Professional Documents
Culture Documents
Syphilis Guideline
Uploaded by
Ma IrmawatiCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Syphilis Guideline
Uploaded by
Ma IrmawatiCopyright:
Available Formats
Syphilis
TEST IF:
MSM (at least annually). HIV positive (at least annually). Routine antenatal screen. Routine immigration screen. A sexual contact of a person with syphilis. Routine sexual health check.
MANAGEMENT SUMMARY
Signs or symptoms of infectious syphilis: Genital ulcers (refer to Genital Ulcer Disease Summary). MSM with any genital symptoms or rash. Any rash affecting the palms of the hands or soles of the feet, or that is persistent or unexplained. Pyrexia of unknown origin, unexplained persistent lymphadenopathy, unexplained liver function disturbance, alopecia.
RECOMMENDED TESTS
Syphilis serology if clinical suspicion of infectious syphilis specify on laboratory form. HIV and hepatitis B serology. Routine STI swabs (see sexual health check guideline). In MSM also request hepatitis A serology. In persons with a history of IDU, incarceration, or who have received blood products, request hepatitis C serology.
Refer or discuss with a sexual health specialist if high index of suspicion of infectious syphilis (e.g. symptoms and/or signs, or contact of index case), or if pregnant. It is recommended to discuss all positive syphilis serology with a sexual health specialist.
MANAGEMENT
Advise to refrain from any sexual activity until assessed or discussed with a specialist service. Do not use/prescribe any topical agents or oral antibiotics for genital ulcers. It is imperative that any intramuscular penicillin formulation used should be long-acting Bicillin LA (benzathine penicillin G) 1.8g, as shortacting formulations provide insufficient treatment duration.
PARTNER NOTIFICATION
Referral or discussion with a sexual health specialist or service is strongly recommended. Be clear about language: partner implies relationship. All sexual contacts within the intervals below should be clinically and serologically evaluated. Infectious syphilis Primary syphilis: 90 days plus empirical treatment for syphilis is recommended, as serology may be negative. Secondary syphilis: 6 months. Early latent syphilis and syphilis of unknown duration where RPR 1:32: 12 months. Late latent syphilis, syphilis of unknown duration with low RPR and tertiary syphilis Serologic evaluation of current or last sexual partner and/or serologic evaluation of children if index case is female.
FOLLOW-UP
Infectious syphilis Repeat serology at 3, 6 and 12 months. Serological cure is defined by consistent four-fold (2 dilutions) drop in RPR titre. Failure of RPR titre to decrease fourfold (2 dilutions) within 12 months indicates treatment failure re-evaluation is necessary. A subsequent four-fold (2 dilution) rise in RPR titre is an indication of re-infection re-evaluation is necessary. Late latent syphilis and tertiary syphilis (excluding neurosyphilis) Repeat serology at 6 and 12 months to ensure remains serofast. Fourfold (2 dilutions) increase in titre indicates either treatment failure or re-infection re-evaluation is necessary. Further guideline information www.nzshs.org or phone the local sexual health service. This Best Practice Guide has been produced by NZSHS, and is adapted from the CMDHB Best Practice Guideline. Every effort has been taken to ensure that the information in this guideline is correct at the time of publishing (July 2012).
Syphilis Management Guidelines
Page 1 of 4
Syphilis
MANAGEMENT GUIDELINE
Introduction
Syphilis is a sexually transmitted disease caused by a bacterium called Treponema pallidum pallidum. Syphilis used to be uncommon in New Zealand but numbers of notified cases have greatly increased since 2000. Syphilis is most commonly diagnosed in: In men who have sex with men, particularly if HIV positive-over 80% of cases. Immigrants from high-prevalence countries (e.g. Eastern Europe, Southeast Asia, China, South America, Africa, Pacific Islands esp. Fiji) New Zealanders who have had sexual contact in a high-prevalence country, Syphilis is spread by intimate contact with muco-cutaneous surfaces so can be easily spread by oral sex and condoms are not fully protective.
Test
People presenting with possible signs or symptoms of syphilis o Genital ulcers (refer to Genital Ulcer Disease Summary) o MSM with any genital symptoms or rash o Any rash affecting the palms of the hands or soles of the feet, or that is persistent or unexplained o In cases of pyrexia of unknown origin, unexplained persistent lymphadenopathy, unexplained liver function disturbance, alopecia Sexual contacts of someone with syphilis MSM (at least annually) HIV positive MSM (at least annually) Pregnant women as part of routine antenatal screening For routine immigration screening When doing a routine sexual health check
Note: If patient is a contact of syphilis they may need presumptive treatment at time of testing-see below. If patient is asymptomatic and not a contact but is concerned about a specific recent sexual event- it is recommended to do a baseline test at time of presentation and do a repeat test at 3 months from time of last sexual intercourse.
Symptoms and signs
Clinically the disease has 3 stages however about 50% of people will have no symptoms and will only be diagnosed by serological testing. Primary Syphilis Patients may present with a genital ulcer or chancre(s) that is usually painless o The ulcer tends to be non-tender and usually has a well-defined margin with an indurated base o May be unnoticed especially if on anal skin or on the cervix Incubation period 10 to 90 days (average 3 weeks). In about 30% of cases there may be multiple chancres Inguinal lymph nodes are usually enlarged, rubbery and non-tender Even if untreated the chancre usually spontaneously heals within a few weeks Secondary Syphilis The patient may present with constitutional symptoms such as fever, malaise, headache and lymphadenopathy The skin is involved in over 90% of cases The rash is usually generalised involving the trunk but may just affect the palms and soles o The rash can be easily confused with drug eruptions, pytariasis rosea or guttate psoriasis There may be alopecia and condylomata lata (warty growths in the ano-genital area). There may also neurological signs and symptoms such as unilateral sensori-neural deafness, ocular nerve palsies, uveitis and meningitis Incubation period 2 to 24 weeks (average 6 weeks) If untreated symptoms slowly resolve over a period of weeks Note: Skin lesions may be extremely infectious so always use gloves during examination of any rash or genital lesion. Latent syphilis This means syphilis with no clinical symptoms or signs Some people never develop symptoms and will only be diagnosed by serological tests If untreated all people become asymptomatic over a period of 12 to 24 months after initial infection. After 12 months people are no longer infectious to sexual partners but women may still pass the infection on to the unborn foetus
Tertiary syphilis Late symptoms/complications may develop months or years later in about one third of cases if not treated Complications include skin lesions (gummas), cardiovascular or neurological disease
Page 2 of 4
Syphilis Management Guidelines
Syphilis is best managed by a specialist sexual health service and all suspected cases should be either referred or discussed with a sexual health specialist.
Diagnostic tests
Diagnosis is usually by serology All blood specimens are initially screened with an enzyme immunoassay (EIA) If this is reactive, then further serological tests will automatically be done by the laboratory for confirmation RPR and TPHA (or TPPA) are usually both performed as confirmatory tests Diagnosis may be confirmed by direct identification of Treponema palliudum either visually (dark-field microscopy) or by antigen tests if there are lesions such as genital ulcers present (specialist services only).
Interpretation of results
General Points: Some serological tests remain reactive for life even after successful treatment Follow-up testing to monitor non-treponemal test titres (RPR/VDRL) is important to establish effective cure Non-venereal Treponematoses: None of the currently available diagnostic tests are able to distinguish between syphilis and other non-venereal treponematoses e.g. Yaws Yaws was formerly endemic in the Pacific region but is unlikely to be the cause of positive treponemal serology in people born in the Pacific after 1960. The decision whether to treat for syphilis or not has to be made on the basis of history and clinical evaluation False Positive Reactions: All of the available serological tests may produce false positive reactions, especially in low prevalence populations Many medical conditions including acute and chronic viral infections, pregnancy, malignancy, and autoimmune disorders can give rise to false positive results However when 2 or 3 different serological tests are positive (EIA, RPR and TPHA) the patient is highly likely to have either current or past infection with syphilis
Management
If a patient has suspected primary or secondary syphilis i.e. symptoms or signs: Early referral or discussion with a sexual health specialist or service is strongly recommended Advise patient to refrain from any sexual activity until assessed and treated and until any rashes or lesions have healed Do not use/prescribe any topical or oral antibiotics for genital ulcers or systemic disease Other recommended tests HIV and hepatitis B serology Routine STI swabs (see sexual health check guideline) In MSM also request hepatitis A serology. In persons with a history of IDU, incarceration or blood product recipients request hepatitis C serology A viral swab for HSV if any genital ulceration present (refer to Genital Ulcer Disease Summary)
Treatment regimens
It is imperative that any intramuscular penicillin formulation used should be long acting. i.e. Bicillin LA(benzathine penicillin) as short acting formulations provide insufficient treatment duration Infectious Syphilis (i.e primary, secondary and early latent syphilis): Bicillin LA (benzathine penicillin) 1.8gm im stat Non-infectious Syphilis (i.e late latent): Bicillin LA (Benzathine penicillin) 1.8gm im weekly for 3 weeks (Total 5.4 g)
Syphilis Management Guidelines
Page 3 of 4
Partner notification and management of sexual partners
Partner notification
Referral or discussion with a sexual health specialist or service is strongly recommended Be clear about language: partner implies relationship. All sexual contacts within the intervals below should be clinically and serologically evaluated:
Primary syphilis 90 days (plus empirical treatment as serology may be negative) Secondary syphilis 6 months Early latent syphilis and syphilis of unknown duration where RPR 1:32: 12 months Late syphilis (late latent and tertiary) current or last sexual partner and/or serologic evaluation of children if index case is female Most choose to tell contacts themselves. Giving written information is helpful. Notifying all contacts may not be possible, e.g. if there insufficient information or a threat of violence.
Management of sexual partners/contacts
Perform a full sexual health check, including serology for syphilis and HIV. Treat empirically for syphilis if sexual contact with infectious syphilis was less than three months ago. Advise them to abstain from sexual contact until serology results are back. Review in person in one week to discuss results and check resolution of any symptoms If they test positive for syphilis partner notification as above.
Follow-up
Infectious Syphilis (Primary, secondary, early latent syphilis and syphilis of unknown duration where RPR titre 1:32): Repeat serology at 3, 6 and 12 months Serological cure is defined by consistent four-fold (2 dilutions) drop in RPR titre Failure of RPR titre to decrease fourfold (2 dilutions) within 12 months indicates treatment failure re-evaluation is necessary A subsequent four-fold(2 dilution) rise in RPR titre is an indication of re-infection re-evaluation is necessary Late latent syphilis and tertiary syphilis (excluding neurosyphilis) Repeat serology at 6 and 12 months to ensure remains serofast Fourfold (2 dilutions) increase in titre indicates either treatment failure or re-infection re-evaluation is necessary
Referral guidelines
Syphilis is best managed by a specialist sexual health service and all suspected cases should be either referred or discussed with a sexual health specialist.
Further guideline information www.nzshs.org or phone the local sexual health service. This Best Practice Guide has been produced by NZSHS, and is adapted from the CMDHB Best Practice Guideline. Every effort has been taken to ensure that the information in this guideline is correct at the time of publishing (July 2012).
Syphilis Management Guidelines
Page 4 of 4
You might also like
- EUROPEAN PHARMACOPOEIA 5ed Sodium Carbonate MonohydrateDocument2 pagesEUROPEAN PHARMACOPOEIA 5ed Sodium Carbonate MonohydrateMa IrmawatiNo ratings yet
- Sp75subject TDocument14 pagesSp75subject TMa IrmawatiNo ratings yet
- Sample ProtocolDocument4 pagesSample ProtocolDrashua AshuaNo ratings yet
- Becoming A Pioneer of Success God's Plan To Help You Win in Life and in BusinessDocument176 pagesBecoming A Pioneer of Success God's Plan To Help You Win in Life and in BusinessMira Lindgren100% (1)
- Formulir LA Lights Indie Movie 2013Document4 pagesFormulir LA Lights Indie Movie 2013-Zinedine ZahidNo ratings yet
- Syphilis 2012Document9 pagesSyphilis 2012Ma IrmawatiNo ratings yet
- Brjvendis00013 0061Document2 pagesBrjvendis00013 0061Ma IrmawatiNo ratings yet
- FibroidsDocument16 pagesFibroidsMa IrmawatiNo ratings yet
- Fibroid GuidelinesDocument8 pagesFibroid GuidelinesMa IrmawatiNo ratings yet
- Considering Surgery For Uterine Fibroids?: The Condition(s)Document8 pagesConsidering Surgery For Uterine Fibroids?: The Condition(s)Ma IrmawatiNo ratings yet
- Adobe Photoshop 120 TipsDocument14 pagesAdobe Photoshop 120 Tipslgunityz100% (2)
- 02-01 Drug DistributionDocument3 pages02-01 Drug DistributionMa Irmawati0% (1)
- Production and DocumentationDocument9 pagesProduction and DocumentationMa IrmawatiNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Class Program Grade 6Document11 pagesClass Program Grade 6Ma Victoria Dumapay Teleb100% (2)
- Cases IncorporationDocument75 pagesCases IncorporationshakiraNo ratings yet
- NBI CLEARANCE-mom PDFDocument1 pageNBI CLEARANCE-mom PDFJr RotasNo ratings yet
- Employment ApplicationDocument3 pagesEmployment Applicationapi-251839072100% (1)
- Extreme Vetting of Immigrants: Estimating Terrorism Vetting FailuresDocument64 pagesExtreme Vetting of Immigrants: Estimating Terrorism Vetting FailuresCato InstituteNo ratings yet
- April 3 2023Document3 pagesApril 3 2023Kier Jhoem mahusayNo ratings yet
- Heirs of Prodon vs. Heirs of AlvarezDocument2 pagesHeirs of Prodon vs. Heirs of AlvarezShane Fernandez JardinicoNo ratings yet
- Raber DS Lantai Bawah Dan Pinere 09-03-22 GHDocument14 pagesRaber DS Lantai Bawah Dan Pinere 09-03-22 GHifanda80No ratings yet
- What is the UNCLOS? Understanding the United Nations Convention on the Law of the SeaDocument4 pagesWhat is the UNCLOS? Understanding the United Nations Convention on the Law of the SeaJane Sudario100% (1)
- Sample Midterm Exams - Consti 2Document5 pagesSample Midterm Exams - Consti 2Ayla Herazade SalendabNo ratings yet
- US Department of Justice Official Release - 01000-399at HTMDocument2 pagesUS Department of Justice Official Release - 01000-399at HTMlegalmattersNo ratings yet
- Texas AG Ken Paxton Letter To Dallas Judge Eric Moye RE: Confinement of Shelley LutherDocument2 pagesTexas AG Ken Paxton Letter To Dallas Judge Eric Moye RE: Confinement of Shelley LutherMyTexasDaily.com100% (1)
- BADGE (Keywords, Nature of The Case) Caption Title: PartiesDocument2 pagesBADGE (Keywords, Nature of The Case) Caption Title: PartiesAnnNo ratings yet
- Sajjan Kumar v. CBI, (2010) 9 SCC 368: Eastern Book Company Generated: Wednesday, April 15, 2020Document1 pageSajjan Kumar v. CBI, (2010) 9 SCC 368: Eastern Book Company Generated: Wednesday, April 15, 2020Sri MuganNo ratings yet
- Judge Breslow OrderDocument9 pagesJudge Breslow OrderKim BurrowsNo ratings yet
- The Play "Trifles" by Susan GlaspellDocument9 pagesThe Play "Trifles" by Susan Glaspellselina_kollsNo ratings yet
- Brain Injury 2014Document356 pagesBrain Injury 2014sandykumala100% (1)
- Weatherly International PLC V Bruni & McLaren and Another ( (P) A 191/2006) (2011) NAHC 263 (14 September 2011)Document12 pagesWeatherly International PLC V Bruni & McLaren and Another ( (P) A 191/2006) (2011) NAHC 263 (14 September 2011)André Le RouxNo ratings yet
- April 26Document10 pagesApril 26Fatima Janine T. FrivaldoNo ratings yet
- Contemporary Army APC'sDocument26 pagesContemporary Army APC'sasim khanNo ratings yet
- Competitive integration models in the Western hemisphere: bilateral trade agreements vs regional blocsDocument23 pagesCompetitive integration models in the Western hemisphere: bilateral trade agreements vs regional blocsLaura RealesNo ratings yet
- Sparta's dual kingship and democratic assemblyDocument2 pagesSparta's dual kingship and democratic assemblyAustin HazelrigNo ratings yet
- Movie Review 1917Document2 pagesMovie Review 1917api-550923881No ratings yet
- Allied Banking Corporation vs. FukuokaDocument20 pagesAllied Banking Corporation vs. FukuokamcffunelasNo ratings yet
- All Conditional Types - Exercises 1 : 1. Fill The Gaps With The Correct Form of The Verb in BracketsDocument1 pageAll Conditional Types - Exercises 1 : 1. Fill The Gaps With The Correct Form of The Verb in BracketsMalory LizarazoNo ratings yet
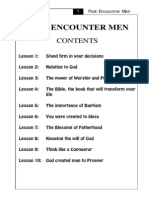
- Post-Encounter Men Manual (Teacher)Document96 pagesPost-Encounter Men Manual (Teacher)anselmo cortes83% (6)
- Sav 0022Document21 pagesSav 0022MichaelNo ratings yet
- LAW Sidd ProjectDocument3 pagesLAW Sidd ProjectNaitik PahujaNo ratings yet
- Complaint Affidavit - Damages For Reckless Imprudence Resulting To Damage To PropertyDocument1 pageComplaint Affidavit - Damages For Reckless Imprudence Resulting To Damage To PropertyRan Ngi100% (7)
- Cybercrime - Notes For UPSC GS IIIDocument2 pagesCybercrime - Notes For UPSC GS IIIskmishra66No ratings yet