Professional Documents
Culture Documents
Medical Treatment For Combined Fusarium and Acanthamoeba Keratitis.
Uploaded by
Rodrigo BarreraOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Medical Treatment For Combined Fusarium and Acanthamoeba Keratitis.
Uploaded by
Rodrigo BarreraCopyright:
Available Formats
Acta Ophthalmologica 2009
Medical treatment for combined Fusarium and Acanthamoeba keratitis
Hsin-Chiung Lin, Ching-Hsi Hsiao, David Hui-Kang Ma, Lung-Kun Yeh, Hsin-Yuan Tan, Meng-Yin Lin and Samuel Chao-Ming Huang
Department of Ophthalmology, Chang Gung Memorial Hospital, Chang Gung University School of Medicine, Taoyuan, Taiwan
ABSTRACT. Purpose: Acanthamoeba and fungal keratitis are rare ocular infections. We report cases of combined Fusarium and Acanthamoeba keratitis and the clinical course of medical treatment. Methods: We reviewed the medical records of patients treated for culture-proven Acanthamoeba keratitis at a referral centre, during 2001)2006. Results: Eleven consecutive patients were treated for culture-proven Acanthamoeba keratitis during the 5 years, two of whom had combined fungal infections. A 29-year-old man presented with ground-glass corneal oedema and epitheliopathy caused by contact lens use. The other patient, a 7-year-old girl, had eye trauma that led to a feathery corneal inltrate. Both cases were treated with topical 0.02% polyhexamethylene biguanide (PHMB), 0.1% propamidine, 1% clotrimazole and 5% natamycin. Therapeutic keratoplasty was not required in either case. Conclusions: Timely identication of the pathogen, with repeated culture and smear if necessary, as well as adequate dosage to prevent recurrence is highly recommended in order to preclude the need for therapeutic penetrating keratoplasty.
Key words: Acanthamoeba Fusarium keratitis
Acta Ophthalmol. 2009: 87: 199203
2008 The Authors Journal compilation 2008 Acta Ophthalmol
doi: 10.1111/j.1755-3768.2008.01192.x
Introduction
Acanthamoeba and fungal keratitis are relatively rare corneal infections that may respond poorly to medical therapy. Combined infection with these two pathogens is even rarer (Gussler et al. 1995; Tien & Sheu 1999; Froumis et al. 2001; Rumelt et al. 2001; Babu & Murthy 2007) . Contact lens wear is an established risk factor for
Acanthamoeba keratitis. Verhelst et al. (2006) reported Acanthamoeba keratitis as second to Pseudomonas as a cause of contact lens-related corneal ulcers. The earliest signs of Acanthamoeba infection are at the epithelial level, with patchy oedema, microcysts and epithelial haze. These symptoms cause an irregular dendritiform ulceration, which is often misdiagnosed as keratitis caused by herpes simplex
virus. Stromal ndings, which occur later, include single or multiple stromal inltrates and nummular keratitis. Ring inltrates or satellite lesions usually suggest advanced disease. Effective medical treatment depends on early diagnosis (Bacon et al. 1993). Treatment regimens have varied from the biguanides polyhexamethylene biguanide (PHMB) and chlorhexidine, to the diamide propamidine, the aminoglycoside neomycin and the antifungal clotrimazole. The drugs have been used in different combinations, with varying degrees of success. Poor outcomes after therapeutic penetrating keratoplasty (TPK) for eradication of Acanthamoeba keratitis (Ficker et al. 1993) have made medical therapy even more signicant. Fungal keratitis often involves a history of trauma with vegetable matter or chronic ocular surface disease. Fusarium is common in warmer climates (Rosa et al. 1994) and the agricultural community, where it is generally found in organic matter such as plants and soil and represents normal ora for rice, beans and soybeans. The standard medical treatment for Fusarium fungal keratitis is frequent use of natamycin 5% drops, but any delay in diagnosis usually leads to TPK (Lin et al. 2005). Diagnosis of mixed infection is often delayed and TPK is frequently required to re-establish integrity and eliminate the infectious process. The purpose of this study was to investigate
199
Acta Ophthalmologica 2009
the efcacy of medical treatment in combined infections.
Materials and Methods
The medical records for cases of Acanthamoeba keratitis treated at Chang Gung Memorial Hospital between January 2001 and December 2006 were retrospectively reviewed. Informed consent was obtained from patients according to the tenets of the Declaration of Helsinki. Corneal scrapings and contact lens case solutions, if available, were sent for culture and smears of bacteria, fungi and Acanthamoeba, on chocolate, 5% sheep blood, anaerobic blood agar, inhibitory mould agar (IMA), IMA supplemented with chloramphenicol and gentamicin (ICG) agar, and nonnutrient agar plates overlaid with Escherichia coli. External eye photographs were documented weekly and re-culture was performed in cases of progression or poor medical response after the cessation of empiric topical antibiotics for 24 hours. Information obtained from the medical records included age, sex, predisposing factors,
prior diagnosis and treatment, complications and visual outcome. Prognostic factors mainly affected the necessity for TPK in the acute infectious status. There were 11 cases of culture-proven Acanthamoeba keratitis, 191 cases of fungal corneal infection, and two of Acanthamoeba keratitis combined with fungal infection that were treated with medication alone. Seven Acanthamoeba keratitis patients underwent surgery other than diagnostic biopsy. These included four TPK procedures, two amniotic membrane transplantations, and one evisceration (Table 1).
Case Reports
Case 7
In June 2003, a 29-year-old man, who had previously worn soft contact lenses, presented with pain, redness and decreased visual acuity (VA) in the right eye. He reported no homemade saline or tap water usage, nor did he wear the lenses overnight. He had been treated in another clinic with topical noroxacin, topical steroids and acyclovir ointment for 3 weeks.
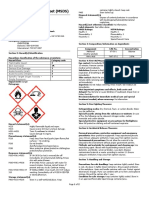
The patient was then transferred to our hospital, where slit-lamp examination revealed diffuse coarse punctate keratitis, keratic precipitates, groundglass oedema and inltration of the stromal inammatory cells. His best corrected visual acuity (BCVA) was 0.2. Corneal scraping and analysis of the solution in his contact lens case revealed the presence of Acanthamoeba. Polyhexamethylene biguanide (0.02% PHMB; Leiters Pharmacy, San Jose, CA, USA) solution was instilled every hour around the clock. A localized inltrate with endothelial plaque occurred in the inferior temporal cornea 10 days later (Fig. 1) and VA dropped to 0.01. Repeat smears and cultures were performed on the new lesion, which revealed hyphae in the smear, whereas the culture grew Fusarium species. Topical 5% natamycin and 0.02% PHMB solution were instilled every hour and 0.1% propamidine and 1% clotrimazole (Leiters Pharmacy) solution was added 13 days later. The applications of PHMB, propamidine and clotrimazole were gradually tapered over the following month
Table 1. Clinical details of patients. Duration of symptoms before diagnosis (weeks) 8 4 4 1 2 5 4 3 3 4 3
Patient no. age sex eye 1 66 M R 2 21 M L 3 18 M L 4 19 M L 5 26 M R 6 23 F R 7 29 M R 87FR 9 15 M R 10 8 M R 11 29 M L
Risk factors Trauma SCL SCL SCL SCL SCL SCL Trauma Ortho K Ortho K SCL
Presenting ocular ndings Sclerokeratitis Ring ulcer hypopyon Stromal inltration Ring inltrate Ground-glass oedema Ground-glass oedema Ground-glass oedema, epitheliopathy Epitheliopathy, ground-glass oedema Feathery stromal inltration Epitheliopathy, ground-glass oedema Ring ulcer Perineuritis, stromal inltration
Duration of anti-amoebic therapy (months) 2* 4* 4* 1* 3* 4* 4 4 1* 4* 4*
VA at initial presentation nal VA CF LP ()) 0.4 0.7 CF 0.01 0.05 0.4 0.2 0.06 0.1 0.5 0.2 1.0 0.1 0.01 0.2 0.6 CF 0.1 0.2 0.6
Medication before diagnosis Pred-Forte, ampho-B, cefazolin, amikacin Cefazolin, amikacin Pred-Forte FML, GM, uconazole Neomycin ciprooxacin Pred-Forte acyclovir Pred-Forte, amikacin, cefazolin Ciprooxacin, acyclovir, Pred-Forte Ciprooxacin, neomycin, amikacin, cefazolin Ciprooxacin Ciprooxaxin, amikacin, cefazolin, GM, ooxacin,
Surgery (except diagnostic biopsies) Scleral exploration enucleation TPK optical PKP TPK optical PKP AMT Nil TPK optical PKP Nil Nil AMT TPK Nil
* Polyhexamethylene biguanide + propamidine. polyhexamethylene biguanide + propamidine + clotrimazole + natamycin. VA = visual acuity; M = male; F = female; SCL = soft contact lens; Ortho K = orthokeratology; CF = counting ngers; LP = light perception; FML = uorometholone solution; GM = gentamicin solution; TPK = therapeutic penetrating keratoplasty; optical PKP = optical penetrating keratoplasty; AMT = amniotic membrane transplantation.
200
Acta Ophthalmologica 2009
Fig. 1. Case 7. Photograph of contact lens-related diffuse supercial keratitis and stromal oedema in a 29-year-old man, showing increased localized inltration in the temporal lower cornea and the appearance of endothelial plaque.
according to the improved corneal condition, and nally discontinued 4 months later. Natamycin was discontinued after 1.5 months. The subjects BCVA at 6 months was 1.0.
Case 8
In December 2003, a 7-year-old girl presented with pain and redness in her right eye after a foreign body struck it
at a school reconstruction site. She went to a local clinic, where ciprooxacin and neomycin solution every 3 hours was prescribed. The corneal ulcer progressed in the following week and she was referred to our hospital. Visual acuity in her right eye was 0.1 and slit-lamp examination revealed central stromal inltrates with feathery margins (Fig. 2A). Samples for smears and cultures were taken and
(A)
topical cefazolin (25 mg ml) and amikacin (25 mg ml) were administered every hour around the clock. After 5 days of treatment, the feathery inltrates were still progressing and natamycin solution was started hourly. Re-cultures of the lesion, including Acanthamoeba, were performed. However, hypopyon, endothelial plaque and a strong anterior chamber reaction appeared 3 days later. Initially the culture grew Fusarium solani. The re-culture revealed Acanthamoeba cysts from corneal scraping with haematoxylin and eosin staining. Hourly treatment with PHMB, propamidine and clotrimazole was started. The hypopyon disappeared within 2 weeks, the stromal inltrates abated and corneal neovascularization formed gradually. The patient was discharged after 1 month. Her medication was adjusted to PHMB hourly, and clotrimazole and natamycin, alternately, administered every 2 hours. However, 1 month after discharge, the stromal inltrates deteriorated and the hypopyon reappeared. The patient reported that she often missed her eyedrop instillations at home. She was re-admitted and received intracameral amphotericin B injection (Kuriakose et al. 2002; Yilmaz et al. 2007) in addition to topical anti-amoebic and antifungal medications. The hypopyon and corneal inltrates decreased gradually over the following month and neovascularization developed (Fig. 2B). The medications were gradually tapered under regular follow-ups and were subsequently discontinued after 4 months. Two years later, the subjects BCVA was 0.01 as a result of central stromal scarring and neovascularization.
Discussion
Of the six cases of combined Acanthamoeba and fungal keratitis reported in the medical literature, ve (Gussler et al. 1995; Tien & Sheu 1999; Froumis et al. 2001) (Table 2) were diagnosed with Acanthamoeba keratitis before fungi were identied in the corneal buttons after TPK. In the sixth patient (Rumelt et al. 2001), Acanthamoeba and fungal co-infection were noted during a second corneal scraping 15 days after the eye trauma had occurred. However, medications were
(B)
Fig. 2. (A) A 7-year-old girl presented with central corneal inltration with a feathery margin and endothelial plaque. (B) Four months later, the cornea showed extensive neovascularization.
201
Acta Ophthalmologica 2009
Table 2. Reported spectrum of corneal co-infection with Acanthamoeba and fungus. Initial clinical diagnosis Bacteria No. of patients 1 Subsequent treatment PHMB, TPK Visual outcome 20 20
Causative agents Acanthamoeba + Fusarium (Gussler et al. 1995) Acanthamoeba + mould (Tien & Sheu 1999) Acanthamoeba + scedosporium apiospermum (Froumis et al. 2001) Acanthamoeba + scedosporium apiospermum (Rumelt et al. 2001) Acanthamoeba + Fusarium (Babu & Murthy 2007)
Risk factors RK + tap water
Initial treatment Ciprooxacin, vancomycin, tobramycin Neomycin, metronidazole (Case 1), amikacin, piperacillin (Cases 2, 3) Cyclosporin A, Pred-Forte
Acanthamoeba and bacteria HSK
DM, mud-related trauma and SCL Contact lens
1 (2 eyes)
Bacteria
Trauma by sewage-contaminated object Agriculturist
Ciprooxacin, cyclogyl, Pred-Forte, bacitracin
Fusarium and Acanthamoeba
Natamycin, propamidine, PHMB
PHMB, uconazole, TPK Propamidine, Neomycin, Cyclogyl, TPK, VT, silicone oil Natamycin, PHMB, clotrimazole, propamidine, TPK, VT
HM 20 100 20 20 CF
20 70
69
RK = radial keratotomy; DM = diabetes mellitus; HM = hand movements; CF = counting ngers; SCL = soft contact lens; PHMB = polyhexamethylene biguanide, HSK = herpes simplex keratitis; TPK = therapeutic penetrating keratoplasty; VT = vitrectomy.
unable to halt the infection and TPK was indicated for cornea perforation. Successful medical treatment of Acanthamoeba keratitis as a result of early diagnosis has been reported (DAversa et al. 1995; Azuara-Blanco et al. 1997). Poor response to medical treatment often leads to TPK (Illingworth et al. l996; Wang et al. 1997). Confocal microscopy provides in vivo views of the cornea and delineates both the trophozoite and cyst. The doublewalled cysts are particularly prominent and radial keratoneuritis can be appreciated, providing an adjunctive modality for early diagnosis (Babu & Murthy 2007). To the best of our knowledge, this study describes the rst reported culture-proven cases of medical treatment for combined Acanthamoeba and fungal keratitis. The unfavourable results reported of combined fungal and Acanthamoeba infection may be attributed to several factors. Firstly, both pathogens are resistant to initial empirical antimicrobial agents. Secondly, in mixed infections, Acanthamoeba may progress faster because the fungi may serve as nutrients for the Acanthamoeba. Studies on contact lens cases contaminated with Acanthamoeba have demonstrated that the presence of bacteria and fungi may be an important factor in the survival and growth of Acanthamoeba. (Donzis et al. 1989; Trevor et al. 1995).
Acanthamoeba are ubiquitous protozoa that exist in two forms. Under unfavourable conditions, trophozoites transform into cysts that are resistant to extremes of temperature, pH and desiccation (Aksozek et al. 2002). Cysts are difcult to kill, which is one reason why this infection is so hard to eradicate. Only one class of medications is known to have cystocidal activity, the biguanides. Polyhexamethylene biguanide has been shown to kill both the trophozoite and cyst without toxic effects to the healing epithelium (Larkin et al. 1992). Some reports have recommended the combined use of propamidine and polymyxin B neomycin gramicidin (Neosporin), or the use of propamidine combined with one of the biguanides or clotrimazole as primary therapy. Some anti-amoebic drugs may have antifungal activity, such as PHMB, which has been shown to inhibit Fusarium keratitis (Fiscella et al. 1997). Clotrimazole, a synthetic imidazole derivative, is an antifungal agent that has been shown to have an excellent effect on Acanthamoeba keratitis (Driebe et al. 1988), but in Fusarium keratitis, a combination with a polyene derivative is suggested (Mselle 2001). Fungal keratitis is characteristically slow-growing and early cessation of antifungal medication usually leads to recrudescence, and a delay in diagno-
sis often leads to blindness (Dursun et al. 2003). The risk of activation of dormant cysts in Acanthamoeba infections can lead to patient relapse following apparently effective treatment. With anti-amoebic and antifungal medications, clinical signs appear to worsen during the rst few days of therapy and improvement may not be evident until 12 weeks have elapsed. In general, therapy should be continued for at least 34 months to eradicate viable cysts or fungi in the deep stroma (ODay & Head 2000). Both Acanthamoeba and fungal keratitis are rare, but they represent infections of the cornea that can potentially cause blindness. Early diagnosis and adequate dosing is essential to prevent recourse to TPK.
References
Aksozek A, McClellan K, Howard K, Niederkorn JY & Alizadeh H (2002): Resistance of Acanthamoeba castellanii cysts to physical, chemical, and radiological conditions. J Parasitol 88: 621623. Azuara-Blanco A, Sadiq AS, Hussain M, Lloyd JH & Dua HS (1997): Successful medical treatment of Acanthamoeba keratitis. Int Ophthalmol 21: 223227. Babu K & Murthy KR (2007): Combined fungal and Acanthamoeba keratitis: diagnosis by in vivo confocal microscopy. Eye 21: 271272. Bacon AS, Dart JK, Ficker LA, Matheson MM & Wright P (1993): Acanthamoeba
202
Acta Ophthalmologica 2009
keratitis. The value of early diagnosis. Ophthalmology 100: 12381243. DAversa G, Stern GA & Driebe WT Jr (1995): Diagnosis and successful treatment of Acanthamoeba keratitis. Arch Ophthalmol 113: 11201123. Donzis PB, Mondino BJ, Weissman BA & Bruckner DA (1989): Microbial analysis of contact lens care systems contaminated with Acanthamoeba. Am J Ophthalmol 108: 5356. Driebe WT Jr, Stern GA, Epstein RJ, Visvesvara GS, Adi M & Komadina T (1988): Acanthamoeba keratitis. Potential role for topical clotrimazole in combination chemotherapy. Arch Ophthalmol 106: 11961201. Dursun D, Fernandez V, Miller D & Alfonso EC (2003): Advanced Fusarium keratitis progressing to endophthalmitis. Cornea 22: 300303. Ficker LA, Kirkness C & Wright P (1993): Prognosis for keratoplasty in Acanthamoeba keratitis. Ophthalmology 100: 105110. Fiscella R, Moshifar M, Messick CR, Pedland SL, Chandler JW & Viana M (1997): Polyhexamethylene biguanide in the treatment of experimental Fusarium keratomycosis. Cornea 16: 447449. Froumis NA, Mondino BJ & Glasgow BJ (2001): Acanthamoeba keratitis associated with fungal keratitis. Am J Ophthalmol 131: 508509. Gussler JR, Miller D, Jaffe M & Alonso EC (1995): Infection after radial keratotomy. Am J Ophthalmol 119: 798799.
Hammersmith KM (2006): Diagnosis and management of Acanthamoeba keratitis. Curr Opin Ophthalmol 17: 327331. Illingworth CD, Cook SD, Karabatsas CH & Easty DL (1996): Acanthamoeba keratitis: risk factors and outcome. Br J Ophthalmol 80: 773774. Kuriakose T, Kothari M, Paul P, Jacob P & Thomas R (2002): Intracameral amphotericin B injection in the management of deep keratomycosis. Cornea 21: 653656. Larkin DF, Kilvington S & Dart JK (1992): Treatment of Acanthamoeba keratitis with polyhexamethylene biguanide. Ophthalmology 99: 185191. Lin HC, Chu PH, Kuo YH & Shen SC (2005): Clinical experience in managing Fusarium solani keratitis. Int J Clin Pract 59: 549554. Mselle J. (2001): Use of topical clotrimazole in human keratomycosis. Ophthalmologica 215: 357360. ODay DM & Head WS (2000): Advances in the management of keratomycosis and Acanthamoeba keratitis. Cornea 19: 681687. Rosa RH, Miller D & Alfonso EC (1994): The changing spectrum of fungal keratitis in Southern Florida. Ophthalmology 101: 10051013. Rumelt S, Cohen I, Leer E & Rehany U (2001): Corneal co-infection with Scedosporium apiospermum and Acanthamoeba after sewage-contaminated ocular injury. Cornea 20: 112116. Tien SH & Sheu MM (1999): Treatment of Acanthamoeba keratitis combined with fun-
gal infection with polyhexamethylene biguanide. Kaohsiung J Med Sci 15: 665673. Trevor BG, Ray TMC, Jane FS & Paul RR (1995): Acanthamoeba, bacterial and fungal contamination of contact lens storage cases. Br J Ophthalmol 79: 601605. Verhelst D, Koppen C, Van Looveren J, Meheus A, Tassignon MJ & the Belgian Keratitis Study Group (2006): Contact lensrelated corneal ulcers requiring hospitalization: a 7-year retrospective study in Belgium. Acta Ophthalmol Scand 84: 522526. Wang IJ, Hong JP & Hu FR (1997): Clinical features and outcome of Acanthamoeba keratitis. J Formos Med Assoc 96: 895900. Yilmaz S, Ture M & Maden A (2007): Efcacy of intracameral amphotericin B injection in the management of refractory keratomycosis and endophthalmitis. Cornea 26: 398402.
Received on May 29th, 2007. Accepted on December 12th, 2007. Correspondence: Hsin-Chiung Lin MD Department of Ophthalmology Chang Gung Memorial Hospital, Chang Gung University School of Medicine 5, Fu-Hsing Street Kweishan, Taoyuan 333 Taiwan Tel: + 886 3 328 1200 (ext. 8666) Fax: + 886 3 328 7798 Email: hclinn@adm.cgmh.org.tw
203
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- 1 s2.0 S0104001413002170 MainDocument15 pages1 s2.0 S0104001413002170 MainRodrigo BarreraNo ratings yet
- Accuracy of Biometry in Pediatric Cataract Extraction With Primary Intraocular Lens ImplantationDocument8 pagesAccuracy of Biometry in Pediatric Cataract Extraction With Primary Intraocular Lens ImplantationRodrigo BarreraNo ratings yet
- 1 s2.0 S0002961013004145 MainDocument7 pages1 s2.0 S0002961013004145 MainRodrigo BarreraNo ratings yet
- 1 s2.0 S0049384813001904 MainDocument6 pages1 s2.0 S0049384813001904 MainRodrigo BarreraNo ratings yet
- Novel Anticoagulants: Anesthetic Implications: A Platelet-Ligand-Platelet Matrix With FibrinogenDocument9 pagesNovel Anticoagulants: Anesthetic Implications: A Platelet-Ligand-Platelet Matrix With FibrinogenRodrigo BarreraNo ratings yet
- Anticoagulants: Newerones, Mechanisms, and Perioperative UpdatesDocument13 pagesAnticoagulants: Newerones, Mechanisms, and Perioperative UpdatesKiria J. BárcenasNo ratings yet
- n57 Obesity Guidelines 131204Document232 pagesn57 Obesity Guidelines 131204Rodrigo BarreraNo ratings yet
- Seasonal Trends of Microbial Keratitis in South India.Document5 pagesSeasonal Trends of Microbial Keratitis in South India.Rodrigo BarreraNo ratings yet
- Successful Medical Management of Recalcitrant Fusarium Solani Keratitis: Molecular Identification and Susceptibility Patterns.Document5 pagesSuccessful Medical Management of Recalcitrant Fusarium Solani Keratitis: Molecular Identification and Susceptibility Patterns.Rodrigo BarreraNo ratings yet
- Fusarium Keratitis in Brazil: Genotyping, in Vitro Susceptibilities, and Clinical OutcomesDocument9 pagesFusarium Keratitis in Brazil: Genotyping, in Vitro Susceptibilities, and Clinical OutcomesRodrigo BarreraNo ratings yet
- Queratitis India 4Document4 pagesQueratitis India 4Rodrigo BarreraNo ratings yet
- Queratitis India 4Document4 pagesQueratitis India 4Rodrigo BarreraNo ratings yet
- Queratitis India 3Document5 pagesQueratitis India 3Rodrigo BarreraNo ratings yet
- ArabiaDocument8 pagesArabiaRodrigo BarreraNo ratings yet
- Epidemiology and Laboratory Diagnosis of Fungal Corneal Ulcer in The Sundarban Region of West Bengal, Eastern India.Document8 pagesEpidemiology and Laboratory Diagnosis of Fungal Corneal Ulcer in The Sundarban Region of West Bengal, Eastern India.Rodrigo BarreraNo ratings yet
- UsaDocument5 pagesUsaRodrigo BarreraNo ratings yet
- Usa 2Document6 pagesUsa 2Rodrigo BarreraNo ratings yet
- AfricaDocument4 pagesAfricaRodrigo BarreraNo ratings yet
- ChinaDocument6 pagesChinaRodrigo BarreraNo ratings yet
- Comparative Evaluation of Topical Versus Intrastromal Voriconazole As An Adjunct To Natamycin in Recalcitrant Fungal Keratitis.Document5 pagesComparative Evaluation of Topical Versus Intrastromal Voriconazole As An Adjunct To Natamycin in Recalcitrant Fungal Keratitis.Rodrigo BarreraNo ratings yet
- Factors Affecting Treatment Outcomes With Voriconazole in Cases With Fungal Keratitis.Document5 pagesFactors Affecting Treatment Outcomes With Voriconazole in Cases With Fungal Keratitis.Rodrigo BarreraNo ratings yet
- Factors Affecting Treatment Outcomes With Voriconazole in Cases With Fungal Keratitis.Document5 pagesFactors Affecting Treatment Outcomes With Voriconazole in Cases With Fungal Keratitis.Rodrigo BarreraNo ratings yet
- Argon Laser Phototherapy in The Treatment of Refractory Fungal Keratitis.Document3 pagesArgon Laser Phototherapy in The Treatment of Refractory Fungal Keratitis.Rodrigo BarreraNo ratings yet
- 1 s2.0 S0883944113001883 MainDocument12 pages1 s2.0 S0883944113001883 MainRodrigo BarreraNo ratings yet
- n57 Obesity Guidelines 131204Document232 pagesn57 Obesity Guidelines 131204Rodrigo BarreraNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- In Silico Sequence Analysis, Homology Modeling and Function Annotation of Ocimum Basilicum Hypothetical Protein G1CT28 - OCIBADocument8 pagesIn Silico Sequence Analysis, Homology Modeling and Function Annotation of Ocimum Basilicum Hypothetical Protein G1CT28 - OCIBAmariohuangNo ratings yet
- Nital EtchDocument2 pagesNital EtchJohn GeddesNo ratings yet
- NMR Lecture SOSDocument43 pagesNMR Lecture SOSpoornanandhanNo ratings yet
- Lecture Notes Materials and Ecological EngineeringDocument463 pagesLecture Notes Materials and Ecological EngineeringInhake AutechreNo ratings yet
- Axis TurbineDocument7 pagesAxis TurbineBhertrand GomesNo ratings yet
- Effects of Three Different Dietary Binders On Juvenile Sea CucumberDocument8 pagesEffects of Three Different Dietary Binders On Juvenile Sea CucumberEnrique MartinezNo ratings yet
- Deocument 9172Document21 pagesDeocument 9172jeffrey.beach2560% (1)
- Eugenio, MC Micko J. Bscrim - 2a-Org. Chem Module 1.1 Post Assessment ActivityDocument6 pagesEugenio, MC Micko J. Bscrim - 2a-Org. Chem Module 1.1 Post Assessment Activitycj santosNo ratings yet
- Risk Assesment For Sand Blasting and PaintingDocument6 pagesRisk Assesment For Sand Blasting and PaintingRochdi Bahiri100% (10)
- Graphene and Semiconductors: International Webinar OnDocument3 pagesGraphene and Semiconductors: International Webinar Onhong kongNo ratings yet
- Main PropulsionDocument27 pagesMain PropulsionalsitorNo ratings yet
- 1996 Seadoo Service Shop ManualDocument316 pages1996 Seadoo Service Shop ManualCésar Augusto100% (1)
- Poultry Growing Drinking Systems Big Dutchman enDocument8 pagesPoultry Growing Drinking Systems Big Dutchman enHeshamKotb0% (1)
- T105 Trojan Data SheetsDocument126 pagesT105 Trojan Data SheetsJose Luis PandoNo ratings yet
- Nutrients Deficiency SymptomsDocument4 pagesNutrients Deficiency SymptomsJodie Mer DayamaNo ratings yet
- Articol Excelent ZerDocument20 pagesArticol Excelent Zerlylya_bejenaruNo ratings yet
- Lecture 1 Ideal Gases and Their MixtureDocument24 pagesLecture 1 Ideal Gases and Their MixtureMuez GhideyNo ratings yet
- 1 Introduction To Manufacturing ProcessesDocument32 pages1 Introduction To Manufacturing ProcessesZubair Ali100% (1)
- Applications and Impact of Nanocellulose Based AdsorbentsDocument24 pagesApplications and Impact of Nanocellulose Based AdsorbentsLuiz CardNo ratings yet
- Drying in Mass TransferDocument57 pagesDrying in Mass TransferMohammad JunaidNo ratings yet
- Laboratory Activity # 1 MICROBIOLOGYDocument4 pagesLaboratory Activity # 1 MICROBIOLOGYatvillasNo ratings yet
- John Cross (Editor) - Anionic Surfactants-Analytical Chemistry, Second Edition, (1998, CRC Press) (10.1201 - 9780367813130) - Libgen - LiDocument367 pagesJohn Cross (Editor) - Anionic Surfactants-Analytical Chemistry, Second Edition, (1998, CRC Press) (10.1201 - 9780367813130) - Libgen - LiGerónimo PerazzoNo ratings yet
- Concentration Term Jee Main Selected 2Document3 pagesConcentration Term Jee Main Selected 2aebafbigiNo ratings yet
- Hygienic Air Handling Unit CatalogueDocument27 pagesHygienic Air Handling Unit Cataloguemoataz medhatNo ratings yet
- Accesorios de Carga CROSBYDocument52 pagesAccesorios de Carga CROSBYRodolfo AlboresNo ratings yet
- Data Management English 19-04-10-BenningerDocument3 pagesData Management English 19-04-10-BenningermicoswNo ratings yet
- Biodegradation of Keratin Waste Theory and Practical AspectsDocument13 pagesBiodegradation of Keratin Waste Theory and Practical AspectsRodrigo Lara100% (1)
- Study Guide NPT220 (3 July 2017)Document12 pagesStudy Guide NPT220 (3 July 2017)Blessed MuyangaNo ratings yet
- Research Proposal - Chaper 1Document10 pagesResearch Proposal - Chaper 1Kia Javar100% (1)
- 12th Chemistry - Revision Test 1 Model Question Paper - English Medium PDF DownloadDocument4 pages12th Chemistry - Revision Test 1 Model Question Paper - English Medium PDF DownloadAathss AadhiNo ratings yet