Professional Documents
Culture Documents
Calcium Channel Blockers (CCBS)
Uploaded by
Yohanes SutrisnoOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Calcium Channel Blockers (CCBS)
Uploaded by
Yohanes SutrisnoCopyright:
Available Formats
Drug Classes
CALCIUM CHANNEL BLOCKERS (CCBs)
Calcium channel blockers (CCBs) or calcium antagonists, are among the most widely used drugs in cardiovascular medicine with roles not only in hypertension but also in angina and (for some CCBs) tachyarrhythmias.
Examples
Amlodipine Diltiazem Felodipine Isradipine Lacidipine Lercanidipine Nicardipine Nifedipine Nisoldipine Verapamil
Mechanism of action CCBs promote vasodilator activity (and reduce blood pressure) by reducing calcium influx into vascular smooth muscle cells by interfering with voltage-operated calcium channels (and to a lesser extent receptor-operated channels) in the cell membrane. Interference with intracellular calcium influx is also important in cardiac muscle, cardiac conduction tissue and gastrointestinal smooth muscle. In cardiac tissues, CCBs have potential for negative inotropic, chronotropic and dromotropic activity while the gastrointestinal effects predispose to constipation. These effects vary with different agents according to ability to penetrate cardiac and other tissues, relative affinity for calcium channels in different tissues and the influence of reflux cardiac stimulation secondary to peripheral vasodilation.
Although often considered as a single class, CCBs can be subdivided according to structural and functional distinctions. Dihydropyridine derivates : amlodipine, felodipine, isradipine, lacidipine, lercanidipine, nicardipine, nifedipine, nisoldipine Phenylalkylamine : verapamil Benzothiazepine derivative : diltiazem
G:\Website\Drug Classes\Drug Classes Final Copy Dec 2008\Calcium Channel Blockers.doc
Dihydropyridine derivatives have pronounced peripheral vasodilator properties and intense reflex cardiac stimulation overcomes any direct cardiac effects. Verapamil and diltiazem are also vasodilators but the balance of actions is such that these drugs have noticeable cardiac effects including reduced heart rate (rate-limiting CCBs).
Pharmacokinetics Most CCBs have low and variable oral bioavailability because of extensive first-pass metabolism. Half-life is relatively short (< 12 hours). The exception is amlodipine which, although extensively metabolised, has a substantially longer half-life (> 40 hours). Diltiazem and verapamil tend to inhibit drug metabolism. This enzyme inhibitory effect is a potential source of drug interactions e.g. with cyclosporin.
Adverse effects Dihydropyridines - headache and flushing due to peripheral vasodilation - tachycardia and palpitation secondary to reflex activation of the sympathetic nervous system Particularly with rapid-onset and short-acting agents (usually declines with time) - swelling of ankles and occasionally hands due to disturbance of haemodynamics of microcirculation (preferential pre-capillary arteriolar vasodilation) - gum hypertrophy Long-term effects (can arise many months after treatment initiated and may be more common with long-acting agents) Rate-limiting CCBs - bradycardia and atrio-ventricular conduction delay due to direct cardiac effects - constipation with verapamil Early onset vasodilator effects less than with dihydropyridines
Practical issues All CCBs are effective antihypertensive agents because of peripheral vasodilator activity. Blood pressure reduction appears to be more marked in those with low renin hypertension such as the elderly and those of Afro-Caribbean descent. Earlier formulations of some dihydropyridines, such as nifedipine capsules, have a rapid onset of action, unpredictable effects on blood pressure and are accompanied by reflex tachycardia and activation of the renin-angiotensin system. Angina can be precipitated. These formulations have no place in the management of hypertension even in the emergency setting. Long-acting dihydropyridine drugs, such as amlodipine, or other CCBs in once-daily formulations are preferred. CCBs combine well with drugs which block the reninangiotensin system (ACE inhibitors and angiotensin receptor blockers) to produce overall antihypertensive effects which are at least additive.
G:\Website\Drug Classes\Drug Classes Final Copy Dec 2008\Calcium Channel Blockers.doc
Side effects can limit the utility of CCBs. Vasodilator effects of dihydropyridines are less marked with naturally long-acting drugs or sustained release formulations. Since peripheral oedema is a consequence of disturbance of the microcirculation, prescription of a diuretic is not helpful. The combined pre-capillary and post-capillary action of lercanidipine may reduce the frequency of this side effect. Peripheral oedema may also be reduced by co-administration of an ACE inhibitor or angiotensin receptor blocker, drugs which cause post-capillary vasodilation. Nondihydropyridines cause less peripheral oedema but are negatively inotropic and chronotropic, and should therefore be avoided in patients with compromised left ventricular function and should be used with extreme caution in combination with beta-blockers. However, the negative cardiac effects of diltiazem and verapamil reduce myocardial oxygen demand such that these drugs are the preferred form of CCB as monotherapy in angina. Rate-limiting CCBs also have a role in the management of tachyarrhythmias such as atrial fibrillation.
Dihydropyridine calcium channel blockers are available in single pill combinations with betablocker or angiotensin receptor blocker; verapamil is available in combination with an ACE inhibitor. These preparations may improve compliance, and should be considered, provided there is no cost disadvantage.
Large scale prospective outcome studies have demonstrated benefits in cardiovascular protection with CCBs at least equivalent to those with other antihypertensive agents. Dihydropyridine CCBs may be particularly useful in elderly patients with isolated systolic hypertension. Rate-limiting CCBs have benefits similar to those of beta-blockers post-myocardial infarction.
Compelling indications include hypertension in the elderly and isolated systolic hypertension (dihydropyridines), and angina (rate-limiting CCBs).
Possible indications include angina (dihydropyridines) and post myocardial infarction (ratelimiting CCBs).
Caution is advised with concomitant beta-blocker (rate-limiting CCBs).
Compelling contraindications are heart block and heart failure (rate-limiting CCBs).
In the absence of a compelling indication for another drug or contraindication to a CCB, these drugs should be used as recommended in the NICE/BHS algorithm. step 1 in people aged 55 years or over, or of Afro-Caribbean descent step 2 option with an ACE inhibitor or angiotensin receptor blocker step 3 therapy with an ACE inhibitor or angiotensin receptor blocker plus a thiazide or thiazide-like diuretic
G:\Website\Drug Classes\Drug Classes Final Copy Dec 2008\Calcium Channel Blockers.doc
You might also like
- Bihs PDFDocument4 pagesBihs PDFFredrikus Lay Berkh MansNo ratings yet
- Lecture 1 antihypertensionSDSDocument7 pagesLecture 1 antihypertensionSDSSara AbbasNo ratings yet
- Anti-Anginal Drugs PharmacologyDocument24 pagesAnti-Anginal Drugs PharmacologyDharun RanganathanNo ratings yet
- Drugs Used in Heart FailureDocument27 pagesDrugs Used in Heart Failurealeah morenoNo ratings yet
- beta-blockers-and-calcium-channel-blockersDocument34 pagesbeta-blockers-and-calcium-channel-blockersnevena.stankovic986No ratings yet
- PharmaAntianginal DrugsDocument175 pagesPharmaAntianginal DrugsNidal AbboudNo ratings yet
- Drugs For Systemic Hypertension and Angina: What's New?Document6 pagesDrugs For Systemic Hypertension and Angina: What's New?Diana GarcíaNo ratings yet
- Heat Failure DrugsDocument8 pagesHeat Failure DrugsDaniel MwiluNo ratings yet
- Pharmacology Chapter 42 p-3Document19 pagesPharmacology Chapter 42 p-3sho bartNo ratings yet
- Cardio Lab MedsDocument11 pagesCardio Lab MedsDianne Erika MeguinesNo ratings yet
- Case Study Number 1Document5 pagesCase Study Number 1Kevin Kyle RizarriNo ratings yet
- Anti Hypertensive 20191211Document35 pagesAnti Hypertensive 20191211helloitsmenadNo ratings yet
- Pharmacotherapy of Hypertention TerbaruDocument45 pagesPharmacotherapy of Hypertention TerbarulisaNo ratings yet
- Angina PectorisDocument4 pagesAngina PectorisKrishnendu RayNo ratings yet
- HTN Treatment Options: Choosing the Right DrugDocument46 pagesHTN Treatment Options: Choosing the Right DrugvishvasNo ratings yet
- Ischemic Heart Diease PDFDocument33 pagesIschemic Heart Diease PDFMahamed Wefkey OmranNo ratings yet
- Calcium Channel Blockers: Mechanisms, Types, Uses & Side EffectsDocument6 pagesCalcium Channel Blockers: Mechanisms, Types, Uses & Side EffectsManyal Kutin KoakNo ratings yet
- Cardiac ArrhythmiaDocument101 pagesCardiac ArrhythmiaYuvraj ChauhanNo ratings yet
- Anesthetic Management of The Hypertensive Patient: Part II: Continuing Education in Honor of Norman Trieger, DMD, MDDocument8 pagesAnesthetic Management of The Hypertensive Patient: Part II: Continuing Education in Honor of Norman Trieger, DMD, MDFitri Aesthetic centerNo ratings yet
- UKMLA QbankDocument1 pageUKMLA Qbankdrjames730No ratings yet
- Pharmacology 3 - Management of Heart FailureDocument59 pagesPharmacology 3 - Management of Heart Failurealbatros000No ratings yet
- ACE Inhibitors and ARBsDocument20 pagesACE Inhibitors and ARBsMylene MendozaNo ratings yet
- Chapter 17 Cardiovascular DrugsDocument35 pagesChapter 17 Cardiovascular Drugsaisyahasrii_No ratings yet
- 6.a.antianginal DrugsDocument19 pages6.a.antianginal DrugswinnirNo ratings yet
- 10 and 11 Treatment of Hypertension and AnginaDocument10 pages10 and 11 Treatment of Hypertension and AnginaBrandon AviciiNo ratings yet
- Drugs Without Positive Inotropic Effect Used in HFDocument12 pagesDrugs Without Positive Inotropic Effect Used in HFDana HamarshehNo ratings yet
- ACE Inhibitors or ARBsDocument3 pagesACE Inhibitors or ARBsJill QuilangNo ratings yet
- Pharmacotherapy of Congestive Heart Failure (CHF)Document163 pagesPharmacotherapy of Congestive Heart Failure (CHF)Aditya rathoreNo ratings yet
- Vasodil - Ischemic Heart DiseaseDocument52 pagesVasodil - Ischemic Heart DiseaseNorms YoramNo ratings yet
- AntiHypertensives (Autosaved)Document64 pagesAntiHypertensives (Autosaved)UsamaNo ratings yet
- Obat Yang Bekerja Pada Sistem KardiovaskulerDocument18 pagesObat Yang Bekerja Pada Sistem KardiovaskulerMuhammad IkbalNo ratings yet
- Anti Hypertensive Drugs - ACE InhibitorDocument16 pagesAnti Hypertensive Drugs - ACE InhibitorApurba Sarker Apu100% (1)
- Cardiovascular System Pharmacology: Pharmacology Ii DR E KeziaDocument15 pagesCardiovascular System Pharmacology: Pharmacology Ii DR E KeziaJohnNo ratings yet
- ACE Inhibitors & Angiotensin II Antagonists: October 1997Document4 pagesACE Inhibitors & Angiotensin II Antagonists: October 1997indee533No ratings yet
- Antihypertension: Prajogo WibowoDocument45 pagesAntihypertension: Prajogo WibowoDesti Ratna PutriNo ratings yet
- Antihypertensive Pharmacologic Agents: Nr33 K Burger, Msed, MSN, RN, CneDocument28 pagesAntihypertensive Pharmacologic Agents: Nr33 K Burger, Msed, MSN, RN, CneLopez JoeNo ratings yet
- FARMAKOGNOSI - Obat AntihipertensiDocument7 pagesFARMAKOGNOSI - Obat AntihipertensiTrianisa FebyNo ratings yet
- Cardiovascular Pharmacology ConceptsDocument11 pagesCardiovascular Pharmacology ConceptsHuney Kumar100% (1)
- Congestive Heart Failure Drug TreatmentDocument12 pagesCongestive Heart Failure Drug TreatmentDian NugraNo ratings yet
- Cardiovascular PharmacologyDocument61 pagesCardiovascular PharmacologyTeeOne920% (1)
- Cilnidipine 1Document62 pagesCilnidipine 1dkhandke0% (1)
- Uses and AdministrationDocument5 pagesUses and AdministrationVera CarolinaNo ratings yet
- Ischemic Heart Disease Revised LMKDocument50 pagesIschemic Heart Disease Revised LMKLateef KhanNo ratings yet
- CVS (HF, HTN) PharmacologyDocument99 pagesCVS (HF, HTN) PharmacologyCherenet TomaNo ratings yet
- HP 200704 Pharmacological PDFDocument5 pagesHP 200704 Pharmacological PDFIndira Damar PangestuNo ratings yet
- 1 Antihypertensive DrugsDocument14 pages1 Antihypertensive DrugsReda SoNo ratings yet
- Antihypertensive Drugs: HypertensionDocument8 pagesAntihypertensive Drugs: Hypertensionalmastar officeNo ratings yet
- Antihypertensive Drugs: S. Parasuraman, M.Pharm., PH.D.Document44 pagesAntihypertensive Drugs: S. Parasuraman, M.Pharm., PH.D.Shreya SinhaNo ratings yet
- Angiotensin Receptor Blockers (ARBs) PDFDocument3 pagesAngiotensin Receptor Blockers (ARBs) PDFpriya singhNo ratings yet
- Heart FailureDocument37 pagesHeart FailureNashita NowshinNo ratings yet
- Antihypertensive Drugs: Dr/Azza Baraka Prof of Clinical Pharmacology Faculty of Medicine Alexandria UniversityDocument71 pagesAntihypertensive Drugs: Dr/Azza Baraka Prof of Clinical Pharmacology Faculty of Medicine Alexandria UniversityMoonAIRNo ratings yet
- Vasodilators by Hiren PatelDocument28 pagesVasodilators by Hiren PatelHiren_Patel_2427No ratings yet
- Use of Angiotensin Converting Enzyme Inhibitors in Heart Failure With Reduced Ejection FractionDocument20 pagesUse of Angiotensin Converting Enzyme Inhibitors in Heart Failure With Reduced Ejection FractionTrung NamNo ratings yet
- Anti-Angina Drugs for Chest Pain ReliefDocument60 pagesAnti-Angina Drugs for Chest Pain ReliefPranish SawantNo ratings yet
- Skema HipertensiDocument4 pagesSkema HipertensiAndri wijayaNo ratings yet
- Anti Arrhythmic DrugsDocument91 pagesAnti Arrhythmic DrugsAlex beharuNo ratings yet
- Cardiovascular Endocrinology and Metabolism: Theory and Practice of Cardiometabolic MedicineFrom EverandCardiovascular Endocrinology and Metabolism: Theory and Practice of Cardiometabolic MedicineAndrew J. KrentzNo ratings yet
- NAPLEX Practice Question Workbook: 1,000+ Comprehensive Practice Questions (2023 Edition)From EverandNAPLEX Practice Question Workbook: 1,000+ Comprehensive Practice Questions (2023 Edition)Rating: 4.5 out of 5 stars4.5/5 (3)
- Aural Test BookDocument1 pageAural Test BookYohanes Sutrisno7% (14)
- ADA Standards of Medical Care in Diabetes 2013 PDFDocument56 pagesADA Standards of Medical Care in Diabetes 2013 PDFPatricio Moncayo DonosoNo ratings yet
- 804c Gastroenterology and Hepatology Clinic Exclusion Crit.Document1 page804c Gastroenterology and Hepatology Clinic Exclusion Crit.Yohanes SutrisnoNo ratings yet
- Potent Direct VasodilatorsDocument2 pagesPotent Direct VasodilatorsYohanes SutrisnoNo ratings yet
- Other DiureticsDocument4 pagesOther DiureticsYohanes SutrisnoNo ratings yet
- Hypertension in Pregnancy 2013-G LipkinDocument35 pagesHypertension in Pregnancy 2013-G LipkinYohanes SutrisnoNo ratings yet
- SALT Is Your Food Full of ItDocument4 pagesSALT Is Your Food Full of ItYohanes SutrisnoNo ratings yet
- Replacing MercuryDocument3 pagesReplacing MercuryYohanes SutrisnoNo ratings yet
- Potent Direct VasodilatorsDocument2 pagesPotent Direct VasodilatorsYohanes SutrisnoNo ratings yet
- Thiazide and Thiazide-Like DiureticsDocument3 pagesThiazide and Thiazide-Like DiureticsYohanes SutrisnoNo ratings yet
- Centrally Acting AgentsDocument2 pagesCentrally Acting AgentsYohanes SutrisnoNo ratings yet
- Direct Renin InhibitorsDocument2 pagesDirect Renin InhibitorsYohanes SutrisnoNo ratings yet
- Lesson 6Document1 pageLesson 6Yohanes SutrisnoNo ratings yet
- Angiotensin Receptor Blockers (ARBs) PDFDocument3 pagesAngiotensin Receptor Blockers (ARBs) PDFpriya singhNo ratings yet
- BHS Standard Operating Procedure For ABPMDocument3 pagesBHS Standard Operating Procedure For ABPMYohanes SutrisnoNo ratings yet
- Jazz XmasDocument13 pagesJazz XmasYohanes SutrisnoNo ratings yet
- Beta Adrenoceptor Antagonists (Beta Blockers)Document4 pagesBeta Adrenoceptor Antagonists (Beta Blockers)Yohanes SutrisnoNo ratings yet
- Alpha Adrenoceptor Antagonists (Alpha Blockers)Document2 pagesAlpha Adrenoceptor Antagonists (Alpha Blockers)محمدأميندماجNo ratings yet
- Lesson 1Document1 pageLesson 1Yohanes SutrisnoNo ratings yet
- Lesson 8Document1 pageLesson 8Yohanes SutrisnoNo ratings yet
- Lesson 5Document1 pageLesson 5Yohanes SutrisnoNo ratings yet
- Angiotensin Converting Enzyme (ACE) InhibitorsDocument4 pagesAngiotensin Converting Enzyme (ACE) InhibitorsPutri Mulia HasibuanNo ratings yet
- Lesson 4Document1 pageLesson 4Yohanes SutrisnoNo ratings yet
- Treatment LipidDocument6 pagesTreatment LipidYohanes SutrisnoNo ratings yet
- Lesson 3Document1 pageLesson 3Yohanes SutrisnoNo ratings yet
- What Is A Migraine With AuraDocument2 pagesWhat Is A Migraine With AuraYohanes SutrisnoNo ratings yet
- Lesson 2Document1 pageLesson 2Yohanes SutrisnoNo ratings yet
- Root of Samsung Galaxy Tab 10Document5 pagesRoot of Samsung Galaxy Tab 10Yohanes SutrisnoNo ratings yet
- ADA Standards of Medical Care in Diabetes 2013 PDFDocument56 pagesADA Standards of Medical Care in Diabetes 2013 PDFPatricio Moncayo DonosoNo ratings yet
- Top 10 prescribed drugs dental interactionsDocument14 pagesTop 10 prescribed drugs dental interactionsAnubhuti SabhlokNo ratings yet
- Pharmacology - Cardiovascular DrugsDocument113 pagesPharmacology - Cardiovascular DrugsBenjamin Joel BreboneriaNo ratings yet
- Problems in Oxygenation HPNDocument13 pagesProblems in Oxygenation HPNRoshin TejeroNo ratings yet
- Affordable medicines price listDocument172 pagesAffordable medicines price listMolka BellasfarNo ratings yet
- 11. 201909 抗高血压 antihypertensionDocument72 pages11. 201909 抗高血压 antihypertensionShanon LimNo ratings yet
- Lista preturi medicamenteDocument936 pagesLista preturi medicamenteCristina Elena NicuNo ratings yet
- Amdocal Final PDFDocument5 pagesAmdocal Final PDFSaifur Rahman SuzonNo ratings yet
- Case Presentation of Bipolar Affective Disorder, Current Episode, Manic With Psychotic DisorderDocument37 pagesCase Presentation of Bipolar Affective Disorder, Current Episode, Manic With Psychotic DisorderEarl John Natividad89% (9)
- Tutorial Report 1 Pharmacology and Therapy: Lecturer: Nurmawati Fatimah DR., M.SiDocument34 pagesTutorial Report 1 Pharmacology and Therapy: Lecturer: Nurmawati Fatimah DR., M.SiGitaaNo ratings yet
- Drugs 3Document43 pagesDrugs 3IonuțHerpeșNo ratings yet
- Amlodipine - Drug StudyDocument2 pagesAmlodipine - Drug StudyAcads useNo ratings yet
- Drug StudyDocument21 pagesDrug StudyRemedios Bandong100% (1)
- Pathophysiology Raynauds Phenomenon Schematic DiagramDocument6 pagesPathophysiology Raynauds Phenomenon Schematic DiagramEerie Era0% (1)
- MecamylanimeDocument15 pagesMecamylanimeNoor HaiderNo ratings yet
- Amlodipine CPDocument2 pagesAmlodipine CPRose EchevarriaNo ratings yet
- Amniodarone (Norvasc) Drug SummDocument1 pageAmniodarone (Norvasc) Drug SummWarrenNo ratings yet
- AHA Hypertension Guidelines 2017Document22 pagesAHA Hypertension Guidelines 2017Anonymous elSqPhzKNo ratings yet
- DIURETICS AND UPPER RESPIRATORY DRUGSDocument40 pagesDIURETICS AND UPPER RESPIRATORY DRUGSNiña Jean Tormis AldabaNo ratings yet
- Amlodipine-10mg TabletDocument7 pagesAmlodipine-10mg TabletMd. Abdur RahmanNo ratings yet
- Empr Prescriber's EditionDocument420 pagesEmpr Prescriber's EditionPatel Pratyk100% (1)
- Classifications of Pharmaceutical DrugsDocument31 pagesClassifications of Pharmaceutical DrugsDeepankar Srigyan100% (30)
- Scholarship ExamDocument16 pagesScholarship ExamRicky Vanguardia IIINo ratings yet
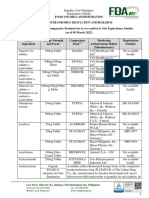
- Food and Drug Administration Center For Drug Regulation and R Food and Drug Administration Center For Drug Regulation and Research EsearchDocument141 pagesFood and Drug Administration Center For Drug Regulation and R Food and Drug Administration Center For Drug Regulation and Research EsearchJha JhaNo ratings yet
- Lercanidipine Drug StudyDocument16 pagesLercanidipine Drug StudylenecarglbnNo ratings yet
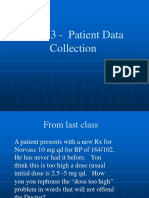
- Rovers - CH - 3 - Patient DataDocument27 pagesRovers - CH - 3 - Patient DataKhalid Bin AliNo ratings yet
- Cardiovascular Agents ReviewerDocument18 pagesCardiovascular Agents ReviewerJoycel CeñidozaNo ratings yet
- Case Study-Congestive Heart FailureDocument71 pagesCase Study-Congestive Heart FailureKentTangcalagan92% (13)
- Diabetes Treatment Plan for 78-Year-Old WomanDocument4 pagesDiabetes Treatment Plan for 78-Year-Old WomanShazaan NadeemNo ratings yet
- Drug Study - AmlodipineDocument1 pageDrug Study - AmlodipineDhanNie Cenita100% (6)
- HTN Topic DiscussionDocument7 pagesHTN Topic Discussionapi-668844754No ratings yet