Professional Documents
Culture Documents
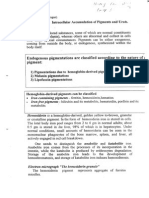
Water Dysbalance. Edema
Uploaded by
Ivan YeohCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Water Dysbalance. Edema
Uploaded by
Ivan YeohCopyright:
Available Formats
Water Dysbalance. Edema.
Case 1 (N 57)
Examination of a 32-year-old patient revealed various signs of pathology,
including excessive body mass: his height is 168 cm, and weight 84.5 kg. The
patient also has a pasty face, periorbital puffiness, pale skin; he had slow
rebound of tissue to its original contour after pressing the feet or shin with the
fingertip. The patient told the physician about tightness of a ring and shoes in
the evening. An investigation of the cardiovascular system revealed the
following: minor arterial hypotension, areas of cardiac dullness are slightly
increased; other parameters are unremarkable. The daily urine volume is
within the normal range.
Questions:
1. What is the possible cause of the patient's excess of body mass?
2. Define the type of pathological process associated with an increase in body
mass in this patient?
3. Explain the mechanisms of development of this pathological process.
Answers:
1. In general there are 2 variants of increase in body mass:
a. Obesity (can be excluded)
b. Accumulation of water (because of signs of generalized edema)
2. Overhydration (water accumulation). Type: Iso osmolar.
3. Cause:
Signs of cardiac insufficiency like:
- increase in cardiac dullness (due to hypertrophy of ventricles
or dilation)
- decrease systemic BP
- In this case is chronic cardiac insufficiency, since chronic is
characterized by generalized edema (In acute cases, it is
not).
- It is also uncompensated at this moment because it is
characterized by generalized edema and decrease in BP.
Mechanisms:
- First this mechanism is associate with compensative
reactions or adaptive reactions
- To increase cardiac function, the body activates
antinatriuretic mechanisms to increase circulatory plasma
volume
- Because, decrease in cardiac output, leads to insufficiency of
kidneys as a result of the general decrease in effective
arterial volume (volume of blood that is necessary to perfuse
all tissues and organs)
- And so, decrease effective arterial volume ! compensation
(increase in diastolic volume). This may be achieved by
sodium retention and accumulation of water.
- Mechanisms of sodium retention are activated through
increase in Renin-Angiotensin-Aldosterone System.
- Also, proximal sodium reabsorption may be also increase in
more severe cases of cardiac insufficiency.
So, chronic cardiac insufficiency first starts with osmotic edema.
But with its progression and loss of contractile function, the start
may be insufficient to remove blood from the lower parts of the
body especially during the night by evening hours with
accumulation of fatigue. And so, one more mechanism is
hemodynamic edema (first was osmotic, now is hemodynamic).
It is uncompensated cardiac insufficiency, so it has 2
mechanisms at the same time: osmotic and hemodynamic.
" With further progression of cardiac insufficiency after several
years, persistent congestion of venous vessels ! dystrophy
of organs especially liver (because it is a metabolically active
organ which requires a large amount of oxygen) ! cirrhosis
! development of ascites ! loss of liver function with poor
synthesis of albumin [In this case more mechanism of edema
which is oncotic]
Case 2
A 40-year-old patient L. was admitted to the therapeutic department of
hospital. On examination: his face is pale and puffy, eyelids are swollen,
applying pressure to a rear aspect of the sole results in indentations that
persist for some time. Over the last two weeks the patients body weight
increased by 6 kg. L.s blood pressure is decreased, areas of the heart
dullness are increased. The patients daily urine volume is close to the lower
boundary of the normal values. Urine test: massive proteinuria (>4 g protein
per day), large amount of hyaline and waxy casts, increased level of
aldosterone in the daily urine. Blood test: hypoproteinemia, albumin/globulin
ratio is decreased, moderate hypernatremia. Pathological changes in the
gastrointestinal tract or liver are not found.
Questions:
1. What type of dyshydria developed in the patient and what variety of it:
hyper-, hypo- or isoosmolar?
2. Explain the cause and pathogenesis of dyshydria in this patient.
3. What syndrome does the patient suffer from?
Answers:
1. Overhydration (due to generalized edema in the body). From blood
test: there is hypernatremia, and since sodium is main osmolarity
substance that contributes largely to the total osmolarity, hypenatremia
leads to hyperosmolarity. Maybe if later drink more water, it may
become isoosmolar, but for now is hyperosmolar.
2. Can see changes in content of urine (large amount of protein and
casts) ! pathology of kidneys. Furthermore changes in blood:
decrease albumin concentration and albumin/globulin ratio. So,
diagnosis is nephrotic syndrome (Its not just renal insufficiency)
because protein losses are more than 4g daily, its a very high loss,
that liver is unable to compensate by increase in protein synthesis and
there is hypoproteinemia. So in this case, it is renal nephrotic edema.
The main mechanism of renal nephrotic edema is oncotic mechanism.
But at the same time there is hypernatremia, because it may be with
some osmotic component. Water is retained in the tissues ! less in
the lumens of the vessel ! decrease in the circulatory plasma volume
! activates Renin Angiotensin Aldosterone System ! starts to retain
sodium ! hypernatremia. (Osmotic mechanisms may also occur but
may be at some delay.)
Other factors of edema:
Pericardiac factors (same symptoms as Case 1). There are
signs of chronic cardiac insufficiency.
*So, it may be a combination of 2 types of edema: cardiac and
nephrotic.
3. Nephrotic syndrome.
Case 3 (N 59)
A 22-year-old patient who recovered from severe scarlet fever 2 weeks
ago complains of headache, pain in the back, dyspnea, and palpitations.
During the last week she has increased her body weight by 11.5 kg. On
examination: her face is pale; she has periorbital puffiness, and edema of
the shins and feet; the boundaries of the heart dullness are increased;
blood pressure is 180/100 mm Hg; daily urine volume is reduced. Urine
tests show the presence of erythrocytes, leukocytes, protein and granular
casts. An increased titer of the antistreptococcal antibodies (antistreptolysin
O) is found in the blood.
Questions:
1. Is there evidence of the kidney pathology in this patient? What is the
possible cause of this pathology?
2. What is the cause of hyperhydration in this case: a decrease in water
excretion by the kidneys or an activation of the water-retention
mechanisms?
3. Explain the mechanisms of edema in this patient.
Answers:
1. Yes. Signs: Change in the volume of urine, change in components of
urine. It is acute inflammatory pathology of the kidneys. It develops
acutely and the urine contains blood, erythrocytes and lymphocytes
(sign of acute inflammation). So we call this pathology nephritis, in this
case, glomerular nephritis because glomeruli are definitely affected.
So, this pathology is associated with infection. Disorder
developed after the infection. So its not the direct effect of
streptococcus on kidney parenchyma. It is the aftermath of the
infection.
Mechanism of disorder is associate with immunity against the
infection, called acute post-streptococcal glomerular nephritis.
Because streptococci do not cause diffuse injury to parenchyma.
They may cause abscesses during septicemia (but there are no
signs of septicemia). So, the mechanism of pathology in this
case is production of antibodies against the streptococcus and
not any streptococcus can cause the disorder, only some
specific strains i.e beta hemolytic of M group, because the
superficial antigens of this strain of streptococcus resemble
antigens of glomerular basement membrane in some individuals
and so antibodies produced against antigens of the
streptococcus may cross react with the basement membrane.
When they react, they bind complement and activate it and
starts the inflammation of the glomeruli.
Type of edema: Nephritic edema.
2. Both of these mechanisms can operate.
Decrease excretion is the result of decrease in glomerular
filtration rate (poor filtration of blood). This is due to the
disturbance of blood flow through the glomeruli, probably
because of some obstruction. Inflammation had caused
activation of the clotting system and thus clots may obstruct the
capillaries of the glomeruli. So, switching off some nephrons
from filtration process. At the same time, the inflammation may
activate Renin Angiotensin Aldosterone System and initiate
retention of sodium and then water.
Type of edema: Osmotic (by its mechanism)
3. See both Q1 & Q2.
Case 4 (N 60)
A 7-year-old boy developed a progressive swelling of the soft palate with
a swallowing difficulty, and then asphyxia after he had drunk mango juice.
The mucosal membrane in the swelled area is hyperemic without
tenderness; a moderate increase in eosinophils is seen in the blood. The
patient's body temperature is normal. His senior sister suffers from attacks of
bronchial asthma.
Questions:
1. Is edema in this case the result of ordinary inflammation?
2. What is the cause of edema in this patient?
3. Explain the pathogenesis of the given pathology.
4. Does this type of edema lead to life-threatening condition?
Answers:
1. Allergic reaction. Not just ordinary inflammation but also allergic
reaction. Difference between allergic inflammation and non-allergic
inflammation (for example caused by infection):
Ordinary inflammation has the first stage that is alteration
(destruction of tissue). Allergic inflammation especially allergic of
the 1
st
type has no destruction of tissue. It is not injury that
initiates inflammatory process. It starts with the release of
mediators. In ordinary inflammation, it starts with injury then
release of mediators.
2. Causes of edema:
Mediators that increase permeability.
3. So by mechanism, this edema is membranogenic edema. It leads to
exit of plasma proteins in the surrounding tissue and accumulation of
water.
4. Yes. Emergency state especially in children. Because swelling of the
soft tissues of throat and trachea leads to complete obstruction of the
upper airways. So sometimes there is a necessity to cut trachea and
insert a tube for breathing.
Case 5
A 50-year-old male patient visited his physician with complaints about
rapid gaining of body weight and edema of the feet. His usual body weight of
about 70kg recently increased to 110kg. The medical history of the patient
includes a long period of alcohol abuse. On examination: blood pressure is
110/70 mmHg; the skin has signs of the dilated capillaries on the torso (spider
angiomata) and hands (palmar erythema). Evaluation of the respiratory and
cardiovascular systems reveals no pathological changes. The abdomen of the
patient is significantly distended; on percussion, the region of dullness is
shifting when the patient is turned from supine position to side-lying (shifting
dullness). Lower extremities are swollen. There are signs of testicular atrophy.
Blood test results: glucose 4.44 mmol/L, total plasma protein 53 g/L (N:
68-81 g/L), albumin 20 g/L (N:35-53 g/L).
Questions:
1. What forms of pathology can be diagnosed in this patient?
2. What is the etiology and pathogenesis of these forms of pathology in
the patient?
3. Define the pattern of water-mineral dysbalance in this patient. What is
the cause of this dysbalance?
Answers:
1. Hepatic insufficiency due to cirrhosis. Patient has signs of cirrhosis:
portal hypertension ! ascites (significant sign of portal hypertension is
ascites). Ascites in this case is manifested as excessive distention of
the abdomen and shifting dullness, because of free water that may
move inside the abdominal cavity.
Cause of cirrhosis: alcoholic.
2. Etiology & pathogenesis:
First, starts as hemodynamic, because of high pressure in portal
vein.
Then with liver insufficiency, it becomes oncotic.
3. In general the pattern of water-mineral dysbalance in this patient is
overhydration.
Case 6
A 25-year-old patient who suffered from diabetes mellitus was admitted
to hospital with complaints of episodes of syncope. He used propranolol
(beta-adrenoblocker) to treat his arterial hypertension. The physician of the
admission ward took a sample of the patients blood to make an electrolyte
analysis. Having assumed that the patient had low blood glucose levels the
physician injected him 20ml of the 50% glucose solution. Soon after the
injection of glucose the patient developed collapse and cardiac arrest.
Repeated administration of the blood electrolyte concentration showed:
On admission After injection of glucose Normal values
Na+ 130 mmol/L 129 mmol/L 135-156 mmol/L
Cl- 90 mmol/L 91 mmol/L 95-105 mmol/L
K+ 6.5 mmol/L 8.5 mmol/L 3.5-5.3 mmol/L
HCO3- 10 mmol/L 11 mmol/L 24-32 mmol/L
Glucose 400 mg/dl 600 mg/dl 65-110 mg/dl
Questions:
1. What disorders of electrolyte balance are found in the patient on
admission? Explain their causes.
2. What disorders of electrolyte balance are found in the patient after
injection of glucose? Explain their causes.
3. Explain the development of cardiac arrest in this patient.
Answers:
1. High concentration (increase) of potassium on admission. Cause:
Lack of insulin because the normal effect of insulin is increase in
transport of potassium inside the cell. If insulin is deficient, more
potassium remains in external environment. Moreover, use of
propranolol may exacerbate this hyperkalaemia because beta-
adrenoblockers prevent active transport of potassium inside the
cell.
2. There is more hyperkalaemia after injection of glucose (more severe).
Cause:
Increase in glucose concentration leads to increase osmolarity.
Because in diabetes mellitus patient, glucose is osmolatically
active agent. It is not the case in normal individuals. If in normal
individuals, glucose will be consumed by the cells and will not
increase the osmolarity of blood.
When osmolarity of plasma is increased, water with dissolved
solutions (potassium in this case) exit from the cell into the
interstitial media and plasma ! hyperkalaemia.
Because osmolarity draws water from inside the cell. If
osmolarity of media outside is higher than inside, water is drawn
out.
3. Cause of cardiac arrest:
Potassium. Concentration of 8.5 mmol/L is already fatal.
Not because of calcium.
Due to depolarization of cardiomyocytes, especially cells of the
conducting system.
Because resting potential is formed by exit of potassium from
inside the cell (outflow of potassium). Actually, there is balance
between inflow of sodium and outflow of potassium. So the
internal surface potential is negative. Thats why resting
potential inside the cell is negative. If current of potassium is
disturbed (decreased), there is accumulation of positive charge
and depolarization.
But with high concentration of potassium, the gradient is
decreased and so slowing of outflow potassium current and this
causes relative accumulation of positive charge inside the cell
and depolarization. Partially depolarized cells are unable to
conduct impulses, cant develop action potential ! heart stop
because of blockade of conduction.
Blockade: stop of propagation of impulses in the heart; due to
partial depolarization of the cells.
Action potential is produced due to opening of fast sodium
channels. With partial depolarization, fast sodium channels are
closed.
Case 7
A 75-year-old female patient was transported to hospital by ambulance that
was called by a health visitor who was used to regularly visit the patient. The
nurse reported to the physician that the patient lived alone and during the last
week suffered from fever and cough. On examination: the patient is confused,
responds slowly to questions; her skin and visible mucous membranes are
dry, turgor of the skin and eyeball is notably decreased. Body temperature is
37.5 degrees, blood pressure 100/60 mmHg (according to the nurse her
usual BP is 150/95 mmHg), heart rate 120 beats/min, breathing rate
20/min. electrolytes of the blood plasema: Na+ = 160 mmol/L (N: 135-156
mmol/L), K+ -5.9 mmol/L (N:3.5-5.3 mmol/L), Cl- 82 mmol/L (N:95-105
mmol/L), HCO3- 25 mmol/L (N:24-32 mmol/L)
Questions:
1. What forms of dyshydria developed in the patient? What is its likely
cause?
2. What changes in the volume and osmolarity of the intracellular
compartment, interstitial fluid, and extracellular compartment are typical
in this type of dyshydria?
3. What other pathological conditions are accompanied by this type of
dyshydria?
4. What solution of NaCl (hypo-, hyper-, or isoosmolar) is recommended
for infusion to this patient to normalize her water-electrolyte balance?
Answers:
1. Dehydration. Clinical signs: dryness, loss of turgor, decrease BP,
tachycardia.
2. Intracellular compartment becomes less, it losses water. Interstitial
fluid: osmolarity is increased while volume is decreased. Extracellular
compartment is decreased.
3. Water starvation. Hyperosmolar dehydration. Patient lived alone and
probably develops an infectious disease and so was lying on the bed
most of the day ! drink less water than required (accompanied by
more water loss due to fever). After several days, develop dehydration.
4. Isoosmolar. But infused slowly, because of great risk of brain edema.
Even if you start to infuse hyperosmolar solution to decrease
concentration of sodium, osmolarity of the intercellular
compartment in the brain may occur higher than osmolarity of
plasma because brain during slow development of
hyperosmolarity develops their own adaptive mechanisms to
prevent water loss. It tries to increase osmolarity by
accumulation of substances like amino acids, myoinositol and
other substances to increase osmolarity.
When start infusion of isoosmolar (or especially hyperosmolar),
the osmolarity of intercellular compartment may occur higher
than extracellular and water may start to enter the cells in
excess and increase the volume of the brain.
So normally there should be infusion of isoosmolar solutions for
one period of time (eg 2 days) but not just several litres at once.
You might also like
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsNo ratings yet
- Hepatic Encephalopathy: Causes, Tests, and Treatment OptionsFrom EverandHepatic Encephalopathy: Causes, Tests, and Treatment OptionsRating: 3.5 out of 5 stars3.5/5 (2)
- ANS (Glenn) 2005 Final-No. 3Document13 pagesANS (Glenn) 2005 Final-No. 3Bryan RzldNo ratings yet
- Pleno Minggu 2 Blok 3.4Document84 pagesPleno Minggu 2 Blok 3.4Devi Yunita PurbaNo ratings yet
- Case Study On Acute GlomerulonephritisDocument3 pagesCase Study On Acute GlomerulonephritisDalene Erika GarbinNo ratings yet
- Seminar On Shock c2Document65 pagesSeminar On Shock c2mubarak abdulkadirNo ratings yet
- ShockDocument25 pagesShockAvneet Maan100% (1)
- Acute Glomerulonephritis (AGN) : Group A Beta Hemolytic StretococcusDocument3 pagesAcute Glomerulonephritis (AGN) : Group A Beta Hemolytic StretococcusKristine Danielle DejeloNo ratings yet
- SESSION 3 - PATHOPHYSIOLOGY With AnswersDocument9 pagesSESSION 3 - PATHOPHYSIOLOGY With AnswersSpeed SamNo ratings yet
- Fluids, electrolytes and acid-base balanceDocument13 pagesFluids, electrolytes and acid-base balanceMansoor TariqNo ratings yet
- Dentistry L5 SHOCKDocument20 pagesDentistry L5 SHOCKHadeer WasfyNo ratings yet
- Leg 5 Renal DisordersDocument82 pagesLeg 5 Renal DisordersAleli DoNo ratings yet
- Imed Case 2 - Group 9Document7 pagesImed Case 2 - Group 9Razeen RiyasatNo ratings yet
- 316 CTDocument6 pages316 CTkvvalencia2128valNo ratings yet
- Shock: Gastrointestinal Surgical Department of Affiliated Hospital of Jining Medical CollegeDocument52 pagesShock: Gastrointestinal Surgical Department of Affiliated Hospital of Jining Medical Collegesanjivdas100% (1)
- Critical Care Nursing Guide to Shock and Multi-Organ DysfunctionDocument63 pagesCritical Care Nursing Guide to Shock and Multi-Organ DysfunctiontikoNo ratings yet
- Shock: DR Uwanuruochi KelechukwuDocument35 pagesShock: DR Uwanuruochi KelechukwuJake MillerNo ratings yet
- Disorders of The PulpDocument7 pagesDisorders of The Pulpابو الجودNo ratings yet
- ABC Lecture NotesDocument7 pagesABC Lecture NotesLady Shayne YapNo ratings yet
- HTTPDocument10 pagesHTTPkasmiatiNo ratings yet
- Understanding Glomerulonephritis: Its Causes, Symptoms, Diagnosis and TreatmentDocument5 pagesUnderstanding Glomerulonephritis: Its Causes, Symptoms, Diagnosis and TreatmentPooja ChapdiNo ratings yet
- Kel 7Document13 pagesKel 7hananNo ratings yet
- Pediatric Renal DisordersDocument9 pagesPediatric Renal DisordersNadia AmroNo ratings yet
- Hypovolemic Shock 09Document58 pagesHypovolemic Shock 09Joanne Bernadette Aguilar100% (2)
- Skenario Ii - Hematuria - Blok 10Document5 pagesSkenario Ii - Hematuria - Blok 10Yoga YudhistiraNo ratings yet
- Lascano, Joanne Alyssa - RheumatologyDocument13 pagesLascano, Joanne Alyssa - RheumatologyJoanne Alyssa Hernandez LascanoNo ratings yet
- PH Protocol For Nephrotic SyndromeDocument4 pagesPH Protocol For Nephrotic Syndromeprachi100% (1)
- Surgery: by DR - Mohammad Z. Abu Sheikha@Document145 pagesSurgery: by DR - Mohammad Z. Abu Sheikha@صقر حورانNo ratings yet
- Nephrotic Syndrome Msn-3Document12 pagesNephrotic Syndrome Msn-3Bibi Renu100% (3)
- Fifth Problem - LouisDocument99 pagesFifth Problem - LouisRioNo ratings yet
- Metabolic & Acid-Base Balance: 1-When Lactic Acid Accumulates, Body Will Respond byDocument8 pagesMetabolic & Acid-Base Balance: 1-When Lactic Acid Accumulates, Body Will Respond byASGHAR ALINo ratings yet
- PBL6Document111 pagesPBL6Sofea IzyanNo ratings yet
- Hepatic Encephalopathy and ComaDocument4 pagesHepatic Encephalopathy and ComaAriana ValenciaNo ratings yet
- Shock Shock: DR Budi Enoch SPPDDocument31 pagesShock Shock: DR Budi Enoch SPPDRoby KieranNo ratings yet
- Individual Assignment Complex Medical Surgery Nursing Care With SepsisDocument6 pagesIndividual Assignment Complex Medical Surgery Nursing Care With Sepsisdea lestariNo ratings yet
- 01 Renal System NotesDocument22 pages01 Renal System NotesLexanCantorFermoNo ratings yet
- ShockDocument30 pagesShockAl QasimNo ratings yet
- Wa0002 PDFDocument4 pagesWa0002 PDFVivin KarlinaNo ratings yet
- Acute Glomerulonep Hritis: By: Edelrose D. Lapitan BSN Iii-CDocument29 pagesAcute Glomerulonep Hritis: By: Edelrose D. Lapitan BSN Iii-CEdelrose Lapitan100% (1)
- Acute Glomerulonephritis (Agn)Document42 pagesAcute Glomerulonephritis (Agn)Rowshon AraNo ratings yet
- Sodium, and 350-500 Meq/L of Chloride. The Combined Effects of Serum Hyperosmolarity, Dehydration, and Acidosis Result in Increased Osmolarity in Brain Cells That ClinicallyDocument5 pagesSodium, and 350-500 Meq/L of Chloride. The Combined Effects of Serum Hyperosmolarity, Dehydration, and Acidosis Result in Increased Osmolarity in Brain Cells That ClinicallyMorgan Mitchell100% (10)
- Septic ShockDocument23 pagesSeptic ShockErica May Formacion SeverinoNo ratings yet
- Definition, Causes, Types and Management of ShockDocument7 pagesDefinition, Causes, Types and Management of ShockShaker MUhammedNo ratings yet
- Standforf 16 ShockDocument8 pagesStandforf 16 ShockamutiarNo ratings yet
- Approach To ShockDocument40 pagesApproach To ShockDivesh NaiduNo ratings yet
- Pathophysiology and Etiology of Edema - IDocument9 pagesPathophysiology and Etiology of Edema - IBrandy MaddoxNo ratings yet
- Nephrotic SyndromeDocument5 pagesNephrotic SyndromeAnjhiene CambaNo ratings yet
- SepsisDocument3 pagesSepsissivaNo ratings yet
- Acute Renal Failure Nursing Care and ManagementDocument7 pagesAcute Renal Failure Nursing Care and ManagementMichelle MallareNo ratings yet
- CBL HypertensionDocument23 pagesCBL HypertensionWan AswanNo ratings yet
- GN causes blood and protein in urineDocument14 pagesGN causes blood and protein in urineエド パジャロンNo ratings yet
- Nephritis: Presented byDocument32 pagesNephritis: Presented byPavan SorathiyaNo ratings yet
- ShockDocument20 pagesShockعبدالواسع الاهنوميNo ratings yet
- NS2881 Renal Revision Worksheet 2022Document10 pagesNS2881 Renal Revision Worksheet 2022Louise GeislerNo ratings yet
- ASPGNDocument17 pagesASPGNAdLi DLi DLiNo ratings yet
- Nephritis by Triveni SidhaDocument23 pagesNephritis by Triveni SidhaTriveni SidhaNo ratings yet
- Infectious Disease ReviewDocument12 pagesInfectious Disease ReviewjyothiNo ratings yet
- Acute Glomerulonephritis Poststreptococcal NCLEX ReviewDocument4 pagesAcute Glomerulonephritis Poststreptococcal NCLEX ReviewJhean MeansNo ratings yet
- Ascites, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandAscites, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- Hepatorenal Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHepatorenal Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- The List of EquipmentDocument1 pageThe List of EquipmentIvan YeohNo ratings yet
- Anatomy and Physiology of The Valves of The Heart: 1) Tricuspid ValveDocument17 pagesAnatomy and Physiology of The Valves of The Heart: 1) Tricuspid ValveIvan YeohNo ratings yet
- Disorders of The Tissue GrowthDocument5 pagesDisorders of The Tissue GrowthIvan YeohNo ratings yet
- Acid Base DisordersDocument3 pagesAcid Base DisordersIvan YeohNo ratings yet
- HepatitisDocument4 pagesHepatitisIvan YeohNo ratings yet
- Surg MCQDocument58 pagesSurg MCQIvan YeohNo ratings yet
- Water Dysbalance. Edema. Case 1-4 AnalysisDocument8 pagesWater Dysbalance. Edema. Case 1-4 AnalysisIvan YeohNo ratings yet
- HypoxiaDocument3 pagesHypoxiaIvan YeohNo ratings yet
- Collected PathPhys Situations 2010Document148 pagesCollected PathPhys Situations 2010Muhammad Ashraf Ahmad50% (2)
- Patho NoteDocument99 pagesPatho NoteIvan YeohNo ratings yet
- Postpartum Infectious DiseaseDocument2 pagesPostpartum Infectious DiseaseIvan YeohNo ratings yet
- Ischemic Stroke TopicsDocument12 pagesIschemic Stroke TopicsIvan YeohNo ratings yet
- Infectious Diseases of the Nervous SystemDocument8 pagesInfectious Diseases of the Nervous SystemIvan YeohNo ratings yet
- Patho NoteDocument99 pagesPatho NoteIvan YeohNo ratings yet
- Dell ComputerDocument3 pagesDell ComputerIvan YeohNo ratings yet
- (Oncologysurgery) Graeme J Poston, Michael DAngelica, Rene ADAM - Surgical Management of Hepatobiliary and Pancreatic Di 1Document630 pages(Oncologysurgery) Graeme J Poston, Michael DAngelica, Rene ADAM - Surgical Management of Hepatobiliary and Pancreatic Di 1Marlene MartínezNo ratings yet
- Nutritional assessment pregnancy lactationDocument11 pagesNutritional assessment pregnancy lactationKathleen Martinez100% (1)
- Porose Gravidez e Puerperio 2021Document15 pagesPorose Gravidez e Puerperio 2021Ben-Hur AlbergariaNo ratings yet
- Toxins: Use of Botulinum Toxin in Orofacial Clinical PracticeDocument16 pagesToxins: Use of Botulinum Toxin in Orofacial Clinical PracticeAfiliado LendárioNo ratings yet
- Glossary of EMTDocument5 pagesGlossary of EMTErnan BaldomeroNo ratings yet
- Appendicitis and Crohn's Disease GuideDocument11 pagesAppendicitis and Crohn's Disease GuideJa DimasNo ratings yet
- NAC - Allergic Rhinitis Treatments Chart - 2020Document1 pageNAC - Allergic Rhinitis Treatments Chart - 2020adham bani younesNo ratings yet
- Barrier Free ArchitectureDocument3 pagesBarrier Free ArchitectureAmarjit SahNo ratings yet
- Peds Shelf NotesDocument88 pagesPeds Shelf Notesskeebs23100% (8)
- Nephrotic/Nephritic Syndrome: AK. Soyibo Department of Medicine Review ClassDocument143 pagesNephrotic/Nephritic Syndrome: AK. Soyibo Department of Medicine Review ClassKay BristolNo ratings yet
- Manila Tytana CollegesDocument1 pageManila Tytana CollegesSkyeNo ratings yet
- Combination of Lisinopril and Nifedipine GITS.10Document7 pagesCombination of Lisinopril and Nifedipine GITS.10Andi PermanaNo ratings yet
- NCMB316 Rle 2-10-7addison's DiseaseDocument4 pagesNCMB316 Rle 2-10-7addison's DiseaseMaica LectanaNo ratings yet
- ACE2 Expression in Kidney and Testis May Cause Kidney and Testis Damage After 2019-nCoV InfectionDocument16 pagesACE2 Expression in Kidney and Testis May Cause Kidney and Testis Damage After 2019-nCoV InfectionSY LodhiNo ratings yet
- Perinatal Factor Journal PediatricDocument8 pagesPerinatal Factor Journal PediatricHasya KinasihNo ratings yet
- Biochemistry Importance for NursesDocument15 pagesBiochemistry Importance for NursesJulius Memeg PanayoNo ratings yet
- (Lecture) Approach To AscitesDocument48 pages(Lecture) Approach To AscitesJirayu Puthhai100% (1)
- HYPETHYROIDISM NURSING CARE PLANDocument6 pagesHYPETHYROIDISM NURSING CARE PLANTrisha Joyce MadriagaNo ratings yet
- Autism AlarmDocument2 pagesAutism AlarmUmair KaziNo ratings yet
- PLE 2019 - Medicine Questions and Answer KeyDocument24 pagesPLE 2019 - Medicine Questions and Answer KeydicksonNo ratings yet
- Artificial MethodsDocument23 pagesArtificial MethodsJanna Broqueza RodriguezNo ratings yet
- Smriti Mishra BCG NCCDocument1 pageSmriti Mishra BCG NCCashish bondiaNo ratings yet
- Androgenetic Alopecia and Current Methods of TreatmentDocument4 pagesAndrogenetic Alopecia and Current Methods of TreatmentPamela TrujilloNo ratings yet
- Classifications of Pharmaceutical Drugs1Document24 pagesClassifications of Pharmaceutical Drugs1RPh Krishna Chandra JagritNo ratings yet
- Science: Quarter 2 - Module 1Document20 pagesScience: Quarter 2 - Module 1Kate BatacNo ratings yet
- SOP 6-Minute-Walk Test 1. General Considerations: 6-Minute Walking Distance: Covered Distance inDocument5 pagesSOP 6-Minute-Walk Test 1. General Considerations: 6-Minute Walking Distance: Covered Distance inadeNo ratings yet
- Hormone Levels For Fertility Patients1Document4 pagesHormone Levels For Fertility Patients1Kunbi Santos-ArinzeNo ratings yet
- Management of Infants BornDocument6 pagesManagement of Infants BornDiana FlorezNo ratings yet
- Comparative Efficacy of SPONTANEOUS BREATHING TRIAL Techniques in Mechanically Ventilated Adult Patients A ReviewDocument6 pagesComparative Efficacy of SPONTANEOUS BREATHING TRIAL Techniques in Mechanically Ventilated Adult Patients A ReviewInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Emergency Medical Technician CPGs PDFDocument121 pagesEmergency Medical Technician CPGs PDFAnonymous OdW7ev100% (1)