Professional Documents
Culture Documents
Cmas 051 G
Uploaded by
NananiniPutriOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cmas 051 G
Uploaded by
NananiniPutriCopyright:
Available Formats
Otras secciones de
este sitio:
ndice de este nmero
Ms revistas
Bsqueda
Others sections in
this web site:
Contents of this number
More journals
Search
Artculo:
Pediatric anesthesia update
Derechos reservados, Copyright 2005:
Colegio Mexicano de Anestesiologa, AC
Revista Mexicana de Anestesiologa
Suplemento
Supplement
1 2005
Volumen
Volume
2 8
edigraphic.com
Revista Mexicana de Anestesiologa
S36
edigraphic.com
CONFERENCIAS MAGISTRALES
Vol. 28. Supl. 1 2005
pp S36-S40
C
C
O
L
E
G
IO
M
E
X
IC
ANO DEANESTESIO
L
O
G
A
A
.C
.
A
N
T
E
S
S
O
C
IE
D
A
D
MEXICANA DEAN
EST
E
S
IO
L
O
G
A
Anestesiologa
R
e
v
i
s
t
a
Mexicana de
Anestesiologa
Pediatric anesthesia update
Scott D. Cook-Sather, M.D.*
* Department of Anesthesiology and Critical Care Medicine, Childrens Hospital of Philadelphia,
University of Pennsylvania. School of Medicine.
OVERVIEW
Improving safety in pediatric anesthesia
POCA
Pediatric care environment
Evolving patterns
Preparatory issues
Respiratory problems:
OSA, RAD, UTI, ETS
Parental presence versus
sedatives at induction
Awareness and general
anesthesia
Intraoperative management
Tracheal intubation
Newer drugs in pediatric
practice
Regional techniques and
ultrasound
Postoperative considerations
Emergence delirium
Nausea and vomiting
POCA: PEDIATRIC PERIOPERATIVE CARDIAC
ARREST REGISTRY
289 cardiac arrests in registry
150 (52%) related to anesthesia
Incidence of 1.4 in 10,000 anesthetics
55% in infants <1 year of age
33% occurred in ASA PS 1-2 patients
Morray JP et al. Anesthesiology 2000;93:6
PEDIATRIC CARDIAC ARREST
MECHANISMS
36%
32%
20%
7%
5%
Medication
Cardiovascular
Respiratory
Equipment
Other
THE SAFETY OF REGIONAL
ANESTHESIA AND ANALGESIA
IN CHILDREN
85,412 pediatric procedures
in France
15,013 caudal blocks and 9,396
peripheral blocks
Most common complications
dural penetration
intravascular injection
Morbidity incidences
0.7/1000 caudal
0.0/1000 peripheral
0.9/1000 overall
Giaufre E et al. Anesth Analg 1996;83:904
Volumen 28, Suplemento 1, 2005 MG
Cook-Sather SD. Pediatric anesthesia update
S37
edigraphic.com
AMERICAN ACADEMY OF PEDIATRICS SECTION
ON ANESTHESIOLOGY
Evaluation and preparation of pediatric patients under-
going anesthesia
Means LM. Pediatrics 1996;98:502
Guidelines for the pediatric perioperative anesthesia en-
vironment
Hackel A. Pediatrics 1999;103:512
PEDIATRIC PERIOPERATIVE ENVIRONMENT
Risk of anesthesia varies with age
Facilities, equipment, staff training appropriate for in-
fants and children
Minimum case volumes to maintain clinical competence
Special clinical privileges: pediatric anesthesia fellows-
hip or equivalent
CHOP AMBULATORY SURGERY CRITERIA
ASA PS 1-3; well-controlled IDDM & SSDz allowed for
short, non-airway procedures
Age: > 1 mo for FT infants, > 60 wk PCA for former pre-
matures, > 3 years for T&A
No apnea monitoring, no severe OSA
Approved surgical procedure
Oral postoperative analgesics sufficient
AMBULATORY SURGERY FACILITY CRITERIA
ASA PS 1-2
Age > 6 mo, > 4 yr for T&A
BMI = Wt (kg)/BSA (m
2
) < 50; Wt < 100 kg
Normal airway, no significant OSA
Short, well-defined procedures
Oral postoperative analgesics sufficient
CARDIAC ARREST AFTER SUCCINYLCHOLINE
Patients (n) Mortality (%)
Receptor upregulation
Thermal trauma, muscle
trauma, denervation,
ICU milieu, Misc. 64 11
Rhabdomyolysis
Duchene, Becker,
Myopathy, Unknown
diagnosis 57 30
Gronert GA. Anesth 2001;94:523
RAPACURONIUM AND BRONCHOSPASM:
A RETROSPECTIVE COHORT STUDY
Bronchospasm None RR
n = 12 n = 275 (95% CI)
ASA III-IV (%) 6 (50) 81 (30) 2.2 (0.8-6.9)
RAD Hx (%) 7 (53) 59 (22) 4.6 (1.5-14.3)
RSI (%) 11 (92) 106 (39) 17.5 (2.9-inf)
Rajchert D, et al. Anesth Analg 2002;94:488
RAPACURONIUM AND BRONCHOSPASM:
A CASE CONTROL STUDY
Cases Controls OR
n = 23 n = 92 (95% CI)
RAD (%) 11 (48) 20 (22) 3.3 (1.3-8.5)
Rapacuronium (%) 12 (52) 9 (10) 10.1 (3.5-28.8)
Rajchert D, et al. Anesth Analg 2002;94:488
CARDIAC INDEX IN INFANTS: SEVOFLURANE
VERSUS HALOTHANE
0
50
100
150
200
250
300
350
Awake MAC 1.0 MAC 1.5
C
I
(
m
l
.
k
g
-
1
.
m
i
n
-
1
)
Halothane
Sevoflurane
Wodey E. Anesthesiology 1997;87:795
SEVOFLURANE OVER HALOTHANE
Decreased OCR incidence during strabismus surgery in
children
Allison CE. Anesth Analg 2000;90:306
Duration of preop fast correlates with ABP response to
halothane in infants
Friesen RH. Anesth Analg 2002;95:1572
Preservation of CI, HR, and less profound decreases in
BP in infants/children with CHD
Rivenes SM. Anesth 2001;94:223
Russell IA. Anesth Analg 2001;92:1152
Revista Mexicana de Anestesiologa
Cook-Sather SD. Pediatric anesthesia update
S38
edigraphic.com
RESPIRATORY ISSUES IN PEDIATRICS
Obstructive sleep apnea
Reactive airway disease
Upper respiratory tract infection
Secondhand tobacco smoke
DECREASED VENTILATORY RESPONSE
TO CO
2
IN CHILDREN WITH OBSTRUCTIVE
SLEEP APNEA
T&A + T&A Non AW
OSA + OSA - OSA
Slope: mL *min-1
*mmHgETCO2-
1
558 607 747
Corrected slope:
slope*m-2 538 338
828 234 850 380
p < 0.05 for OSA vs none
Strauss SG. Anesth Analg 1999;89:328
SALBUTAMOL PREVENTS THE INCREASE
OF RESPIRATORY RESISTANCE CAUSED
BY TRACHEAL INTUBATION DURING
SEVOFLURANE ANESTHESIA IN
ASTHMATIC CHILDREN
-10
-5
0
5
10
15
20
placebo
treatment
%
c
o
n
t
r
o
l
Rrs
Scalfaro P. Anesth Analg 2001;93:898
LARYNGOSPASM AND THE URI
Risk variable OR 95% CI P value
Parent: active URI 2.05 1.21-3.45 0.01
Age (continuous variable) 0.92 0.87-0.99 0.02
Procedure: Airway vs non 2.08 1.21-3.59 0.01
Midazolam vs none 0.57 0.32-1.05 0.07
Inexperienced vs
experienced supervisor 1.69 1.04-2.7 0.03
Schreiner MS. Anesthesiology 1996;85:475
TOBACCO SMOKE AND ADVERSE RESPIRATORY
EVENTS IN CHILDREN
Urinary Severe Sp O
2
Severe
cotinine cough < 95% Breath cough Laryngo-
(mg/ml) in OR in OR holding in RR spasm
0.0-9.9 1.0 1.0 1.0 1.0 1.0
10.0-39.9 1.8 1.1 1.7 1.8 0.7
(0.9-3.5) (0.5-2.6) (0.4-6.7) (0.7-4.6) (0.2-2.4)
> 40.0 2.3 2.6 5.1 2.3 2.3
(1.0-5.5) (1.1-6.2) (1.2-22.4) (0.7-7.7) (0.8-7.3)
Linear trend
test (p) 0.03 0.07 0.04 0.10 0.31
Skolnick ET. Anesthesiology 1998;88:1144
PARENTAL ANXIETY AT INDUCTION
Subgroup N Parent VAS
reception Induction
Calm-treatment 30 12.2 11.0 31.2 33.5
Calm-control 33 19.2 13.3 42.1 35.1
Anxious-treatment 24 78.8 16.6 81.7 18.7
Anxious-control 25 72.5 18.0 65.6 29.3
Bevan JC. Can J Anaesth 1990;37:177
PARENTAL ANXIETY AT INDUCTION:
CHILDRENS MOOD RESPONSE
Child s GMS
Subgroup N reception Induction
Calm-treatment 30 1.7 0.9 3.4 1.6
Calm-control 33 2.1 1.4 3.5 1.8
Anxious-treatment 24 1.7 1.2 4.5 1.5*
Anxious-control 25 1.6 0.8 3.4 1.5
* p < 0.05 A-T vs A-C at induction
Bevan JC. Can J Anaesth 1990;37:177
PPIA: ELEMENTS THAT UPSET PARENTS
1) Separation from the child
2) Watching or feeling the child go limp
3) Seeing the child upset
Vessey JA. Can J Anaesth 1994;41:276
Volumen 28, Suplemento 1, 2005 MG
Cook-Sather SD. Pediatric anesthesia update
S39
edigraphic.com
PEDIATRIC PERIOPERATIVE
ANXIETY: PPIA VS SEDATIVE
PREMEDICATION
0
10
20
30
40
50
60
Holding Area Induction 1 Induction 2
Control
PPIA
Premed
Y
P
A
S
S
c
o
r
e
Kain ZN. Anesthesiology 1998;89:1147
SEDATIVE PREMEDICATION
AND BEHAVIOR
0
10
20
30
40
50
60
70
80
90
Day 1 Day 2 Day 3 Week 1 Week 2
Placebo
Treatment
%
S
u
b
j
e
c
t
s
w
i
t
h
n
e
g
a
t
i
v
e
b
e
h
a
v
i
o
r
a
l
c
h
a
n
g
e
s
Kain ZN. Anesthesiology 1999;90:758
TRACHEAL INTUBATION WITHOUT
MUSCLE RELAXANT IN PEDIATRIC
ANESTHESIA
Rationale
Muscle relaxant not needed for intubation or surgery
NDMRs last too long, prefer to avoid succinylcholine
Lack assistant to start IV, difficult venous access
Educational tool
Politis GD. Anesth Analg 1999;88:737
Timing
140-190 sec under 8% sevoflurane
Ablation of SV associated with better conditions
Politis GD. Anesth Analg 2002;95:615
CUFFED VERSUS UNCUFFED TRACHEAL
TUBES IN PEDIATRIC ANESTHESIA
Cuffed Uncuffed
N = 251 N = 237 P value
Age (yr) 3.3 2.4 2.9 2.2 NS
Weight (kg) 15.4 7.4 14.3 7.7 NS
Intubation duration
(min) 55 60 NS
Pts needing TT
change 3 (1.2%) 54 (23%) < 0.001
Pts needing > 2 lpm
FGF 3 (1.2%) 26 (11%) < 0.001
Pts with croup sx 6 (2.4%) 7 (1.3) NS
Treated 3 (1.2%) 3 (1.3%) NS
Admitted 1 (0.4%) 1 (0.4%) NS
Khine HH. Anesthesiology 1997;86:627
REMIFENTANYL COMPARED TO ALFENTANYL,
ISOFLURANE, OR PROPOFOL FOR PEDIATRIC
STRABISMUS SURGERY
No difference in times to tracheal extubation, purposeful
movement, PACU or hospital DC
Remifentanil group: higher PACU pain scores
Alfentanil group had greater incidences of decreased
SpO2 and need for naloxone
No difference in incidences of emesis
Hemodynamic profiles similar
Davis PJ. Anesth Analg 1997;84:982
EPINEPHRINE TEST DOSING IN CHILDREN
DURING SEVOFLURANE VERSUS
HALOTHANE ANESTHESIA
0
0.05
0.1
0.15
0.2
0.25
0.3
0.35
0 0.5 1 2 3 4
Minutes after test dose injection
Sevoflurane
Halothane
Kozek-Langenecker SA. Anesth Analg 2000;90:579
Revista Mexicana de Anestesiologa
Cook-Sather SD. Pediatric anesthesia update
S40
edigraphic.com
ROPIVACAINE IN PEDIATRIC CAUDAL BLOCKS
Bupivacaine Ropivacaine Ropivacaine
0.25% 0.25% 0.5%
N 17 18 21
Analgesia duration 220 208 1,440
med.& range (min) (100-390) (175-340) (335-1,440)*
Stand (min) 253 39 248 30 362 42*
Void (min) 248 75 243 30 291 75***
* p < 0.0001 R0.5 vs other groups; ***p < 0.05 R0.5 vs other groups
Koining H. Anesthesiology 1999;90:1339
PEDIATRIC EPIDURAL ADJUVANTS
Ketamine
Koinig H. Anesth 2000;93:976
Clonidine
De Negri P. Anesth Analg 2001;93:71
Hager H. Anesth Analg 2002;94:1169
Fellmann C. Paed Anaesth 2002;12:637
Neostigmine
Abdulatif M. Anesth Analg 2002;95:1215
DELIRIUM AFTER SEVOFLURANE ANESTHESIA
Preschool School
Variable Halo Sevo Halo Sevo
N 30 30 26 26
Age (yr) 3 1 3 1 8 1 9 1
Wt (kg) 18.9 3.4 18.6 3.3 29.5 3.7 28.3 2.8
Surg (min) 29 4 28 8 41 6 43 6
Ext (min) 13 3 8 2* 12 2 8 3*
Emg (min) 15 3 12 3 15 4 12 4
Delirium 3/30 12/30 4/26 3/26
Incidence (10%) (40%)*** (15.4%) (11.5%)
* p < 0.0001, p < 0.01, p < 0.05, ***p < 0.01, 0.03
Aono J. Anesthesiology 1997;87:1298
RECOVERY CHARACTERISTICS: HALOTHANE
VERSUS SEVOFLURANE
Agitation PACU PACU 24 hr Home
pain med emesis emesis pain med
Group
H/K 12* 14* 2 10 48
H/P 42 48 14 17 61
S/K 14*** 22*** 6 12 65
S/P 38 46 6 11 61
Values in %; * p < 0.05 vs H/P group; ***p < 0.05 vs S/P group
Davis PJ. Anesth Analg 1999;88:34
NASAL FENTANYL & RECOVERY
CHARACTERISTICS AFTER BILATERAL
MYRINGOTOMY/TUBE PLACEMENT
Group CHEOPS Agitation Agitation PACU Emesis Emesis
max max score of 4 VAS hospital home
S/P 8.6 1.8 2.7 1.0 16/69 (23%) 53 36 13% 34/135 (25%)
S/F 7.2 1.6* 1.8 0.9* 1/64 (2%)* 82 25* 18%
H/P 8.4 2.0 2.3 1.0 7/63 (11%) 62 37 19% 65/130 (50%)***
H/F 6.8 1.7* 1.5 0.9* 1/67 (1%)* 85 25* 26%
* p < 0.05 when compared to both placebo groups, ***p < 0.05 H vs S
Galinkin JL. SPA Abstract 2000
SYSTEMIC POSTOPERATIVE ANALGESIA
Acetaminophen (20-40 mg/kg PR)
Birmingham PK. Anesthesiology 1997;87:244
Ketorolac (0.5-1.0 mg/kg IV)
Romsing J. Anaesthesia 1997;52:673
Morphine sulfate (0.05-0.1 mg/kg IV)
Weinstein MS. Anesthesiology 1994;81:572
Oxycodone (0.05-0.15 mg/kg PO)
Tramadol (50 mg tablets, unscored)
SINGLE-DOSE ONDANSETRON FOR PEDIATRIC
AMBULATORY SURGERY: PREVENTION OF
POSTOPERATIVE EMETIC EPISODES
Placebo Ondansetron
0-2 h 153/215 (71%) 190/213 (89)*
0-24 h 86/215 (40%) 143/210 (68)*
* p < 0.001 ondansetron vs placebo
Patel RI. Anesth Analg 1997;85:538
ONDANSETRON DEXAMETHASONE: EFFECT ON
VOMITING AFTER STRABISMUS SURGERY
Emetic episode Ondansetron
location 50 mg/kg +
dexamethasone Ondansetron P
150 mg/kg 150 mg/kg value
In-hospital 1% 7% < 0.05
At home day of
surgery 7% 14% NS
Next day 5% 15% < 0.05
Overall 9% 28% < 0.001
Splinter WM. Anesthesiology 1998;88:72
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Drugs in SportDocument180 pagesDrugs in Sportaermal89100% (1)
- Drug Categories According To The AHFSDocument6 pagesDrug Categories According To The AHFSBrian HarrisNo ratings yet
- CHEMICAL COMPOUNDS LISTDocument33 pagesCHEMICAL COMPOUNDS LISTHajellah AmpasoNo ratings yet
- Aseptic TechniquesDocument6 pagesAseptic TechniquesAinun MokhtarNo ratings yet
- RutaDocument7 pagesRutayvranprasadNo ratings yet
- Pharmacological Rationale For The Treatment of Chronic UrticariaDocument10 pagesPharmacological Rationale For The Treatment of Chronic Urticariaseptian88_cahyoNo ratings yet
- Medical Consent FormDocument2 pagesMedical Consent Formapi-235272235100% (1)
- Practice Test Questions Downloaded From FILIPINO NURSES CENTRALDocument4 pagesPractice Test Questions Downloaded From FILIPINO NURSES CENTRALFilipino Nurses CentralNo ratings yet
- mc-2 cmptd30-12-2019 3-1 SEC-B PDFDocument37 pagesmc-2 cmptd30-12-2019 3-1 SEC-B PDFvijay100% (1)
- Amitriptyline PDFDocument3 pagesAmitriptyline PDFscribdseewalNo ratings yet
- CRAFFTDocument2 pagesCRAFFTКонстантин КрахмалевNo ratings yet
- 1 - DS SATK Form - Initial Application of LTO 1.2Document4 pages1 - DS SATK Form - Initial Application of LTO 1.2Sophia TokieNo ratings yet
- Laporan Triwulan 2Document87 pagesLaporan Triwulan 2Nanda HotmanNo ratings yet
- United Arab Emirates Medicines Banned ListDocument15 pagesUnited Arab Emirates Medicines Banned ListAbdullah AnsariNo ratings yet
- Ebook BenzodiazepinesDocument26 pagesEbook BenzodiazepinesAnonymous Puj7S1tNo ratings yet
- Notice: Bischoff, James S., M.D.Document3 pagesNotice: Bischoff, James S., M.D.Justia.comNo ratings yet
- Understanding pain management for terminal cancer patientsDocument6 pagesUnderstanding pain management for terminal cancer patientsGunners CoolNo ratings yet
- Temozolomide 1Document3 pagesTemozolomide 1Prasetya BaktiNo ratings yet
- CMW Administrative Supervisory Checklist - AAP-Health-MNCHDocument5 pagesCMW Administrative Supervisory Checklist - AAP-Health-MNCHRehmatullahNo ratings yet
- Managing dental patients with cardiovascular diseasesDocument54 pagesManaging dental patients with cardiovascular diseasesSafiraMaulidaNo ratings yet
- Bronchitis: Causes, Symptoms and TreatmentDocument3 pagesBronchitis: Causes, Symptoms and TreatmentulfhasNo ratings yet
- RopDocument364 pagesRopIeie MawonNo ratings yet
- Antagonis Kolinergik Antagonis AdrenergikDocument8 pagesAntagonis Kolinergik Antagonis AdrenergikmarsellaNo ratings yet
- Daftar Nama Obat Klinik Pratama Satkeslap Sintang No Nama Obat KomposisiDocument4 pagesDaftar Nama Obat Klinik Pratama Satkeslap Sintang No Nama Obat Komposisinadya hermawanNo ratings yet
- Oktober 2017Document195 pagesOktober 2017Barkah Gitu AjaNo ratings yet
- Drug Related ProblemDocument13 pagesDrug Related ProblemLinda Yuni LestariNo ratings yet
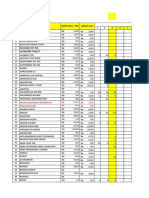
- Medication list with prices and categoriesDocument60 pagesMedication list with prices and categoriesThư PhùngNo ratings yet
- Antibiotics, Antibacterials, Antiprotozoals, NSAIDs, and other drugsDocument1 pageAntibiotics, Antibacterials, Antiprotozoals, NSAIDs, and other drugsMaria Francheska OsiNo ratings yet
- Divalproex Sodium brain disorder medicines guideDocument13 pagesDivalproex Sodium brain disorder medicines guideMiguelito Galagar GultianoNo ratings yet