Professional Documents
Culture Documents
Ultrasound Guided Thoracentesis
Uploaded by
Orion John0 ratings0% found this document useful (0 votes)
142 views6 pagesPleural Effusion
Thoracentesis
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentPleural Effusion
Thoracentesis
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
142 views6 pagesUltrasound Guided Thoracentesis
Uploaded by
Orion JohnPleural Effusion
Thoracentesis
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 6
Ultrasound-Guided Thoracentesis*
David Feller-Kopman, MD, FCCP
Pleural effusions are an extremely common problem affecting approximately 1.5 million people
in the United States each year. Over the last several years, the use of portable ultrasound
machines has greatly enhanced the evaluation and management of patients with pleural disease.
This article will review the relevant literature supporting the use of ultrasound for the evaluation
of patients with pleural disease and address some practical practice management issues regarding
ultrasonography. (CHEST 2006; 129:17091714)
Key words: pleural effusion; practice management; ultrasound
Abbreviations: ACEP American College of Emergency Physicians; AMA American Medical Association;
CPT current procedural terminology
A
pproximately 1.5 million persons are found to
have pleural effusions each year in the United
States.
1
Over the last several years, the use of
portable ultrasound machines has greatly enhanced
the evaluation and management of patients with
pleural disease. Advantages of ultrasonography over
standard chest radiography and CT include the
absence of radiation, portability, real-time imaging,
and the ability to perform dynamic evaluations.
Ultrasonography has also been found to be more
sensitive than chest radiography for the detection of
pleural fluid,
2
and although slightly less sensitive
than CT scanning,
3
ultrasonography is easier to
perform and may better distinguish pleural thicken-
ing from pleural effusion. Although there is a learn-
ing curve associated with the use of ultrasound, it is
relatively short.
4
Ultrasonography is also an excellent
teaching tool, and we use it routinely to reinforce the
physical examination of residents and medical stu-
dents.
5
The American Medical Association supports
the use of ultrasonography by nonradiologists. It is
the responsibility of physicians in the other medical
specialties, such as pulmonary and critical care med-
icine, anesthesia, emergency medicine, and surgery,
to develop guidelines for training and incorporate
this technology into daily practice. This article will
review the relevant literature supporting the use of
ultrasound for the evaluation of patients with pleural
disease and address some practical practice manage-
ment issues regarding ultrasonography, primarily as
it pertains to nonradiologists.
Technical Aspects
Chest ultrasonography is primarily limited by re-
flection of ultrasound waves by bone and air. The
acoustic window, therefore, is limited to the inter-
costal space. Fortunately, the presence of pleural
fluid provides excellent contrast for pleural-based
lesions on both the parietal and visceral pleura and
can easily be seen between the hyperechoic air-filled
lung and the diaphragm/liver/spleen or kidney. Ex-
amination of the pleural space with ultrasonography
is best when using a convex array 3.5- to 5-MHz
probe.
6
This frequency range provides both excellent
resolution and penetration to allow visualization of
deep structures in the chest. All ultrasound probes
have a groove on one side that corresponds to a dot
on the screen, typically found in the upper-left
corner (Fig 1). By convention, the groove on the
transducer is directed cephalad. It is therefore nec-
essary to rotate the image on the screen 90 coun-
*From the Department of Interventional Pulmonology, Beth
Israel Deaconess Medical Center, Boston, MA.
The author has no conflict of interests.
Manuscript received January 13, 2006; revision accepted Febru-
ary 16, 2006.
Reproduction of this article is prohibited without written permission
from the American College of Chest Physicians (www.chestjournal.
org/misc/reprints.shtml).
Correspondence to: David Feller-Kopman, MD, FCCP, Interven-
tional Pulmonology, Beth Israel Deaconess Medical Center, One
Deaconess Rd, Suite 201, Boston, MA 02215; e-mail: dfellerk@
bidmc.harvard.edu
CHEST Topics in Practice Management
www.chestjournal.org CHEST / 129 / 6 / JUNE, 2006 1709
terclockwise in your minds eye in order to corre-
late the ultrasound image with the patients anatomy.
Practically, with the probe on the patients back, the
left side of the screen is cephalad, the right side of
the screen is caudad, the top of the screen is
posterior, and the bottom of the screen is anterior.
The probe should then be moved in both the
superior-inferior axis as well as transversely across
the chest, within the intercostal space.
The skin and subcutaneous tissues are seen as
multiple layers of soft-tissue echogenicity, and the
parietal and visceral pleura are seen as two hypere-
choic lines, typically 2 mm thick.
7
In the absence
of pleural fluid, identification of the hyperechoic
visceral and parietal pleurae can be difficult.
6,8
Air-
filled lung appears as patterns of bright echoes
caused by reverberation artifact. As air enters the
lung during inspiration, these echoes become
brighter, ie, more hyperechoic. Movement of the
underlying lung with respiration produces a sliding
or gliding sign, and this dynamic movement iden-
tifies the visceral pleura and lung parenchyma. Dia-
phragmatic movement can also be visualized in
real-time and is a key reference point when starting
to perform ultrasound examination of the pleural
space. The liver is used as an echo reference for the
definition of hypoechoic, isoechoic, and hyperechoic
reflections (Fig 1).
Ultrasonographic Features of Effusions
Several studies have found that ultrasonography
can be helpful in distinguishing transudative from
exudative pleural fluid. Although an early study
9
found that complex, or septated, fluid correctly
identified exudates 74% of the time, more recent
data
10
suggest that complex effusions (either sep-
tated or nonseptated) or homogenously echoic effu-
sions are always exudates. The converse, however,
may not be true. Although transudates are almost
always anechoic, anechoic fluid can be either tran-
sudative or exudative. Pleural thickening in associa-
tion with a parenchymal abnormality also correlates
with exudative fluid, and homogenously echogenic
effusions are typically seen with hemorrhage or
empyema.
10
Clearly, in order to correctly correlate
the ultrasonographic characteristics of effusions,
more experience is necessary than what is required
solely for identification of pleural fluid. The presence
of septations on ultrasound imaging has been found
to predict the need for pleural interventions such as
intrapleural fibrinolysis or surgical debridement, and
is also associated with an increased duration of chest
tube drainage and hospital stay.
11
These data, how-
ever, were reported prior to the recent trial by
Moskell and colleagues,
12
suggesting a lack of effi-
cacy of fibrinolytics for treating empyema. The exact
role of ultrasound for predicting further invasive
therapy remains to be defined.
The volume of fluid in the pleural space can be
estimated sonographically, and when examining pa-
tients in the supine position, the volume of fluid seen
on ultrasound correlates better with actual fluid
volume than the amount of fluid estimated from a
lateral decubitus chest radiograph.
13
Two important
points in using this method of evaluating pleural
fluid volume are that the transducer needs to be
perpendicular to the chest, as an oblique angle will
overestimate or underestimate volume. Additionally,
patients with larger chests will distribute a given
amount of fluid over a larger area, and therefore
reduce the estimated volume seen with ultrasound.
As pleural thickening can be anechoic, the sole
presence of an echo-free space does not guarantee
the presence of pleural fluid. Dynamic changes,
including the change of shape with respiratory move-
ment, or the presence of movable echo densities, are
therefore considered the sine quo non of pleural
fluid.
14
Some authors
15,16
advocate the use of the
fluid color signal, the change in color seen during
respiratory or cardiac motion, to identify small or
loculated effusions.
Ultrasound has also been evaluated in patients
with white out of a hemithorax. Using CT as the
gold standard, ultrasound has a 95% sensitivity for
detecting pleural lesions in this group of patients.
3
As
one would expect, the ability of ultrasound to detect
parenchymal or mediastinal pathology is more lim-
ited when compared to CT. The benefits of ultra-
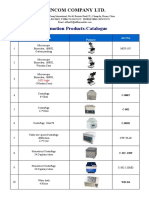
Figure 1. Overview of the right pleural space. The diaphragm
can be seen on the right side of the image. The liver is used as a
reference point to describe the echogenicity of the other struc-
tures. The hyperechoic air-filled lung can be seen floating in
hypoechoic pleural fluid. (2006 from Ultrasound Guided Pro-
cedures and Investigations, Armin Ernst, David Feller-Kopman,
eds., Taylor and Francis, New York, NY 2006, Reproduced by
permission of Routlege/Taylor & Francis Group, LLC).
1710 Topics in Practice Management
sound, however, include its portability, cost, lack of
radiation exposure, and ability to perform dynamic
and real-time procedural guidance at the bedside.
Ultrasound has also been shown to aid in obtaining
adequate fluid from small effusions (defined as
obliteration of less than half of the hemidiaphragm),
regardless of whether the fluid was loculated or
not.
17
Guidance for Thoracentesis
Thoracentesis is typically thought to be a relatively
safe procedure with few complications. The inci-
dence of pneumothorax, however, has been reported
to be as high as 20 to 39%.
18
Procedural factors that
have been shown to reduce the rate of pneumotho-
rax include the performance by experienced person-
nel,
19
as well as the use of ultrasound.
18,20,21
Although there are no blinded randomized trials
comparing ultrasound-guided vs physical examina-
tion-guided thoracentesis, several studies have asso-
ciated ultrasound use with lower complications. Gro-
gan and colleagues
18
found a significant reduction in
the pneumothorax rate when ultrasound was utilized
for identification of needle placement (0% vs approx-
imately 29%). A similar reduction in the rate of
pneumothorax was also seen by Raptopoulos et al
21
(18% vs 3%). This held true whether the amount of
pleural fluid was deemed small or large, whether the
thoracenteses were diagnostic or therapeutic, and
whether the tap was dry or near dry. Perhaps
even more clinically relevant, the occurrence of
pneumothorax requiring tube thoracostomy is also
significantly reduced with ultrasound guidance.
21,22
Most studies of ultrasound guided thoracentesis
do not use real-time guidance for needle insertion,
but insert the needle immediately after identification
of an appropriate site. Interestingly, this X marks
the spot technique, when performed with delay in
needle insertion, ie, having a radiologist use ultra-
sound to mark the needle insertion site with the
thoracentesis being performed when the patient
returned to the floor, is not associated with a reduc-
tion in the pneumothorax rate.
21
Another benefit of ultrasound has been an in-
creased success in thoracentesis even after a failed
clinically directed thoracentesis. Several studies
9,17,23
suggest that fluid can be successfully obtained in up
to 88% of patients after unsuccessful clinically
guided thoracentesis. Perhaps even more impor-
tantly, in 58% of clinically attempted dry taps, the
needle insertion site was found to be below the
diaphragm.
23
Diacon et al
24
found that ultrasound
increased the rate of accurate site selection by 26%,
and decreased the number of near misses, ie, the
number of potentially dangerous needle insertion
sites by 10% when compared to fluid localization by
physical examination and chest radiography.
Critical care physicians can easily acquire the sonog-
raphy skills required to guide thoracentesis in the ICU,
and can do so without formal radiology training.
4
Mayo
and colleagues
4
had a 1.3% pneumothorax rate in their
study of 232 ultrasound-guided thoracenteses in pa-
tients requiring mechanical ventilation. For patients in
the ICU, it is uncommon for us to sit the patient
upright, a task that often requires at least two assistants.
We generally scan the lateral chest wall with the patient
supine and the ipsilateral arm brought over the chest to
the opposite side. This position is easiest for the patient
and the nurse, and moderate effusions can easily be
seen. With smaller effusions, the head of the bed may
need to be raised, or we slide the patient closer to the
edge of the bed so the ultrasound probe can be placed
more posteriorly.
Pneumothorax
Although easily seen by conventional chest radiog-
raphy or chest CT, the portability of ultrasound,
especially when used at the point of care, makes this
technology especially useful for ruling out a postpro-
cedural pneumothorax. Loss of lung sliding as well as
the loss of comet tail artifacts strongly associate
with the presence of pleural air.
25
Comet tail artifacts
are caused by echo reverberations of the air-filled
lung, and appear as narrow hyperechoic ray-like
opacities extending from the pleural line to the edge
of the ultrasound screen. Lung sliding can also be
limited by pleural-parenchymal adhesions or dia-
phragmatic paralysis, and therefore the main utility
of ultrasound for assessment of pneumothorax re-
lates to its ability to rule out a pneumothorax. That is,
the presence of comet tail artifacts and lung sliding
rules out a pneumothorax with a negative predictive
value of 100%.
26,27
Although ultrasound can rule out
a pneumothorax, it cannot quantitate its size when
present, and standard radiographs are required.
Lichtenstein et al
28
has recently reviewed the utility
of ultrasound for the identification of pneumothorax,
and describes the visualization of the lung point
with the time-motion mode as a very specific sign
(100%) to identify pneumothorax. Also important to
the pulmonologist is a recent small study
29
using
ultrasound to rule out pneumothorax after trans-
bronchial biopsy.
Practice Management Implications
The policy of the American Medical Association
(AMA) on privileging for ultrasound imaging states
the following:
www.chestjournal.org CHEST / 129 / 6 / JUNE, 2006 1711
ultrasound imaging is within the scope of practice of
appropriately trained physicians. . . broad and diverse use
and application of ultrasound imaging technologies exist in
medical practice. . . privileging of the physician to perform
ultrasound imaging procedures in a hospital setting should
be a function of hospital medical staffs and should be
specifically delineated on the Departments Delineation of
Privileges form. . . each hospital medical staff should
review and approve criteria for granting ultrasound privi-
leges based on background and training for the use of
ultrasound technology and strongly recommends that
these criteria are in accordance with recommended train-
ing and education standards developed by each physicians
respective specialty.
30
This policy affirms that ultrasound is not limited to
the domain of radiologists, and the AMA also sup-
ports reimbursement for appropriately trained phy-
sicians.
The American College of Emergency Physicians
(ACEP), for example, has taken action and devel-
oped a policy statement
31
addressing the scope of
practice, training, and proficiency recommendations,
quality improvement, and documentation issues re-
garding the use of ultrasonography in the emergency
setting. Likewise, the American College of Surgeons
has also approved a statement
32
describing the use of
ultrasound by surgeons. Both of these documents
strongly support the use of ultrasound by members
of their societies and address ways to obtain and
maintain competency, as well as ensuring quality
control. Unfortunately, the American College of
Chest Physicians, the American Thoracic Society,
and the Society of Critical Care Medicine have yet to
develop or publish their recommendations. As the
use of ultrasonography is expanding among pulmo-
nologists and intensivists,
33,34
we need to develop a
policy that addresses similar issues, as well as how to
train our fellows in a procedure that they will
certainly need to be as facile with as the flexible
bronchoscope.
To gain the skills required to incorporate ultra-
sonography in clinical practice, the nonradiologist
needs to become proficient in both cognitive and
psychomotor skill sets. Training in image acquisition
and interpretation needs to include didactic lectures,
demonstrations, and most importantly, proctoring by
a skill sonographer. The ACEP suggests a 2-day
(16-h) course to cover all aspects of ultrasonography
geared toward the emergency department physician,
but also acknowledges that less training is necessary
for those wishing to learn only one application.
31
For
a single application, the ACEP recommends 3 to 4 h
of didactics and 2 to 4 h of laboratory training.
Although it is difficult to determine competence
solely based on the number of examinations per-
formed, the ACEP suggests at least 25 cases be
documented and reviewed for each primary applica-
tion. The cases should include both normal and
abnormal findings, and continued training in order
to ensure skill maintenance is a must.
31
There are
several continuing medical education courses given
throughout the country, and attendance at the
American College of Chest Physicians and Society
for Critical Care Medicine sessions on ultrasound
use have been increasing almost logarithmically.
Additionally, self-study courses are also available
specifically geared toward pleural ultrasound (www.
sonographytraining.com). Continued quality assur-
ance for both the sonographer and the equipment is
also essential. As the AMA suggests, it will the
responsibility of our societies to develop specific
guidelines addressing training and education stan-
dards.
The chest physician should review the current
procedural terminology (CPT) codes with their local
billing expert as well as their local third-party payers,
as reimbursements vary between regions, and even
within a state. The two most commonly used codes
for thoracentesis are 32000 and 32002. Code 32000
describes thoracentesis, puncture of pleural cavity
for aspiration, initial or subsequent and has an
associated Medicare payment of approximately
$190.69 (nonfacility) and $82.00 (facility) in Massa-
chusetts (www.catalog.ama-assn.org/Catalog/cpt/cpt_
search.jsp?_requestid244532). Code 32002, how-
ever, is described as thoracentesis with insertion of
tube with or without water seal (eg, for pneumotho-
rax) (separate procedure) and has an associated
Medicare payment of approximately $223.87 (nonfa-
cility) and $132.94 (facility) in Massachusetts. This is
a distinct code from 32020, tube thoracostomy with
or without water seal (eg, for abscess, hemothorax,
empyema) (separate procedure), which has a Medi-
care reimbursement of $222.00 (nonfacility and fa-
cility) in Massachusetts. These codes distinguish
diagnostic thoracenteses, when just a small needle
is used, from therapeutic thoracenteses, in which a
kit containing a catheter over a needle is used, from
frank tube thoracostomy. The physician therefore
should appropriately document when a therapeutic
thoracentesis is performed, and should bill 32002 if a
kit containing a catheter is used for the procedure.
The most commonly used CPT codes for ultra-
sound guidance relevant to the chest physician/
intensivist include 76942 (ultrasonic guidance for
needle placement, [eg, biopsy, aspiration, injection,
localization device], imaging supervision and inter-
pretation); 76937 (ultrasound guidance for vascular
access requiring ultrasound evaluation of potential
access sites, documentation of selected vessel pa-
tency, concurrent real-time ultrasound visualization
of vascular needle entry, with permanent recording
and reporting [list separately in addition to code for
1712 Topics in Practice Management
primary procedure]); and 76604 (ultrasound, chest,
B-scan [includes mediastinum] and/or real time with
image documentation) [www.catalog.ama-assn.org/
Catalog/cpt/cpt_search.jsp?_requestid244532]. It
should be noted, however, that the above codes are
the technical component and can only be billed by
the service that owns the ultrasound equipment. The
professional component is billed by using the -26
modifier. Since the technical component is signifi-
cantly higher than the professional component, it
may make financial sense for the physicians office or
division to purchase the ultrasound unit themselves,
as opposed to using one owned by the hospital. In
metropolitan Boston, the reimbursement for code
76942 is $175.00 ($138.56 technical, $36.44 profes-
sional component), and the reimbursement for
code 76937 is $38.13 ($21.25 technical, $16.88
professional component) [www.cms.hhs.gov/apps/
pfslookup/].
As with all billing practices, it is the physicians
responsibility to ensure proper billing and documen-
tation, and the reader is urged to review local
requirements with their insurance companies and
billing experts. It is also crucial to discuss reimburse-
ment with third-party payers, as they may wish to
have a letter from the chief of radiology at your
institution stating you have achieved competency.
This is yet another reason why our societies need to
take an active role in advocating for our own ability
to determine competency.
In addition to using the proper CPT codes, ade-
quate documentation is a must. For ultrasound,
either a hard copy or electronic copy of the pertinent
images need to be saved in the medical record. This
needs to be done in accordance with the Health
Insurance Portability and Accountability Act guide-
lines, and all patient identifiers need to be safe-
guarded if the images are to be stored electronically.
Limitations to Ultrasonography
There are some realities one needs to face, how-
ever, prior to embracing ultrasound for all thoracen-
teses. First, there are no blinded randomized trials
proving improved outcome. As these trials would be
extremely difficult, if not impossible, to design, we
will likely need to rely on the current grade B
evidence. Clearly, experienced pulmonologists can
perform thoracentesis safely without ultrasound
guidance.
35
At this time, each of the relevant risks
and benefits of performing thoracentesis with or
without ultrasound guidance need to be assessed on
a case-by-case basis. The obvious benefits of the
pulmonologist performing the thoracentesis, as op-
posed to having the procedure performed by a
radiologist, in an off-site location include patient
continuity, the guarantee that the appropriate pro-
cedure is performed (diagnostic vs therapeutic tap),
and the fact that the pulmonologist has been trained
in the interpretation of pleural fluid results and can
provide pleural-specific follow-up. There are, how-
ever, cases in which the pulmonologist who does not
perform ultrasound would clearly want his/her radi-
ology colleagues to perform the procedure. Addi-
tionally, some small/loculated effusions would be
better drained by CT as opposed to ultrasound
guidance. Secondly, there are numerous ultrasound
machines available, each with their own advantages
and disadvantages, and although bells and whistles
may be nice to have, they are not required, and
simple/older machines can be adequate for most
needs. The initial financial investment can be quite
significant (approximately $25,000 to $40,000), al-
though new and used equipment can even be found
on Internet sites such as e-Bay for significantly less
money. Additionally, maintenance costs and costs of
additional supplies such as sterile sheaths and a
printer need to be budgeted. Thirdly, and perhaps
most importantly, quality assurance needs to be high
on all of our priorities. Although easily learned, both
didactic and real-time education is required. As with
other procedures, competence is likely partly num-
bers based; in order to maintain proficiency, a
certain number of examinations should be per-
formed on a regular basis.
Summary
Ultrasonography is an easily learned procedure
that not only enhances the physical examination but
has the distinct advantages of being a portable tool
that can provide real-time evaluation of the pleural
space. Its use has been associated with an improved
yield and reduced complication rate for thoracente-
sis, and is quickly becoming the standard of care for
procedural guidance. As chest physicians/intensiv-
ists, we need to embrace ultrasounds broad clinical
applications in patients with pleural disease, as well
as guidance for vascular access, and even cardiac
echo and trauma evaluation. It is crucial that chest
physicians take the lead in advocating for ultrasound
to become part of our daily practice, create educa-
tional opportunities for members of our societies,
and incorporate ultrasound training in our fellowship
programs.
References
1 Light RW. Pleural diseases, 4th ed. Philadelphia, PA: Lippin-
cott, Williams & Wilkins, 2001
www.chestjournal.org CHEST / 129 / 6 / JUNE, 2006 1713
2 Gryminski J, Krakowka P, Lypacewicz G. The diagnosis of
pleural effusion by ultrasonic and radiologic techniques.
Chest 1976; 70:3337
3 Yu CJ, Yang PC, Wu HD, et al. Ultrasound study in unilateral
hemithorax opacification. Image comparison with computed
tomography. Am Rev Respir Dis 1993; 147:430434
4 Mayo PH, Goltz HR, Tafreshi M, et al. Safety of ultrasound-
guided thoracentesis in patients receiving mechanical venti-
lation. Chest 2004; 125:10591062
5 Rozycki GS, Pennington SD, Feliciano DV. Surgeon-per-
formed ultrasound in the critical care setting: its use as an
extension of the physical examination to detect pleural effu-
sion. J Trauma 2001; 50:636642
6 Beckh S, Bolcskei PL, Lessnau KD. Real-time chest ultra-
sonography: a comprehensive review for the pulmonologist.
Chest 2002; 122:17591773
7 Mathis G. Thoraxsonography: part I. Chest wall and pleura.
Ultrasound Med Biol 1997; 23:11311139
8 Tsai TH, Yang PC. Ultrasound in the diagnosis and manage-
ment of pleural disease. Curr Opin Pulm Med 2003; 9:282
290
9 Hirsch JH, Rogers JV, Mack LA. Real-time sonography of
pleural opacities. AJR Am J Roentgenol 1981; 136:297301
10 Yang PC, Luh KT, Chang DB et al. Value of sonography in
determining the nature of pleural effusion: analysis of 320
cases. AJR Am J Roentgenol 1992; 159:2933
11 Chen KY, Liaw YS, Wang HC et al. Sonographic septation: a
useful prognostic indicator of acute thoracic empyema. J
Ultrasound Med 2000; 19:837843
12 Maskell NA, Davies CW, Nunn AJ et al. U.K. controlled trial
of intrapleural streptokinase for pleural infection. N Engl
J Med 2005; 352:865874
13 Eibenberger KL, Dock WI, Ammann ME, et al. Quantifica-
tion of pleural effusions: sonography versus radiography.
Radiology 1994; 191:681684
14 Marks WM, Filly RA, Callen PW. Real-time evaluation of
pleural lesions: new observations regarding the probability of
obtaining free fluid. Radiology 1982; 142:163164
15 Wu RG, Yang PC, Kuo SH, et al. Fluid color sign: a useful
indicator for discrimination between pleural thickening and
pleural effusion. J Ultrasound Med 1995; 14:767769
16 Wu RG, Yuan A, Liaw YS, et al. Image comparison of
real-time gray-scale ultrasound and color Doppler ultrasound
for use in diagnosis of minimal pleural effusion. Am J Respir
Crit Care Med 1994; 150:510514
17 Kohan JM, Poe RH, Israel RH, et al. Value of chest ultra-
sonography versus decubitus roentgenography for thoracen-
tesis. Am Rev Respir Dis 1986; 133:11241126
18 Grogan DR, Irwin RS, Channick R, et al. Complications
associated with thoracentesis: a prospective, randomized
study comparing three different methods. Arch Intern Med
1990; 150:873877
19 Bartter T, Mayo PD, Pratter MR, et al. Lower risk and higher
yield for thoracentesis when performed by experienced op-
erators. Chest 1993; 103:18731876
20 Jones PW, Moyers JP, Rogers JT, et al. Ultrasound-guided
thoracentesis: is it a safer method? Chest 2003; 123:418423
21 Raptopoulos V, Davis LM, Lee G, et al. Factors affecting the
development of pneumothorax associated with thoracentesis.
AJR Am J Roentgenol 1991; 156:917920
22 Barnes TW, Morgenthaler TI, Olson EJ, et al. Sonographi-
cally guided thoracentesis and rate of pneumothorax. J Clin
Ultrasound 2005; 33:442446
23 Weingardt JP, Guico RR, Nemcek AA Jr, et al. Ultrasound
findings following failed, clinically directed thoracenteses.
J Clin Ultrasound 1994; 22:419426
24 Diacon AH, Brutsche MH, Soler M. Accuracy of pleural
puncture sites: a prospective comparison of clinical examina-
tion with ultrasound. Chest 2003; 123:436441
25 Targhetta R, Bourgeois JM, Chavagneux R, et al. Ultrasonic
signs of pneumothorax: preliminary work. J Clin Ultrasound
1993; 21:245250
26 Lichtenstein D, Meziere G, Biderman P, et al. The comet-tail
artifact: an ultrasound sign ruling out pneumothorax. Inten-
sive Care Med 1999; 25:383388
27 Maury E, Guglielminotti J, Alzieu M, et al. Ultrasonic
examination: an alternative to chest radiography after central
venous catheter insertion? Am J Respir Crit Care Med 2001;
164:403405
28 Lichtenstein DA, Meziere G, Lascols N, et al. Ultrasound
diagnosis of occult pneumothorax. Crit Care Med 2005;
33:12311238
29 Reissig A, Kroegel C. Accuracy of transthoracic sonography in
excluding post-interventional pneumothorax and hydropneu-
mothorax: comparison to chest radiography. Eur J Radiol
2005; 53:463470
30 American Medical Association. Res. 802 I, Reaffirmed:
Sub.Res. 108 A. Privileging for ultrasound imaging. Available at:
http://www.ama-assn.org/apps/pf_newpf_online?f_nbrowse/
docpolicyfiles/HnE/H-230.960.HTM. Accessed February
15, 2006
31 American College of Emergency Physicians. AECP policy
statement: emergency ultrasound guidelines. 2001. Available
at: www.acep.org/NR/rdonlyres/8024079E-28E8-4875-93E6-
6867EA705A2A/0/ultrasound_guidelines.pdf. Accessed Feb-
ruary 15, 2006
32 American College of Surgeons. Ultrasound examinations
by surgeons. 1998. Available at: www.facs.org/fellows_info/
statements/st-31.html. Accessed February 16, 2006
33 Beaulieu Y, Marik PE. Bedside ultrasonography in the ICU:
part 1. Chest 2005; 128:881895
34 Beaulieu Y, Marik PE. Bedside ultrasonography in the ICU:
part 2. Chest 2005; 128:17661781
35 Aelony Y. Thoracentesis without ultrasonic guidance: infre-
quent complications when performed by an experienced
pulmonologist. J Bronchology 2005; 14:200202
1714 Topics in Practice Management
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Post-Polio Syndrome - Management of PCPDocument65 pagesPost-Polio Syndrome - Management of PCPOrion JohnNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- VACEP Sepsis UpdateDocument62 pagesVACEP Sepsis UpdateOrion JohnNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- 2017 ATS 6mwtDocument32 pages2017 ATS 6mwtOrion JohnNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Elsevier grants free access to COVID-19 researchDocument12 pagesElsevier grants free access to COVID-19 researchOrion JohnNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Pegasus - Timi 54 PDFDocument21 pagesPegasus - Timi 54 PDFOrion JohnNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- VACEP Sepsis UpdateDocument62 pagesVACEP Sepsis UpdateOrion JohnNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- 2016 Guideline For Atrial FibrillationDocument16 pages2016 Guideline For Atrial FibrillationOrion JohnNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Carvedilol in Heart FailureDocument5 pagesCarvedilol in Heart FailureOrion JohnNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Management of CTD in ILDDocument16 pagesManagement of CTD in ILDOrion JohnNo ratings yet
- Pegasus - Timi 54 PDFDocument21 pagesPegasus - Timi 54 PDFOrion JohnNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Wikstrand Et Al-2014-Journal of Internal Medicine PDFDocument10 pagesWikstrand Et Al-2014-Journal of Internal Medicine PDFOrion JohnNo ratings yet
- Pulmonary FibrosisDocument43 pagesPulmonary FibrosisOrion JohnNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Comparable B-Blocker in Heart FailureDocument6 pagesComparable B-Blocker in Heart FailureOrion JohnNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Wikstrand Et Al-2014-Journal of Internal MedicineDocument10 pagesWikstrand Et Al-2014-Journal of Internal MedicineOrion JohnNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- An Introduction To Insulin TherapyDocument23 pagesAn Introduction To Insulin TherapyOrion JohnNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- An Introduction To Insulin TherapyDocument23 pagesAn Introduction To Insulin TherapyOrion JohnNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- 2016 Sepsis Septic ShockDocument39 pages2016 Sepsis Septic ShockOrion JohnNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- Fluids in SepsisDocument27 pagesFluids in SepsisOrion JohnNo ratings yet
- 2014 Sepsis & DrugsDocument24 pages2014 Sepsis & DrugsOrion JohnNo ratings yet
- 2015 SepsisDocument41 pages2015 SepsisOrion JohnNo ratings yet
- Noninvasive Ventilation Indications and MonitoringDocument32 pagesNoninvasive Ventilation Indications and MonitoringOrion JohnNo ratings yet
- Pulmonary FibrosisDocument43 pagesPulmonary FibrosisOrion JohnNo ratings yet
- Management of Septic ShockDocument31 pagesManagement of Septic ShockDawn MarcoNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Vasopressors in ShockDocument8 pagesVasopressors in ShockOrion JohnNo ratings yet
- Continuous Hemodynamic MonitoringDocument54 pagesContinuous Hemodynamic MonitoringOrion JohnNo ratings yet
- Continuous Hemodynamic MonitoringDocument54 pagesContinuous Hemodynamic MonitoringOrion JohnNo ratings yet
- Pulmonary Function TestsDocument29 pagesPulmonary Function TestsOrion JohnNo ratings yet
- Screening Lung CancerDocument17 pagesScreening Lung CancerOrion JohnNo ratings yet
- Pulmonary Hypertension Drug TherapyDocument337 pagesPulmonary Hypertension Drug TherapyOrion JohnNo ratings yet
- Sickle Cell DiseaseDocument14 pagesSickle Cell DiseaseOrion JohnNo ratings yet
- Surgery For Endocrinological Diseases and Malformations in ChildhoodDocument155 pagesSurgery For Endocrinological Diseases and Malformations in ChildhoodBeng DinNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- IntroductionDocument10 pagesIntroductionFebri WantoNo ratings yet
- Brianna Carden Resume For Portfolio PDFDocument2 pagesBrianna Carden Resume For Portfolio PDFapi-209274086No ratings yet
- ONCOLOGY Board Exam QuestionDocument11 pagesONCOLOGY Board Exam Questiondimplejane100% (2)
- Wincom Company Catalogue Features Microscopes, Centrifuges and More Medical EquipmentDocument9 pagesWincom Company Catalogue Features Microscopes, Centrifuges and More Medical EquipmentJuan Carlos CrespoNo ratings yet
- Low Intensity Pulsed Ultrasound 2012Document12 pagesLow Intensity Pulsed Ultrasound 2012Joseph SmithNo ratings yet
- Real-Time Tissue Elastography SectionDocument42 pagesReal-Time Tissue Elastography SectionAndrei DumitruNo ratings yet
- Draper & Dash BI Apps For HealthcareDocument22 pagesDraper & Dash BI Apps For HealthcareAnalytics8No ratings yet
- SonoBook 8-9 User Manual V1.0-20170429Document236 pagesSonoBook 8-9 User Manual V1.0-20170429Luis Macías Borges100% (1)
- Ectopic Pregnancy Diagnosis and TreatmentDocument39 pagesEctopic Pregnancy Diagnosis and TreatmentFecky Fihayatul IchsanNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Color Doppler Ultrasound System: Datasheet Release 1.0Document17 pagesColor Doppler Ultrasound System: Datasheet Release 1.0Hea CHNo ratings yet
- Revision History and SpecificationsDocument304 pagesRevision History and SpecificationsSyarif AlfathNo ratings yet
- Ultrasonographic Examination of The Small Intestine, Large IntestineDocument6 pagesUltrasonographic Examination of The Small Intestine, Large IntestineYans PangerunganNo ratings yet
- Submission of RadiologyDocument48 pagesSubmission of RadiologyKartika Singh NarukaNo ratings yet
- Brochure Acuson P500Document12 pagesBrochure Acuson P500Pedro Alexander Romero RodriguezNo ratings yet
- Academy of Life Underwriting - ALU 101 - Basic Life Insurance Underwriting - Textbook For 2022 Exam Cycle (2021)Document359 pagesAcademy of Life Underwriting - ALU 101 - Basic Life Insurance Underwriting - Textbook For 2022 Exam Cycle (2021)KALPESH SHAHNo ratings yet
- Philips Iu22 BrochureDocument16 pagesPhilips Iu22 BrochurecontactoNo ratings yet
- Full Sonography Principles and Instruments 9Th Edition Kremkau Test Bank PDF Docx Full Chapter ChapterDocument33 pagesFull Sonography Principles and Instruments 9Th Edition Kremkau Test Bank PDF Docx Full Chapter Chaptermolecast.bassawkzaa100% (9)
- 5-FUJIFILM-Endoscopy-GuidebookDocument33 pages5-FUJIFILM-Endoscopy-Guidebooklied cnNo ratings yet
- Physics NotesDocument43 pagesPhysics NotesRaj ManovaNo ratings yet
- Operators Manual: E-Z Scan 5500+ SeriesDocument44 pagesOperators Manual: E-Z Scan 5500+ SeriesSadegh ShebaniNo ratings yet
- Instant Download Ebook PDF Essential Ultrasound Anatomy First Edition PDF ScribdDocument47 pagesInstant Download Ebook PDF Essential Ultrasound Anatomy First Edition PDF Scribdandrew.harrell532100% (40)
- CancerDocument228 pagesCancerCrystal Grace100% (1)
- Image Analysis For Biological Sciences - C. A. Glasbey, G. W. HorganDocument211 pagesImage Analysis For Biological Sciences - C. A. Glasbey, G. W. HorganUlises MarmolejoNo ratings yet
- Characterisig Triphasic, Biphasic and MonophasicDocument9 pagesCharacterisig Triphasic, Biphasic and Monophasicraviks34No ratings yet
- Current Concepts in Orthopedic Management of Multiple TraumaDocument8 pagesCurrent Concepts in Orthopedic Management of Multiple TraumanellieauthorNo ratings yet
- Logiq P5: Product DescriptionDocument14 pagesLogiq P5: Product DescriptionrsketchNo ratings yet
- Upper Extremity Venous Doppler Ultrasound PDFDocument12 pagesUpper Extremity Venous Doppler Ultrasound PDFLayla Salomão0% (1)
- AF201 Managerial Accounting Group Assignment Analysis (39Document4 pagesAF201 Managerial Accounting Group Assignment Analysis (39Navinesh Nand100% (1)
- Basic Principles and Safety of Diagnostic Ultrasound in Obstetrics and Gynecology - UpToDateDocument9 pagesBasic Principles and Safety of Diagnostic Ultrasound in Obstetrics and Gynecology - UpToDatemasterchipNo ratings yet
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (402)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (327)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (13)
- The Ultimate Guide To Memory Improvement TechniquesFrom EverandThe Ultimate Guide To Memory Improvement TechniquesRating: 5 out of 5 stars5/5 (34)
- Techniques Exercises And Tricks For Memory ImprovementFrom EverandTechniques Exercises And Tricks For Memory ImprovementRating: 4.5 out of 5 stars4.5/5 (40)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet