitiesBernice GyapongNo ratings yet
- Physical Science - q3 - Slm3Document15 pagesPhysical Science - q3 - Slm3Boyet Alvarez AtibagosNo ratings yet
- Lappasieugd - 01 12 2022 - 31 12 2022Document224 pagesLappasieugd - 01 12 2022 - 31 12 2022Sri AriatiNo ratings yet
- Chapter-14 - Person and CareersDocument69 pagesChapter-14 - Person and CareersMarlon SagunNo ratings yet
- Fire & Gas Design BasisDocument2 pagesFire & Gas Design BasisAdil MominNo ratings yet
- Tips For Establish Ball Pen Refill PlantDocument5 pagesTips For Establish Ball Pen Refill PlantSingam Sridhar100% (1)
- Understand TSGLI BenefitsDocument2 pagesUnderstand TSGLI BenefitsJoseph LawerenceNo ratings yet
- Modified Micro Marsupialization in Pediatric Patients: A Minimally Invasive TechniqueDocument4 pagesModified Micro Marsupialization in Pediatric Patients: A Minimally Invasive TechniquerinahpsNo ratings yet
- اللائحة التنظيمية لسفن الكروز - النسخة العربية - TransDocument10 pagesاللائحة التنظيمية لسفن الكروز - النسخة العربية - TranssalsabilNo ratings yet
- Clean Room Laboratory ReportDocument6 pagesClean Room Laboratory ReportHaider IftikarNo ratings yet
- PC 4. Emulsiones Tipo MayonesasDocument10 pagesPC 4. Emulsiones Tipo MayonesasmadarahuchihaNo ratings yet
- FOCAL DYSTONIA-A NEUROLOGICAL CONDITION-TREATED WITH CAUSTICUM - Karl Robinson MDDocument2 pagesFOCAL DYSTONIA-A NEUROLOGICAL CONDITION-TREATED WITH CAUSTICUM - Karl Robinson MDFaker FockerNo ratings yet