Professional Documents
Culture Documents
Pediatric Clinical H&P
Uploaded by
Jay VeeCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pediatric Clinical H&P
Uploaded by
Jay VeeCopyright:
Available Formats
THE PEDIATRIC HISTORY
I. General Principles:
Smile and greet parents, child if old enough.
Introduce yourself.
Establish rapport and try to make family feel comfortable.
II. Date of interview, source and reliability.
III. General Data: Name, age, sex, residence, number of times admitted and date of
present admission.
IV. Chief Complaint: Brief statement of the primary problem that caused the family to
seek medical attention, preferably using patients or informants own words.
V. History of the Present Illness: Concise chronological account of the illness, from
the onset to the latest including any previous treatment with full description of
symptoms, pertinent positives and pertinent negatives. It belongs here if related to
the differential diagnosis for the chief complaint.
Tip for describing symptoms if applicable: CLITAA
C Character
L Location
I Intensity
T Timing
A Associated signs and symptoms
A Aggravating and relieving factors
If neonate, start HPI from birth.
VI. Medical History: General state of health as the parents or patient perceives it.
A. Birth History: Particularly important during the first 2 years of life and when
dealing with neurologic and developmental problems
1. Neonates and Infants
Prenatal history: mother's age, gravida, parity, abortions, health during
pregnancy (bleeding, trauma, hypertension, gestational diabetes,fever,
infections, medications, radiation exposure, drugs, alcohol, smoking, rubella
immunity status, hepatitis B, rupture of membranes), nutritional patterna and
specific illnesses
Natal history (Labor and Delivery): gestational age at delivery, spontaneous
or induced, duration of labor, duration of rupture of membranes prior to
delivery, complications, medications or anesthesia, vertex or breech
presentation, vaginal or cesarean section, meconium staining of amniotic
fluid, birth order, if a multiple birth and birth weight
2. All Children
Neonatal history: Apgar score, breathing problems, use of oxygen, need for
intensive care, problems in nursery ( e.g. meconium stained, birth injuries,
jaundice, feeding difficulty, respiratory distress), length of stay in nursery,
estimated gestational age by ballard score, if AGA, SGA or LGA
B. Nutrition/Dietary History
1. Infancy: breast or formula, frequency, amount, problems, when was the
introduction of solids and problems, any change in formula and why, peculiar
eating habits (pica), vitamin/mineral supplements
2. Childhood: good appetite or "picky eater", special diets, milk intake, "junk
foods", concerns about weight, vitamin/mineral supplements
C. Growth and Developmental History
1. Physical growth: actual or approximate weight and height at 1, 2, 5 and 10
years, history of slow or rapid gains or losses, tooth eruption and loss pattern
2. Developmental milestones:
Gross Motor:
Fine Motor:
Language:
Personal-Social: eating, dressing, grooming, household chores, toileting,
sleep patterns, habits, discipline and temperament, play and relationship
with others, personality
3. School Performance (Preschool and School Children)
a. Language skills
b. Reading skills
c. Writing skills
d. Sequential concepts and math skills
e. Problem solving, reasoning and moral development
4. Pubertal History (Adolescents)
a. Male
Age of onset
Genital Enlargement
Pubic Hair
b. Female
Age of onset
Breast
Pubic Hair
Age of Menarche, Frequency, Duration, LMP, Dysmenorrhea, Meds
D. Past Illnesses
1. Childhood illnesses, age, complications, treatment
2. Recent infection exposures, date, travel to other locations, animal exposure
3. Previous hospitalizations, age, length of stay, reason, location
4. Previous surgery/ transfusions age, reason for procedure, complication
5. Trauma/ injuries/ ingestions, age, circumstances surrounding event,
treatment, complication
6. Screening procedures
7. Allergies and drug reactions
8. Previous and current medications and disabilities
E. Immunization History: Don't rely on memory; ask to see record. Check if up to
date.
BCG
DPT
OPV
Hepatitis B
HIB
PCV
Rotavirus
Measles
Varicella
MMR
Typhoid
Hepatitis A
Meningoccocal
Flu
Booster doses
Others: Rabies,
HPV, Pneumo 23
VII. Family History
A. Illnesses: cardiac disease, hypertension, stroke, diabetes, cancer, abnormal
bleeding, asthma, epilepsy, kidney disease
B. Others: mental retardation, developmental delay, congenital anomalies,
chromosomal problems, miscarriages, infant or childhood deaths, growth
problems, consanguinity, ethnic background
VIII. Psychosocial History: An outline or narrative description that captures important
and relevant information about patient as person, patients lifestyle, home situation
and significant others
A. Infants and Older Children
1. Living situation and conditions - daycare, safety issues including water source
2. Composition of family
3. Occupation of parents
4. Religious and health beliefs of family
B. Adolescents (HEADSSS)
1. Home: What is the living arrangement? Any recent changes in the living
arrangement? Relationships in the home? Any issues that causes
arguments? Economic issues? Stresses in the home? Forms of discipline?
Anything the adolescent wishes to change in the family?
2. Education/Employment: Is patient currently in or out of school or employed?
Where? Favorite subject? Average last grading/semester? Any problems with
classmates or teachers? Ever been truant/suspended/expelled from school?
What are the patients future education/employment goals?
3. Activities: What does the patient do in spare time? Hobbies and interests?
How much time does he spend watching TV, playing computer games and
using the internet? With whom does the patient spend time with? Any close
friends? Are the patients friends attending school?
4. Drugs/Other Substance of Abuse: Does the adolescent or any of his friends
use tobacco, alcohol, drugs? If yes, details (what, frequency, amount) and
how/why started? Effects on daily activities? Selling drugs?
5. Sexuality/Sexual Activity: Sexual orientation? Sexual development?
Dating? Details such as is patient having sex or have had sex? With whom,
how often or when was the last time? Any use of contraception? Having
symptoms of STD? Any history of physical or sexual abuse?
6. Suicide/Depression: Is the adolescent ever sad? Unmotivated? Hopeless?
Lonely? Why? What does he do when the feeling comes? Who does he talk
to? Has the adolescent ever thought of hurting others or himself?Has suicide
plan? If yes, assess seriousness and whether needs immediate referral.
7. Safety: Does the adolescent use seat belts/helmets? Is he a member of a
fraternity or gang? Does he carry a weapon for protection? Is there a firearm
in the adolescents home?
IX. Review of Systems
A. General: fever, recent changes in weight, also include patient's activity level,
playfulness, appetite, sleep habits, days of school missed
B. Skin and Lymph: rashes, adenopathy, lumps, easy bruising, bleeding,
pigmentation changes, eczema
C. HEENT: headache, dizziness/fainting, seizures, strabismus, conjunctivitis, visual
problems, hearing, ear infections, draining ears, neck mass, stuffy or runny nose,
allergic rhinitis, sore throat, mouth breathing, snoring, apnea, epistaxis, teeth or
gum problem
D. Cardiovascular: cyanosis, heart murmurs, exercise tolerance, squatting, chest
pain, palpitations
E. Respiratory: wheezing, chronic cough,dyspnea, asthma, hemoptysis, PTB
F. GIT: abdominal pain or colic, changes in appetite, vomiting, diarrhea, stool color
and character, constipation, hematemesis, jaundice/hepatitis
G. GUT: urinary frequency, nocturia, polyuria,dysuria, bladder control, hematuria,
discharge, quality of urinary stream, previous infections, facial edema! change in
urinary pattern such as enuresis in previously toilet trained child
H. Musculoskeletal: joint pains or swelling, scoliosis, myalgia or weakness,
injuries, gait changes
I. Reproductive (Adolescents): secondary sexual characteristics, menses and
menstrual problems, pregnancies, sexual activity, genital discharges
THE PEDIATRIC PHYSICAL EXAMINATION
I. General Approach
A. Gather as much data as possible by observation first
B. Position of child: parents lap vs. exam table
C. Stay at the childs level as much as possible. Do not tower!!
D. Order of exam: from least distressing to most distressing with painful area last
E. Establish rapport with child
1. Explain to the childs level
2. Distraction is a valuable tool
F. Be honest. If something is going to hurt, tell them in a calm fashion. Dont lie or
you lose credibility!
G. Understand developmental stages impact on childs response. For example,
stranger anxiety is a normal stage of development, which tends to make
examining a previously cooperative child more difficult.
H. For adolescents, while doing PE, teach females the breast self-exam and males
the testicular exam.
II. General Survey
Development
Nutritional status: weight, height, BMI (kg/m
2
)
Presence or absence of distress
Sensorium and orientation
Type of cry or voice
State of hydration (ask about urine output)
Posture and gait
III. Vital Signs
Temperature
Heart rate (HR)
Respiratory rate (RR)
Blood pressure (BP): appropriate size cuff is 2/3 width of upper arm
Other anthropometric measurements
Head circumference (HC) during 1st 3 years
Chest circumference (CC)
Abdominal circumference (AC)
Pain
IV. Skin and Lymphatics
A. Birthmarks: nevi, hemangiomas, mongolian spots, etc
B. Color: pale or sallow, cyanotic, flushed, jaundice
C. Lesions: rashes, petechiae, desquamation, pigmentation, infections
D. Texture: turgor, moisture, CRT
E. Lymph node: enlargement, location, mobility, consistency
F. Scars or injuries, especially in patterns suggestive of abuse
V. HEENT
A. Face: expression, asymmetry, paralysis, facies
B. Head: contour, bossing, texture of hair, scalp, fontanelles
C. Eyes: conjunctivae, sclerae, PERLA, strabismus, EOM, ptosis, red orange reflex,
vision, eye contact and visual tracking
D. Ears: position, deformities, hearing, discharges, ear canals, tympanic
membranes, mastoid tenderness
E. Nose: patency, flaring of the alae nasi, discharges, nasal septum, nasal mucosa
color, polyps, sinus tenderness
F. Mouth and Throat: color of lips and buccal mucosa, fissures, lesions or sores,
tongue color and character, dental caries, color and character of gums, size,
color and exudates of tonsils and pharynx, gag relex
G. Neck: thyroid enlargement, trachea at midline, masses, sizes and character of
lymph nodes, presence or absence of nuchal rigidity
VI. Chest and Lungs
A. Inspection: contour of thorax and spine, symmetry of expansion, rate and
regularity of respiration, use of accessory muscles, retraction location
B. Palpation and percussion often not possible and rarely helpful
C. Auscultation: equality of breath sounds, stridor, wheezes, rhonchi, rales
VII. Heart
A. Inspection: precordial bulge or heave
B. Palpation: PMI diffused or circumscribed, thrills
C. Percussion: heart borders
D. Auscultation: rate, rhythm, murmurs, quality of heart sounds
VIII. Abdomen
A. Inspection: distended or scaphoid, visible veins, visible masses, umbilical
infection or hernia
B. Palpation: masses, organomegaly, direct and rebound tenderness
C. Percussion: tympanitic, dullness
D. Auscultation: bowel sounds
IX. Genito-Urinary Tract
A. Male: circumcision, phimosis, meatus, descent of testes, hydrocoele, inguinal
hernia, Tanner staging or SMR in adolescents
B. Female: external examination only, vulva, clitoris, discharge, Tanner staging or
SMR in adolescents
X. Rectal
Look for fissures, hemorrhoids, prolapse, sphincter tone, masses, tenderness, stool
in ampulla
XI. Extremities
A. General: deformity, symmetry, color, warmth, clubbing, edema
B. Pulses: presence, quality, equality
C. Joints: motion, stability, swelling, tenderness
D. Hips: Ortolanis and Barlows signs
E. Back: sacral dimple, kyphosis, lordosis or scoliosis
F. Gait: in-toeing or out-toeing, bow legs or knock knees, limping
XII. Neurologic
A. Cranial nerves I-XII (mnemonic: On Old Obando Tower Top A Filipino Army
Guard Villages And Huts)
B. Motor: paresis, paralysis, spasticity, romberg, rigidity, flaccidity, clonus,
carpopedal spasm, tics, tremors, athetosis
C. Reflexes: DTRs (biceps, triceps, radial, knee, ankle), superficial (abdominal,
cremasteric, primitive (moro, rooting, sucking, grasp, ATNR)
D. Sensory: superficial and deep sensations, pin-prick, touch, sense of position,
vibratory sense
E. Cerebellar signs: incoordination ataxia, intention tremor, past pointing,
dysdiadochokinesia, nystagmus on extreme lateral gaze
You might also like
- The Pediatric History and Physical Exam PDFDocument18 pagesThe Pediatric History and Physical Exam PDFOxana TurcuNo ratings yet
- (3F) Pediatrics - Pediatric HistoryDocument9 pages(3F) Pediatrics - Pediatric HistoryNomar Nonato100% (2)
- Pediatric History and Physical Exam TemplateDocument4 pagesPediatric History and Physical Exam TemplateJay Pee Tumaliuan Tumanguil0% (2)
- Tickler Final PDFDocument29 pagesTickler Final PDFSerious LeoNo ratings yet
- 01.15.01 Pediatric History Taking and Physical ExamDocument14 pages01.15.01 Pediatric History Taking and Physical ExamMikmik DGNo ratings yet
- Pediatrics H&P TemplateDocument3 pagesPediatrics H&P TemplateMark Ma80% (5)
- OBGYN Revalida Review 2019Document74 pagesOBGYN Revalida Review 2019anonymous100% (1)
- Pedia Revalida ReviewDocument83 pagesPedia Revalida Reviewcbac1990No ratings yet
- Clinical Clerkship Survival GuideDocument100 pagesClinical Clerkship Survival GuideRoendel Bustillo100% (3)
- MCU-FDT Outpatient ENT ServicesDocument2 pagesMCU-FDT Outpatient ENT ServicesvinbNo ratings yet
- Pedia ComputationsDocument5 pagesPedia ComputationsRheenz Fornoles100% (1)
- Philippine Pediatric Society, IncDocument19 pagesPhilippine Pediatric Society, IncAsmphLibrary OrtigasNo ratings yet
- Adolescent health assessmentDocument2 pagesAdolescent health assessmentBobet Reña80% (5)
- History and PEDocument3 pagesHistory and PEBom TnaNo ratings yet
- The Seven Habits of Highly Effective PeopleDocument60 pagesThe Seven Habits of Highly Effective PeopleBBCherriNo ratings yet
- Clinical Practice Guideline on Approach and Treatment of Urinary Tract Infection in ChildrenDocument8 pagesClinical Practice Guideline on Approach and Treatment of Urinary Tract Infection in ChildrenPaula QuiñonesNo ratings yet
- CEA SkillsDocument15 pagesCEA SkillsLloyd Fyl O. Razo75% (4)
- Pediatrics Pediatrics Pediatrics Pediatrics Pediatrics: Pediatrics Pediatrics Pediatrics Pediatrics PediatricsDocument2 pagesPediatrics Pediatrics Pediatrics Pediatrics Pediatrics: Pediatrics Pediatrics Pediatrics Pediatrics PediatricsBobet Reña100% (2)
- Luminare PGI Primer PDFDocument62 pagesLuminare PGI Primer PDFChristine Evan HoNo ratings yet
- FCM - The Impact of Illness To The FamilyDocument4 pagesFCM - The Impact of Illness To The FamilyEzekiel Arteta50% (2)
- Case Report: Pregnant Patient with VomitingDocument8 pagesCase Report: Pregnant Patient with VomitingAbdullah Matar86% (7)
- Derain Carla Elize-Group9 DXRDocument6 pagesDerain Carla Elize-Group9 DXRCarla Elize Derain100% (1)
- History Cs Admitting Notes: + 10 "U" Oxytocin X 8 HDocument7 pagesHistory Cs Admitting Notes: + 10 "U" Oxytocin X 8 HKarl Martin PinedaNo ratings yet
- 02 PEDIA250 (5) Pediatric History Taking PDFDocument11 pages02 PEDIA250 (5) Pediatric History Taking PDFJudith Dianne Ignacio100% (1)
- Febrile SeizuresDocument5 pagesFebrile SeizuresJulmajir Salipmugdar100% (1)
- Pedia HXDocument3 pagesPedia HXeyakoyNo ratings yet
- Med History & PE GuideDocument7 pagesMed History & PE GuideStephanie GaerlanNo ratings yet
- Pediatric Sample Case (Seizure) PDFDocument8 pagesPediatric Sample Case (Seizure) PDFIvan RoiNo ratings yet
- Notes For Pedia HandoutDocument2 pagesNotes For Pedia HandoutAiszel Angeli Pepito Ligo100% (2)
- Obstetric and Clinical Medicine - Gynaecological History and ExaminationDocument7 pagesObstetric and Clinical Medicine - Gynaecological History and ExaminationShahin Kazemzadeh100% (1)
- De La Salle Medical department valuesDocument26 pagesDe La Salle Medical department valuesIsabelle SampangNo ratings yet
- PPS Core PediatricsDocument53 pagesPPS Core PediatricsDenise Castro100% (3)
- 10 Warning Signs of ImmunodeficiencyDocument24 pages10 Warning Signs of Immunodeficiencyacque100% (2)
- Pediatric Respiratory Distress: Causes and ManagementDocument323 pagesPediatric Respiratory Distress: Causes and Managementmefav7778520100% (1)
- Leah Paula Briones, MD Marifi Rivera, MD: 2nd Edition 2011Document50 pagesLeah Paula Briones, MD Marifi Rivera, MD: 2nd Edition 2011deniseonscribdNo ratings yet
- Cirrhosis Complications and TreatmentsDocument8 pagesCirrhosis Complications and TreatmentsAlka Sangwan100% (2)
- Pediatrics NotesDocument25 pagesPediatrics Noteskcxie100% (12)
- Pedia Small Notebook EditedDocument17 pagesPedia Small Notebook EditedStarlet Rhonadez Bito-onon Oriel100% (12)
- Intern TicklerDocument10 pagesIntern TicklerRem AlfelorNo ratings yet
- History and Pe ObgynDocument4 pagesHistory and Pe ObgynCara Marrero IguidNo ratings yet
- Quizlet PDFDocument191 pagesQuizlet PDFsr100% (1)
- Pedia Notes: Anthropometric FluidsDocument9 pagesPedia Notes: Anthropometric FluidsIxc Nxc50% (2)
- PEDIATRIC NURSING GROWTH AND DEVELOPMENTDocument55 pagesPEDIATRIC NURSING GROWTH AND DEVELOPMENTJade Q Osit100% (6)
- PPHCH 2012Document41 pagesPPHCH 2012Jill P100% (1)
- Surgery Ple ReviewerDocument5 pagesSurgery Ple ReviewerReinhard Ivan MansibangNo ratings yet
- 1-Review of Neonatal History Taking and Physical ExaminationDocument9 pages1-Review of Neonatal History Taking and Physical ExaminationRogelio Blanco100% (2)
- Gynecology Review: Abigail Elsie Dg. Castro, MD, Maed, Fpogs, Fpsuog August 11, 2017Document198 pagesGynecology Review: Abigail Elsie Dg. Castro, MD, Maed, Fpogs, Fpsuog August 11, 2017Jojo Mendoza100% (1)
- (IM Ward) History Taking Tool PDFDocument15 pages(IM Ward) History Taking Tool PDFleapacis100% (1)
- History Taking in ObgynDocument17 pagesHistory Taking in Obgynselvie87100% (1)
- Formulas and DripsDocument6 pagesFormulas and DripsStarlet Rhonadez Bito-onon Oriel100% (2)
- CPG PCP ListDocument5 pagesCPG PCP ListBryan AtasNo ratings yet
- Pedia Case 1 Dengue 1Document9 pagesPedia Case 1 Dengue 1Rishi Du Agbugay100% (1)
- PM PFC MatrixDocument4 pagesPM PFC MatrixFamed residentsNo ratings yet
- Pharmacology Table - GonzalesDocument14 pagesPharmacology Table - GonzalesMark Angelo PonferradoNo ratings yet
- Essentials for Practice of Medicine in the Frontline: From Tropical Africa; Pleasantly Different Volume 2From EverandEssentials for Practice of Medicine in the Frontline: From Tropical Africa; Pleasantly Different Volume 2No ratings yet
- Pediatric Clinical History Physical Examination TemplateDocument9 pagesPediatric Clinical History Physical Examination TemplateTrisNo ratings yet
- Outline For Pediatric History and Physical Examination History I. Presenting Complaint (Informant/Reliability of Informant)Document4 pagesOutline For Pediatric History and Physical Examination History I. Presenting Complaint (Informant/Reliability of Informant)Hawkar SaeedNo ratings yet
- 7 Pediatric History and Physical ExaminationDocument45 pages7 Pediatric History and Physical ExaminationAmaetenNo ratings yet
- UNDERGRADUATE TEACHING-2 - PagenumberDocument13 pagesUNDERGRADUATE TEACHING-2 - PagenumberZaeem KhalidNo ratings yet
- Guide To The Comprehensive Pediatric H and P Write Up PDFDocument16 pagesGuide To The Comprehensive Pediatric H and P Write Up PDFnanaNo ratings yet
- From Er To Ward 1, 3, Micu: ToopdàDocument2 pagesFrom Er To Ward 1, 3, Micu: ToopdàJay VeeNo ratings yet
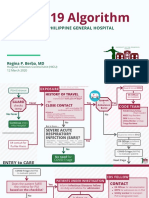
- COVID-19 Algorithm: For The Philippine General HospitalDocument10 pagesCOVID-19 Algorithm: For The Philippine General HospitalJay VeeNo ratings yet
- Emergency DashboardDocument1 pageEmergency DashboardJay VeeNo ratings yet
- RP Manual TemplateDocument9 pagesRP Manual TemplateJay VeeNo ratings yet
- Manual-R B-Medical ClearanceDocument2 pagesManual-R B-Medical ClearanceJay VeeNo ratings yet
- K1MTZDocument1 pageK1MTZJay VeeNo ratings yet
- Gym Work OutDocument19 pagesGym Work OutJay Vee100% (1)
- PPE Selection and Use GuideDocument5 pagesPPE Selection and Use GuideJay Vee100% (1)
- Biological Safety Cabinet Operation and Maintenance ProceduresDocument4 pagesBiological Safety Cabinet Operation and Maintenance ProceduresJay VeeNo ratings yet
- Sample Medical Guidelines: Congestive Heart FailureDocument2 pagesSample Medical Guidelines: Congestive Heart FailureJohanna ShuulukaNo ratings yet
- Department of Emergency Medicine: Philippine General Hospital University of The Philippines Manila Taft Avenue, ManilaDocument1 pageDepartment of Emergency Medicine: Philippine General Hospital University of The Philippines Manila Taft Avenue, ManilaJay VeeNo ratings yet
- Annex 2: Laboratory Assessment Tool / Facility QuestionnaireDocument57 pagesAnnex 2: Laboratory Assessment Tool / Facility QuestionnaireJay VeeNo ratings yet
- Near NCR (National Capital Region) - Quezon CityDocument1 pageNear NCR (National Capital Region) - Quezon CityJay VeeNo ratings yet
- Diseases of The Joint OutlineDocument1 pageDiseases of The Joint OutlineJay VeeNo ratings yet
- Final Covid Guideline PsmidDocument26 pagesFinal Covid Guideline PsmidJay VeeNo ratings yet
- Mental HealthDocument2 pagesMental HealthJay VeeNo ratings yet
- Workout Set A:: Barbell Front Squat (If You Don'T Have Access, Use DBS)Document1 pageWorkout Set A:: Barbell Front Squat (If You Don'T Have Access, Use DBS)Jay VeeNo ratings yet
- ENT-Larynx by Dr. Nixon SeeDocument7 pagesENT-Larynx by Dr. Nixon SeeJay VeeNo ratings yet
- Census MayDocument8 pagesCensus MayJay VeeNo ratings yet
- CK History Final W Pe Sample MentalDocument4 pagesCK History Final W Pe Sample MentalJay VeeNo ratings yet
- CK History Final W Pe Sample MentalDocument4 pagesCK History Final W Pe Sample MentalJay VeeNo ratings yet
- Revised Clinical HX For NewbornDocument3 pagesRevised Clinical HX For NewbornJay VeeNo ratings yet
- Pediatric History and Physical Exam GuideDocument7 pagesPediatric History and Physical Exam GuideIndunil AnuruddhikaNo ratings yet
- Anesthesia Finalsurgical AnestheisaDocument66 pagesAnesthesia Finalsurgical AnestheisaJay VeeNo ratings yet
- The Unhealthy Fast FoodDocument2 pagesThe Unhealthy Fast FoodRikudo AmubaNo ratings yet
- Common Psychosocial Problem in Adolescence: - Substance Abuse - Juvenile Delinquency - Smoking and AlcoholismDocument59 pagesCommon Psychosocial Problem in Adolescence: - Substance Abuse - Juvenile Delinquency - Smoking and AlcoholismSamjhana GautamNo ratings yet
- Microalbuminuria Is Associated With Cardiovascular Risk in Prediabetes and PrehypertensionDocument14 pagesMicroalbuminuria Is Associated With Cardiovascular Risk in Prediabetes and Prehypertensionد.عليالنجارالموسويNo ratings yet
- Camacho-Reyes v. ReyesDocument8 pagesCamacho-Reyes v. ReyesStradivariumNo ratings yet
- Prestigi0us BiochemistryDocument30 pagesPrestigi0us Biochemistrybovey69015No ratings yet
- Fatima Memorial Medical & Dental College & AHS, LahoreDocument8 pagesFatima Memorial Medical & Dental College & AHS, LahoreAqsa MohsinNo ratings yet
- The Top 10 Most Common Chronic Diseases For Older AdultsDocument9 pagesThe Top 10 Most Common Chronic Diseases For Older AdultstessahurintNo ratings yet
- Maple Syrup Urine DiseaseDocument14 pagesMaple Syrup Urine DiseasefantasticoolNo ratings yet
- Anesthesia and Myasthenia Gravis2012Document22 pagesAnesthesia and Myasthenia Gravis2012Alisher AgzamovNo ratings yet
- ANTI Ulcer DrugsDocument1 pageANTI Ulcer Drugsapi-3739910100% (1)
- Ca 19 9Document3 pagesCa 19 9डा. सत्यदेव त्यागी आर्यNo ratings yet
- Delusional DisorderDocument4 pagesDelusional DisorderNajm Us Saqib BhatNo ratings yet
- OtitaDocument99 pagesOtitaRoxana SurliuNo ratings yet
- Uswatun Hasanah-195037-2a Rmik (KKPMT)Document4 pagesUswatun Hasanah-195037-2a Rmik (KKPMT)Uswatun HasanahNo ratings yet
- Mon Surgical Infections Boils, Abscess, Ulcer, Cellulitis, Curbuncle, Gangrene, Sinus, Fistula CDocument48 pagesMon Surgical Infections Boils, Abscess, Ulcer, Cellulitis, Curbuncle, Gangrene, Sinus, Fistula CPanna SahaNo ratings yet
- The Weight Loss ManualDocument56 pagesThe Weight Loss ManualSomashekarNo ratings yet
- 2013 BAA - Glossary of Common Medical Prefixes and Suffixes For BAA and BLSDocument5 pages2013 BAA - Glossary of Common Medical Prefixes and Suffixes For BAA and BLSM GavinNo ratings yet
- The Easy Book of Cancer PharmacologyDocument526 pagesThe Easy Book of Cancer Pharmacologybianca100% (3)
- Acute Disease Case Study: Metabolism - HypothermiaDocument8 pagesAcute Disease Case Study: Metabolism - HypothermiaRegina PerkinsNo ratings yet
- Rosenhan - On-Being-Sane-In-Insane-Places PDFDocument10 pagesRosenhan - On-Being-Sane-In-Insane-Places PDFAlexandru Ioan CretuNo ratings yet
- Management of Diabetic Cats With Long Acting InsulinDocument16 pagesManagement of Diabetic Cats With Long Acting Insulindia_dianneNo ratings yet
- Quick Reference DMARDsDocument12 pagesQuick Reference DMARDsEman MohamedNo ratings yet
- PRIMARY HEALTH CARE - IMMUNIZATIONDocument24 pagesPRIMARY HEALTH CARE - IMMUNIZATIONAhmed Azeez100% (1)
- Digestive Health & You - 03062018Document8 pagesDigestive Health & You - 03062018Times MediaNo ratings yet
- Lesson Plan On SchizophreniaDocument22 pagesLesson Plan On SchizophreniaDurga KohaleNo ratings yet
- The Last LeafDocument22 pagesThe Last Leafdunitha dechamma kbNo ratings yet
- Bone Tumor: A. Nithya 1 Year M.SC (Nursing)Document46 pagesBone Tumor: A. Nithya 1 Year M.SC (Nursing)nithya nithyaNo ratings yet
- AP3 Form ApplicationDocument1 pageAP3 Form ApplicationBenjamin AcompaniadoNo ratings yet
- Introduction to Epidemiology and Public HealthDocument22 pagesIntroduction to Epidemiology and Public HealthIbrar Faisal0% (1)
- A Dictionary of Dentistry (Oxford Paperback Reference) by Robert IrelandDocument928 pagesA Dictionary of Dentistry (Oxford Paperback Reference) by Robert IrelandSalam Alyaseen100% (2)