Professional Documents
Culture Documents
LO Week 5
Uploaded by
noorgianilestariOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
LO Week 5
Uploaded by
noorgianilestariCopyright:
Available Formats
LEARNING OBJECTIVE ICM 1 WEEK V
LO.1. > Rotator Cuff tear , when one or more of the rotator cuff tendons is torn, the
tendon no longer fully attaches to the head of the humerus. Most tears occur in the
supraspinatus muscle and tendon, but other parts of the rotator cuff may also be
involved.
In many cases, torn tendons begin by fraying. As the damage progresses, the tendon
can completely tear, sometimes with lifting a heavy object.
There are different types of tears :
1. Partial Tear, this type of tear damages the soft tissue, but does not completely
sever it.
2. Full-Thickness Tear, this type of tear is also called a complete tear. It splits the
soft tissue into two pieces. In many cases, tendons tear off where they attach
to the head of the humerus. With a full-thickness tear, there is basically a hole
in the tendon.
there are two main causes of rotator cuff tears: injury and degeneration.
Acute tear, if fall down on outstretched arm or lift something too heavy with a jerking
motion, can tear your rotator cuff. This type of tear can occur with other shoulder
injuries, such as a broken collarbone or dislocated shoulder.
Degenerative tear, most tears are the result of a wearing down of the tendon that
occurs slowly over time or by rotator cuff impingement. This degeneration naturally
occurs as we age. Rotator cuff tears are more common in the dominant arm. If you
have a degenerative tear in one shoulder, there is a greater risk for a rotator cuff tear
in the opposite shoulder -- even if you have no pain in that shoulder.
Several factors contribute to degenerative, or chronic, rotator cuff tears :
- Repetitive stress. Repeating the same shoulder motions again and again can
stress your rotator cuff muscles and tendons. Baseball, tennis, rowing, and
weightlifting are examples of sports activities that can put you at risk for
overuse tears. Many jobs and routine chores can cause overuse tears, as well.
- Lack of blood supply. As we get older, the blood supply in our rotator cuff
tendons lessens. Without a good blood supply, the body's natural ability to
repair tendon damage is impaired. This can ultimately lead to a tendon tear.
- Bone spurs. As we age, bone spurs (bone overgrowth) often develop on the
underside of the acromion bone. When we lift our arms, the spurs rub on the
rotator cuff tendon. This condition is called shoulder impingement, and over
time will weaken the tendon and make it more likely to tear.
The most common symptoms of a rotator cuff tear include:
Pain at rest and at night, particularly if lying on the affected shoulder
Pain when lifting and lowering your arm or with specific movements
Weakness when lifting or rotating your arm
Crepitus or crackling sensation when moving your shoulder in certain positions
Tears that happen suddenly, such as from a fall, usually cause intense pain. There may be a
Noorgiani Lestari-07120100056
snapping sensation and immediate weakness in your upper arm
LO.2. > Rotator cuff tendinitis refers to irritation of these tendons and inflammation
of the bursa (a normally smooth layer) lining these tendons or damage the rotator cuff
tendons. A rotator cuff tear occurs when one of the tendons is torn from overuse or
injury.
Symptoms :
Early on, pain occurs with overhead activities and lifting your arm to the side.
Activities include brushing hair, reaching for objects on shelves, or playing an
overhead sport.
Pain is more likely in the front of the shoulder and may radiate to the side of the
arm. However, this pain always stops before the elbow. If the pain travels
beyond the arm to the elbow and hand, this may indicate a pinched nerve.
There may also be pain with lowering the shoulder from a raised position.
At first, this pain may be mild and occur only with certain movements of the
arm. Over time, pain may be present at rest or at night, especially when lying on the
affected shoulder. Weakness and loss of motion when raising the arm above your
head. Your shoulder can feel stiff with lifting or movement. It may become more
difficult to place the arm behind your back.
LO.3.>Frozen shoulder, also called adhesive capsulitis, causes pain and stiffness in
the shoulder. Over time, the shoulder becomes very hard to move.
Frozen shoulder occurs in about 2% of the general population. It most commonly
affects people between the ages of 40 and 60, and occurs in women more often than
men.
frozen shoulder, the shoulder capsule thickens and becomes tight. Stiff bands of
tissue called adhesions develop. In many cases, there is less synovial fluid in
the joint.
The hallmark sign of this condition is being unable to move your shoulder - either on
your own or with the help of someone else. It develops in three stages:
1. Freezing, In the"freezing" stage, you
slowly have more and more pain. As
the pain worsens, your shoulder loses
range of motion. Freezing typically
lasts from 6 weeks to 9 months.
2. Frozen, Painful symptoms may
actually improve during this stage, but
the stiffness remains. During the 4 to 6
months of the "frozen" stage, daily
activities may be very difficult.
3. Thawing, Shoulder motion slowly
improves during the "thawing" stage.
Complete return to normal or close to
normal strength and motion typically
takes from 6 months to 2 years.
The causes of frozen shoulder are not fully understood. There is no clear connection
to arm dominance or occupation. A few factors may put you more at risk for
developing frozen shoulder.
Diabetes. Frozen shoulder occurs much more often in people with diabetes, affecting
10% to 20% of these individuals. The reason for this is not known.
Other diseases. Some additional medical problems associated with frozen shoulder
include hypothyroidism, hyperthyroidism, Parkinson's disease, and cardiac disease.
Immobilization. Frozen shoulder can develop after a shoulder has been immobilized
for a period of time due to surgery, a fracture, or other injury. Having patients move
their shoulders soon after injury or surgery is one measure prescribed to prevent
frozen shoulder.
Pain from frozen shoulder is usually dull or aching. It is typically worse early in the
course of the disease and when you move your arm. The pain is usually located over
the outer shoulder area and sometimes the upper arm.
LO.4.> Paraneoplastic syndromes are a group of rare disorders that are triggered by
an abnormal immune system response to a cancerous tumor known as a "neoplasm."
Paraneoplastic syndromes are thought to happen when cancer-fighting antibodies or
white blood cells (known as T cells) mistakenly attack normal cells in the nervous
system. These disorders typically affect middle-aged to older people and are most
common in individuals with lung, ovarian, lymphatic, or breast cancer. Neurologic
symptoms generally develop over a period of days to weeks and usually occur prior to
the tumor being discovered. These symptoms may include difficulty in walking or
swallowing, loss of muscle tone, loss of fine motor coordination, slurred speech,
memory loss, vision problems, sleep disturbances, dementia, seizures, sensory loss in
the limbs, and vertigo or dizziness. Paraneoplastic syndromes include Lambert-Eaton
myasthenic syndrome, stiff-person syndrome, encephalomyelitis, myasthenia gravis,
cerebellar degeneration, limbic or brainstem encephalitis, neuromyotonia, opsoclonus,
and sensory neuropathy.
The pathophysiology of paraneoplastic syndromes is complex and intriguing.
When a tumor arises, the body may produce antibodies to fight it by binding to and
destroying tumor cells. Unfortunately, in some cases, these antibodies cross-react with
normal tissues and destroy them, which may result in a paraneoplastic disorder.[5]
For example, antibodies or T cells directed against the tumor may mistakenly attack
normal nerve cells. The detection of paraneoplastic anti-neural antibody was first
reported in 1965.[6]
In other cases, paraneoplastic syndromes result from the production and release of
physiologically active substances by the tumor. Tumors may produce hormones,
hormone precursors, a variety of enzymes, or cytokines. Several cancers produce
proteins that are physiologically expressed in utero by embryonic and fetal cells but
not expressed by normal adult cells. These substances may serve as tumor markers
(eg, carcinoembryonic antigen [CEA], alpha-fetoprotein [AFP], carbohydrate antigen
19-9 [CA 19-9]). More rarely, the tumor may interfere with normal metabolic
pathways or steroid metabolism. Finally, some paraneoplastic syndromes are
idiopathic.
Paraneoplastic syndromes most commonly occur in patients not known to have
cancer, as well as in those with active cancer and those in remission after treatment. A
complete history and physical examination findings can suggest neoplasia. Persons
with a family history of malignancies (eg, breast,[7, 8] colon) may be at increased risk
and should be screened for cancer. Nonspecific syndromes can precede the clinical
manifestations of the tumor, and this occurrence is a negative prognostic factor.
Because of their complexity and variety, the clinical presentations of these syndromes
may vary greatly. Usually, paraneoplastic syndromes are divided into the following
categories: (1) miscellaneous (nonspecific), (2) rheumatologic, (3) renal, (4)
gastrointestinal, (5) hematologic, (6) cutaneous, (7) endocrine, and (8) neuromuscular.
Miscellaneous (nonspecific)
Fever, dysgeusia, anorexia, and cachexia
are included in this category.
Fever is frequently associated with
lymphomas,[9] acute leukemias,
sarcomas, renal cell carcinomas
(Grawitz tumors), and digestive
malignancies (including the liver).
Rheumatologic
Paraneoplastic arthropathies arise as
rheumatic polyarthritis[10] or
polymyalgia, particularly in patients
with myelomas; lymphomas; acute
leukemia; malignant histiocytosis;
and tumors of the colon, pancreas,
prostate, and CNS.
Hypertrophic osteoarthropathy may be
observed in patients with lung
cancers, pleural mesothelioma, or
phrenic neurilemmoma.
Scleroderma may precede direct evidence
of tumor
The widespread form is typical of
malignancies of the breast,
uterus, and lung (both alveolar
and bronchial forms).
The localized form is characteristic
of carcinoids and of lung
tumors (bronchoalveolar
forms).
Systemic lupus erythematosus (SLE) may
develop in patients with lymphomas
or cancers of the lung, breast, or
gonads.
Secondary amyloidosis of the connective
tissues is a rare presentation in
patients with myeloma, renal
carcinoma, and lymphomas.
Renal
Hypokalemic nephropathy, which is
characterized by urinary potassium
leakage of more than 20 mEq per 24
hours, may develop in patients with
tumors that secrete
adrenocorticotropic hormone
(ACTH) or ACTH-like substances. It
occurs in 50% of individuals with
ACTH-secreting tumors of the lung
(ie, small cell lung cancer[11] ).
Hypokalemia, hyponatremia or
hypernatremia, hyperphosphatemia,
and alkalosis or acidosis may result
from other types of tumors that
produce ACTH, antidiuretic hormone
(ADH), or gut hormones (see
Endocrine and neuromuscular,
below).
Nephrotic syndrome is observed, although
infrequently, in patients who have
Hodgkin lymphoma (HL); non-
Hodgkin lymphoma (NHL);
leukemias; melanomas; or
malignancies of lung, thyroid, colon,
breast, ovary, or pancreatic head.
Secondary amyloidosis of the kidneys,
heart, or CNS may rarely be a
presenting feature in patients with
myeloma, renal carcinoma, or
lymphomas. The clinical picture of
secondary amyloidosis is related to
renal and cardiac injuries.
Gastrointestinal
Watery diarrhea[12] accompanied by an
electrolyte imbalance leads to
asthenia, confusion, and exhaustion.
These problems are typical of patients with
proctosigmoid tumors (both benign
and malignant) and of medullary
thyroid carcinomas (MTCs) that
produce several prostaglandins (PGs;
especially PG E2 and F2) that lead to
malabsorption and, consequently,
unavailability of nutrients.
These alterations also can be observed in
patients with melanomas, myelomas,
ovarian tumors, pineal body tumors,
and lung metastases.
Hematologic
Symptoms related to erythrocytosis or
anemia,[12] thrombocytosis,
disseminated intravascular
coagulation (DIC), and leukemoid
reactions may result from many types
of cancers.
In some cases, symptoms result from
migrating vascular thrombosis (ie,
Trousseau syndrome)[13] occurring
in at least 2 sites.
Leukemoid reactions, characterized by the
presence of immature WBCs in the
bloodstream, are usually
accompanied by hypereosinophilia
and itching. These reactions are
typically observed in patients with
lymphomas or cancers of the lung,
breast, or stomach.
Cryoglobulinemia may occur in patients
with lung cancer or pleural
mesothelioma.
Cutaneous[14]
Itching is the most frequent cutaneous
manifestation in patients with cancer.
Herpes zoster, ichthyosis,[15] flushes,
alopecia, or hypertrichosis also may
be observed.
Acanthosis nigricans and dermic melanosis
are characterized by a blackish
pigmentation of the skin and usually
occur in patients with metastatic
melanomas or pancreatic tumors.
Endocrine
Endocrine symptoms related to
paraneoplastic syndromes usually
resemble the more common
endocrine disorders (eg, Cushing
syndrome). Neuromuscular
symptoms may mimic common
neurological conditions (eg,
dementia).
Cushing syndrome, accompanied by
hypokalemia, very high plasma
ACTH levels, and increased serum
and urine cortisol concentrations, is
the most common example of an
endocrine disorder linked to a
malignancy.[16, 17, 3, 18] This is
related to the ectopic production of
ACTH or ACTH-like molecules from
many tumors (eg, small cell cancer of
the lung).
Neuromuscular
Neuromuscular disorders related to cancers
are now included among the
paraneoplastic syndromes. Such
disorders affect 6% of all patients
with cancer and are prevalent in
ovarian and pulmonary cancers.
Examples include the following:
Myasthenia gravis[19] is the most
common paraneoplastic
syndrome in patients with
thymoma,[20] a malignancy
arising from epithelial cells of
the thymus. Indeed, thymoma
is the underlying cause in
approximately 10% to 15% of
cases of myasthenia
gravis.[21] Rarely,
hypogammaglobulinemia and
pure red cell aplasia occur as
paraneoplastic syndromes in
patients with thymoma.[20]
Lambert-Eaton myasthenic
syndrome (LEMS), which
manifests as asthenia of the
scapular and pelvic girdles
and a reduction of tendon
reflexes. LEMS sometimes
can be accompanied by
xerostomia, sexual impotence,
myopathy, and peripheral
neuropathy. It is associated
with cancer 40-70% of the
time, most commonly small
cell lung cancer (SCLC). It
seems to result from
interference with the release
of acetylcholine due to
immunologic attack against
the presynaptic voltage-gated
calcium channel.
Opsoclonus-myoclonus
syndrome[22] usually affects
children younger than 4 years.
It is associated with
hypotonia, ataxia, and
irritability. One in two
patients has neuroblastoma.
Paraneoplastic limbic
encephalitis[23] is
characterized by depression,
seizures, irritability, and
short-term memory loss. The
neurologic symptoms develop
rapidly and can resesmble
dementia. Paraneoplastic
limbic encephalitis is most
commonly associated with
SCLC.[24]
Paraneoplastic encephalomyelitis is
characterized by a complex of
symptoms derived from
brainstem encephalitis, limbic
encephalitis, cerebellar
degeneration, myelitis, and
autonomic dysfunction. Such
neurologic deficits and signs
seem to be related to an
inflammatory process
involving multiple areas of
the nervous system.
Paraneoplastic cerebellar
degeneration causes gait
difficulties, dizziness, nausea,
and diplopia, followed by
ataxia, dysarthria, and
dysphagia. Paraneoplastic
cerebellar degeneration is
frequently associated with
Hodgkin lymphoma,[25]
breast cancer,[26] SCLC, and
ovarian cancer; it may occur
in association with prostate
carcinoma.[27]
Paraneoplastic sensory neuropathy
affects lower and upper
extremities and is
characterized by progressive
sensory loss, either symmetric
or asymmetric. It seems to be
related to the loss of the
dorsal root ganglia with early
involvement of major fibers
responsible for detecting
vibration and position.
You might also like
- Lebel Contoh PrintDocument1 pageLebel Contoh PrintnoorgianilestariNo ratings yet
- Kahlil Gibran Part ViiDocument1 pageKahlil Gibran Part ViinoorgianilestariNo ratings yet
- Supraventricular TachycardiaDocument37 pagesSupraventricular TachycardianoorgianilestariNo ratings yet
- Proteomic ReportDocument25 pagesProteomic ReportnoorgianilestariNo ratings yet
- ACHMDocument1 pageACHMnoorgianilestariNo ratings yet
- Body Dysmorphic TraynorDocument12 pagesBody Dysmorphic TraynornoorgianilestariNo ratings yet
- Basic Concepts of Fluid and Electrolyte TherapyDocument136 pagesBasic Concepts of Fluid and Electrolyte Therapynoorgianilestari100% (2)
- Medical Disciplinary-Tugas Prof EkaDocument3 pagesMedical Disciplinary-Tugas Prof EkanoorgianilestariNo ratings yet
- Pa To GenesisDocument1 pagePa To GenesisnoorgianilestariNo ratings yet
- Daftar Pustaka Hipertensi, Diabetes dan AsmaDocument2 pagesDaftar Pustaka Hipertensi, Diabetes dan AsmanoorgianilestariNo ratings yet
- Van Den Berghe G, Wouters P, Weekers F, Et Al. Intensive Insulin Therapy in Critically Ill Patients. N Engl J Med 345: 1359-1367, 2001Document1 pageVan Den Berghe G, Wouters P, Weekers F, Et Al. Intensive Insulin Therapy in Critically Ill Patients. N Engl J Med 345: 1359-1367, 2001noorgianilestariNo ratings yet
- Van Den Berghe G, Wouters P, Weekers F, Et Al. Intensive Insulin Therapy in Critically Ill Patients. N Engl J Med 345: 1359-1367, 2001Document1 pageVan Den Berghe G, Wouters P, Weekers F, Et Al. Intensive Insulin Therapy in Critically Ill Patients. N Engl J Med 345: 1359-1367, 2001noorgianilestariNo ratings yet
- Family Medicine Residents Orthopedic Rotation HandoutDocument18 pagesFamily Medicine Residents Orthopedic Rotation HandoutRuth PoeryNo ratings yet
- Blood TransfusionDocument30 pagesBlood TransfusionnoorgianilestariNo ratings yet
- Jadwal Koas IPDDocument11 pagesJadwal Koas IPDnoorgianilestariNo ratings yet
- Diagnosis MeningitisDocument25 pagesDiagnosis MeningitisnoorgianilestariNo ratings yet
- Hasil UrinalysisDocument1 pageHasil UrinalysisnoorgianilestariNo ratings yet
- Visum et repertum report 1 October 2014Document4 pagesVisum et repertum report 1 October 2014noorgianilestariNo ratings yet
- Otitis Media AkutDocument9 pagesOtitis Media AkutnoorgianilestariNo ratings yet
- Frozen ShoulderDocument14 pagesFrozen ShouldernoorgianilestariNo ratings yet
- WEEK Orthopedics DR JohnDocument16 pagesWEEK Orthopedics DR JohnnoorgianilestariNo ratings yet
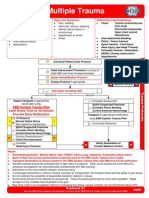
- Multiple Trauma: EMS System Trauma Plan Limit Scene Time To 10 Minutes Provide Early NotificationDocument1 pageMultiple Trauma: EMS System Trauma Plan Limit Scene Time To 10 Minutes Provide Early NotificationKelly JacksonNo ratings yet
- CiminoDocument2 pagesCiminonoorgianilestariNo ratings yet
- Diagnosis MeningitisDocument25 pagesDiagnosis MeningitisnoorgianilestariNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5784)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Flight Instructor Patter Ex17Document1 pageFlight Instructor Patter Ex17s ramanNo ratings yet
- Pub - Perspectives On Global Cultures Issues in Cultural PDFDocument190 pagesPub - Perspectives On Global Cultures Issues in Cultural PDFCherlyn Jane Ventura TuliaoNo ratings yet
- Agitators: Robert L. Bates, President Chemineer, IncDocument24 pagesAgitators: Robert L. Bates, President Chemineer, InctenshinomiyukiNo ratings yet
- Footprints 080311 For All Basic IcsDocument18 pagesFootprints 080311 For All Basic IcsAmit PujarNo ratings yet
- WP1019 CharterDocument5 pagesWP1019 CharternocnexNo ratings yet
- Soil Testing Lab Results SummaryDocument2 pagesSoil Testing Lab Results SummaryMd SohagNo ratings yet
- 2022 - J - Chir - Nastase Managementul Neoplaziilor Pancreatice PapilareDocument8 pages2022 - J - Chir - Nastase Managementul Neoplaziilor Pancreatice PapilarecorinaNo ratings yet
- Graphs & Charts SummariesDocument20 pagesGraphs & Charts SummariesMaj Ma Salvador-Bandiola100% (1)
- Community Development A Critical Approach PDFDocument2 pagesCommunity Development A Critical Approach PDFNatasha50% (2)
- All Types of Switch CommandsDocument11 pagesAll Types of Switch CommandsKunal SahooNo ratings yet
- Vsip - Info - Ga16de Ecu Pinout PDF FreeDocument4 pagesVsip - Info - Ga16de Ecu Pinout PDF FreeCameron VeldmanNo ratings yet
- RFID Receiver Antenna Project For 13.56 MHZ BandDocument5 pagesRFID Receiver Antenna Project For 13.56 MHZ BandJay KhandharNo ratings yet
- Jiangsu Changjiang Electronics Technology Co., Ltd. SOT-89-3L Transistor SpecificationsDocument2 pagesJiangsu Changjiang Electronics Technology Co., Ltd. SOT-89-3L Transistor SpecificationsIsrael AldabaNo ratings yet
- Monetary System 1Document6 pagesMonetary System 1priyankabgNo ratings yet
- MATH6113 - PPT5 - W5 - R0 - Applications of IntegralsDocument58 pagesMATH6113 - PPT5 - W5 - R0 - Applications of IntegralsYudho KusumoNo ratings yet
- The Power of Networking for Entrepreneurs and Founding TeamsDocument28 pagesThe Power of Networking for Entrepreneurs and Founding TeamsAngela FigueroaNo ratings yet
- Fire Pump System Test ReportDocument12 pagesFire Pump System Test Reportcoolsummer1112143100% (2)
- GEd 105 Midterm ReviewerDocument17 pagesGEd 105 Midterm ReviewerAndryl MedallionNo ratings yet
- Classification of MatterDocument2 pagesClassification of Matterapi-280247238No ratings yet
- English ProjectDocument10 pagesEnglish ProjectHarshman Singh HarshmanNo ratings yet
- Pankaj Screener 10 Oct 2014Document127 pagesPankaj Screener 10 Oct 2014Sadul Singh Naruka100% (1)
- Ethics Book of TAMIL NADU HSC 11th Standard Tamil MediumDocument140 pagesEthics Book of TAMIL NADU HSC 11th Standard Tamil MediumkumardjayaNo ratings yet
- Chapter 1 - The Empirical Beginnings and Basic Contents of Educational PsychologyDocument9 pagesChapter 1 - The Empirical Beginnings and Basic Contents of Educational PsychologyJoshua Almuete71% (7)
- Unit 01 Family Life Lesson 1 Getting Started - 2Document39 pagesUnit 01 Family Life Lesson 1 Getting Started - 2Minh Đức NghiêmNo ratings yet
- Hearing God Through Biblical Meditation - 1 PDFDocument20 pagesHearing God Through Biblical Meditation - 1 PDFAlexander PeñaNo ratings yet
- LAU Paleoart Workbook - 2023Document16 pagesLAU Paleoart Workbook - 2023samuelaguilar990No ratings yet
- Escalado / PLC - 1 (CPU 1214C AC/DC/Rly) / Program BlocksDocument2 pagesEscalado / PLC - 1 (CPU 1214C AC/DC/Rly) / Program BlocksSegundo Angel Vasquez HuamanNo ratings yet
- "The Meeting of Meditative Disciplines and Western Psychology" Roger Walsh Shauna L. ShapiroDocument13 pages"The Meeting of Meditative Disciplines and Western Psychology" Roger Walsh Shauna L. ShapiroSayako87No ratings yet
- Clinnic Panel Penag 2014Document8 pagesClinnic Panel Penag 2014Cikgu Mohd NoorNo ratings yet
- AWS S3 Interview QuestionsDocument4 pagesAWS S3 Interview QuestionsHarsha KasireddyNo ratings yet