Professional Documents
Culture Documents
Path of Physiology
Uploaded by
Carla JimenezCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Path of Physiology
Uploaded by
Carla JimenezCopyright:
Available Formats
Pathophysiology - Pneumonia
Pneumonia inflammatory process of the lung parenchyma Classification 1. Community Acquired used to describe infections found in the community rather than the hospital/nursing home. Defined as an infection that begins outside the hospital or is diagnosed 48 hours after admission to the hospital in a person who has not resided in a long term facility for 14 days or more before admission 2. Hospital Acquired or Nosocomial is defined as a lower respiratory tract infection that was not present or incubating on admission to the hospital. Increase risk for those with mechanical ventilation, compromised immune function, chronic lung disease and airway instrumentation such as e-tube, tracheostomy, etc. Types According to Causative Agent 1. Gram Positive Bacteria Streptococcus pneumonia (pneumococcal pneumonia) most common cause of community acquired pneumonia. follows influenza I situations in which groups of people live in close contact rust colored sputum, blood tinged, purulent Staphylococcus aureus acquired thru blood or by aspiration creamy yellow sputum
2. Gram Negative Bacteria Haemophilus influenza common cause of infection in children high mortality rate greenish colored sputum Klebsiella pneumoniae (Friedlanders bacillus) most common gram negative organism acquired outside hospitals occurs in people with malignancies necrosis, abscess foration, hemoptysis and fibrotic changes occur high mortality rate red gelatinous sputum Pseudomonas aeroginosa most common gram negative organism acquired in the hospital common in the respiratory tract of hospital employees and those with cystic fibrosis greenish colored sputum Legionella pneumophilia (Legionnaires disease) most common cause of community acquired pneumonia found in warm standing water
3. ANAEROIC BACTERIAL PNEUMONIAS Commonly caused by anaerobic streptococcus History of poor dental hygiene, periodontal disease, dysphagia and altered consciousness
4. OTHER INFECTIOUS AGENTS Mycoplasma pneumoniae Fungi an organism with the characteristics of both bacteria and viruses it causes atypical/interstitial pneumonia Viral agents influenza virus, adenovirus and parainfluenza virus self-limiting may predispose to secondary bacterial infection
candidiasis, histoplasmosis, blastomycosis, cryptococcosis, aspergillosis, actinomycosis and nocardiosis follows after extended antibiotic use, immunocompromised and seriously ill people Non-infectious causes
inhalation of toxic gases, chemicals or smoke from fires and aspiration of water due to near drowning, gastric contents, vegetable/mineral oils, liquid petroleum function Pneumocystis carinii pneumonia opportunistic, often fatal form of lung infection seen in debilitated, impaired immune
RISK FACTORS Smoking Air pollution Upper Respiratory Tract Infection
Altered consciousness: alcoholism, head injury, seizure disorder, drug overdose, general anesthesia Tracheal intubation Prolonged immobility Immunosuppressive therapy: corticosteroids, chemotherapy Non-functional immune system: AIDS Severe periodontal disorders Prolonged exposure to virulent organisms Malnutrition Dehydration Chronic disease: Diabetes Mellitus, Heart disease, chronic lung disease Prolonged debilitating disorders Inhalation of noxious substances Aspiration of oral/gastric material Aspiration of foreign material
Chronically ill, elderly people who generally have poor immune systems, often residing in group living situations where there is an increase in probability of disease transmission especially through the respiratory system SIGNS AND SYMPTOMS Fever
Chills Sweats Dullness on percussion on affected area Sputum production Hemoptysis Pleuritic chest pain Dyspnea Headache Fatigue Unequal chest expansion Cough
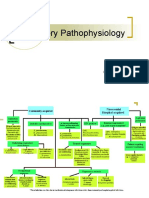
Pathophysiology Inhalation of droplet nuclei Establishes in the alveolus (usually lower lobe) Bacterial infection develops Vascular engorgement, presence of large number of bacteria Serous exudate pours into alveoli from dilated leaking vessels (engorgement first 4-12 hours) Decrease in RBC and Increase in Neutrophils and precipitation of fibrin that fills the alveoli Continuing accumulation of fibrin Consolidation of leukocytes and fibrin Exudate is lyzed and reabsorbed by macrophage DIAGNOSTIC TESTS Chest x-ray Sputum smear Blood cultures Bronchoscopy Transtracheal aspirate
MEDICAL MANAGEMENT 1. medications antimicrobial therapy, pain medication for pleuritic chest pain 2. 3. 4. oxygen therapy bed rest high-calorie diet
5.
adequate fluid intake
NURSING MANAGEMENT 1. Secure airways and ensure adequate oxygenation. 2. 3. 4. 5. 6. Administer analgesics when needed. Administer antibiotics as prescribed. Maintain adequate nutrition. Educate the patient how to cough properly and deep breathing exercises. Position the client properly so as to help clear secretions.
http://nursearchives.blogspot.com/2012/07/pathophysiology-pneumonia.html
You might also like
- PneumoniaDocument50 pagesPneumoniaannududi378556No ratings yet
- Pathology Slide #6+7Document73 pagesPathology Slide #6+7Ibrahim MigdadyNo ratings yet
- Pneumonia CHN Case ReportDocument6 pagesPneumonia CHN Case ReportRhaine MagtotoNo ratings yet
- Community Acquired PneumoniaDocument9 pagesCommunity Acquired PneumoniaSuzette Rae TateNo ratings yet
- Clinical Presentation On PnemoniaDocument37 pagesClinical Presentation On PnemoniasreekalaNo ratings yet
- Pneumonia: DefinitionDocument5 pagesPneumonia: DefinitionhemaanandhyNo ratings yet
- Chapter 1Document30 pagesChapter 1Ayro Business CenterNo ratings yet
- Community Acquired Pneumonia Nelson 400Document37 pagesCommunity Acquired Pneumonia Nelson 400fatima chrystelle nuñalNo ratings yet
- Pediatric Community-Acquired Pneumonia: Causes, Symptoms & TreatmentDocument43 pagesPediatric Community-Acquired Pneumonia: Causes, Symptoms & TreatmentRazel Kinette AzotesNo ratings yet
- PneumoniaDocument5 pagesPneumoniasamtaynbNo ratings yet
- Lower Airway DiseasesDocument70 pagesLower Airway DiseasesAavash PradhanNo ratings yet
- PneumoniaDocument79 pagesPneumoniaEjiro OnoroNo ratings yet
- Pneumonia 3Document8 pagesPneumonia 3janinecasilenNo ratings yet
- Childhood Pneumonia Diagnosis and TreatmentDocument65 pagesChildhood Pneumonia Diagnosis and TreatmentYemata HailuNo ratings yet
- Pneumonia: ANAND. TO, 1ST MSC Student Nursinc NsgstudentDocument11 pagesPneumonia: ANAND. TO, 1ST MSC Student Nursinc NsgstudentArunNo ratings yet
- Respiratory Pathophysiology: B. Pimentel, M.D. University of Makati College of NursingDocument12 pagesRespiratory Pathophysiology: B. Pimentel, M.D. University of Makati College of NursingDoc JacqueNo ratings yet
- Hospital Acquired PneumoniaDocument36 pagesHospital Acquired Pneumoniaadamu mohammadNo ratings yet
- Pneumonia PresentationDocument54 pagesPneumonia PresentationSêrâphîm HâdíNo ratings yet
- ncm112 FinalsDocument18 pagesncm112 FinalsAbegail MierNo ratings yet
- Aspiration Pneumonia Risk Factors and TreatmentDocument23 pagesAspiration Pneumonia Risk Factors and TreatmentBerto UsmanNo ratings yet
- Pneumonia 150514133315 Lva1 App6892Document34 pagesPneumonia 150514133315 Lva1 App6892SadiaNo ratings yet
- 3 - PneumoniaDocument6 pages3 - PneumoniaAmmar AlnajjarNo ratings yet
- Pcap Didactics ChanDocument61 pagesPcap Didactics ChanValerie Anne BebitaNo ratings yet
- PneumoniaDocument68 pagesPneumoniaJelmalyn Basali100% (1)
- Week 1 TropMedDocument96 pagesWeek 1 TropMedmyqurandiaryNo ratings yet
- Oxygen Saturation (If Available) : IagnosisDocument3 pagesOxygen Saturation (If Available) : Iagnosisrezairfan221No ratings yet
- Pneumonia 1Document17 pagesPneumonia 1Jonathan katanaNo ratings yet
- Group 2 Community Acquired PneumoniaDocument24 pagesGroup 2 Community Acquired PneumoniaalyanadayritNo ratings yet
- PneumoniaDocument9 pagesPneumonianachiketpanchal8No ratings yet
- Pneumonia WrittenDocument12 pagesPneumonia WrittenFereli Joy SupanNo ratings yet
- Lung Abscess Causes, Symptoms and TreatmentDocument38 pagesLung Abscess Causes, Symptoms and Treatmentprabad dunusingheNo ratings yet
- BPNDocument49 pagesBPNlovelots1234100% (1)
- Pneumonia: Shervin GolbariDocument24 pagesPneumonia: Shervin GolbarisgolbariNo ratings yet
- Pediatric Community-Acquired PneumoniaDocument60 pagesPediatric Community-Acquired PneumoniaIkea Balhon100% (1)
- PneumoniaDocument3 pagesPneumoniaKami KhanNo ratings yet
- Week 4 Restrictive DisordersDocument212 pagesWeek 4 Restrictive Disordersdelrosariojm87No ratings yet
- Communicable DiseasesDocument101 pagesCommunicable DiseasesKira100% (4)
- Lect 8 Pneumonia PDFDocument68 pagesLect 8 Pneumonia PDFRaghad AbdullaNo ratings yet
- Aspiration PneumoniaDocument18 pagesAspiration PneumoniaRaja Alfian IrawanNo ratings yet
- Epidemiology of TBDocument4 pagesEpidemiology of TByam pdNo ratings yet
- Pneumonia: Anjitha JosephDocument43 pagesPneumonia: Anjitha JosephanjithaNo ratings yet
- Revise PneumoniaDocument7 pagesRevise PneumoniaMelai AvilaNo ratings yet
- Pneumonia WW ReportDocument29 pagesPneumonia WW ReportAradhanaRamchandaniNo ratings yet
- Pneumonia: Prof. Ezekiel M. WafulaDocument20 pagesPneumonia: Prof. Ezekiel M. Wafulaokwadha simion100% (1)
- Pneumonia in ChildrenDocument22 pagesPneumonia in ChildrenHarsha HinklesNo ratings yet
- Lung Abscess Bronchoectasis PleurisynDocument19 pagesLung Abscess Bronchoectasis Pleurisynmarco luenaNo ratings yet
- PneumoniaDocument2 pagesPneumoniaMargaret EricksonNo ratings yet
- Pneumonia: Heny Ekowati, PH.D., AptDocument19 pagesPneumonia: Heny Ekowati, PH.D., Aptaryati yayaNo ratings yet
- Pneumonia Pathophysiology, Diagnosis and TreatmentDocument57 pagesPneumonia Pathophysiology, Diagnosis and TreatmentAnas FikriNo ratings yet
- PneumoniaDocument24 pagesPneumoniaWidhi AstutiNo ratings yet
- Sistem Respirasi Sesak Napas: Problem Based LearningDocument61 pagesSistem Respirasi Sesak Napas: Problem Based LearningAkbar IskandarNo ratings yet
- Care of Patient With Respiratory DisordersDocument35 pagesCare of Patient With Respiratory Disorderskriiteeabns100% (1)
- Lec 9 Respiratory Disorders Part 2Document11 pagesLec 9 Respiratory Disorders Part 2iam2117No ratings yet
- Lung Abscess: BackgroundDocument12 pagesLung Abscess: BackgroundTaufik TiasNo ratings yet
- Pneumonia and GastroentiritisDocument3 pagesPneumonia and Gastroentiritismarie100% (5)
- Pneumonia: DR - Dr. Tahan P.H.,Spp.,Dtce.,Mars Fk-Uwk, 1 April 2011Document42 pagesPneumonia: DR - Dr. Tahan P.H.,Spp.,Dtce.,Mars Fk-Uwk, 1 April 2011Nurfatin adilah kamarudinNo ratings yet
- Pneumonia Is An: ClinicalDocument13 pagesPneumonia Is An: ClinicaldfgsfsfssdNo ratings yet
- The Flu: A Guide for Prevention and TreatmentFrom EverandThe Flu: A Guide for Prevention and TreatmentRating: 5 out of 5 stars5/5 (1)
- Hospital Acquired Pneumonia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHospital Acquired Pneumonia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- 911 Pigeon Disease & Treatment Protocols!From Everand911 Pigeon Disease & Treatment Protocols!Rating: 4 out of 5 stars4/5 (1)
- Essential Neonatal & Infant Skin Care GuideDocument10 pagesEssential Neonatal & Infant Skin Care GuideCarla JimenezNo ratings yet
- FOR CPDocument13 pagesFOR CPCarla JimenezNo ratings yet
- Path of PhysiologyDocument4 pagesPath of PhysiologyCarla JimenezNo ratings yet
- Perception and RealityDocument2 pagesPerception and RealityCarla JimenezNo ratings yet
- Path of PhysiologyDocument4 pagesPath of PhysiologyCarla JimenezNo ratings yet
- Philippine Constitution PDFDocument53 pagesPhilippine Constitution PDFVanessa SantosNo ratings yet
- Contract Services Agreement for Land Bank of the Philippines VOS TransactionDocument1 pageContract Services Agreement for Land Bank of the Philippines VOS TransactionCarla JimenezNo ratings yet
- SPA - Special Power of Atty.Document1 pageSPA - Special Power of Atty.Carla JimenezNo ratings yet
- Table of ContentsDocument2 pagesTable of ContentsCarla JimenezNo ratings yet
- NGESDocument8 pagesNGESCarla JimenezNo ratings yet
- 861 Drug Prescribing For Dentistry 2 Web 2 Email PDFDocument94 pages861 Drug Prescribing For Dentistry 2 Web 2 Email PDFRaphaela TravassosNo ratings yet
- Conscious Sedation PaediatricsDocument44 pagesConscious Sedation PaediatricsReeta TaxakNo ratings yet
- Final Written Lab Exam Form ADocument4 pagesFinal Written Lab Exam Form AErvin T MileNo ratings yet
- Buletin Farmasi 1/2014Document14 pagesBuletin Farmasi 1/2014afiq83100% (1)
- Mini-implant molar intrusion caseDocument1 pageMini-implant molar intrusion caseVesna AndreevskaNo ratings yet
- Auditory Brainstem Response - ABR - in Clinical Practice PDFDocument9 pagesAuditory Brainstem Response - ABR - in Clinical Practice PDFary wisma dewiNo ratings yet
- KenyaEMR v17.3.1 Release Notes SummaryDocument3 pagesKenyaEMR v17.3.1 Release Notes SummaryMigori Art DataNo ratings yet
- Biology 1Document18 pagesBiology 1zaydeeeeNo ratings yet
- Smart + Smart Enhancer: Medic MedicDocument11 pagesSmart + Smart Enhancer: Medic MedicmiazainuddinNo ratings yet
- NCM - 116 Lectute Prelim ModuleDocument7 pagesNCM - 116 Lectute Prelim ModuleHelen GonzalesNo ratings yet
- Prevalence of Hypothyroidism in Adults An EpidemioDocument6 pagesPrevalence of Hypothyroidism in Adults An EpidemioCindy Auliah NasutionNo ratings yet
- Dental Perspective of Pemphigus VulgarisDocument5 pagesDental Perspective of Pemphigus VulgarisSherlyNo ratings yet
- GROUP 10 Senstive Abt Food and Food AllergiesDocument16 pagesGROUP 10 Senstive Abt Food and Food AllergiesLilis nopita SarryNo ratings yet
- Sgot & SGPTDocument2 pagesSgot & SGPT우영박No ratings yet
- Evaluation of Fetal HeartDocument59 pagesEvaluation of Fetal Heartاد ريما البدر100% (3)
- Eric Berg CVDocument6 pagesEric Berg CVHaralambicNo ratings yet
- Unipex Onepager CapixylDocument1 pageUnipex Onepager CapixylalbertitorubinNo ratings yet
- Centenarian Gut Microbiota Effects On Bile AcidDocument32 pagesCentenarian Gut Microbiota Effects On Bile Acidjl18904lamNo ratings yet
- Bladder Cancer Types, Symptoms, Tests & TreatmentDocument1 pageBladder Cancer Types, Symptoms, Tests & TreatmentCarmina AguilarNo ratings yet
- Chapter 15 - Hormones & Endocrine GlandsDocument17 pagesChapter 15 - Hormones & Endocrine Glandsapi-3728508100% (1)
- Route To: Nnovative Joints Ejuvenation CentreDocument2 pagesRoute To: Nnovative Joints Ejuvenation CentreAnil Kumar.VNo ratings yet
- Critical Thinking Case Study #18:: Sickle-Cell AnemiaDocument15 pagesCritical Thinking Case Study #18:: Sickle-Cell AnemiaHakima Hadji DaudNo ratings yet
- Multiple PregnancyDocument16 pagesMultiple Pregnancyjane7arian7berzabalNo ratings yet
- Study On The Efficacy of Nosocomial Infection Control (Senic Project) - Summary of Study DesignDocument14 pagesStudy On The Efficacy of Nosocomial Infection Control (Senic Project) - Summary of Study DesignMunawir GazaliNo ratings yet
- Advances in Extraction TechniquesDocument13 pagesAdvances in Extraction TechniquesashajangamNo ratings yet
- Full-Mouth Adhesive Rehabilitation in Case of Severe Dental Erosion, A Minimally Invasive Approach Following The 3-Step TechniqueDocument18 pagesFull-Mouth Adhesive Rehabilitation in Case of Severe Dental Erosion, A Minimally Invasive Approach Following The 3-Step TechniqueHoracio Mendia100% (1)
- Cerebral Palsy Assessment ImportantDocument7 pagesCerebral Palsy Assessment Importantabra_arr100% (2)
- Clinical Biochemistry ReviewDocument10 pagesClinical Biochemistry Reviewyaykatai100% (2)
- Interpretting ABG SuccessfullyDocument15 pagesInterpretting ABG Successfullyanimathz100% (1)
- Community Health and Program Services (CHAPS) : Health Disparities Among Racial/Ethnic PopulationsDocument4 pagesCommunity Health and Program Services (CHAPS) : Health Disparities Among Racial/Ethnic PopulationsMuhammad Bachiar SafrudinNo ratings yet