Professional Documents
Culture Documents
Final For Guidelinecom
Uploaded by
api-2550842530 ratings0% found this document useful (0 votes)
67 views10 pagesOriginal Title
final for guidelinecom
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
67 views10 pagesFinal For Guidelinecom
Uploaded by
api-255084253Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 10
Page 1 of 10
University of Colorado Hospital Nursing Practice Guideline
Bone Marrow Transplant Unit: Neutropenic/Immunocompromised
Management for Hematologic Malignancies and Hematopoietic Stem Cell
Transplant Patients
Related Policies and Procedures:
Neutropenic Management for Oncology and Hematopoietic Stem Cell Transplant Patients
Standard Precautions
Hand Hygiene-Outside the Surgical Setting
Infection Control Surveillance
Isolation/Transmission Based Precautions
Blood/Body Fluid Spills
Aseptic Technique in Invasive and Operative Procedures
Clean/Sterile Supply Storage in Clinical Areas
Infectious/Regulated Waste Management
Employee Work Restrictions for Infectious Diseases
Live Plant and Flower Restrictions
Diet Restrictions and Recommendations for the Hematology and Oncology
Central Venous Lines
Animal Assisted Activities/Therapy Program
Approved by:
Director Hematologic Malignancies and BMT Programs
Oncology/Bone Marrow Transplant Clinical Nurse Specialist
Bone Marrow Transplant/Cancer Center Practice Manager
Effective: 5/14
Description:
This guideline defines neutropenia, as well as febrile neutropenia, and the necessary assessment
parameters, guidelines, interventions, and environmental modification that must be implemented
by University of Colorado Hospital health care providers in UCH clinical settings when caring
for neutropenic/immunocompromised Hematologic Malignancies and Hematopoietic Stem Cell
Transplant Patients.
Accountability:
All University of Colorado Hospital employees, physicians, volunteers, students, temporary and
contract employees are responsible for complying with the precautions/measures described in
this guideline. Visitors and other non-hospital-employee personnel will be informed of and asked
to comply with the provisions of this guideline by the University of Colorado Hospital staff.
Non-compliance will be dealt with on an individual basis.
Definitions:
Neutrophils are the bodys first line of defense against microbial invasion. They constitute
Bone Marrow Transplant Unit: Neutropenic/Immunocompromised
Management for Hematologic Malignancies and Hematopoietic Stem Cell
Transplant Patients
Page 2 of 10
approximately 40%-60% of the total white blood cell count that usually ranges from 4,000-
10,000/mm
3
.
Neutropenia is defined as an absolute neutrophil count (ANC) less than 500/mm
3
1. The relative risk for infection increases as the ANC decreases. The ANC is categorized
into grades, which reflect the risk for infection.
a. Grade 1: ANC 1500-2000/mm
3
= No Significant Risk
b. Grade 2: ANC 1000-1500/mm
3
=Slight Increase in Risk
c. Grade 3: ANC 500-1000/mm
3
=Moderate Risk=Neutropenia
d. Grade 4: ANC less than 500/mm
3
=High Risk=Neutropenia
Signs and Symptoms of I nfection
1. Localized symptoms of infection: pain at the site of infection that may or may not include
erythema or exudate.
2. Generalized symptoms of infection: chills, myalgias, arthralgias, cognitive or mental
status changes, anorexia, nausea/vomiting, fatigue, tachycardia, hypotension, tachypnea,
hypoxemia, oliguria, and fever.
3. Site-Specific symptomatology/exam findings: cough, dyspnea, abnormal breath sounds
oral pain, back pain, rigors, rectal discomfort with bowel elimination, pain at vascular
access device site, burning/urgency with urination.
Sources of I nfection
1. The skin and mucous membranes are vulnerable sources of microbial invasion due to
IV/Central line access and mucositis. Additional risk factors include GVHD (Graft
versus Host Disease), and toxicities from conditioning regimens that cause prolonged
neutropenia (10-30 days).
2. Primary sites of infection in the neutropenic patient are the digestive tract (mouth,
pharynx, esophagus, large and small bowel, rectum), as well as the sinuses, lungs, and
skin.
3. Hand hygiene is considered the most important procedure to prevent the spread of
infections. Refer UCH Policy and Procedure: Hand Hygiene-Outside The Surgical
Setting.
Practice Guidelines:
A. Assessment Parameters
1. Fever (single temperature greater than or equal to 38.3 degrees Celsius or a
temperature greater than or equal to 38 degrees Celsius sustained for greater than one
hour) is usually the first and only sign of a potentially life-threatening infection.
2. Localized symptoms of infection such as redness, swelling, pain, and exudate may
not be present due to the inability of the patients body to create an inflammatory
response resulting from the absence or decreased number of neutrophils.
Bone Marrow Transplant Unit: Neutropenic/Immunocompromised
Management for Hematologic Malignancies and Hematopoietic Stem Cell
Transplant Patients
Page 3 of 10
3. Although uncommon, a patient with neutropenia and signs or symptoms of infection
(i.e. abdominal pain, severe mucositis, or perirectal pain) without fever, should be
considered to have an active infection.
B. Assessment Guidelines
1. Determine expected duration and severity of neutropenia
a. Consider the patients current and past treatment regimens including one or
more of the following: chemotherapy, radiation therapy, immunotherapy,
immunosuppressive therapy, HSCT.
b. Consider the patients comorbitities, medications, history of prior documented
infections, recent antibiotic therapy, exposure to infections from household
members, pets, travel (including Tuberculosis exposure), HIV status, and
recent blood product administration.
2. Assess for common sites of infection in patients with fever and neutropenia: the
alimentary tract, groin, skin, lungs, sinus, ears, perivagina, perirectum, and vascular
access device sites
3. Monitor vital signs (T,P,R,BP) Q4h or more often depending on clinical situation
(Provider decision)
4. Monitor Intake and Output Q4h
5. Obtain BID weights on all active HSCT patients and all HSCT that are readmitted
post transplant.
6. Monitor laboratory data:
a. CBC with differential, including WBC count. If ANC less than 1000, institute
neutropenic precautions. Refer to Neutropenic Precautions sign (Appendix
A).
b. Comprehensive Metabolic Panel, LDH, Uric Acid, Creatinine, BUN, LFTs,
Total Serum Bilirubin, and lactate as ordered by provider.
c. Blood and other Culture Reports-notify Provider if positive and institute
appropriate transmission based precautions if necessary. Refer to UCH Policy
and Procedure: Isolation/Transmission Based Precautions.
d. Consult Provider for potential chest x-ray, urinalysis, urine culture/sensitivity,
and pulse ox. Chest x-ray for all patients with respiratory symptoms.
C. Nursing Intervention For Treatment of Febrile Neutropenia
1. Febrile Neutropenia/Immunocompromised Fever in Hematologic Malignancies
and HSCT
a. Patients admitted for HSCT are treated with prophylactic antibiotics prior to
becoming neutropenic and throughout the expected neutropenic state during
hospitalization. Once patients receive their stem cells, they may begin G-CSF
(Dual cord SCT or Autologous SCT) therapy to assist in WBC recovery.
Refer to EHR for details.
Bone Marrow Transplant Unit: Neutropenic/Immunocompromised
Management for Hematologic Malignancies and Hematopoietic Stem Cell
Transplant Patients
Page 4 of 10
b. When a patient becomes febrile (a single temperature greater than or
equal to 38.3 degrees Celsius or temperature greater than or equal to 38
degrees Celsius sustained for greater than one hour), refer to EHR , which
indicate obtaining a chest x-ray, urinalysis, urine culture and sensitivity, and at
least two sets of blood cultures. At least one of the two sets of cultures is to
be obtained from the patients vascular access device if present.
1. Collaborate with the Provider regarding obtaining one of the two sets
of blood cultures peripherally.
c. According to the 2013 NCCN guidelines, if there is entry or exit site
inflammation around the vascular access device; 1) obtain a set of blood
cultures from each lumen 2) swab exit site drainage (if present) for culture
and 3)Vancomycin should be considered. If the vascular access device
cultures are positive for infection, collaborate with the Provider regarding
obtaining further blood cultures from each lumen, removal of vascular access
device, and additional antibiotic therapy. Notify provider immediately if port
pocket infection is suspected. Do not access the implanted port if infection
is suspected due to increased risk of further infection.
d. If patient symptomatology warrants, collaborate with the Provider regarding
obtaining site-specific cultures including rectal, stool, skin, mouth, throat,
sputum, and nasopharynx.
e. If patient continues to be febrile, blood cultures are to be done once every 24
hours. Other diagnostic tests such as, chest x-ray, urinalysis, urine culture and
sensitivity, ect. may be ordered based on provider preference.
f. Refer to EHR for fever day antibiotic instructions. Once the patient is febrile
(a single temperature greater than or equal to 38.3 degrees Celsius or
temperature greater than or equal to 38 degrees Celsius sustained for greater
than one hour ), antibiotics are to be given according to Fever Day 1
instructions. Initiate antibiotic therapy within the hour of the fever but not
before obtaining blood cultures. DO NOT HOLD ANTIBIOTICS FOR
COMPLETION OF CHEST X-RAY AND/OR URINE TESTS. For each
subsequent fever not within consecutive 24-hour periods, collaborate with
Provider regarding antibiotics to start/discontinue. If a patient continues to be
febrile for consecutive 24-hour periods, continue to follow the EHR indicating
which antibiotics to administer.
g. S/P Hematopoietic Stem Cell Transplant Patients returning to the hospital for
complications related to their transplant, including infection, are to be
directly admitted to the Hematopoietic Stem Cell Transplant unit when
possible. When a bed is not available, consult with provider regarding
appropriate triage.
1. If patient is febrile, ED Provider is to collaborate with Heme/BMT
Provider regarding ED Approach to Patient with Possible Neutropenic
Fever (Appendix B). Heme/BMT Pager: 303-266-4162
2. If patient is being admitted through the ED or Inpatient due to a fever
refer to the BMT/HEME ED/INPATIENT RAPID RESPONSE FEVER
PROTOCOL (RRFP) (Appendix C)
Bone Marrow Transplant Unit: Neutropenic/Immunocompromised
Management for Hematologic Malignancies and Hematopoietic Stem Cell
Transplant Patients
Page 5 of 10
2. Environmental Modification
a. All neutropenic patients are placed in private rooms. Patients admitted for
HSCT are to be placed in positive pressure rooms with HEPA filtration.
b. Neutropenia precaution sign is to be placed beside the door to alert staff and
visitors of infection prevention protocol/measures. Refer to Neutropenic
Precautions sign (Appendix A).
3. Protective Measures for Neutropenic Patients
a. Handwashing is the single most important intervention to prevent infection.
1. All persons entering the room will soap and wash hands at time of entry
and time of exit with either alcohol based gel or with soap and water for
15 seconds.
b. Anyone with symptoms of illness is to avoid contact with neutropenic
patients. When contact is unavoidable, staff/visitors are to wear masks when
entering the patients room and adhere to proper hand hygiene.
c. Children under the age of 12 are not to enter the Hematopoietic Stem Cell
Transplant unit regardless of the presence of neutropenic patients.
d. Once neutropenic, ANC less than 1000, these patients are to be instructed to
wear this mask whenever they leave their room.
e. HSCT patients who are under contact isolation due to their being infected with
a highly transmissible infectious organism, such as VRE and MRSA, are to
remain in their room at all times, unless required to leave their room for
testing. In this case, the patient is to wear appropriate PPE, including yellow
gown, and gloves. If the patient is neutropenic and/or under airborne/droplet
precautions a mask is to be worn
f. Avoid rectal maneuvers (rectal temperatures, enemas, rectal medications,
rectal tubes, digital exams) and urinary catheterizations.
g. Avoid breakdown of skin and mucous membranes by limiting venipunctures
or other invasive procedures. Cleanse and protect wounds that break the skin
as directed by the Provider.
h. Refer to the Diet Restrictions and Recommendations for the Hematology and
Oncology Immunocompromised Patient
i. Change urinals and hats when visibly soiled. Change nasal canulas, O2 masks
weekly and when visibly soiled.
j. Encourage consistent patient personal hygiene
1. Daily shower or bath, including shampooing head/hair. Use CHG wipes
as directed for central line care.
2. Change linens daily and more frequently if visibly soiled.
3. Routine oral care. Recommended to brush teeth with a soft toothbrush
four times daily and then rinse with salt and soda mixture (provided by
nursing staff) after each brushing.
k. Live plant and flowers are not allowed in the rooms of neutropenic patients
whose immune compromise is such that infection can be acquired from
Bone Marrow Transplant Unit: Neutropenic/Immunocompromised
Management for Hematologic Malignancies and Hematopoietic Stem Cell
Transplant Patients
Page 6 of 10
soil/plant organisms. Refer to UCH Policy and Procedure: Live Plant and
Fresh Flower Restrictions.
l. Animals are restricted from the HSCT unit due to the potential infection risk
for the immunocompromised patient population. Refer to UCH Policy and
Procedure: Animal Assisted Activities/Therapy Program.
References:
1. Dellinger R.P., Levy M.M., Rhodes A, et al. (2012) Surviving sepsis campaign:
international guidelines for management of severe sepsis and septic shock: 2012.
Critical Care Medicine. 41(2):580-637. (LOE 7)
2. Irwin, M., Erb, C., Williams, C., Wilson, B., & Zitella, L. (2013). Putting Evidence Into
Practice:Improving Oncology Patient Outcomes. Pittsburgh, PA: Oncology Nursing Society.
(LOE 1)
3. Marrs, J. (2006). Care of Patients With Neutropenia. Clinical Journal of Oncology Nursing,
10(2), 164-166. (LOE 8)
4. NCCN. (2013). Fever and Neutropenia-v.1.2013. NCCN Clinical Practice Guidelines in
Oncology. (CD). Jenkintown, PA: NCCN. (LOE 7)
5. Nirenberg, A., Bush, A.P., Davis, A., Friese, C.R., Gillespie, T.W., Rice, R.D. (2006).
Neutropenia: State of the Knowledge Part I/Part II. Clinical Journal of Oncology Nursing,
33(6), 1193-1201, 1202-1208. (LOE 1)
6. Shelton, B.K. (2003). Evidence-Based Care for the Neutropenic Patient with Leukemia.
Seminars in Oncology Nursing, 19(2), 133-141. (LOE 7)
7. Zitella, L., Friese, C., Hauser, J., Holmes, B.G., Woolery, M.A., OLeary, C., Andrews, F.
(2006). Putting Evidence Into Practice: Preventions of Infection. Clinical Journal of
Oncology Nursing, 10(6), 739-750. (LOE 1)
Bone Marrow Transplant Unit: Neutropenic/Immunocompromised
Management for Hematologic Malignancies and Hematopoietic Stem Cell
Transplant Patients
Page 7 of 10
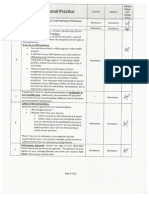
Appendix A
NEUTROPENIC PRECAUTIONS/IMMUNOCOMPROMISED PATIENTS
WASH HANDS BEFORE PATIENT CONTACT
Visitors with cold symptoms or contagious illness should not visit patient at this time.
Patient MUST wear a mask when leaving room.
NO FRESH FLOWERS OR PLANTS.
DIETARY RESTRICTIONS INCLUDE:
Fresh fruit and vegetables ONLY if washed under running water prior to peeling, cutting, or
eating (berries and sprouts excluded)
NO soft cheeses, unpasteurized foods/fluids, or pepper (from pepper shakers or pepper mills)
NO undercooked or raw meat, fish, eggs, or tofu.
Unroasted nuts or nuts in a shell
Teas will be prepared directly by staff for patient by request.
PLEASE SEE THE NURSE IF YOU HAVE ANY QUESTIONS REGARDING THESE
PRECAUTIONS
Bone Marrow Transplant Unit: Neutropenic/Immunocompromised
Management for Hematologic Malignancies and Hematopoietic Stem Cell
Transplant Patients
Page 8 of 10
Appendix B
ED Approach to Immunocompromised Patients and/or Possible Neutropenic Fever
ED GOAL:
PLEASE PAGE THE BMT/HEME TEAM I MMEDI ATELY UPON PATI ENT TRI AGE
Pager: 303-266-4162
To administer antibiotics within 1 hour of ED presentation for
Immunocompromised/Neutropenic Patients
PIVOT PROCEDURE:
Identify high risk patient at Pivot
Patient s/p chemotherapy/radiation treatment within 14 days
Patient s/p hematopoietic stem cell transplant
Hematologic Malignancies with fevers or other vague complaints
Provide and instruct suspected neutropenic patient to wear a mask
Obtain patients weight
Document Neutropenic Patient in comments on tracking board
Assign patient to an Intake room from pivot (single patient area) to be evaluated by an
attending physician. Intake attending may include neutropenic precautions if the patient has
known or suspected neutropenia. The patient may then be placed in an ED treatment room in
Main ED if recommended by provider.
Notify Resource Nurse, who will notify attending or senior resident of patients arrival. Call
HEME/BMT Pager 303-266-4162 upon patient arrival to the Emergency Department.
Place Neutropenic packet of algorithms on patients chart and verify allergies once patient is
in the Main ED.
ED PROCEDURE:
INITIATE RAPID RESPONSE FEVER PROTOCOL (RRFP) BASED ON ED OR
HEME/BMT PROVIDER ORDER ENTRY. FOLLOW APPENDIX C.
Bone Marrow Transplant Unit: Neutropenic/Immunocompromised
Management for Hematologic Malignancies and Hematopoietic Stem Cell
Transplant Patients
Page 9 of 10
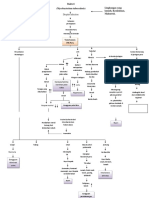
Appendix C
BMT/HEME ED/INPATIENT RAPID RESPONSE FEVER PROTOCOL (RRFP)
Patient Qualifies for
RAPID RESPONSE FEVER PROTOCOL
Hospital Admission
Please note: This pathway is NOT an order set. This is a guideline for MDs/RNs
for the INITIAL (first hour) management of Heme/BMT patients who present to
the ED or Inpatient Unit with FEVER or other signs of serious infection. This
pathway will be accompanied by an order set.
PLEASE PAGE THE BMT/HEME TEAM IMMEDIATELY UPON PATIENT TRIAGE
Pager: 303-266-4162
Vital Signs
Every 15min. X4, then every 30min. X2, then every 60min.
Labs
(CBC/diff, CMP, Mg, Phos, LDH, Uric acid, Lactate)
Blood cultures
(2 sets from Central Line and 1 simultaneous peripheral set)
If difficult peripheral stick, complete Central Line cultures only
OR
2 set peripherally if no Central Line
IV Fluid Bolus
(NS 1000cc wide open)
If patient unstable (SBP<90, HR>120, dizziness, altered mental status), start IV
Fluid Bolus immediately after Vital Signs and notify NP/MD immediately
ANTIBIOTICS
(Please use the RRFP FEVER order set)
cefepime 2gm IV Q8
+/-
Vancomycin (use ONLY if hemodynamic instability, suspected line or skin
infection, suspected MRSA, PNA, mucositis)
If severe allergy to PCN/cephalosporins, use alternative antibiotics per RRFP
Bone Marrow Transplant Unit: Neutropenic/Immunocompromised
Management for Hematologic Malignancies and Hematopoietic Stem Cell
Transplant Patients
Page 10 of 10
order set
Above interventions to be completed within 30 min. of patient
arrival to ED/Inpatient Unit if Direct Admit
Diagnostic Testing/Source ID
CXR, CT, UA C&S, etc.
Do NOT delay antibiotics waiting for CXR or UA!!
11
th
Floor Inpatient Management
OR
ICU Transfer for EGDT if Unstable
You might also like
- OriginalneutropolicyDocument9 pagesOriginalneutropolicyapi-255084253No ratings yet
- Cna AcpcounciltemplateaprilDocument1 pageCna Acpcounciltemplateaprilapi-255084253No ratings yet
- NeutrotoppppcDocument10 pagesNeutrotoppppcapi-255084253No ratings yet
- Advisor ChecklistDocument6 pagesAdvisor Checklistapi-255084253No ratings yet
- Pdca 2Document7 pagesPdca 2api-255084253No ratings yet
- Cna FlyerDocument1 pageCna Flyerapi-255084253No ratings yet
- Cnaacuitytool 3Document1 pageCnaacuitytool 3api-255084253No ratings yet
- Cna AcpcounciltemplatemarchDocument1 pageCna Acpcounciltemplatemarchapi-255084253No ratings yet
- Kyles Email Precepting AttendanceDocument2 pagesKyles Email Precepting Attendanceapi-255084253No ratings yet
- Meeting Minutes From March EmailDocument1 pageMeeting Minutes From March Emailapi-255084253No ratings yet
- Summary Email of April MeetingsDocument2 pagesSummary Email of April Meetingsapi-255084253No ratings yet
- Cna AcpcounciltemplatefebDocument1 pageCna Acpcounciltemplatefebapi-255084253No ratings yet
- Email Confirmation From Anita All Cnas Are AddedDocument2 pagesEmail Confirmation From Anita All Cnas Are Addedapi-255084253No ratings yet
- Minutes From 3-14 MeetingDocument2 pagesMinutes From 3-14 Meetingapi-255084253No ratings yet
- Mandatory April Meeting EmailDocument1 pageMandatory April Meeting Emailapi-255084253No ratings yet
- Sharepoint Vs Staff MeetingsDocument2 pagesSharepoint Vs Staff Meetingsapi-255084253No ratings yet
- Minutes From 2-14 MeetingDocument4 pagesMinutes From 2-14 Meetingapi-255084253No ratings yet
- Annsleys Response To FallsDocument2 pagesAnnsleys Response To Fallsapi-255084253No ratings yet
- Feedback Barb From Focus PdcaDocument2 pagesFeedback Barb From Focus Pdcaapi-255084253No ratings yet
- Falls Question CnaacpsDocument2 pagesFalls Question Cnaacpsapi-255084253No ratings yet
- Email To Cnaacps About How To Access SPDocument1 pageEmail To Cnaacps About How To Access SPapi-255084253No ratings yet
- 1st Sharepoint Posting CnaDocument2 pages1st Sharepoint Posting Cnaapi-255084253No ratings yet
- Post Survey Respondent Unmatched Demographics UnmatchedDocument1 pagePost Survey Respondent Unmatched Demographics Unmatchedapi-255084253No ratings yet
- Post Survey Table MatchedDocument1 pagePost Survey Table Matchedapi-255084253No ratings yet
- Email To Anita About SPDocument1 pageEmail To Anita About SPapi-255084253No ratings yet
- Kayla Eval On MeDocument1 pageKayla Eval On Meapi-255084253No ratings yet
- Email About Sharepoint and TitlingDocument1 pageEmail About Sharepoint and Titlingapi-255084253No ratings yet
- Precept Form From KaylaDocument3 pagesPrecept Form From Kaylaapi-255084253No ratings yet
- 5314 Look Report Cna EmailDocument2 pages5314 Look Report Cna Emailapi-255084253No ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5782)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Menstrual Disorders WDDDocument43 pagesMenstrual Disorders WDDadystiNo ratings yet
- 7 Xray Questions Handout793266145Document3 pages7 Xray Questions Handout793266145jojoNo ratings yet
- Fundamentos de Auscultacion Pulmonar NEJM PDFDocument8 pagesFundamentos de Auscultacion Pulmonar NEJM PDFMaría Fernanda RíosNo ratings yet
- Droplet Infection: Tuberkulosis (TB) ParuDocument2 pagesDroplet Infection: Tuberkulosis (TB) ParuMiiniieNo ratings yet
- Anemia and Thrombocytopenia in Acute and Chronic Renal Failure PDFDocument6 pagesAnemia and Thrombocytopenia in Acute and Chronic Renal Failure PDFSatriyo Dwi SuryantoroNo ratings yet
- Medical Surgical Nursing Bullets Nle NclexDocument95 pagesMedical Surgical Nursing Bullets Nle NclexRichard Ines Valino100% (2)
- Ultimate Cancer Survival GuideDocument38 pagesUltimate Cancer Survival GuideMichel PillotNo ratings yet
- Presented by - R Hemamalini 2010CYZ8795 Group G1Document29 pagesPresented by - R Hemamalini 2010CYZ8795 Group G1h_rajagopalan100% (1)
- Tuberculum Sellae MeningiomaDocument9 pagesTuberculum Sellae MeningiomaFerina Nur HaqiqiNo ratings yet
- Household Chemicals and Personal Care Products GuideDocument5 pagesHousehold Chemicals and Personal Care Products GuidePhoebe Mariano100% (1)
- Rachmat Gunadi Wachjudi's resume and clinical relevance of vitamin DDocument38 pagesRachmat Gunadi Wachjudi's resume and clinical relevance of vitamin DNururrohmahNo ratings yet
- @enmagazine Psr7bcdt2ridkoDocument28 pages@enmagazine Psr7bcdt2ridkorahulNo ratings yet
- Gluteal Fold V Y Advancement Flap For Vulvar And.20Document6 pagesGluteal Fold V Y Advancement Flap For Vulvar And.20Ximenita GhilardiNo ratings yet
- How Artificial Intelligence Is Impacting HealthcareDocument2 pagesHow Artificial Intelligence Is Impacting HealthcareAlexNo ratings yet
- MTLBE Midterms PDFDocument4 pagesMTLBE Midterms PDFKristine Marie PateñoNo ratings yet
- Nursing Q and A (Volume 2)Document7 pagesNursing Q and A (Volume 2)Rem Yriz100% (1)
- Synthesis and Functions of Steroid HormonesDocument54 pagesSynthesis and Functions of Steroid HormonesfanyazharNo ratings yet
- Ent Diseases of The Oral and Pharynx Dr. UyDocument7 pagesEnt Diseases of The Oral and Pharynx Dr. UyAileen EmyNo ratings yet
- Basics of Neoplasm: Understanding Benign vs Malignant TumorsDocument30 pagesBasics of Neoplasm: Understanding Benign vs Malignant TumorsSaraNo ratings yet
- Claim Form For Secure Mind PolicyDocument4 pagesClaim Form For Secure Mind PolicyRamya RaviNo ratings yet
- Liver Function TestsDocument70 pagesLiver Function TestsG Venkatesh100% (4)
- Competency Appraisal II: Lung/Bronchogenic CancerDocument7 pagesCompetency Appraisal II: Lung/Bronchogenic CancerArnie Jude CaridoNo ratings yet
- Limfadenitis Akut Dan KronisDocument24 pagesLimfadenitis Akut Dan KronisRezy Pysesia AlfaniNo ratings yet
- NLE Topics by Dr Asif AliDocument8 pagesNLE Topics by Dr Asif AliMueen AhmadNo ratings yet
- Eyelid Lumps and BumpsDocument43 pagesEyelid Lumps and BumpsAbdul HannanNo ratings yet
- Hirsutism and HomoeopathyDocument9 pagesHirsutism and HomoeopathyDr. Rajneesh Kumar Sharma MD HomNo ratings yet
- Cross Talk Between Oxidative Stress and Inflammation in Alopecia AreataDocument6 pagesCross Talk Between Oxidative Stress and Inflammation in Alopecia AreataDr-Iman NutritionistNo ratings yet
- Ethnomedicine Traditional Knowledge Nort PDFDocument11 pagesEthnomedicine Traditional Knowledge Nort PDFMigjofNo ratings yet
- The Truth About Cancer and Essential OilsDocument4 pagesThe Truth About Cancer and Essential Oilscristian964No ratings yet
- Irritable Bowel SyndromeDocument4 pagesIrritable Bowel SyndromeJehanzeb ZebNo ratings yet