Professional Documents
Culture Documents
Do Calcium Channel Blockers Increase The Risk of Myocardial
Uploaded by
Yolita Satya Gitya UtamiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Do Calcium Channel Blockers Increase The Risk of Myocardial
Uploaded by
Yolita Satya Gitya UtamiCopyright:
Available Formats
MWAIMIZIMA3
MW
5K
Leikqwe]:40 0LOI
Do calcium channel blockers increase the risk of myocardial infarction in hypertensive patients with diabetes mellitus?
Laura Park Choo Pin Por, PHARMD
Michael F Evans, MD, CCFP
cardiovascular outcomes.5'6 While evidence of this is largely based on observational studies, the general consensus among practitioners has been to avoid shortacting calcium channel blockers, especially immediaterelease nifedipine (eg, Adalat). Long-acting calcium channel blockers have raised fewer concerns. The Appropriate Blood-Pressure Control in Diabetes trial, Research question however, has now added fuel to what seems to be an Are long-acting dihydropyridines, such as nisoldipine already raging fire because it suggests that long-acting (Sular), associated with increased rates of adverse car- dihydropyridine calcium channel blockers could harm diovascular events in hypertensive patients with type 2 hypertensive diabetic patients.! diabetes? Should we continue to prescribe calcium channel blockers for hypertensive patients with type 2 diabetes? Type of article and design How can we integrate the results of this trial with the Double-blind, randomized, parallel-group study. recommendations of the JNC-6 to arrive at a bottomline decision on when to use calcium channel blockers Relevance to family physicians for our hypertensive diabetic patients, if at all? Calcium channel blockers are among the most frequently prescribed medications for treating hyperten- Overview of study and outcomes sion.' They are also widely used for patients with other The main objective of the study was to investigate the illnesses, such as angina pectoris, certain cardiac relative effects of various levels of blood pressure conarrhythmias, and Raynaud's phenomenon. Recent evi- trol on the glomerular filtration rate of hypertensive dence has shown that calcium channel blockers protect and normotensive patients with type 2 diabetes. The the renal systems of hypertensive patients with diabetic secondary objective was to compare nisoldipine with nephropathy.23 In line with this evidence, the Sixth enalapril (Vasotec) for outcomes. such as cardiovascuReport of the Joint National Committee on the lar events, neuropathy, urinary albumin excretion, and Prevention, Detection, Evaluation left ventricular hypertrophy. The and Treatment of Hypertension Critical Appraisal revviews important arti- published study reports on only UNC-6)4 named calcium channel cles in the literaturl e relevant to family a subset of the study populablockers as one of the preferred physicians. Reviews are by family physi- tion-diabetic patients with therapies for patients with hyper- cians, not experts c n the topics. They hypertension. tension and diabetes. Other assess not only the s3trength of the studIn the subset, 470 patients preferred therapies included ies but the "bottom line" clinical impor- were randomized to moderate or angiotensin-converting enzyme tance for family praictice. We invite you intensive antihypertensive regi(ACE) inhibitors, a-blockers, and to comment on theL reviews, suggest mens. All subjects were required low-dose diuretics. articles for review, c)r become a review- to have a diastolic blood pressure Concurrently, enormous con- er. Contact CoordinaLtor, Michael Evans, of at least 80mmHg not treated troversy has arisen around the by e-mail michael.ev.,ans@utoronto.ca or with antihypertensive medicasafety of calcium channel block- by fax (416) 603-58211. tions. Moderate antihypertensive ers, particularly regarding adverse treatrnent was defined as a target
Estacio RO, Jeffers BW, Hiatt WR, Biggi SL, Gifford N, Schrier RW. The effect of nisoldipine as compared with enalapril on cardiovascular events in patients with non-insulin-dependent diabetes and hypertension. NEngl JMed 1998;338:645-52.
Ms Park is a student in the Doctor ofPharmacy Program at the University of Toronto. Dr Choo Pin Por, a pharmacotherapy specialist the Toronto Hospital Family and Community Medicine site, is an Assistant Professor in the Doctor of Pharmacy Program. Dr Evans practises at The Toronto Hospital and teaches in the Department ofFamily and Community Medicine at the University of Toronto.
--
FOR PRESCRIBING INFORMATION SEE PAGE 2556
VOL44: NOVEMBER * NOVEMBRE 1998. Canadian Family Physician . Le Medecin defamille canadien 2405
IA
diastolic blood pressure of 80 to 89mmHg; intensive antihypertensive treatment was defined as a target diastolic blood pressure of 75mmHg. Patients ranged in age from 40 to 74 years and had been diagnosed with type 2 diabetes. Moderate and intensive treatment groups were then further randomized to either nisoldipine or enalapril. If monotherapy with the study medication was inadequate to achieve target blood pressure control, patients could also receive open-label metoprolol (eg, Betaloc) or hydrochlorothiazide (HydroDiuril). Patients who had experienced recent myocardial infarction (MI), cerebrovascular accident (CVA), or coronary artery bypass grafting (CABG) were excluded, as were patients with recent unstable angina, with New York Heart Association functional class 3 or 4 congestive heart failure (CHF), on dialysis, and with serum creatinine levels of >265gmo/L. Baseline cardiovascular diseases (demonstrated on electrocardiogram), such as coronary artery disease (CAD), angina, CVA, CHF, abnormal ankle-brachial index, and left ventricular hypertrophy, were recorded during a placebo run-in period.
receiving nisoldipine more likely to have MIs, they were also more likely to have them earlier than the patients receiving enalapril. A high rate of discontinuations was seen in both groups: 142 patients (60%) in the nisoldipine arm and 129 patients (55%9) in the enalapril arm stopped treatment. Patients receiving nisoldipine were most likely to stop because of headaches, those receiving enalapril because of malaise, fatigue, or uncontrolled hypertension. Rates of discontinuation were not statistically different for the two groups. Analysis of methodology While this study was well-designed and equipped to respond to the intended primary research question, it is important to remember that the cardiovascular data are presented in the context of secondary end point analysis. As such, this is a hypothesis-generating trial that identifies the need for further randomized controlled trials. In addition, the study was limited by the absence of placebo control, making interpretation of the results difficult. Do the results reflect enalapril's protective effect on cardiovascular events, or is nisoldipine exerting a deleterious effect on cardiovascular outcomes? Could it be an interaction of both effects?6 Finally, we cannot exclude the possibility that the findings are a product of the higher treatment discontinuation rate in the nisoldipine group coupled with the greater diuretic or ,B blocker use in the enalapril group.
Results
Patients were followed for 67 months at which time the Drug and Safety Monitoring Committee detected a significant difference in the rate of MIs among patients treated with nisoldipine compared with those treated with enalapril. Termination of nisoldipine treatment was recommended, and patients receiving nisoldipine were switched to enalapril. The two treatment arms were relatively well balanced at entry. Slight differences in baseline characteristics included a lower high-density lipoprotein profile in the enalapril group (1.03 mmol/L vs 1.l1 mmol/L) and a higher percentage of patients with abnormal anklebrachial indices (6% enalapril vs 3% nisoldipine) and with angina (3% enalapril vs < 1% nisoldipine). The treatments provided similar blood pressure control, although more patients receiving enalapril required open-label treatment with f,Bblockers (42% enalapril vs 38% nisoldipine) and diuretics (51% enalapril vs 40% nisoldipine). A higher rate of cardiovascular events (particularly MI) was seen in the nisoldipine group: 25 patients experienced fatal or nonfatal MIs compared with only five in the enalapril arm (adjusted risk ratio 7.0; 95% confidence interval 2.3 to 21.4). These results were consistent throughout both moderate and intensive blood pressure control regimens. Kaplan-Meier survival curves also demonstrated an early split; the split was maintained throughout the study. This suggests that, not only were the patients
Application to clinical practice
The results of this trial reiterate the general consensus that, for all situations, ACE inhibitors should be preferred to calcium channel blockers for diabetic patients with hypertension. The strikingly higher rate of fatal and nonfatal MIs in patients randomized to nisoldipine should not and cannot be ignored. The findings of this trial are consistent with results of the Fosinopril versus Amlodipine Cardiovascular Events Trial,7 which found that diabetic patients randomized to fosinopril (Monopril) for hypertension had a significantly lower risk of vascular events than patients receiving amlodipine (Norvasc). Calculation of the number needed to harm reveals that only 11 patients would have to be treated with nisoldipine instead of enalapril to see one preventable MI. For patients who are intolerant of ACE inhibitors or angiotensin II-receptor antagonists, it would be prudent to avoid calcium channel blockers in favour of other well-established therapies, such as low-dose diuretics and n-blockers.
2406 Canadian Family Physician Le Medecin defamille canadien * VOL 44: NOVEMBER * NOVEMBRE 1998
Bottom line There is insufficient evidence to decide whether calcium channel blockers actually increase the risk of MI or whether the ACE inhibitors exert a cardioprotective effect. The dramatically higher cardiovascular event rate with nisoldipine, however, further confirms that ACE inhibitors should continue to be preferred over calcium channel blockers for hypertensive patients with type 2 diabetes. For diabetic patients receiving calcium channel blocker monotherapy for hypertension, it would be worthwhile to consider switching to ACE inhibitors, because treating 11 people with long-acting dihydropyridines instead of ACE inhibitors for 5 years could allow one preventable MI to occur. For diabetic patients who are ACE-inhibitor intolerant, angiotensin II-receptor antagonists, low-dose diuretics, and even ,-blockers should be initiated rather than long-acting dihydropyridines. Extrapolation of the results of this trial is difficult for diabetic patients receiving both ACE inhibitors and calcium channel blockers, but if monotherapy is even a possibility, physicians should attempt to withdraw the calcium channel blockers. 4
References
1. Beaulieu M-D, Dufresne L, LeBlanc D. Treating hypertension: are the right drugs given to the right patients? Can Fam Physician 1998;44:294-302. 2. Velussi M, Brocco E, Frigato F, Zolli M, Muollo B, Maioli M. Effects of cilazepril and amlodipine on kidney function in hypertensive NIDDM patients. Diabetes 1996;45:216-22. 3. Bakris GL, Copley JB, Vicknair N, Sadler R, Leurgans S. Calcium channel blockers versus other antihypertensive therapies on progression of NIDDM-associated nephropathy. Kidney Int 1996;50:1641-50. 4. Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure. The sixth report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (NC VD. Arch Intern Med 1997;157:2413-46. 5. Psaty BM, Heckbert SR, Koepsell TD. The risk of myocardial infarction associated with antihypertensive drug therapies. JAMA 1995;274:620-5. 6. Cutler JA. Calcium channel blockers for hypertensionuncertainty continues. N Engl J Med 1998;338:679-81. 7. Tatti P, Pahor M, Byington RP, Di Mauro P, Guarisco R, Strollo G. Outcome results of the Fosinopril versus Amlodipine Cardiovascular Events Randomized Trial (FACET) in patients with hypertension and NIDDM. Diabetes Care 1998;21:597-603.
Anaphylactoid reactions during membrane Other: Bioavailability of fosinoprilat not altered Anaphylactoid reactions have been with chlorthalidone, nifedipine, propranolol, in patients dialysed with high-flux hydrochlorothiazide,cimetidine, metoclopramide (e.g., polyacrylonitrile (PAN)) and and propantheline. treated concomitantly with an ACE inhibitor. ADVERSE REACTIONS: Dialysis should be stopped immediately. Severe adverse reactions occurring in 1548 reactions during desensitization: hypertensive patients treated with MONOPRIL Anaphylactoid Angitensn Covertng EzymeInhiitor There have been isolated reports of patients were. angioedema (1 case) and orthostati c INDICATIONS AND CLINICAL USE: experiencing sustained life-threatening hypotension (2.7%). Myocardial infarction Mild to moderate essential hypertension. May be anaphylactoid reactions while receiving ACE (2 cases) and cerebrovascular accident (4 casesn thiazide usedaloe o inassciaionwith used inhibitors during desensitizing treatment with occurred, possibly secondary to excessive ecsie alone in association diuretics. Use in renovascular hypertension not or hymenoptera (bees, wasps) venom. hypotension in high risk patients. In 516 heart established. Use of antihypertensive agents other Valvular Stenosis: Theoretically patients with failure patients, the severe adverse reaction than thiazide diuretics has not been established. aotcseoimihbearikoderae ocuinwthheigstfqecyasnia the management of aprticrstenosis Adjunctive treatment in heart mightpbeatbrisknofodecreasedroccurringmwithmthe:highestfrequencycwasaangina when treated with coronary perfusion failure. Initiate symptomatic congestive petri16%.Itpaeo-otole ypr tension trials (688 patients), the most frequent vasodilators as they do not develop much treatmnt undr medcal suervison Whe used clinical adverse reactions were nausea/vomiting, afterload reduction. in pregnancy during he second and third
O'M ONOPRII! (fosinoprilsodiuni) (fosinoprilsodium) TABLETS 10 and 20 mg
~~~~~exposure: ~~~~~~reported
m~~~embranes
TEAngioTenIn ConverIngIEzymeIONhiio
20-40 mg 00. The occurrence of hypotension after the initial dose may not preclude careful dose titration with MONOPRIL following effective management of hypotension. In severe congestive heart failure with or without renal insufficiency, therapy with MONOPRIL should be with caution (see WARNINGS ~~~~~~~~~~~~initiated Hypotension). A lower starting dose should be considered.
wt er alr,teaysol cauion and No
fai lure,,th e recommended initial dose of MONOPRIL is 10 mg initiated under close medical supervision, IfODO, initial dose is well tolerated, it should be titrated over 1 to 3 weeks to
(see PRECAUTIONS -Drug Interactions). In heart
henalt 10mguOd.binisuhiatewiets Imai-rment:eap
eiiitdwt
cn eatuse n trimester, ACE inhbItors
or
Patintswltb mpaired
~musculoseletal pan,
fori ofleayVA%o hs 1onin ma ras ninuationl ains0npaeb-oto.dCi g ecinswr:dzzns,cog,haacead
Iteradp.
oal hapd,
RenaRenalFunction
COtrietr,ANDCAT Weirs: cnw
WARnINGS:
f
L einehrie
mosietcae* h hne1eervesdo patinswthpeeltiglvrabomltes
Nrsig Mthes: houd nt b adiniteed,
VMIII alt r white to off-hie M0IP1.0m n wthapril ietbr nrvdwihBSo
OORI0ad2
areinvlve adiniter0.3to .5
pregnancy is de
ot recommended. liv~~~edaricUe Nny
ades
supervisiondandbs olwdclsl o h first DuGtIuNTEATIN MONOPRIL ordiureti isoincreased and mohnitrfeunl.1m 00.Rane: COTANeuroeIa/AgraNuocyosis MonitorhitePcatiously-0mgiOD)
iscntiueddueto irsIdoe evets a .%o 6 ains og DOSAGE ANDhADMINISTRATION:1
whie 08%
ompessdytblesoegraedbit
gtbesaeaalbei
0-4mJ
0(aiu
can caue etl eniv effetisoagmethed.d~-s dirtcfotwioohe ay,eoe OORL aC ihibitors Uspeirsegnsiiiyancy and nenatalmorbiity ad moranlitym whn Lthu:Ma6eul1ninraedsrm ihu Falue MONPRseisgenralylueds Heart1mol. adminiteredo pregant wmen.Dscontiue cauiousl abndrmonitor aleelts. cnuctinwteadueicsiho Coadmreinisterg an WAsNIsoon aspsilrqunl.dgxn Blo peressurzie; an g renalawihu
e
haptlbrisetolIryeswqib
lhaed compressedtablet egroup it BRISTonoL-MYERS SQUIB CANADAI I 0nC.ethr PRL MO an20mtblsare,hvev365Cle-d-LisseRd
lT autorzduser Mooraph-yr SquibbeCaonad Ines.
PreCAUinolvdamnis:
Rea maimn:Us Surger/Anestesia:May aument tehyptien
o05m pnprn Ausntais Maytmpars aShorptionof fosadinoptrid. ihcuto,I camnstainiidctd,sprt
shoulde mdsonitoredubot bueforefiand during treatmentin withcontiutoPRL, bheause seveeto e Pdoingriby twot hors.omedhypotrseentson wand m ore 8 rarelytrenalsfailug
of therap requirescntsidrto.frcn dirtieteap,indteaosiiltyofsvee ndvodulume doaeplto. Ifypostesible, Mntherdoepo
PoasimSaringr hyeartailur,iemiacn Diebovsulretc Fresonsemidre:aCoadminsistraitio increasibed AUCo Incinicale trialds,tlearte 2%adCa y2% poasucoiorltb uosemde
sherayumde
(geaerso theanm5.5 mEq/L waseobservdoed in
appoximately 2ont.6%oyetnieptetn
weremonstlre teof-regnavntome.Dsotne
lgevels werndcmaigSremPtaed. m:salt/er Watarsine Bffoavaisabimeityeffsnord torwrai
feunotaltee.
diutcsouldantbeireduce bhefrepy beiscnninguMAePA cowmnjuntion wiu.Atha diueic, wihdtho winthoutirstlMyrnS
ub
VOL 44: NOVEMBER * NOVEMBRE 1998+ Canadian Family Physician Le Medecin defamille canadien 2407
You might also like
- How COVID-19-is-changing-consumer-behaviornow-and-foreverDocument6 pagesHow COVID-19-is-changing-consumer-behaviornow-and-forevermesay83No ratings yet
- Prednisone - Pediatric Drug InformationDocument11 pagesPrednisone - Pediatric Drug InformationYolita Satya Gitya UtamiNo ratings yet
- 1996 Bookmatter FinancialAspectsOfMarketingDocument1 page1996 Bookmatter FinancialAspectsOfMarketingYolita Satya Gitya UtamiNo ratings yet
- Offensive Pricing Strategies For Online PlatformsDocument18 pagesOffensive Pricing Strategies For Online PlatformsYolita Satya Gitya UtamiNo ratings yet
- Structural DeterminantsDocument9 pagesStructural DeterminantsYolita Satya Gitya UtamiNo ratings yet
- 2012cancprevres 5 351 4 Metformin Cscs - SemimDocument5 pages2012cancprevres 5 351 4 Metformin Cscs - SemimYolita Satya Gitya UtamiNo ratings yet
- Educational Case Series Mechanisms of Drug AllergyDocument9 pagesEducational Case Series Mechanisms of Drug AllergyYolita Satya Gitya UtamiNo ratings yet
- American Journal of Kidney Diseases Volume 38 Issue 2 2001 (Doi 10.1053/ajkd.2001.26118) Ali Owda Sayed Osama - Hemodialysis in Management of HypothermiaDocument2 pagesAmerican Journal of Kidney Diseases Volume 38 Issue 2 2001 (Doi 10.1053/ajkd.2001.26118) Ali Owda Sayed Osama - Hemodialysis in Management of HypothermiaYolita Satya Gitya UtamiNo ratings yet
- The Society of Hospital Pharmacists of Australia - Standards of Practice For Clinical Pharmacy - 2004Document25 pagesThe Society of Hospital Pharmacists of Australia - Standards of Practice For Clinical Pharmacy - 2004Yolita Satya Gitya UtamiNo ratings yet
- Journal of Minimally Invasive Gynecology Volume 19 Issue 5 2012 [Doi 10.1016%2Fj.jmig.2012.05.009] Armstrong, Amy J.; Hurd, William W.; Elguero, Sonia; Barker, Nic -- Diagnosis and Management of Endometrial HyperplasiDocument10 pagesJournal of Minimally Invasive Gynecology Volume 19 Issue 5 2012 [Doi 10.1016%2Fj.jmig.2012.05.009] Armstrong, Amy J.; Hurd, William W.; Elguero, Sonia; Barker, Nic -- Diagnosis and Management of Endometrial HyperplasiYolita Satya Gitya UtamiNo ratings yet
- Annals of Allergy, Asthma & Immunology Volume 102 Issue 1 2009 [Doi 10.1016%2FS1081-1206%2810%2960101-9] Nelson, Harold S.; Carr, Warner; Nathan, Robert; Portnoy, Jay M. -- Update on the Safety of Long-Acting Β-AgonisDocument5 pagesAnnals of Allergy, Asthma & Immunology Volume 102 Issue 1 2009 [Doi 10.1016%2FS1081-1206%2810%2960101-9] Nelson, Harold S.; Carr, Warner; Nathan, Robert; Portnoy, Jay M. -- Update on the Safety of Long-Acting Β-AgonisYolita Satya Gitya UtamiNo ratings yet
- ABC of The Upper Gastrointestinal TractDocument63 pagesABC of The Upper Gastrointestinal TractHisham ZayatNo ratings yet
- Sag 40 6 3 0910 355Document8 pagesSag 40 6 3 0910 355Yolita Satya Gitya UtamiNo ratings yet
- XDocument6 pagesXYolita Satya Gitya UtamiNo ratings yet
- Contribution of Lip Proportions To Facial Aesthetics inDocument8 pagesContribution of Lip Proportions To Facial Aesthetics inYolita Satya Gitya UtamiNo ratings yet
- 03 HiralDocument12 pages03 HiralYolita Satya Gitya UtamiNo ratings yet
- 1 s2.0 S0168365912005172 MainDocument7 pages1 s2.0 S0168365912005172 MainYolita Satya Gitya UtamiNo ratings yet
- The Expression of Prolactin and Oxytocin Genes in LactatingDocument5 pagesThe Expression of Prolactin and Oxytocin Genes in LactatingYolita Satya Gitya UtamiNo ratings yet
- Vaginal Drug DeliveryDocument37 pagesVaginal Drug DeliveryYolita Satya Gitya UtamiNo ratings yet
- 1 s2.0 S037851730700244X MainDocument8 pages1 s2.0 S037851730700244X MainYolita Satya Gitya UtamiNo ratings yet
- BradiaritmiaDocument12 pagesBradiaritmiaYolita Satya Gitya UtamiNo ratings yet
- 1219 2521 1 SMDocument10 pages1219 2521 1 SMYolita Satya Gitya UtamiNo ratings yet
- HPLC Analysis of Artificial Sweeteners and Preservatives in Soft DrinksDocument12 pagesHPLC Analysis of Artificial Sweeteners and Preservatives in Soft DrinksYolita Satya Gitya UtamiNo ratings yet
- HPLC Analysis of Artificial Sweeteners and Preservatives in Soft DrinksDocument12 pagesHPLC Analysis of Artificial Sweeteners and Preservatives in Soft DrinksYolita Satya Gitya UtamiNo ratings yet
- HPLC Analysis of Artificial Sweeteners and Preservatives in Soft DrinksDocument12 pagesHPLC Analysis of Artificial Sweeteners and Preservatives in Soft DrinksYolita Satya Gitya UtamiNo ratings yet
- New Progestins ComparedDocument9 pagesNew Progestins ComparedYolita Satya Gitya UtamiNo ratings yet
- Ready 0918Document6 pagesReady 0918Yolita Satya Gitya UtamiNo ratings yet
- Quantitation of Curcuminoids in Curcuma RhizomeDocument6 pagesQuantitation of Curcuminoids in Curcuma RhizomeYolita Satya Gitya UtamiNo ratings yet
- HPLC Analysis of Artificial Sweeteners and Preservatives in Soft DrinksDocument12 pagesHPLC Analysis of Artificial Sweeteners and Preservatives in Soft DrinksYolita Satya Gitya UtamiNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5782)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Do Any Supplements Help For Varicose Veins or Chronic Venous Insufficiency?Document2 pagesDo Any Supplements Help For Varicose Veins or Chronic Venous Insufficiency?PeterNo ratings yet
- ECG and Echo Procedure Guidelines for Outpatients and InpatientsDocument18 pagesECG and Echo Procedure Guidelines for Outpatients and InpatientsElloide PajutanNo ratings yet
- Cardiac Arrest Upon Induction of General AnesthesiaDocument7 pagesCardiac Arrest Upon Induction of General AnesthesiaIlona HiariejNo ratings yet
- Pre Eclampsia of Severe FeaturesDocument3 pagesPre Eclampsia of Severe FeaturesPrincess Diane S. VillegasNo ratings yet
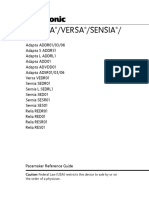
- Adapta Versa®sensiaDocument346 pagesAdapta Versa®sensiabobo samNo ratings yet
- Edexcel A-Level BIOLOGY Exchange and Transport Circulation 2 Question PaperDocument10 pagesEdexcel A-Level BIOLOGY Exchange and Transport Circulation 2 Question PaperAthenaNo ratings yet
- 6a1. Stroke - DR SubandiDocument67 pages6a1. Stroke - DR SubandiLiustar BrownNo ratings yet
- Jurnal Syah SemangkaDocument9 pagesJurnal Syah SemangkaDian PuspitaNo ratings yet
- Self-Learning Module For Grade 11: Earth and Life Science How Animals Survive How Will You Use This Module?Document8 pagesSelf-Learning Module For Grade 11: Earth and Life Science How Animals Survive How Will You Use This Module?MIMOYOUNo ratings yet
- ACUTE DECOMPENSATED HEART FAILUREDocument71 pagesACUTE DECOMPENSATED HEART FAILUREVivek Anandan100% (1)
- BARORECEPTORS AND CHEMORECEPTORS: REGULATION OF CARDIAC PRESSURESDocument4 pagesBARORECEPTORS AND CHEMORECEPTORS: REGULATION OF CARDIAC PRESSURESDrbee10No ratings yet
- JOURNALDocument4 pagesJOURNALChiara FajardoNo ratings yet
- Physioex Lab Report: Pre-Lab Quiz ResultsDocument3 pagesPhysioex Lab Report: Pre-Lab Quiz ResultsPavel MilenkovskiNo ratings yet
- Electrocardiography in Ischemic Heart Disease Clinical and Imaging Correlations and Prognostic ImplicationsDocument422 pagesElectrocardiography in Ischemic Heart Disease Clinical and Imaging Correlations and Prognostic ImplicationsAndonis AngelovNo ratings yet
- 5 EkgDocument6 pages5 EkgJessica BNo ratings yet
- Kalnirnay 2023 Marathi CalendarDocument24 pagesKalnirnay 2023 Marathi CalendarAparna Sachin Tembulkar50% (2)
- 05 N501 28766Document23 pages05 N501 28766Rumela Ganguly ChakrabortyNo ratings yet
- SBAR Patient CareDocument6 pagesSBAR Patient CareFreddie254No ratings yet
- Cardiac PathophysiologyDocument36 pagesCardiac Pathophysiologykim suhoNo ratings yet
- Jakarta Cardiovascular Care Unit Network System PDFDocument52 pagesJakarta Cardiovascular Care Unit Network System PDFekaNo ratings yet
- Jurnal Media Keperawatan: Politeknik Kesehatan Makassar Vol. 11 No. 01 2020 E-Issn: 2087-0035Document6 pagesJurnal Media Keperawatan: Politeknik Kesehatan Makassar Vol. 11 No. 01 2020 E-Issn: 2087-0035ちかお 千春No ratings yet
- Crossfit Gym Membership Contract and Receipt TemplateDocument6 pagesCrossfit Gym Membership Contract and Receipt Templatemohit jNo ratings yet
- Activity Intolerance (NCP)Document3 pagesActivity Intolerance (NCP)Sonia Letran Singson100% (3)
- Racial Disparities in Heart Disease Deaths and Risk FactorsDocument2 pagesRacial Disparities in Heart Disease Deaths and Risk FactorsJann ericka JaoNo ratings yet
- Couretask SampleDocument2 pagesCouretask Sampleej ragoNo ratings yet
- HOPE 11 Hand-OutsDocument3 pagesHOPE 11 Hand-OutsGrace AzucenasNo ratings yet
- Exercise Ecg: Stress Test Patient InformationDocument2 pagesExercise Ecg: Stress Test Patient InformationMauricioDinizNo ratings yet
- Valvular Heart Disease: Etiology PathophysiologyDocument34 pagesValvular Heart Disease: Etiology PathophysiologyensiNo ratings yet
- Edexcel Circulary System Past Paper Questions 1Document10 pagesEdexcel Circulary System Past Paper Questions 1binura desilvaNo ratings yet
- ACE Inhibitors - HFDocument1 pageACE Inhibitors - HFMartha TreviñoNo ratings yet









![Journal of Minimally Invasive Gynecology Volume 19 Issue 5 2012 [Doi 10.1016%2Fj.jmig.2012.05.009] Armstrong, Amy J.; Hurd, William W.; Elguero, Sonia; Barker, Nic -- Diagnosis and Management of Endometrial Hyperplasi](https://imgv2-1-f.scribdassets.com/img/document/227799411/149x198/4c372f3e21/1401772514?v=1)
![Annals of Allergy, Asthma & Immunology Volume 102 Issue 1 2009 [Doi 10.1016%2FS1081-1206%2810%2960101-9] Nelson, Harold S.; Carr, Warner; Nathan, Robert; Portnoy, Jay M. -- Update on the Safety of Long-Acting Β-Agonis](https://imgv2-1-f.scribdassets.com/img/document/248542176/149x198/5ef8798ba3/1417179985?v=1)