Professional Documents
Culture Documents
Obesity
Uploaded by
bertouwCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Obesity
Uploaded by
bertouwCopyright:
Available Formats
Special feature CLINICAL PRACTICE
Obesity in children
Tackling a growing problem
John McLennan, MBBS, FRACP, is a general paediatrician, Bendigo, Victoria. BACKGROUND Childhood and adolescent obesity has increased dramatically over the past 25 years in Australia. Currently over 20% of Australian children are overweight or obese. The National Health and Medical Research Council has recently developed the 'Clinical practice guidelines for the management of overweight and obesity in children and adolescents'. OBJECTIVE This article discusses the assessment and management of childhood and adolescent overweight and obesity. DISCUSSION Children and adolescents with a body mass index over the 85th centile for age are classified overweight and those over the 95th centile, obese. Obesity has significant health consequences for children and adolescents, both in the short term and for their adult life. Family involvement is important in management, particularly in primary aged children. A combination of dietary modification, increased physical activity, decreased sedentary activity and behaviour modification is recommended. tions of overweight/obesity in children.25 This demonstrated a rise in overweight and obese children from 11.8% of boys and 10.7% of girls in the 1985 ACHPER study to over 19% of boys and 21% of girls in the three 19972000 studies (Table 1).15 Most developed and some developing countries worldwide have shown similar trends. and obesity are multifactorial, with changes in energy intake and expenditure related to both subtle and obvious movements in societal behavioural habits. Technology has contributed to obesity by making food more abundant, attractive, promoted and simply obtained. Energy expenditure has been reduced by an increase in sedentary activities, a decrease in the need to expend energy in daily routines, and an increase in the use of cars and other forms of transport. Exercise has now become a formal activity for many children. Fortunately, some of these contributors have been recognised, acknowledged and are being addressed. Table 3 outlines the risk factors for the development of obesity, some of which are modifiable and some not.
Defining childhood obesity
The most widely accepted definition of obesity relates to the body mass index (BMI): weight (kg)/height (2/m). Children above the 85th percentile are classified overweight and those above the 95 th percentile, obese. 6 There are currently no BMI growth reference charts for the Australian population. Pending the development of Australian based reference values, the National Health and Medical Research Council (NHMRC) recommends use of the United States Centres for Disease Control and Prevention BMI percentile charts (Figure 1a, b). Less precise guidelines refer to being more than 20% above expected weight for height on standard percentile charts and the use of skin fold thickness these are not commonly used in children.
Why childhood obesity matters?
Effects in childhood
Short term complications of obesity relate to its effects on growing bone, the endocrine, cardiovascular, and gastrointestinal systems. These problems are not rare and may be identified in most general practices (Table 4). The prevalence of type 2 diabetes is increasing children and adolescents, particularly in certain ethnic groups, including Aboriginal and Torres Strait Islanders and those from middle eastern backgrounds. This increase appears to be associated with high levels of obesity in these populations.6
Why are obesity rates increasing?
Genetic, endocrine and other medical problems can cause obesity in children. Some genetic, endocrine and other medical problems may have obesity as a significant presenting factor but the contribution they make to the overall level of obesity is small (Table 2). Apart from Prader-Willi syndrome, where hyperphagia is a major issue, the management of obesity in these children is likely to be secondary to other problems. The causes of the general increase in overweight
he increasing prevalence of overweight and obese children in Australia since the mid 1980s is well documented. The 1985 Australian Health and Fitness survey was conducted by the Australian Council for Health, Physical Education and Recreation (ACHPER) on a sample of over 8000 Australian school children, aged 715 years.1 Booth et al compared this data to three more recent studies in the light of current defini-
Effects in adult life
Childhood obesity tracks into adulthood, ie. obese children are likely to remain obese adults, with the associated health risks. Studies cited in the NHMRC obesity guidelines reveal that up to 50% of obese
Reprinted from Australian Family Physician Vol. 33, No. 1/2, January/February 2004
33
Clinical practice: Obesity in children tackling a growing problem
Figure 1a, b. CDC BMI percentile charts. Reproduced with permission: Centers for Disease Control and Prevention, 2000
Table 1. Trends in obesity in Australian children
ACHPER 19851 n=8492 Boys Girls % overweight 11.8 10.7 or obese SFPAS 19973 n=5518 Boys Girls 20.1 21.3 NNS 19984 n=2962 Boys Girls 19.3 22.3 HOYUS 20005 n=3104 Boys Girls 21.1 23.5
Table 2. Medical conditions associated with childhood obesity
Chromosomal Prader-Willi, Down syndrome, Lawrence-Moon-Bardet-Biedl Endocrine Cushing syndrome, hypothyroidism, GH deficiencies, hypogonadism Pharmacological Antimigraine, antihistamine, antiepileptic, haloperidol, resperidone, tricyclic antidepressants Psychiatric Depression, psychogenic polyphagia seem to recognise they are overweight or have accepted their stature. However, they may be unaware of both the short term and adult health consequences of obesity in their children. The role of the medical profession, therefore, should be to: identify obesity discuss health related factors, and recommend effective interventions.
Source: Booth2 as cited in NHMRC guidelines6
adolescents remain obese in adulthood.713 The greater the degree of overweight, and the later in adolescence it persists, the greater the likelihood of adult obesity. In addition, obesity in childhood is associated with increased adult cardiovascular mortality, regardless of adult weight.1418
NHMRC, 6 the recruitment of Australian cricket star Brett Lee to encourage increased activity and fitness in children, and the increasing availability of low fat options on the fast food market.
What can GPs do?
With so much community activity, what is the role of the medical profession and, in particular, general practice? The effects of obesity on self esteem, mood and social interaction are understandable, but seem insufficient for many to motivate change in their habits and lose weight. Many do not
Community role
Recognition of the rising incidence of obesity has led to responses such as the issuing of new dietary guidelines for children and adolescents and management guidelines for childhood and adolescent obesity by the
34
Reprinted from Australian Family Physician Vol. 33, No. 1/2, January/February 2004
Clinical practice: Obesity in children tackling a growing problem
Table 3. Risk factors for obesity6
Nonmodifiable Genetic predisposition: parental obesity is a strong risk factor for future obesity Ethnicity: overweight and obesity is higher in those of middle eastern and Mediterranean origin A number of single gene abnormalities (Table 2) Medical conditions (Table 2) High weight for gestational age babies Low weight for gestational age babies with rapid catch up Modifiable Television viewing: US studies show positive correlation between television viewing and overweight (evidence is not yet available for other small screen entertainments) Reduced physical activity energy expenditure
Table 4. Pathology associated with obesity
Orthopaedic Slipped femoral epiphysis, genu valgum Endocrine Diabetes type 2, advanced growth, early puberty, polycystic ovary syndrome Cardiovascular Hypertension, hyperlipidemia, cor pulmonale Respiratory Obstructive sleep apnoea, Pickwickian syndrome Hepatic Fatty liver, cholelithiasis Psychological and social problems Impaired psychosocial function is greater in females and with increasing age Adult obesity and complications
Disordered eating in a parent Certain medical conditions (Table 2)
NB: The role of diet composition in the role of overweight/obesity in children is unclear and more studies are required to elucidate this. Breastfeeding is protective against childhood obesity
Assessment of obesity
To identify, assess and monitor children with obesity it is important to: calculate BMI and plot this on percentile charts, and measure waist circumference. Although there are as yet no Australian reference values for waist circumference in children, direct measurements of central fat correlates with cardiovascular risk. 6 Establishing a baseline and serial measurements are important in monitoring response to interventions.
Acanthosis nigrans and those from certain ethnic backgrounds (eg. Aboriginal and Torres Strait Islander, middle eastern).
Management of obesity
Before considering an intervention, it needs to be established whether the parents, and preferably the child, agree there is a problem. Familial factors, whether physiological, psychological or cultural, are relevant. Change will not occur without agreement and motivation in a family setting. The NHMRC guidelines state: For children and adolescents, there is (level III2) evidence that weight management programs that involve parents achieve better outcomes than programs that do not. For children of primary school age ... a program that involves parents alone does better than one that requires regular attendance by their children as well. The evidence for effective intervention for obesity is not strong. There is a single review in the Cochrane Library.19 A meta-analysis was not possible because of the variation in populations, measurements of obesity and aims of outcomes. To be expected, specialist clinics with physicians, dietician and psychologists and, presumably, motivated clients did best. In the absence of clear evidence as to which strategies are the most effective in childhood and adolescent obesity, the NHMRC recommendations are to make use
Investigations
Generally, investigations are not necessary for overweight or mildly obese children. For those with moderate obesity, and associated physical signs, blood glucose (postprandial), serum lipids, liver function tests, ultrasound of the liver and thyroid function tests should be considered. In some cases investigation for an underlying medical cause may be appropriate, eg. chromosomes, adrenal function, growth hormone. The NHMRC recommends: a fasting lipid profile should be considered in obese children and adolescents, particularly those with a family history of cardiovascular risk factors fasting insulin and glucose should be considered in obese children, particularly with a family history of type 2 diabetes,
of all the conventional components of weight management.6 These are: dietary modification increased physical activity decreased sedentary activity family involvement, and behaviour modification. The following strategies are suggested to stimulate ideas that may make a difference: Encourage appropriate eating patterns from a young age see Table 5 and NHMRC website for current guidelines Parents should have an appropriate body image of their children, ie. it is normal to see a childs ribs School canteens should actively promote appropriate eating patterns Avoid using food as a reward Encourage an increase in casual activity, eg. walking to school Reduce sedentary pursuits, especially those associated with eating, eg. after school television. Lose the remote control! Information about dietary recommendations in the waiting room might include the idea of BMI. Offer to measure BMI and help with weight loss if parents agree. Aim for a small initial weight loss, celebrate it and consolidate it Encourage a long term change of life habits. Look for positives in these
35
Reprinted from Australian Family Physician Vol. 33, No. 1/2, January/February 2004
Clinical practice: Obesity in children tackling a growing problem
Table 5. NHMRC recommendations for healthy eating in children20
Encourage and support breastfeeding Physical activity is important for all children and adolescents Enjoy a wide variety of nutritious foods Children and adolescents should be encouraged to: eat plenty of vegetables, legumes and fruits eat plenty of cereals (including bread, pasta, rice and noodles), preferably wholegrain include lean meat, fish, poultry and/or alternatives include milks, yoghurts, cheese and/or alternatives (reduced fat milks are not suitable for children under 2 years but reduced fat varieties should be encouraged for older children and adolescents) choose water as a drink (alcohol is not recommended for children) Care should be taken to: limit saturated fat and moderate total fat intake (low fat diets are not suitable for infants) choose foods low in salt consume only moderate amounts of sugars and foods containing added sugars
material in their surgeries, contact with patients, and community activities (eg. visits to schools) have a duty to include obesity in their list of preventable diseases.
6.
Summary of important points
Children with a BMI over the 85 centile for age are classified as overweight. Children with a BMI over the 95th centile for age are classified as obese. Follow NHMRC recommendations for healthy eating in children and adolescents. Involve parents in weight management in children, particularly those of primary school age. A combination of dietary modification, increased physical activity, decreased sedentary activity and behaviour modification is recommended for treatment of overweight and obese children.
th
7.
8.
9.
10.
11.
Resources
BMI percentile charts are available on the Royal Childrens hospital website at: http://www.rch.org.au/emplibrary/genmed/ cdc_bmiboys.pdf http://www.rch.org.au/emplibrary/genmed/cdc_bmi girls.pdf NHMRC obesity management guidelines: www.obesityguidelines.gov.au. Hard copies are available free to GPs. Order forms are on the website NHMRC. Food for Health: Dietary guidelines for children and adolescents in Australia. Canberra: Commonwealth Department of Health and Ageing, 2003. Available at: http://www.nhmrc.gov.au/ publications/order.htm To obtain copies of pamphlets, poster or A4 information booklet phone 1800 020 103 extension 8654 (toll free number) or email: phd.publications@health.gov.au.
12.
13.
14.
15.
16. 17.
changes apart from weight loss, eg. a sport or physical activity that is seen by the child as cool and rewarding.
Conclusion
Obesity is an increasing problem in children and will lead to significant morbidity in adults in the next decade. There are already changes at the macro level with Brett Lee being appointed as a fitness ambassador specifically aimed and preventing and reducing obesity, articles in the popular press, and some fast food manufacturers promoting nutritional aspects of their products. Unfortunately, the effects of the convenience of packaged food and decreased activity will require a more individual and conscious effort by parents to reverse. General practitioners and others in the health industry through promotional
36
Conflict of interest: none declared.
References
1. Pyke JE. Australian Health and Fitness Survey 1985. Parkside, SA: The Australian Council for Health, Physical Education and Recreation Inc, 1987. Booth ML, Chey T, Wake M, et al. Change in the prevalence of overweight and obesity among young Australians, 19691997. Am J Clin Nutr 2003;77(1):2936. Department of Education and Training. NSW Schools Fitness and Physical Activity Survey. Sydney: NSW Department of Education and Training, 1997. McLennan W, Podger A. National Nutrition Survey Users Guide 1995. Canberra: Australian Government Publishing Service, 1998. Lazarus R, Wake M, Hesketh K, Waters E. Change in body mass index in Australian
18.
19.
2.
20.
3.
primary school children, 19851997. Int J Obes Relat Metab Disord 2000;24:679681. The NHMRC. Clinical practice guidelines for the management of overweight and obesity in children and adolescents. Canberra: Commonwealth Department of Health and Ageing, 2003. Accessed at: http://www.obesityguidelines.gov.au. Guo SS, Huang C, Maynard LM, et al. Body mass index during childhood, adolescence and young adulthood in relation to adult overweight and adiposity: the Fels Longitudinal Study. Int J Obesity Relat Metab Disord 2000;24:16281635. Kelly JL, Stanton WR, McGee R, Silva PA. Tracking relative weight in subjects studied longitudinally from ages 3-13 years. J Paediatr Child Health 1992;28:158161. Peckham CS, Stack O, Simonite V, Wolft OH. Prevalence of obesity in British children born in 1946 and 1958. BMJ 1983;286:12371242. Braddon FEM, Rodgers B, Wadsworth MEJ, Davies JMC. Onset of obesity in a 36 year birth cohort study. BMJ 1986;293:299303. Stark O, Atkins E, Wolff OH, Douglas JW. Longitudinal study of obesity in the National Survey of Growth and Development. BMJ 1981;283:1317. Freedman DS, Srinivasan SR, Valdez RA, et al. Secular increases in relative weight and adiposity among children over two decades: The Bogalusa Heart Study. Pediatrics 1997;99:420426. Freedman DS, Shear CL, Burke GL, et al. Persistence of juvenile onset obesity over eight years: The Bogalusa Heart Study. Am J Public Health 1987;77:588592. Power C, Lake JK, Cole TJ. Measurement and long term health risks of child and adolescent fatness. Int J Obes 1997;21:507526. Freedman DS, Dietz WH, Srinivisan SR, Berenson GS. The relation of overweight to cardiovascular risk factors among children and adolescents: The Bogalusa Heart Study. Pediatrics 1999;103:11751182. Mossberg HO. Forty year follow up of overweight children. Lancet 1989;2:491493. Must A, Jacques PF, Dallal GE, et al. Long term morbidity and mortality of overweight adolescents. A follow up of the Harvard Growth Study. N Engl J Med 1992;327:13501355. Nieto FJ, Szklo M, Comstock GW. Childhood weight and growth rate as predictors of adult mortality. Am J Epidemiol 1992;136:201213. Summerbell CD, Ashton V, Campbell KJ, et al. Interventions for treating obesity in children. In: The Cochrane Library (4). Chichester, UK: John Wiley & Sons, Ltd, 2003. The NHMRC. Food for Health: Dietary guidelines for children and adolescents in Australia. Canberra: Commonwealth Department of Health and Ageing, 2003.
AFP
4.
5.
Correspondence Email: mclennab1@iinet.net.au
Reprinted from Australian Family Physician Vol. 33, No. 1/2, January/February 2004
You might also like
- Habits Loop PDFDocument37 pagesHabits Loop PDFGhassan Qutob94% (34)
- Effects of ObesityDocument48 pagesEffects of ObesityFairuz KangNo ratings yet
- Childhood Obesity BookDocument13 pagesChildhood Obesity Bookapi-282235174No ratings yet
- Proposal On Child ObesityDocument25 pagesProposal On Child ObesityEcaroh Hew Smailliw100% (1)
- Childhood Obesity: Laura Stewart, PHD, RD, RnutrDocument7 pagesChildhood Obesity: Laura Stewart, PHD, RD, RnutryudisNo ratings yet
- AAP Committee On Nutrition-Pediatrics. 2003 112Document9 pagesAAP Committee On Nutrition-Pediatrics. 2003 112Rang PasamanNo ratings yet
- Viewpoint Article: Childhood Obesity - Looking Back Over 50 Years To Begin To Look ForwardDocument5 pagesViewpoint Article: Childhood Obesity - Looking Back Over 50 Years To Begin To Look ForwardichalsajaNo ratings yet
- Obesity Presentation-640Document12 pagesObesity Presentation-640api-284092317No ratings yet
- Role of Hcps in The Prevention of Obesity: Dr. Abdul JabbarDocument73 pagesRole of Hcps in The Prevention of Obesity: Dr. Abdul JabbarMinerva StanciuNo ratings yet
- The Role of Dietary Factors and Food Habits in The Development of Childhood ObesityDocument23 pagesThe Role of Dietary Factors and Food Habits in The Development of Childhood ObesitydnllkzaNo ratings yet
- Obesity in Children and AdolescentsDocument2 pagesObesity in Children and Adolescentsrenas23No ratings yet
- Effectiveness of Nursing Intervention in Prevention of Childhood Obesity: A Systematic ReviewDocument26 pagesEffectiveness of Nursing Intervention in Prevention of Childhood Obesity: A Systematic ReviewAVINASH NNo ratings yet
- NIH Public Access: Author ManuscriptDocument24 pagesNIH Public Access: Author ManuscriptMichael JohnsonNo ratings yet
- Nutrition Journal: Childhood Obesity, Prevalence and PreventionDocument8 pagesNutrition Journal: Childhood Obesity, Prevalence and PreventionqwertyuiopNo ratings yet
- Literature Review On Causes of Childhood ObesityDocument4 pagesLiterature Review On Causes of Childhood Obesityjsmyxkvkg100% (1)
- Obesity in ChildrenDocument15 pagesObesity in ChildrenJohn ConnorNo ratings yet
- Articless41572 023 00435 4.Pdfpdf Button20stickyDocument19 pagesArticless41572 023 00435 4.Pdfpdf Button20stickyTabitha MenezesNo ratings yet
- Overweight COMPETENCY-The Resident Should Be Able ToDocument4 pagesOverweight COMPETENCY-The Resident Should Be Able ToadhitiaNo ratings yet
- How Can Primary Care Providers Manage Pediatric Obesity in The Real World?Document12 pagesHow Can Primary Care Providers Manage Pediatric Obesity in The Real World?Iarias22No ratings yet
- Thesis On Childhood Obesity in IndiaDocument4 pagesThesis On Childhood Obesity in Indiabshpab74100% (2)
- Foundation of Growth and Development: 7-Childhood ObesityDocument15 pagesFoundation of Growth and Development: 7-Childhood ObesityMarah aydiNo ratings yet
- Jebeile, 2022Document15 pagesJebeile, 2022cassio.mouraNo ratings yet
- 2Document52 pages2Evaristus Lokuruka EkadeliNo ratings yet
- Preventing Childhood Obesity Through Family EducationDocument15 pagesPreventing Childhood Obesity Through Family EducationKiana TehraniNo ratings yet
- Childhood Obesity: Causes and Consequences, Prevention and Management.From EverandChildhood Obesity: Causes and Consequences, Prevention and Management.No ratings yet
- CHILDHOOD OBESIT WordDocument31 pagesCHILDHOOD OBESIT WordNICKY SAMBONo ratings yet
- The epidemiological transition: incorporating obesity prevention into nutrition programmesDocument8 pagesThe epidemiological transition: incorporating obesity prevention into nutrition programmesrc513No ratings yet
- Research Paper On Childhood Obesity in IndiaDocument7 pagesResearch Paper On Childhood Obesity in Indiafvg1rph4100% (1)
- Literature Review Article On Childhood ObesityDocument8 pagesLiterature Review Article On Childhood Obesityc5qvf1q1100% (1)
- Research Paper About Childhood ObesityDocument4 pagesResearch Paper About Childhood Obesityafnhdqfvufitoa100% (1)
- Obesity Thesis PDFDocument8 pagesObesity Thesis PDFmariaparkslasvegas100% (2)
- Childhood Obesity Research Paper PDFDocument5 pagesChildhood Obesity Research Paper PDFfvjebmpk100% (1)
- Childhood Obesity Research Paper ExampleDocument5 pagesChildhood Obesity Research Paper Examplecakvaw0q100% (1)
- Literature Review FinalDocument11 pagesLiterature Review Finalapi-253949835No ratings yet
- Pediatric Obesity and Cardiometabolic Disorders: Risk Factors and BiomarkersDocument19 pagesPediatric Obesity and Cardiometabolic Disorders: Risk Factors and BiomarkersPriscila Lemasson DuranteNo ratings yet
- Management of Childhood DiabetesDocument10 pagesManagement of Childhood Diabetesmcruzin12No ratings yet
- Obes CHDocument21 pagesObes CHFiorella Portella CordobaNo ratings yet
- Clinical Evaluation of The Obese Child and Adolescent (UptoDate Mai 013)Document59 pagesClinical Evaluation of The Obese Child and Adolescent (UptoDate Mai 013)jose matosNo ratings yet
- International Childhood Obesity Prevention StrategiesDocument12 pagesInternational Childhood Obesity Prevention StrategiesMarkNo ratings yet
- International Journal of Obesity outlines European perspective on pediatric obesityDocument8 pagesInternational Journal of Obesity outlines European perspective on pediatric obesityDyah Annisa AnggrainiNo ratings yet
- Research Paper On Childhood Obesity PDFDocument4 pagesResearch Paper On Childhood Obesity PDFzhzafmhkf100% (1)
- Obesity and Physical Activity Literature ReviewDocument5 pagesObesity and Physical Activity Literature Reviewea8d1b6n100% (1)
- Childhood Obesity A Global Public Health Crisis (International Journal of Preventif Medicine)Document7 pagesChildhood Obesity A Global Public Health Crisis (International Journal of Preventif Medicine)faisalNo ratings yet
- Literature ReviewDocument6 pagesLiterature Reviewapi-550562221No ratings yet
- Childhood Obesity Research Paper SampleDocument4 pagesChildhood Obesity Research Paper Samplepxihigrif100% (1)
- Obesity General Presentation: Body Mass Index (BMI) Is Calculated As Weight (KG) Divided by Height Squared (MDocument8 pagesObesity General Presentation: Body Mass Index (BMI) Is Calculated As Weight (KG) Divided by Height Squared (MAssma Haytham MuradNo ratings yet
- Childhood Obesity PDFDocument7 pagesChildhood Obesity PDFdevdoll24No ratings yet
- Childhood Obesity Research Paper ThesisDocument5 pagesChildhood Obesity Research Paper ThesisCourtney Esco100% (2)
- Briefing Causes of Childhood ObesityDocument3 pagesBriefing Causes of Childhood ObesityHafiz hanan Hafiz hananNo ratings yet
- 13E3 02 Z PoprawkamiDocument5 pages13E3 02 Z PoprawkamiTophat CherryNo ratings yet
- Obesidad InfantilDocument13 pagesObesidad InfantilBrenda Anali Pariona NapaNo ratings yet
- Bariatric SurgeryDocument15 pagesBariatric SurgeryIsabela Rebellon MartinezNo ratings yet
- Childhood Obesity Prevention MLRDocument10 pagesChildhood Obesity Prevention MLRdsaitta108100% (1)
- Nutrients 12 03134Document27 pagesNutrients 12 03134Meryan MirallesNo ratings yet
- Childhood Obesity Research Paper UkDocument5 pagesChildhood Obesity Research Paper Ukxilllqwhf100% (1)
- Childhood ObesityDocument146 pagesChildhood ObesityLe HuyNo ratings yet
- Childhood ObesityDocument42 pagesChildhood ObesityLaTasha Ann Steven100% (3)
- Obesity Is The Most Nutritional Among Children Developed CountriesDocument14 pagesObesity Is The Most Nutritional Among Children Developed CountriesBulanBiruNo ratings yet
- Thesis ObesityDocument8 pagesThesis ObesityProfessionalPaperWritingServiceManchester100% (2)
- Nutrition and Childhood ObesityDocument8 pagesNutrition and Childhood ObesityErick MuthengiNo ratings yet
- Childhood Obesity: Causes, Consequences and Prevention ApproachesFrom EverandChildhood Obesity: Causes, Consequences and Prevention ApproachesNo ratings yet
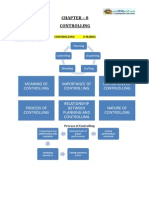
- Directing and Leadership Concepts ExplainedDocument9 pagesDirecting and Leadership Concepts ExplaineddeepashajiNo ratings yet
- Police Injustice Responding Together To Chaengnge The StoryDocument4 pagesPolice Injustice Responding Together To Chaengnge The StorydeepashajiNo ratings yet
- Article Speech Writing PDFDocument14 pagesArticle Speech Writing PDFdeepashajiNo ratings yet
- Article Speech Writing PDFDocument14 pagesArticle Speech Writing PDFdeepashajiNo ratings yet
- NWMP Engfull PackageDocument38 pagesNWMP Engfull Packagedeepashaji100% (1)
- 170 Eng 10Document224 pages170 Eng 10deepashajiNo ratings yet
- English MattersDocument1 pageEnglish MattersdeepashajiNo ratings yet
- 12 Business Studies Impq CH08 ControllingDocument9 pages12 Business Studies Impq CH08 ControllingdeepashajiNo ratings yet
- 12 Business Studies Impq CH09 Financial ManagementDocument13 pages12 Business Studies Impq CH09 Financial ManagementdeepashajiNo ratings yet
- Eng20110310 100610 Media Backgrounder ANPDocument1 pageEng20110310 100610 Media Backgrounder ANPdeepashajiNo ratings yet
- The Ethical Issues Arising From The Relationship Between Police and MediaDocument76 pagesThe Ethical Issues Arising From The Relationship Between Police and Mediaj_townendNo ratings yet
- Pages Froebom Police StoriesDocument17 pagesPages Froebom Police StoriesdeepashajiNo ratings yet
- Areportnnual Report 2009Document67 pagesAreportnnual Report 2009deepashajiNo ratings yet
- 38432reading 4Document28 pages38432reading 4deepashajiNo ratings yet
- Eng080221 LawSocietyReviewPolicingDocument44 pagesEng080221 LawSocietyReviewPolicingdeepashajiNo ratings yet
- QLD Legislative Assembly Standing RulesDocument130 pagesQLD Legislative Assembly Standing RulesdeepashajiNo ratings yet
- Commonlit Reading LiteratureDocument77 pagesCommonlit Reading LiteraturedeepashajiNo ratings yet
- Police On Police ShootingsDocument83 pagesPolice On Police ShootingsJason SmathersNo ratings yet
- Aswrmilan Document Jan10Document5 pagesAswrmilan Document Jan10deepashajiNo ratings yet
- Nucenglear DisarmamentCF909Document20 pagesNucenglear DisarmamentCF909deepashajiNo ratings yet
- Police Injustice Responding Together To Chaengnge The StoryDocument4 pagesPolice Injustice Responding Together To Chaengnge The StorydeepashajiNo ratings yet
- Readingporqn01 - 2586Document1 pageReadingporqn01 - 2586deepashajiNo ratings yet
- Disreadingarmament Yearbook-Other Publications Fact SheetDocument2 pagesDisreadingarmament Yearbook-Other Publications Fact SheetdeepashajiNo ratings yet
- Readingporqn01 - 2586Document1 pageReadingporqn01 - 2586deepashajiNo ratings yet
- Engl 07Document17 pagesEngl 07deepashajiNo ratings yet
- Reading PM1781Document16 pagesReading PM1781deepashajiNo ratings yet
- Engl 07Document17 pagesEngl 07deepashajiNo ratings yet
- Thesis 07Document82 pagesThesis 07Dhanyaa NairNo ratings yet
- Parliamentary Procedure: Simplified Handbook ofDocument23 pagesParliamentary Procedure: Simplified Handbook ofdeepashajiNo ratings yet