Professional Documents
Culture Documents
Biophysical Assessment
Uploaded by
Sanjeev Nambalate0 ratings0% found this document useful (0 votes)
66 views9 pagesself asessment
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentself asessment
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
66 views9 pagesBiophysical Assessment
Uploaded by
Sanjeev Nambalateself asessment
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 9
1
Biophysical Assessment of the High-Risk Fetus
Michael Emerson, M.D.
2
I. Background of Biophysical Assessment
A. Definition: multiple biophysical parameters are evaluated at a
single setting
1. Dynamic
a. Fetal heart rate (FHR): nonstress test (NST)
b. Fetal breathing movements (FBM)
(1) Incidence
(2) Rate
c. Fetal body movements (FM): incidence
d. Fetal blood flow: Doppler velocimetry
2. Static
a. Amniotic fluid volume (AFV)
(1) Pockets
(2) Quadrants
b. Neurologic tone: flexion-extension
c. Placental grade
B. Significance of biophysical parameters
1. FHR: interrelationship of autonomic nervous system
(ANS), acid-base balance, oxygenation, conduction,
contract
a. Clinical significance: standard tool assessing fetal-
placental respiration, caloric reserves
b. Baseline data
(1) Rate
(2) Variability
(3) Response to stimuli
(4) Periodic changes
2. FBMs
a. Examples
(1) Central respiratory regulation
(2) Acid-base balance
(3) Oxygenation
(4) Neuromuscular integrity.
(5) Maturity
b. Clinical significance
(1) Episodic
(2) Related to time of day
(3) Electrocortical state
(4) Maternal fed state
c. Baseline data
(1) Incidence (percent time spent breathing)
(2) Rate
(3) Variability
(4) Fetal body movements
a. Examples
The heart rate test was more likely to be abnormal first, decreased breathing
activity next, decreased movement next and tone last. This exactly reflects
the model that I gave you at the beginning so that our clinical observation
of what goes wrong mirrors perfectly what was hypothesized in the model
to be the way in which things disappear. It tells you that if your NST is your
only abnormal component, and everything else is still pretty much intact,
that the likelihood of significant hypoxia is small. If your NST and your
fetal breathing activity are both either diminished or absent, your likelihood
of hypoxia goes up substantially and if you add a third element, you might
as well stop at the point because you have enough information to consider
intervening on that baby.
Let's go on to the issue of the fact that you could probably get away from
having to do all of these variables and really you can eliminate movement,
because once you get anything past breathing and NST your prognosis
doesn't change whether you add movement or whether you add tone in
terms of the likelihood of a compromised outcome.
I am going to come back to tone because tone is our best window of
anything that we look at into things occurring above the brainstem.
Remember one of the things I mentioned in my previous talk that was a
concern is that you can have a brain injury, unrecognized, the fetus recovers,
survives and goes on and produces an apparently okay NST and may
produce an okay AFV. How are you going to know that? The fact of the
matter is that you may only know that by looking at fine motor activity of
the fetus. You may only know that by watching the pattern of activity and
the fact of making an observation that the fetus doesn't change state. So
these are things that become more subtle. We are still a long way away
from being able to reach this holy grail of predicting antenatal brain damage
at the time that it occurs so that when they baby comes out and looks
terrible and becomes a casualty that we are not consistently taken to task for
doing something wrong during the process of labor and delivery.
Again, if we take a look at management schemes, if we do testing, most of
our testing is done on babies near term and if we have a normal test, this is
a very robust statement of fetal condition, because we have the chronic
component which is the amniotic fluid and we have the activity components.
Together, that test can be robust enough to keep you in good stead for up
to a week as opposed to the NST which is generally a two to three time a
week exercise. If you did a perfectly normal biophysical profile and a
patient's clinical status didn't change, then that could be good and be robust
for you up to a week.
If you have one abnormal parameter, it really depends on what it is. But in
general, you want to look at the baby a little more closely and probably
repeat that test to see whether you are dealing with a process in becoming,
if that is a nonreactive NST, or if that is oligohydramnios. Again, amniotic
fluid is not an absolute. You are allowed about a 10-20% variation in your
AFI between the examination of sessions. The fetus urinates, the fetus
swallows and so forth but you do want to look at the baby within 24 hours.
Then, if you are still not satisfied, that is when you invoke your CST. That
is when we most commonly invoke our CSTs.
If you have two or more abnormal parameters, we look at that in a mature
baby as being an indication to go ahead and deliver. In an immature baby,
we would probably back that up with a CST. We want to be sure because
we are looking at events that bear some relationship to fetal behavior that
we are not looking at the possible influence of maternal medication. The
maternal medications that are notorious for reducing the biophysical scores
are medications that interfere with CNS function. Mag sulfate certainly is
a classic. When you have babies on mag they just lie there because their
mag levels get to the same level as their mother's. So if you want to know
what the baby is doing, look at the mom. If she is lying back there, she can't
watch her soap operas because she's got diplopia, she is groggy, sleepy, not
moving around, the baby is doing the same thing. So when you are trying
to evaluate babies whose mothers are receiving magnesium for preterm
labor, for example, if you are doing biophysical assessment, that becomes
a issue. It is a problem because you have blunted the things that you are
3
(1) Neuromuscular integrity
(2) Oxygenation
(3) Caloric reserves
b. Clinical significance: rough measure of caloric homeo-
stasis
c. Baseline data
(1) Incidence (percent time spent moving)
(2) Numeric counts
4. AFV
a. Examples
(1) Aggregate of fetal urination
(2) Gastrointestinal motility
(3) Tracheal flow
(4) Membrane exchange
b. Clinical significance
(1) Peaks at 34-36 weeks
(2) Reflects visceral shunting in high-risk adaptions
(3) Anomalies
(4) Growth disturbances
c. Baseline data: quantitative assessment
(1) Pockets
(2) Quadrants
5. Neurologic tone: reflex activity which may be elicited with
sound or it may be spontaneous
a. Clinical significance
(1) Oxygenation
(2) Central nervous system integrity
(3) Motor function
b. Baseline data
(1) Flexion-extension
(2) Attitude
(3) Startle reflex
(4) Sucking
6. Placental grade
a. Morphologic description of placental maturity (senes-
cence)
b. Clinical significance
(1) Crude estimate of placental aging
(2) May be more advanced in disease states
C. Concept of fetal states
1. Biophysical behavior is related at term to organized
clusters called "states"
a. State 1: quiet sleep
b. State 2: rapid eye movement sleep
c. State 3: intermediate
looking for most carefully so then you are reduced to looking for issues that
get very basic like are there late decelerations associated with contractions
in this mother that you are tocolyzing?
The standard score, as I mentioned to you, has five components in it. The
thresholds for scoring these components are really, quite frankly, arbitrary.
Generally, fetal breathing of more than 60 seconds would be reassuring
under most circumstances. Movements, tone, AFV, or AFI and your NST.
We use a modified scoring system that works out to 10 and 10 is a nice
number. Eight and 10 are not necessarily equivalent because as I mentioned
to you it depends on what you've lost points for. What happens when your
score goes down is that you start this exponential increment in bad
outcomes, whether it is antepartal death you can see here, there is no
linear relationship at all. It just shoots right up there and your incidence of
fetal distress and your incidence of neonatal depression are all elevated and
you can make the same statement about babies that end up with abnormal
neurologic outcome as a result of asphyxial injury. So there is a very, very
sharp demarcation once you get to scores that are less than 6 and that
should be regarded as being, again, a signal to intervene.
Now let's get to the evidence. The evidence unfortunately is very limited.
There really have only been a couple of trials that have compared the
biophysical profile, the comprehensive profile, to the NST. The NST at that
time was the gold standard. These are trials that are 10 years old. The
numbers are not very large but what you see here, and this is actually not
what the, I think, authors really wanted to show, but it is what in fact they
have shown is that compared to the NST, the biophysical profile in these
two studies doesn't appear to make a difference in your outcomes. Your
perinatal deaths, your low Apgars, your intrapartal fetal distress cases were
similar. I can say this because your confidence intervals include the number
1.
Why is that? Why do you suppose that is the case? The reason that is the
case is what you have done is you have taken a test which is part your
biophysical profile, you set that off as your gold standard, and now you are
comparing the rest of your biophysical profile to that test. Remember, in
these centers the NST was done separately from the rest of the biophysical
profiles so you could have tests in which the NST, had they been done
together, would have been different than when they were done separately.
But I would say that the overwhelming issue here is the numbers are far too
small to make you feel comfortable that this is a definitive statement about
how good the biophysical profile really is.
I think the other issue here is that we probably won't get better control data
than what I have shown here. There just isn't money to do the studies. The
NICHD isn't interested funding that kind of work anymore and so we are
going to have to take it on faith that what I have told you physiologically
makes a lot of sense. If you understand the components and what they are
trying to tell you and interpret the differences between the chronic and acute
components and remember that the test is not perfect, it gives you more
information than does any single component. I think at that point what we
are seeing here is the fact that this is the best case scenario we are going to
have. This doesn't stop me from doing biophysical profiles but it makes me
very careful in terms of interpreting the biophysical profile as a single stand
alone test.
Let's talk about umbilical flow velocimetry and let's put this into a location
where you can take something away that might be helpful for your practice.
The story of Doppler really goes back now a decade and a half so it is not
really news but I think if we take a look at the cord.
Let's look at the circulation that we are dealing with and why this is a very
interesting part of the fetal circulatory system. Again, I promised I would
give you a little bit of physiology here because I think it makes you better
consumers to understand what the label means rather than just going ahead
and buying the product. Here, actually, is the part of the circulation that we
are interested in and it is way, way downstream but here are the umbilical
arteries. As you know, the umbilical arteries course along either side of the
4
d. State 4: "wakefulness" (active)
2. State influences
a. Time of day: circadian rhythms
b. Maternal diet status, oxygenation
c. Maternal drugs
d. Gestational age
III. Technique of Biophysical assessment
A. Instrumentation
1. Electronic FHR monitor
a. Doppler
b. Air encephalogram (AECG)
2. Realtime ultrasound (US)
B. Test conditions
1. Standardized for
a. Time of day
b. Maternal status
c. Length of observation
2. Concurrent acquisition of biophysical
IV.Test Interpretation
A. "Standard" biophysical profile:
1. Sequential NST and US
2. NST: two or more accelerations >15 beats per minute
(bpm) in 20 minutes
3. Realtime scan
a. FBM: >30 seconds of continuous breathing
b. FM: >3 movements
c. Fetal tone: >1 flexion-extension episode
d. AFV: one pocket of 10 mm x 10 mm
e. Placement grade <3
4. Overall test requires 25-70 minutes
5. Scoring system
a. Each parameter ranges from 0 (abnormal) to 2
(normal)
b. Total score >8 is normal; <4 is abnormal
B. Alternative approach
1. Concurrent recording of all parameters under standardized
conditions
2. Data relaxed to institutional normal values
3. Value >two standard deviations from normal: abnormal
4. Test performed for 60 minutes
5. Normal test: all parameters normal
6. Abnormal test equals two or more of the parameters
abnormal PR decline >50%
bladder and eventually join the central circulation and are tributaries off the
iliac, the aorta and receive a fairly downstream blood flow from the main
pump up here. Here you see the umbilical vein going back up and getting
admixed with the enterohepatic circulation. Eventually that oxygenated
blood enters the right atrium where it encounters a current coming from the
superior vena cava.
So what the arterial circulation of the umbilical cord really is doing is it is
the last tributary to bring blood back to the placenta for processing. So it
has an obviously very important physiologic role because the placenta is a
surrogate lung, it is a surrogate GI system, it is a surrogate kidney and it
acts as a way of dealing with the acquiring of essential nutrients, substrates,
oxygen and the detoxification of the blood by getting rid of CO
2
and
hydrogen ions and broken down metabolites from substrates that have
already been processed.
Now, if we take a look at the developmental basis for velocimetry, we
know that after the mid trimester, placental adaptation generally is fixed in
terms of the number of cotyledons, the number of central vessels that exist
on the chorionic plate. The main change that occurs in the placental
circulation of the fetus is a large increase in terminal villus units or the so-
called microvasculature of the placenta.
Physiologically, this is a system that is adapted to give you a low resistance
to flow in its terminal end. Abnormal resistance to umbilical blood flow then
is a process that suggests that something is going wrong, either by
infarction of this vascular tree or by perhaps initially a hypoplastic situation
where you don't get this great proliferation of vessels to great quantities.
Experimentally, abnormal systolic/diastolic patterns, which I will show you
shortly, can be created with placental infarction and this has been done
successfully in laboratory animals through embolization. So you can
recreate this by destroying selectively parts of your placenta. You can
recreate this increased resistance to flow that you get in a compromised
baby. In addition, pathologic examination of the placenta has shown a very
good correlation between terminal villus capillary counts and the waveform
patterns that are seen, again, in disturbed pregnancies.
The nice thing about looking at the umbilical vessels is that it is easy and
96% of the time you've got two shots at getting one. They are easy to
identify. They are easy to see. They have long courses and this is just
recapitulation of what I have already told you, but the fact of the matter is
why pick a target that is hard to find? Part of the appeal also is the fact that
this is a circulation that is very stable. Under situations where there is
chronic hypoxemia, we have preservation and actually an increase in blood
flow to the placenta which is your umbilical arterial circulation, the brain
and the heart and you can see under a chronic hypoxemia - the white boxes
- that everything else is diminished. This tells you how well adapted the
fetal circulatory system is to environmental stress resulting in chronic
hypoxemia.
If we take a look at the Doppler examination itself, again it is a very simple
technique and that has really been part of the appeal because you can do it
in an office. The technology now for operating the Doppler equipment is
really very simple and it has been made even simpler because it has onboard
computers. It is the same technology that we have used for years to just
capture fetal heart rate. It is just specially adapted to both an auditory and
visual display that captures the waveform that is unique to the umbilical
arterial circulation. I can take anybody from scratch who has never done it
before and make them experts in about 20 minutes. The probes here are
standardized, generally operating at about 3.5 MHz, and we get a nice
display screen. When we use the continuous wave, which are the cheaper,
more mobile machines, we generally take a look at the cord with a real time
ultrasound before so we pick a part of the cord that is neither near the
beginning, near the egress of the cord from the abdomen, nor near the end
where it is implanted into the chorionic plate. Because in that intervening
space it makes relatively little difference where you intersect the artery
when you are doing repetitive examinations.
5
V. Summary of Previous Clinical Experience
A. Benefits
1. Improved detection of anomalies, intrauterine growth
retardation (IUGR) cord problems
2. Diagnosis of neuromuscular, neurologic problems
3. Two or more abnormal parameters appear to increase
sensitivity
4. Corroboration of abnormal fetal acid-base.
B. Drawbacks
1. Placental grade: not useful
2. Fetal breathing affected by
a. Diet
b. Labor
c. Time of day
3. Tone: questionable benefit
4. AFV: no standards
5. Time-consuming, labor intensive, expensive
6. Not proven superior to FHR testing with or without AFV
assessment
VII. Doppler Velocimetry
A. Fetal-placental circulation
1. The fetal umbilical-placental circulation
a. Anatomy
(1) The fetal cardiovascular system is characterized
by a relatively high output, low pressure/low
resistance network which oxygen delivery is
regulated
(2) Blood flow is phasic and influenced by
(a) Cardiac cycle: systole and diastole, which
provide two surges; the direction of flow is
rate-dependent
(b) Afterload: increases with peak systolic flow
and decreases with peak diastolic flow
(c) Breathing: increased tracheal pressure in-
creases venous forward flow and umbilical
vein pulsations
b. Umbilical vessels
(1) Two arteries
(a) One to two millimeters in diameter
anastomosing at chorionic plate
(b) The number of cotyledons and three orders
of branches are constant after 14-16 weeks
(c) Growth results from proliferation of terminal
syncytial budding stemming form capillary
plexus which protect villi from blood pressure
If we are going to be more sophisticated and use a continuous viewing
system, the so-called duplex Doppler system that you have in most of your
mainframe ultrasound machines, then there are a couple of issues that
become critical. One is your scanning angle or angle of insonation. The
advantage of this, of course, is that you can see your waveform unequivo-
cally as you are scanning your vessels so you know that you are not looking
at something else. But I can tell you as well that the data that you get from
this approach are very, very similar to those that you get from a good
continuous wave machine that is well aimed.
I throw this in here. We have color and I am sure many of you have color
also. Is there an advantage in using color in terms of insonating the umbilical
arteries? I would submit to you that it unequivocally tells you that you are
looking at arteries well, maybe that is going to be an issue it certainly
is helpful when you are dealing with babies that are oligohydramniotic. So
it helps you visualize the cord and aim your Doppler probe better. It is not
absolutely necessary and you can effectively do this kind of insonation
without having color.
Again, what you are doing with either approach is you are sending a beam
into a moving stream of red cells. These red cells will send you back a
reflection that is at a slightly different frequency. There is a shift. You hear
it. It is the "whoosh-whoosh" that you hear. That is the difference in
Doppler signal going in and reflective signal coming back. It is processed
by your machine and then it is displayed on the screen. The display on the
screen, the so-called waveform, is really a Fourier transformation of zillions
of data points that are all reflected by these populations of red cells that are
moving in different directions at different speeds. You could never deal with
this on a three-dimensional plot. It would look like a mountain range so it
is reduced to two dimensions by Fourier transformation.
There are different ways of dealing with the waveform. Most of the
schemes use a peak. Either a peak to trough, the so-called S/D ratio or a
peak to mean velocity. A peak to mean velocity is the so-called pulsatility
index. There are advantages and disadvantages to both approaches. They
convey similar information. The only advantage of using the pulsatility index
is when you have either an absent or a reverse end diastolic velocity, you
can still get a number. Not that it is necessarily important if you ever have
an absent or a reverse end diastolic velocity.
We generally take a number of cycles. We sample them. We average them
and this reduces the likelihood that the fluctuation you see from session to
session is going to be just due to an observational technique issue. We do
at least three repetitions. We take about 15 cycles and then we pool them,
average them and come up with our results. Our onboard computer, of
course, gives you the PI. It gives you also, I should mention, the resistance
index because you will see this in some publications. It is the peak less
trough over the peak. Again, PI and S/D and RI all convey similar types of
information. They are not really apples and oranges.
If we take a look then at clinical interpretation, which is really sort of the
big payoff here, what is the clinical interpretation? What do we get from
that? You are going to get a number. Obstetricians are enamored of
numbers. We have Apgar scores, we have Bishop's score, we have the
breech score, we have various pelvic scores. I mean, we really love numbers
and this is a number so we should love it. But we have to understand how
to use it and what it really means. What it really means is nothing unless you
have a scale of reference in which to apply the number that you get. If you
don't have that then all that you have is a number. There are times when that
is not necessary and there are times where you have abnormalities of your
end diastolic flow. Remember that it should always be a positive waveform
in diastole and the only time that the positive waveform disappears are
under circumstances of extremely increased downstream resistance.
Depending on degree, it may disappear or it may appear on the other side
of the x-axis.
In addition, we look at this clinically in sequence over time because this is
not a static observation. It is a moving target. If we take a look at here at
6
(BP) changes
(2) Intervillous pressure: 10-15 mm Hg
(3) Umbilical arterial pressure equals fetal systemic
pressure
(4) Umbilical blood flow
(a) Peaks at midgestation
(b) Resistance falls by 3% per day
(c) Blood flow decreases in proportion to fetal
weight
c. Control of umbilical flow
(1) No feedback system for pressure or resistance,
not directly affected by hypoxia
(2) Not innervated beyond first 2 cm proximal
(3) Constricted by vasoactive agents
(a) Prostanoids
(b) Angiotensin-II
(c) Bradykinins
(d) Vasoconstriction leads to increased O
2
extraction
(4) Flow rate
(a) Determined by systemic perfusion pressure
difference (A-V)
(b) Responds to changes in
i. FHR
ii. Stroke volume
iii. Cardiac contractility
d. Responses to stress
(1) Acute hypoxia: redistribution or cardiac output
leads to decreased umbilical blood flow to de-
crease in cardiac output which leads to venous
return
(2) Chronic hypoxemia: restricted placental growth
leads to decreased capillary bed size; terminal
resistance does not fall or may increase
C. Clinical manifestations of vascular flow
1. Determinants of volume flow
a. Vessel diameter and wall thickness
b. Vessel linearity and uniformity (distensibility)
c. Turbulence: transmission and reflection
d. Blood volume properties
(1) Density
(2) Viscosity
(3) Cell morphology
e. Applied pressure
(1) Pulsatility
what is known for normal pregnancy, and we now have a lot of data on
normal pregnancy, basically over time there is a decline in the overall trend
of the S/D ratio or pulsatility index as the fetus becomes more mature. The
reason for that is really very simple. Over time as the placenta increases in
size, your downstream vasculature continues to grow and you continue to
reduce your downstream resistance.
If you take a look at a waveform, and this is just one graph. There is an S/D
ratio that however old the fetus is going to be distinctly abnormal and that
is an S/D ratio over 4. From that point forward, an abnormal S/D ratio is
really going to depend on where you are in gestation and that is an important
point. Because as you get closer to term, at 40 weeks, if you have an S/D
ratio that is over 3, that is an abnormal ratio. It would not be an abnormal
S/D ratio, say, at 30 weeks. You can see here there is a pretty broad spread
between these are the 5th and 95th percentiles so that again gestational
age trends and there are few absolutes unless you are greater than 4 or at
term, if you are greater than 3.
Now let's look at what happens as we start losing the integrity of the fetal-
placental circulation. You start getting a gradual widening between peak and
trough until we get down towards the bottom here. You can see that the
trough almost has disappeared and then at the bottom we see the trough
appears on the other side of the x-axis. So this is a progression from normal
to absent end diastolic and finally to reverse end diastolic velocity. You very
rarely see this evolve over single pregnancy because the absent or reverse
end diastolic velocity in and of itself is a very uncommon finding.
If we take a look, even without numbers, if you take a look at two
waveforms on the same scale, you don't have to have numbers to tell you
that this looks a lot different from this. This baby has a normal S/D ratio of
about 2.5 and this baby has an S/D ratio that is about 5. How did we do
that? We took the peak, we took the trough and we did a ratio. Simple. This
is actually done for you. You might be able to see on the machine here, you
actually have these computers for you on board so there is no processing
you have to do yourself. Here is an absent end diastolic velocity and here
is one in which the end diastolic velocity appears on the other side of the x-
axis.
Where is the payoff for this particular technology? The payoff is really
limited but there is an area in which I think it makes sense to consider
adding Doppler to your armamentarium. That is in the situation where you
have a pregnancy that is either thought to be growth restricted or has a very
high probability based on maternal disease or past history or lifestyle of
being a growth restricted pregnancy. The reason that we pick this is the
clinical studies that have been done so far suggest that the yield is very high
in this particular subgroup. Further, there is a collection of pathologic
observations that have looked at the placentas of these babies and have
correlated placental morphology with Doppler velocimetry.
Remember, IUGR is not a pure population. It is a spectrum and you may
have IUGR in which the baby is asymmetrically poorly grown in which the
head generally is relatively spared, the body is not and then you have the
symmetrically IUGR baby where everything is small. This is generally the
asymmetrics are the ones that appear later in pregnancy, the symmetrics
earlier and remember that the symmetrics are the ones that are more likely
to have other very serious problems - chromosomal problems, infections
and other malformations.
The interesting thing here is because you are looking at a developmental
process in the placenta, what you are observing here is that the waveforms
on sequential Doppler velocimetry of the umbilical vasculature may start
appearing to be abnormal before you have any other evidence to support
that this baby is having trouble growing or adapting to an intrauterine
environment. The general lead time can be as much as several weeks so that
if had a situation, if you had a pregnancy in which you thought that here is
a high-risk for IUGR, mom is hypertensive or has advanced diabetes,
wouldn't it be nice to get a heads up on things that are going to be going
7
(2) Amplitude
f. Peripheral resistance
2. Characteristics of fetal-placental vasculature
a. Small diameters, thin walls
b. Short length, nonlinear, easily distended
c. Numerous branch points: angle turbulence
d. Differences in maternal and fetal blood
e. Pulsatile flow related to rate and systemic pressure
f. Low resistance systems
3. Semiquantitative measurements of circulation
a. Empirical indices of flow velocity
(1) A:B (S/D) ratio: f(max): systolic peak/f(min):
diastolic peak
(2) Pulsatility index (PI): f(max) - f(min)/f(mean)
(3) Pourcelot's ratio (resistance index): f(max) -
f(min)/f(max)
(4) Frequency index profile: median of peak/mean
during cycle
D. Doppler studies of normal and complicated pregnancies
1. Normal pregnancies
a. Waveforms are characterized by high flows with low
resistance
b. Curves generated across pregnancy are similar for
systolic/diastolic (S/D) ratio, pulsatility index
(1) Slope changes at 28 and 36 weeks
(2) Variation inversely proportional to gestational
length
c. No significant effect with changes in viscosity either at
high shear (RBC aggregates broken up) or low shear
(RBCs clumped)
d. No significant relationship to umbilical venous flow
2. Intrauterine growth retardation
a. High sensitivity and consistent finding of elevated flow
resistance indices
b. Worst prognosis associated with absent or reversed
end-diastolic flows
c. Highly predictive or placental pathology
d. Histology: obliterated or reduced terminal arterioles in
villi
e. Separate population of IUGR fetuses with anomalies
had normal S/D ratios, indicating nonplacental source
of problem
f. Waveform indices may be elevated weeks to months
prior to clinical diagnosis of IUGR. This sign is typi-
cally, the first abnormal sign in testing schemes
wrong downstream so that you can start looking at the baby more closely?
That is certainly something that has been observed by a number of authors
that have looked at the application of Doppler to this population.
The other area in which there has been some value in the use of Doppler
have been twins. I am not going to belabor that point. You had a very nice
talk on twin pregnancy before. But the fact of the matter is that twins are
more prone to having growth disturbances. They are more prone to having
abnormalities of placental circulation to begin with and discordance between
twins and discrepant fetal growth are the hallmarks of twin gestations. We
have altered the distribution of twins in our population by assisted reproduc-
tive technologies so we are seeing more of them and certainly of the areas
where one could apply Doppler, this area makes sense.
Again, this is sort of an extreme example. I know these babies are the same
age because I saw them when they born although they don't look like they
are at all related. Here you have this nice robust twin over here and then
you've got his little brother over here who really doesn't look quite so
healthy. Here is another parable of Doppler done in twin pregnancy. This
is the parable of the good girl and the bad boy. Over here you see twin 1.
Nice normal Doppler velocimetry, nice heart rate tracing. On the right,
you've got twin 2. Absent end diastolic velocity, sort of a nonreactive trace
here. Here you can see the graph of twin 2. The bad boy who never has
normal Dopplers in the third trimester and the good girl's whose Dopplers
are always within the normal range and so you go ahead and deliver these
babies. You sort of split the difference and deliver them at about 34 weeks
and the good girl weighs 2,000 grams and the bad boy weighs 1,000 grams.
The point here is as an adjunct to measure to supporting your hypothesis
that the placenta is not functioning well in a discordant growth that again
Doppler has a role in twin gestation.
As a sole screening modality for fetal well being in the third trimester,
Doppler is very limited. Again, I show you this slide for the NSTs. Here is
the same basic slide for Doppler. The big four. Postdates, diabetes, IUGR
and hypertension. Not surprisingly, the only populations in which Doppler
appears to have potentially assisted detection of compromise have been the
IUGR and the hypertensive group and you can see that is really below 50%
sensitivity here. In the diabetic group and in the postdates group it is
relatively useless. The only exception in the diabetic group are those who
have advanced diabetes with vascular complications. So we don't do it all
in our postdate pregnancies. We long ago abandoned using Doppler in that
group and we focus on the hypertensive, IUGR and multi-fetal gestations.
In closing the session on Doppler, I have to tell you the reason that I spent
time on this subject is that Doppler is the best studied from the standpoint
of evidence and outcomes based of all of the modalities that I have shared
with you this morning. There have been about a dozen trials in the past
decade that have been reported in Europe looking at umbilical Doppler.
Nine included only high risk patients which I think really is the province of
this particular investigation. If we take a look again of this table of
outcomes here, if you look at all of the outcomes and this is all of the trials
pooled together, what you see here for the most part is that if you look at
general populations, there appear to be no advantages in using Doppler. If
we focus on perinatal death, this is now getting into the general population,
perinatal death as an endpoint, what you see here in the area of most
importance is stillbirth because that is something we can do something
about potentially by antepartal surveillance, you can see that we are starting
to make a dent. In fact, the application of Doppler as part of the surveillance
in the high risk populations resulted in a 38% decrease in stillbirth and this
contributed to about a 33% fall in overall perinatal death and this was
significant. You see this confidence interval falls below 1. If we focus only
on high risk pregnancies, which is the true province, it is even more
dramatic. You can see here that perinatal mortality falls by 50% or greater
for stillbirths in the population in which Doppler was used as part of the
screening modality.
If we take this to heart, what we can we really take away from this? First
of all, these were not trials done in the United States so you could attribute
8
3. Multiple gestation (twins)
a. Clinical concerns
(1) Relative IUGR after 28-29 weeks
(2) Twin-twin transfusion syndrome
b. Methodology
(1) Realtime scan to locate individual cords
(2) Values are similar to singletons except when IUGR
is present
(3) Twin-twin transfusion syndrome characterized by
size disparity with equivalent S/D ratios
c. Study results: S/D ratio differences of >0.4 associated
with IUGR
4. Diabetes mellitus
a. Few data reported indicates that, regardless of
size-for-dates classification, elevated S/D ratio sug-
gests an arrest of fetal growth over time
b. Elevated S/D ratios are also associated with higher
incidence of perinatal complications
5. Normal labor
a. Fleischer et al in 1987 studied twelve normal
parturients
(1) No significant differences in S/D ratios during any
phase of uterine contraction
(2) No differences noted between latent phase, active
phase, after rupture of membranes, or with
administration of oxytocin
b. Smart et al in 1981 studied ten normal patients with
similar findings
6. Postdatism
a. Recent ,data suggest that S/D ratio may be a good
predictor of perinatal morbidity in this population
b. S/D ratio is not reflective of oligohydramnios
7. Establish relationship of velocity parameters to clinical
conditions
E. Conclusions
1. Doppler waveform analysis is a relatively new application
which can be performed with moderately priced equipment
2. The semiquantitative measurement of velocity waveforms
are now generated by current hardware, and are relatively
reproducible throughout gestation
3. Doppler information can be obtained rapidly by easily
trained personnel
4. The usefulness of Doppler measurements of fetal umbilical
vessels remains to be established but shows promise in
the evaluation of fetuses at risk for IUGR
this to different forms of antenatal care. They were trials that are done very
close to our particular era of practice. That in addition, we could either say
that we refuse to believe this because it wasn't done in a U.S. center or we
can say that perhaps there is something to the addition of Doppler to
selected high risk populations. That, in fact, that if we are to really call it
like it is, let's now put our collective thoughts together and perhaps retrace
where we have gone this morning before I open this up to general questions
once again.
What are we really trying to accomplish with antepartal testing? We are
really trying to prevent stillbirth, but preventing stillbirth due to possible
preventable causes and what is the major preventable cause is preventable
perinatal asphyxia. So I am backing this up because really if we had a good
way of reliably reproducibly measuring health so that we could confidently
say that asphyxia is either present, the risk of asphyxia is either highly
present or highly absent, that would be a giant step forward. A relatively
accessible testing scheme which uses clinical features that we can get our
hands around to identify fetuses at such high risk that labor should be
avoided and perhaps early intervention should be encouraged. Translating
that possibly into model systems to even improve our ability to forecast
intrapartum outcomes before the onset of active labor. Because you know
that the intrapartum area is where a number of unforeseen problems might
occur.
Now, if we take a look at antepartal testing, if accelerations are present, the
likelihood of not having an asphyxiated baby is pretty high. If accelerations
are absent and persistently absent, the likelihood of having a baby that is
affected by hypoxemia or acidemia is almost as high but not quite as high.
If we look at heart rate variability, as measured objectively by computer, not
by the eyeball, normal variability, again, very low likelihood of asphyxia.
Certainly not zero and if variability is abnormal or absent, again, very high.
Decelerations the same story. So what you see here with antepartal heart
rate testing is that, again, normal or abnormal antepartal heart rate testing
alone approaches the target but you can see that you have to be willing to
accept a significant error. I would call an error of 15-20% in calling a baby
well and an error of 30-40% in calling a baby ill a significant error. Because
it means that you are going to intervene much more likely on a baby that is
going to be well on the one hand and you are going to miss babies that you
should have delivered.
Now let's look at biophysical profile testing. If you look at biophysical
profile testing, if you have a score of less than 8, there was a 90%
sensitivity in positive predictive value for asphyxia. This was a selected
population delivered without labor. If you look at Manning's study, looking
at the correlation of biophysical profile with cordocentesis for blood gases
done at the same time, there is a stepwise linear relationship between
biophysical score and umbilical venous pH. If you look at a computerized
biophysical profile that we do in cord blood gases, there is a linear
relationship between score and ultimate umbilical artery pH at delivery. So
again, it suggests that biophysical profile testing by multiple components
moves you a step closer to making a good assessment for the absence or
presence of asphyxia without either over or undercalling the situation.
If we look at Doppler velocimetry, again, as a sole predictor, this varies a
lot from study to study but the bottom line here is that as a sole predictor,
that again, is no better than any of the other isolated tests that we do. Again,
these are based principally on high risk populations. You might ask
yourself, "Gee. What does a 40% likelihood of hypoxia do for me?" I can
assure you if somebody told me that this baby has a 40% likelihood of
getting hypoxia, that would get my attention. We intervene for likelihood
of compromise far, far lower than that in our obstetric practice. That would
get my attention.
9
The markers for perinatal asphyxia, conventional testing, trying to use what we currently have to predict it consistently or
sufficiently early really have problems. I am being very honest with you because part of my career has really been in this area. I
am saying that we have to understand that there are limitations in trying to go after this target. When we look at studies, remember
that we are looking at studies that are all population based and the populations, even though I have melded them together to give
you these meta-analyses, the populations may tend to be somewhat different from each other. My population, I know, is different
from yours. They don't talk the same way. Their lifestyles are different and therefore the findings from one state might not be
generalizable to another. In reality, there should be a lot more work done in this area. Even though it has been around for two
decades or more, some of the real seminal basic work that should have been done has not been done and that is a pity.
But I think that also gives us an opportunity here to look at where we should go. These are areas that we are working at and other
centers are working at to give us a better handle on how to best assess babies. I happen to be an advocate of the computer approach
because I think that deals with a lot of number crunching that is very hard to do with pencil and paper. But also there is context.
We should really approach this issue of perinatal assessment trying to uncover the risk in these babies and we should do it really
with the knowledge that we already know a lot about each pregnancy, or we should. We should know a lot about the antecedent
risk factors. We should know a lot about that patient's prior history. We should know a lot about her current state of health and
the things that are really putting this baby at risk. Those invariably should reflect on how we interpret the data and how we use it.
That again means that you do have to do some individualization.
There is, again, little question that if you get your hands on a high risk pregnancy early, then you are able to establish early the
baseline age of this pregnancy through good ultrasound, rule out anomalies through good ultrasound. Make an assessment of where
you are starting from, again, with good ultrasound, and using that as your backbone, you will end up with a better scheme for
prospectively following this baby. I am not dismissing the possibility that as we get further into the information age, that some of
this assessment could be translated into a home environment. So in other words, we could take patients that we don't want to have
doing a lot of running around, we can bring technology to their homes through home visits, through telemetry, bring it back to us
and make it actually more convenient for our patients. I know that is probably more difficult to do in Chicago where you have
weather. We don't have that problem. We just have a fairly difficult road structure to deal with. But that is again something that
I am sure is going to happen progressively more and more in the future.
You might also like
- Hyper Bilirubin Emi ADocument29 pagesHyper Bilirubin Emi ANinz NunezNo ratings yet
- Family Planning Methods - LatestDocument59 pagesFamily Planning Methods - LatestGenevieve VillaflorNo ratings yet
- Shock and HemorrhageDocument29 pagesShock and HemorrhageDr djNo ratings yet
- Assessing Nurses' Knowledge on Using Partographs During LaborDocument22 pagesAssessing Nurses' Knowledge on Using Partographs During Laborrevathidadam55555No ratings yet
- Pregnancy Hypertension LessonDocument13 pagesPregnancy Hypertension LessonsasikalaNo ratings yet
- Polyhydramnios 10Document4 pagesPolyhydramnios 10hussain AltaherNo ratings yet
- Dissertation Presentation: REG - NO.19N02102035 Obstetrics and Gynecological NursingDocument62 pagesDissertation Presentation: REG - NO.19N02102035 Obstetrics and Gynecological NursingSanju SudhaNo ratings yet
- Exercise Stress Testing GuidelinesDocument15 pagesExercise Stress Testing GuidelinesStevco Donev MakedonskiNo ratings yet
- Fetal Biophysical Profile PDFDocument2 pagesFetal Biophysical Profile PDFVickiNo ratings yet
- Signs and Symptoms of PregnancyDocument9 pagesSigns and Symptoms of PregnancyTrina Joy DomantayNo ratings yet
- Managing Rhesus Isoimmunization in PregnancyDocument29 pagesManaging Rhesus Isoimmunization in PregnancyIshen PerumalNo ratings yet
- Forceps DeliveryDocument13 pagesForceps DeliveryStar AlvarezNo ratings yet
- Pap Smear - Overview, Indications, PreparationDocument11 pagesPap Smear - Overview, Indications, PreparationBayu Surya DanaNo ratings yet
- Induction of Labour Techniq SADocument18 pagesInduction of Labour Techniq SAPujanaWiaktaNo ratings yet
- Clinical Diagnosis of Pregnancy: Dr. Archana Vikram Asst ProfDocument24 pagesClinical Diagnosis of Pregnancy: Dr. Archana Vikram Asst ProfMaizura Syahirah Mohtada100% (1)
- Brest Feeding - FinalDocument25 pagesBrest Feeding - FinalPranabh KushwahaNo ratings yet
- Ida Jean Orlando: "Nursing Process Theory"Document10 pagesIda Jean Orlando: "Nursing Process Theory"zeeky35No ratings yet
- Understanding Twin PregnancyDocument56 pagesUnderstanding Twin Pregnancyangel panchalNo ratings yet
- Disease Condition:: Hyperemsis Gravidarum: DefinitionDocument4 pagesDisease Condition:: Hyperemsis Gravidarum: DefinitionPriyanka JohnNo ratings yet
- Demonstrating the Benefits of Kangaroo Mother CareDocument13 pagesDemonstrating the Benefits of Kangaroo Mother CareDiksha DuhanNo ratings yet
- E-Nursing MicroteachingDocument14 pagesE-Nursing MicroteachingManisha SamsonNo ratings yet
- Welcome To Case Presentation: Presented byDocument26 pagesWelcome To Case Presentation: Presented byHemant ShahNo ratings yet
- BREASTFEEDING BENEFITSDocument5 pagesBREASTFEEDING BENEFITSJeya vanithaNo ratings yet
- POSTNATAL ASSESSMENT: Measuring Uterine Involution After DeliveryDocument18 pagesPOSTNATAL ASSESSMENT: Measuring Uterine Involution After DeliveryMiu MiuNo ratings yet
- Abdominal Palpation & Examination in Pregnancy 5.0 PDFDocument11 pagesAbdominal Palpation & Examination in Pregnancy 5.0 PDFPalaniswami Palaniswami100% (1)
- Multiple Pregnancies: Shanelle ThomasDocument40 pagesMultiple Pregnancies: Shanelle Thomasshanellethomas1820100% (1)
- Hypoglycemia in NewbornsDocument32 pagesHypoglycemia in NewbornsEmily EresumaNo ratings yet
- PROM-PPROM GuideDocument25 pagesPROM-PPROM Guideizyanzati100% (1)
- Orem's Self-Care Theory BY: Josephine NecorDocument40 pagesOrem's Self-Care Theory BY: Josephine NecorCamille Honeyleith Lanuza FernandoNo ratings yet
- Preventive ObstetricsDocument8 pagesPreventive ObstetricsMahima LalNo ratings yet
- Obg ResearchDocument15 pagesObg ResearchAGERI PUSHPALATHANo ratings yet
- 9fetal Well Being in PregnancyDocument10 pages9fetal Well Being in PregnancyuouoNo ratings yet
- Case Study 29-APHDocument31 pagesCase Study 29-APHZarul Naim Mohd TamiziNo ratings yet
- Assessment of Fetal Well-BeingDocument63 pagesAssessment of Fetal Well-BeingArhum Siddiqi100% (1)
- Insertion and Removal of Intrauterine Devices-AAFPDocument8 pagesInsertion and Removal of Intrauterine Devices-AAFPnouval_iqbalNo ratings yet
- Evidence Based Practices in ObstetricsDocument46 pagesEvidence Based Practices in Obstetricsvikas takNo ratings yet
- Unit 10: Disorder of Pregnancy and Their Nursing ManagementDocument59 pagesUnit 10: Disorder of Pregnancy and Their Nursing ManagementSrijana DahalNo ratings yet
- 05 N141 31673Document21 pages05 N141 31673priya thakurNo ratings yet
- Active Management of LabourDocument4 pagesActive Management of LabourHytham AtiaNo ratings yet
- High Risk Antenatal AssessmentDocument15 pagesHigh Risk Antenatal AssessmentAbishaNo ratings yet
- Sexual Dysfunctions and ParaphiliasDocument10 pagesSexual Dysfunctions and ParaphiliasGino Al Ballano BorinagaNo ratings yet
- Glasgow Coma ScaleDocument94 pagesGlasgow Coma Scaleriya priyaNo ratings yet
- FEOTAL MEASURE Clinical ParametersDocument13 pagesFEOTAL MEASURE Clinical Parameterssuman guptaNo ratings yet
- Postterm Pregnancy Risks and ManagementDocument29 pagesPostterm Pregnancy Risks and ManagementNur Agami100% (1)
- IEC Role Health ServicesDocument70 pagesIEC Role Health ServicesAparna Aby100% (1)
- Rh-INCOMPATIBILITYDocument14 pagesRh-INCOMPATIBILITYNithiya NadesanNo ratings yet
- Vancouver Style Referencing SystemDocument20 pagesVancouver Style Referencing SystemKarthik ManoharanNo ratings yet
- Oxytocics and TocolyticsDocument6 pagesOxytocics and TocolyticsFarheen khanNo ratings yet
- Journal Homepage: - : IntroductionDocument8 pagesJournal Homepage: - : IntroductionIJAR JOURNALNo ratings yet
- 29 - Abnormal Uterine ActionDocument31 pages29 - Abnormal Uterine Actiondr_asaleh94% (18)
- AEFI KIT and Dosage InformationDocument5 pagesAEFI KIT and Dosage InformationArif ShaikNo ratings yet
- Prolonged Labour - Print DR AdilDocument2 pagesProlonged Labour - Print DR AdilAri Puji AstutiNo ratings yet
- Malposition AND Malpresentat ION: Regala, Bianca Ysabelle M. BSN Ii - B Rle Group IiiDocument57 pagesMalposition AND Malpresentat ION: Regala, Bianca Ysabelle M. BSN Ii - B Rle Group IiiBiway RegalaNo ratings yet
- Physiological Changes of The PuerperiumDocument6 pagesPhysiological Changes of The PuerperiumBladimir CentenoNo ratings yet
- Estimation of Fetal WeightDocument38 pagesEstimation of Fetal Weightkennedy14344No ratings yet
- RANZCOG CTG Guideline SummaryDocument23 pagesRANZCOG CTG Guideline SummaryAndi Farid ANo ratings yet
- Hypertrophic Pyloric StenosisDocument3 pagesHypertrophic Pyloric StenosisCandice ChengNo ratings yet
- Artificial Insemination GuideDocument3 pagesArtificial Insemination Guidesagi muNo ratings yet
- Alzhymas DiseaseDocument12 pagesAlzhymas Diseasekids dance BNo ratings yet
- PROLOG: Obstetrics, Ninth Edition (Assessment & Critique)From EverandPROLOG: Obstetrics, Ninth Edition (Assessment & Critique)No ratings yet
- MillJ 0381-01 EBk v6.0Document314 pagesMillJ 0381-01 EBk v6.0Sanjeev NambalateNo ratings yet
- Rays of The Harmonist No1 Vol 1 1Document42 pagesRays of The Harmonist No1 Vol 1 1Mike DinesNo ratings yet
- A List of Factorial Math ConstantsDocument57 pagesA List of Factorial Math ConstantsSanjeev NambalateNo ratings yet
- Gaudiya Kanthahara HindiDocument377 pagesGaudiya Kanthahara HindiVivek DuaNo ratings yet
- Shri Camatkara Chandrika - Vishvanath Chakravarti ThakurDocument103 pagesShri Camatkara Chandrika - Vishvanath Chakravarti Thakurindology2100% (1)
- Benign Essential TremorDocument1 pageBenign Essential TremorSanjeev NambalateNo ratings yet
- Nectar of Govinda-Lila-latest EditionDocument128 pagesNectar of Govinda-Lila-latest EditionSanjeev NambalateNo ratings yet
- Caitanya MangalaDocument245 pagesCaitanya MangalaSubho DasNo ratings yet
- Enhancing Creativity Through Brainstorming Six Hats Mind MappingDocument29 pagesEnhancing Creativity Through Brainstorming Six Hats Mind MappingVasile MesesanNo ratings yet
- Labrador Ebook009723 PDFDocument122 pagesLabrador Ebook009723 PDFAdriana PopNo ratings yet
- Radha Kripa KatakshaDocument10 pagesRadha Kripa Katakshaadya_tripathiNo ratings yet
- Bond Yield CalculatorDocument1 pageBond Yield CalculatorSanjeev NambalateNo ratings yet
- Balacharitham PDFDocument29 pagesBalacharitham PDFjigarmistry86No ratings yet
- Buddha Dhamma C AkraDocument76 pagesBuddha Dhamma C AkraEricson ChewNo ratings yet
- Durga ChalisaDocument1 pageDurga Chalisaapi-3844610100% (1)
- Human Life Very Rarely ObtainedDocument11 pagesHuman Life Very Rarely ObtainedSanjeev NambalateNo ratings yet
- Drinking Poison KnowinglyDocument6 pagesDrinking Poison KnowinglySanjeev NambalateNo ratings yet
- Garga SamhitaDocument1,795 pagesGarga SamhitaSanjeev Nambalate100% (3)
- Enlightened EgoismDocument19 pagesEnlightened EgoismSanjeev NambalateNo ratings yet
- Bhagavad Gita MahatmyamDocument18 pagesBhagavad Gita MahatmyamJulen OsorioNo ratings yet
- BlackBerry Curve 8310 User GuideDocument137 pagesBlackBerry Curve 8310 User GuideSanjeev NambalateNo ratings yet
- Evolution and ElevationDocument13 pagesEvolution and ElevationSanjeev NambalateNo ratings yet
- Good and NotDocument10 pagesGood and NotSanjeev NambalateNo ratings yet
- Accounting For ManagersDocument228 pagesAccounting For ManagersNarayanan VkNo ratings yet
- Krsna and Guru Not in EverybirthDocument9 pagesKrsna and Guru Not in EverybirthSanjeev NambalateNo ratings yet
- Cardinal Danielou-Dont KillDocument13 pagesCardinal Danielou-Dont KillSanjeev NambalateNo ratings yet
- HighDocument14 pagesHighSanjeev NambalateNo ratings yet
- God IsnDocument16 pagesGod IsnSanjeev NambalateNo ratings yet
- God and GuruDocument8 pagesGod and GuruSanjeev NambalateNo ratings yet
- Puskesmas PDFDocument24 pagesPuskesmas PDFChristopher AdhisasmitaNo ratings yet
- Pengetahuan Ergonomi Dan Postur Kerja Perawat Pada Perawatan Luka Dengan Gangguan Muskuloskeletal Di Dr. H. Koesnadi BondowosoDocument5 pagesPengetahuan Ergonomi Dan Postur Kerja Perawat Pada Perawatan Luka Dengan Gangguan Muskuloskeletal Di Dr. H. Koesnadi BondowosoImanuel SihotangNo ratings yet
- CHAPTER 2 - Ethics in Pharmacy PracticeDocument15 pagesCHAPTER 2 - Ethics in Pharmacy PracticeMona GhazyNo ratings yet
- Career Trade Research ProjectDocument13 pagesCareer Trade Research Projectapi-497653037No ratings yet
- Paranoid SchizophreniaDocument21 pagesParanoid SchizophreniaRizwan ZafarNo ratings yet
- 三民高三上第二次月考複習 教師卷Document12 pages三民高三上第二次月考複習 教師卷黃紘志No ratings yet
- First Aid: NSTP 002Document5 pagesFirst Aid: NSTP 002Alvin VelasquezNo ratings yet
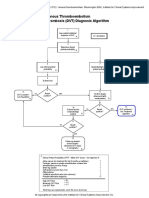
- Venous Thromboembolism Deep Vein Thrombosis (DVT) Diagnosis AlgorithmDocument1 pageVenous Thromboembolism Deep Vein Thrombosis (DVT) Diagnosis AlgorithmImam Nur Alif KhusnudinNo ratings yet
- Parenteral FeedingDocument7 pagesParenteral Feeding4gen_7No ratings yet
- Colorado Family Resilience Theory Focuses on RegulationDocument23 pagesColorado Family Resilience Theory Focuses on Regulationvbdfg5No ratings yet
- Methods of Public RelationsDocument3 pagesMethods of Public RelationsAnusha Verghese100% (2)
- Exam ChecklistDocument13 pagesExam Checklistmahmoud selimNo ratings yet
- 2013 Sample Psychology Cover LettersDocument2 pages2013 Sample Psychology Cover LettersLavander Meggie100% (1)
- Perioperative Nursing 101Document2 pagesPerioperative Nursing 101Anthony Dema-ala0% (1)
- Aorn Laser SafetyDocument16 pagesAorn Laser SafetyAmanda RapaNo ratings yet
- Registration Requirments of Animal Derived Non Medicated ProductsDocument2 pagesRegistration Requirments of Animal Derived Non Medicated ProductsValeria DumitrescuNo ratings yet
- Meal Plan MenDocument35 pagesMeal Plan Menoddo_mneNo ratings yet
- NZREX Bridging Programme OverviewDocument12 pagesNZREX Bridging Programme OverviewGus LionsNo ratings yet
- 9 H q1 l1.2 The Concept of Community HealthDocument16 pages9 H q1 l1.2 The Concept of Community HealthRegine Rellores BaliatNo ratings yet
- Medication: Expected Pharmacological Action Therapeutic UseDocument1 pageMedication: Expected Pharmacological Action Therapeutic UseMarina Wasem NetzlaffNo ratings yet
- Systemic Ophthalmology Disorders GuideDocument4 pagesSystemic Ophthalmology Disorders GuideAslesa Wangpathi Pagehgiri100% (1)
- Course Details: Assessment Task SITXINV002 Maintain The Quality of Perishable Items Page 1 of 9Document9 pagesCourse Details: Assessment Task SITXINV002 Maintain The Quality of Perishable Items Page 1 of 9Boban GorgievNo ratings yet
- Personality, cognitive flexibility, and motivation among medical professionalsDocument12 pagesPersonality, cognitive flexibility, and motivation among medical professionalsBishal.P 1830401No ratings yet
- 2010 - 3 Idsp Detail Information BKDocument73 pages2010 - 3 Idsp Detail Information BKPankaj ModhNo ratings yet
- Visual Acuity RecordDocument1 pageVisual Acuity RecordMydestiny Istobe WhityouNo ratings yet
- Managing The Health Insurance PortfolioDocument3 pagesManaging The Health Insurance PortfolioShantanuNo ratings yet
- NCM 104 Family Nursing Care PlanDocument8 pagesNCM 104 Family Nursing Care PlanMa RieNo ratings yet
- Health and Safety CultureDocument2 pagesHealth and Safety CultureAbdul WahabNo ratings yet
- PEDIATRIC AUDIOLOGY WEEKLY TOPICSDocument3 pagesPEDIATRIC AUDIOLOGY WEEKLY TOPICSAhiawortor KplorlaNo ratings yet
- Adolescent Romantic Relationships (Article) Author Sarah SorensenDocument4 pagesAdolescent Romantic Relationships (Article) Author Sarah SorensenDavidNo ratings yet