Professional Documents
Culture Documents
Capillary Blood Glucose
Uploaded by
Dennis Cobb0 ratings0% found this document useful (0 votes)
539 views4 pagesImproving diabetic control can significantly reduce the risk of microvascular complications (kidney, nerve and eye damage) good blood glucose control has been shown to be associated with more favourable clinical outcomes in patients who have acute cardiovascular events. The procedure blood specimens are obtained using a finger pricking device and results are analysed by a near patient blood glucose meter.
Original Description:
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentImproving diabetic control can significantly reduce the risk of microvascular complications (kidney, nerve and eye damage) good blood glucose control has been shown to be associated with more favourable clinical outcomes in patients who have acute cardiovascular events. The procedure blood specimens are obtained using a finger pricking device and results are analysed by a near patient blood glucose meter.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
539 views4 pagesCapillary Blood Glucose
Uploaded by
Dennis CobbImproving diabetic control can significantly reduce the risk of microvascular complications (kidney, nerve and eye damage) good blood glucose control has been shown to be associated with more favourable clinical outcomes in patients who have acute cardiovascular events. The procedure blood specimens are obtained using a finger pricking device and results are analysed by a near patient blood glucose meter.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 4
Wallymahmed M (2007) Capillary blood glucose monitoring. Nursing Standard. 21, 38, 35-38.
Date of acceptance: December 15 2006.
patients with type 1 and type 2 diabetes especially
during periods of instability, for example, illness or
frequent hypoglycaemia. Improving diabetic
control can significantly reduce the risk of
microvascular complications (kidney, nerve and
eye damage) in patients with type 1 and type 2
diabetes (Diabetes Control and Complications
Trial (DCCT) Research Group 1993, UK
Prospective Diabetes Study (UKPDS) Group
1998). In addition, good blood glucose control has
been shown to be associated with more favourable
clinical outcomes in patients who have acute
cardiovascular events such as myocardial
infarction and stroke (Malmberg et al 1995).
The procedure
Blood specimens are obtained using a finger
pricking device and results are analysed by a near
patient blood glucose meter. A variety of meters
are available and to ensure accuracy of results the
manufacturers advice must be followed carefully.
Serious errors, leading to inappropriate
management decisions, have been identified and
the Department of Health (DH) has issued hazard
warnings. These warnings highlight the need
for staff training and formal quality control
programmes (DH 1987, Medical Devices Agency
(MDA) 1996). The MDA (2002) has issued
recommendations for the training of staff using
point of care devices such as blood glucose
meters. These recommendations include
education and training in the following areas:
Knowledge of what results to expect in normal
and abnormal situations.
Correct use of equipment and knowledge of the
consequences of incorrect use.
Instruction in the collection of blood samples
including gaining consent and health and safety
issues.
The importance of documentation of results.
Capillary blood glucose monitoring
may 30 :: vol 21 no 38 :: 2007 35 NURSING STANDARD
BLOOD GLUCOSE levels are normally
maintained within relatively narrow limits at
about 5-7mmol/l (Williams and Pickup 2004).
Insulin and glucagon, produced by the pancreas,
are largely responsible for the regulation of blood
glucose. Insulin is synthesised in and secreted
from the beta cells within the islets of Langerhans.
Insulin levels are low during periods of fasting
with increased stimulated levels in response to
high blood glucose levels, for example, after
meals. Glucagon is secreted by the alpha cells in
response to low blood glucose levels and inhibited
by high blood glucose levels.
Rationale
Capillary blood glucose monitoring is a convenient
way of monitoring blood glucose patterns and can
be a useful aid in guiding treatment changes in
Summary
This article, the first in a series of articles relating to clinical skills
in nursing, outlines the procedure of capillary blood glucose
monitoring. This is a convenient way of monitoring blood glucose
patterns and can be a useful aid in guiding treatment changes in
patients with type 1 and type 2 diabetes, especially during periods
of illness or frequent hypoglycaemia.
Author
Maureen Wallymahmed is nurse consultant, Aintree Hospitals NHS
Trust, Diabetes Centre, Walton Hospital, Liverpool.
Email: maureen.wallymahmed@aintree.nhs.uk
Keywords
Blood glucose monitoring; Clinical procedures; Diabetes;
Hyperglycaemia; Hypoglycaemia
These keywords are based on the subject headings from the British
Nursing Index. This article has been subject to double-blind review.
For author and research article guidelines visit the Nursing Standard
home page at www.nursing-standard.co.uk. For related articles
visit our online archive and search using the keywords.
If you would like to contribute to the art and science section contact: Gwen Clarke, art and science editor, Nursing Standard,
The Heights, 59-65 Lowlands Road, Harrow-on-the-Hill, Middlesex HA1 3AW. email: gwen.clarke@rcnpublishing.co.uk
p35-38w38 22/5/07 2:21 pm Page 35
A knowledge of the meters limitations and
when use is contraindicated.
An in-depth knowledge of the individual
meter, including error codes, calibration and
quality control techniques.
Staff performing blood glucose monitoring should
also be involved in a formal quality control
programme. This involves performing and
documenting quality control checks in the clinical
area using specific high and low quality control
solutions on a daily basis. This is known as
internal quality control. External quality control
programmes should also be in operation. These
involve solutions of an unknown glucose level
being sent from the laboratories to the clinical
areas on a regular basis. Each user should perform
a quality control test and return the result to the
laboratory. In this way inaccurate performance
can be identified and additional training arranged.
Each trust has a responsibility to develop and
implement a training and quality control
programme for all staff performing capillary
blood glucose monitoring.
Indications Capillary blood glucose monitoring
is indicated in the following situations:
Day-to-day management of patients with type
1 and type 2 diabetes.
Detection of hypoglycaemia.
Detection of persistent hyperglycaemia, for
example, during periods of illness.
Management of acute complications of
diabetes causing metabolic decompensation,
for example, diabetic ketoacidosis and
hyperosmolar non-ketotic coma (once severe
dehydration is corrected).
Management of patients during periods of
fasting, for example, surgery when a glucose-
potassium-insulin regimen may be required.
It is important to note that a diagnosis of diabetes
should not be made on the basis of a capillary
blood glucose measurement obtained using a
blood glucose meter. While meters are
convenient and readily available, there is
potential for error and the diagnosis should be
confirmed on a laboratory specimen. Blood
glucose levels for the diagnosis of diabetes and
other categories of glucose intolerance have been
agreed by the World Health Organization
(Alberti and Zimmet 1998). In the UK it is
estimated that there are currently more than two
million people with diagnosed diabetes and up
to 750,000 who have diabetes but are not yet
diagnosed (Diabetes UK 2006). Other possible
indications for capillary blood glucose
monitoring:
Patients taking medications such as steroids
and atypical antipsychotics which can cause
blood glucose levels to rise.
Specific situations, for example, parenteral
feeding which can lead to a rise in blood
glucose levels.
Contraindications Staff performing capillary
blood glucose monitoring should be aware that
the accuracy of results can be affected by the
following clinical conditions (MDA 1996):
Peripheral circulatory failure and severe
dehydration, for example, diabetic
ketoacidosis, hyperosmolar non-ketotic coma,
shock and hypotension. In these situations
capillary blood glucose readings can be
artificially low due to peripheral shut down.
Haematocrit values above 55% may lead to
inaccurate results if the blood glucose level
is more than 11mmol/l.
Intravenous (IV) infusion of ascorbic acid.
Pre-eclampsia.
Some treatments for renal dialysis.
Hyperlipidaemia cholesterol levels above
13mmol/l may lead to artificially raised
capillary blood glucose readings.
Capillary blood glucose monitoring should only
be performed by staff who have undergone
formal training as agreed by each trust (Table 1).
Hypoglycaemia:low blood glucose
Hypoglycaemia occurs when blood glucose
levels fall below 4mmol/l and should be treated
promptly. It can occur in patients on insulin and
sulphonylureas. Causes of hypoglycaemia
include missed or late meals, not eating enough,
taking too much insulin or tablets, exercise and
excessive alcohol. Common manifestations
include sweating, shaking, palpitations, hunger
and poor concentration. Hypoglycaemia should
be treated with fast-acting carbohydrate, for
example, three to six glucose tablets, 150ml fizzy
drink or 50-100ml Lucozade and followed up
with some longer-acting carbohydrate such as
biscuits or a sandwich. Blood glucose should be
recorded five to ten minutes after treatment.
Severe hypoglycaemia can be managed with
intramuscular glucagon or IV dextrose.
It is important to remember that bedside blood
glucose meters are not always accurate at low
readings and that hypoglycaemia should be
36 may 30 :: vol 21 no 38 :: 2007 NURSING STANDARD
&
art &science clinical skills: 1
p35-38w38 22/5/07 2:21 pm Page 36
may 30 :: vol 21 no 38 :: 2007 37 NURSING STANDARD
TABLE 1
Capillary blood glucose monitoring procedure
Action
Check that the blood glucose meter is ready for use. Ensure the following:
The test strips are in date, have been stored correctly and have not been exposed to
the air (this does not apply to strips that are individually wrapped).
The monitor is calibrated for use* with the pack of strips in use.
If a new pack of strips is required ensure the machine is recalibrated.
Quality control tests (high and low) have been carried out and documented on that day.
*Some meters use test strips that have an automatic calibration system while others
need to be recalibrated when a new pack of strips is opened.
Refer to manufacturers instructions for information.
Ensure that you have the following equipment:
Blood glucose meter (as above).
Test strips.
Finger pricking device or lancets.
Cotton wool.
Sharps disposal container.
Gloves.
Prepare the patient
Describe the procedure to the patient, explain why it is needed, answer any questions and
gain verbal consent. Ask the patient to wash his or her hands in warm, soapy water and dry
thoroughly. Do not use alcohol swabs or rub as this can lead to an inaccurate result. Position
the patient comfortably.
Wash your hands and put on protective gloves
Take a sample of blood
Using a single use, retractable lancet take a sample from the side of the finger. If the finger
does not bleed readily, milk the finger until enough blood is obtained. Most strips need only
a small volume of blood for accurate testing (0.3-4l).
Apply the blood to the test strip
Most strips are now hydrophilic. The tip of the strip is gently applied to the drop of blood
and the blood is sucked up automatically, stopping when the correct volume of blood has
been obtained. However, some strips still require the blood to be dropped directly onto the
reagent strip.
Dispose of the lancet in the sharps disposal container
When the result is available record on the appropriate charts/nursing documentation
Dispose of waste, for example, gloves and cotton wool, appropriately
Observe the test site for bleeding, ensure that the patient is comfortable and explain the
result as required
Report any unexpected, out of range results to the nurse in charge
Results that are outside the expected range for an individual patient should be reported to
the nurse in charge and appropriate action taken.
Rationale
To ensure maximum efficiency, patient
comfort and safety.
To reduce anxiety and ensure that the
patient is aware of the reasons for
blood glucose monitoring.
To prevent cross-infection and reduce
the risk of contamination.
A single use retractable lancet is
recommended to reduce the risk of
needlestick injury and cross-infection.
The side of the finger is generally less
sensitive than the tip and sensitivity in
tips of fingers may be lost if used
regularly. Rotation of sites is advised
to avoid over use of one site as the
skin may become hard and painful.
To obtain an accurate blood
glucose measurement.
To reduce the risk of needlestick injury
and cross-infection.
To ensure accurate recording of results
which may influence management.
To reduce the risk of cross-infection.
To ensure that the patient is
comfortable and aware of the blood
glucose result. This is important
because many patients self-monitor
blood glucose at home and make
adjustments to insulin accordingly.
To ensure patient safety.
p35-38w38 22/5/07 2:21 pm Page 37
considered in patients with typical symptoms.
Diabetic treatment should not be omitted because
of a single hypoglycaemic episode; the
hypoglycaemia should be treated and the usual
medication given. However, if hypoglycaemia
occurs frequently a review of the patients
treatment should be sought.
Hyperglycaemia:raised blood glucose
Intercurrent illness can have an effect on
glycaemic control causing blood sugars to rise
and can lead to diabetic ketoacidosis especially
in patients with type 1 diabetes. If blood glucose
is persistently raised, the patients urine should
be tested for ketones and advice sought from
the diabetes team. If vomiting and diarrhoea
are present, dehydration can occur quickly
and advice should be sought. Other causes of
hyperglycaemia include systemic steroids,
dietary factors, non-concordance with
medication and stress.
Frequency of monitoring
All hospital inpatients with diabetes need regular
blood glucose monitoring because acute illness
can seriously affect blood glucose levels. The
frequency of monitoring should be decided on an
individual patient basis depending on the clinical
condition. However, on admission to hospital it
is advisable to monitor capillary blood glucose
four times a day pre-meal and pre-bed for 48
hours and then to review the frequency of
monitoring according to the results and the
patients condition. Patients being cared for at
home should have blood glucose monitoring
according to individual need.
Glycosylated haemoglobin
Glycosylated haemoglobin (HbA
1c
) is a
measurement of long-term diabetic control. This
blood test measures the percentage of
haemoglobin bound to glucose and is useful as it
reflects about two to three months of blood
glucose control. Target HbA
1c
levels are
6.5-7.5% depending on individual
circumstances, for example, complications
(National Institute for Clinical Excellence 2002,
2004). In addition to HbA
1c
and capillary blood
glucose monitoring, the following should be
considered when monitoring control: symptoms,
frequency of hypoglycaemia and weight. As
acute illness can adversely affect blood sugar
control, it is useful for all inpatients with diabetes
to have a HbA
1c
blood test while in hospital.
Conclusion
Capillary blood glucose monitoring is a useful
tool in the management of patients with diabetes.
However, there is potential for serious error if the
procedure is not followed correctly. All staff
performing capillary blood glucose monitoring
should be trained and assessed according to trust
policy, be aware of what results to expect and
when to seek advice NS
38 may 30 :: vol 21 no 38 :: 2007 NURSING STANDARD
&
art &science clinical skills: 1
Alberti KG, Zimmet PZ (1998)
Definition, diagnosis and
classification of diabetes mellitus
and its complications. Part 1:
diagnosis and classification of
diabetes mellitus provisional report
of a WHO consultation. Diabetic
Medicine. 15, 7, 539-553.
Department of Health (1987)
Blood Glucose Measurements:
Reliability of Results Produced in
Extra-laboratory Areas. DHSS
Hazard Notice 15 October. NHS
Procurement Directorate DHSS
Blood Glucose Measurement
Department of Health and Social
Security, London.
Diabetes Control and
Complications Trial Research
Group (1993) The effect of
intensive treatment of diabetes on
the development and progression of
long-term complications in insulin
dependent diabetes mellitus. New
England Journal of Medicine. 329,
14, 977-986.
Diabetes UK (2006) What is
Diabetes? www.diabetes.org.uk/
Guide-to-diabetes/What_is_
diabetes/What_is_diabetes/ (Last
accessed: May 10 2007.)
Malmberg K, Ryden L, Efendic S
et al (1995) Randomized trial of
insulin-glucose infusion followed by
subcutaneous insulin treatment in
diabetic patients with acute
myocardial infarction (DIGAMI
study): effects on mortality at 1
year. Journal of the American
College of Cardiology. 26, 1, 57-65.
Medical Devices Agency (1996)
Extra-laboratory Use of Blood
Glucose Meters and Test Strips:
Contra-indications, Training and
Advice to the Users. Safety Notice
MDA SN 9616. www.mhra.gov.uk/
home/idcplg?IdcService=SS_GET_P
AGE&useSecondary=true&ssDocNa
me=CON2022746&ssTargetNodeId
=420 (Last accessed: May 1 2007.)
Medical Devices Agency (2002)
Management and Use of IVD Point
of Care Test Devices. The Stationery
Office, London.
National Institute for Clinical
Excellence (2002) Management of
Type 2 Diabetes. Management of
Blood Glucose. NICE, London.
National Institute for Clinical
Excellence (2004) Type 1 Diabetes:
Diagnosis and Management of Type
1 Diabetes in Children, Young People
and Adults. NICE, London.
United Kingdom Prospective
Diabetes Study Group (1998)
Intensive blood glucose control with
sulphonylureas or insulin compared
with conventional treatment and
risk of complications in patients
with type 2 diabetes (UKPDS 33).
The Lancet. 352, 9131, 837-853.
Williams G, Pickup JC (Eds)
(2004) Handbook of Diabetes. Third
edition. Blackwell Publishing, Oxford.
References
p35-38w38 22/5/07 2:21 pm Page 38
You might also like
- Impaired Tissue Perfusion Related To The Weakening / Decreased Blood Flow To The Area of Gangrene Due To Obstruction of Blood VesselsDocument3 pagesImpaired Tissue Perfusion Related To The Weakening / Decreased Blood Flow To The Area of Gangrene Due To Obstruction of Blood VesselsKat AlaNo ratings yet
- Case StudyDocument49 pagesCase StudyLennie Marie B Pelaez100% (1)
- CystoclysisDocument2 pagesCystoclysisRaymond BasiloniaNo ratings yet
- Mcdonald Case StudyDocument12 pagesMcdonald Case StudyJohn WickNo ratings yet
- NCP Micu Hascvd Cad - RioDocument5 pagesNCP Micu Hascvd Cad - RioRio BonifacioNo ratings yet
- A Project Proposal On Case Study and Management of A Type 1 Diabetes Mellitus ClientDocument6 pagesA Project Proposal On Case Study and Management of A Type 1 Diabetes Mellitus ClientMichael Kivumbi100% (3)
- Recurrent PAF Case StudyDocument3 pagesRecurrent PAF Case StudyDanae Kristina Natasia BangkanNo ratings yet
- Blood Glucose MonitoringDocument30 pagesBlood Glucose MonitoringVictoria Castillo TamayoNo ratings yet
- Risk Factors and Treatments for Alzheimer's DiseaseDocument3 pagesRisk Factors and Treatments for Alzheimer's DiseaseKristian Karl Bautista Kiw-isNo ratings yet
- Alc Intra1 Questionnaire HypertensiveDocument5 pagesAlc Intra1 Questionnaire HypertensiveAndrea Blanca100% (1)
- Nursing Care Plan for Patient with Risk of BleedingDocument11 pagesNursing Care Plan for Patient with Risk of BleedingKimsha ConcepcionNo ratings yet
- HemodialysisDocument2 pagesHemodialysisJanelle MarceraNo ratings yet
- Medication and Health Teaching Discharge PlanDocument1 pageMedication and Health Teaching Discharge PlanBernalene SyNo ratings yet
- Drug Study On DigoxinDocument8 pagesDrug Study On DigoxinDonald BidenNo ratings yet
- Health TeachingDocument3 pagesHealth TeachingNyj QuiñoNo ratings yet
- Different Iv FluidsDocument2 pagesDifferent Iv FluidsBeverly DatuNo ratings yet
- CBI Procedure Guide for NursesDocument9 pagesCBI Procedure Guide for NursesAlvin OccianoNo ratings yet
- Giving of Medication 12 RightsDocument41 pagesGiving of Medication 12 RightsLeslie PaguioNo ratings yet
- Bioethical Components of CareDocument2 pagesBioethical Components of CarekeiitNo ratings yet
- Galvus Met TabDocument23 pagesGalvus Met TabMaria Nicole EconasNo ratings yet
- Selecting the Right IV Catheter SizeDocument1 pageSelecting the Right IV Catheter SizeRafael BagusNo ratings yet
- CNN Practice QuestionsDocument5 pagesCNN Practice QuestionsUri Perez MontedeRamosNo ratings yet
- Capillary Blood Glucose Monitoring or CBG MonitoringDocument5 pagesCapillary Blood Glucose Monitoring or CBG MonitoringRonilyn Mae Alvarez100% (1)
- Urinalysis Procedure & ResultsDocument6 pagesUrinalysis Procedure & ResultsbobtagubaNo ratings yet
- HemodialysisDocument3 pagesHemodialysisReem NurNo ratings yet
- Skill Performance Evaluation - Measuring Intake and OutputDocument2 pagesSkill Performance Evaluation - Measuring Intake and OutputLemuel Que100% (1)
- Nursing Responsibilities For Oxygen AdministrationDocument3 pagesNursing Responsibilities For Oxygen AdministrationJahseh WolfeNo ratings yet
- Ranitidine, ParacetamolDocument3 pagesRanitidine, ParacetamoltaekadoNo ratings yet
- G-CFA Instructor Tab 6-2 Handout 2 Sample Adequate Nursing Care Plan-R6Document2 pagesG-CFA Instructor Tab 6-2 Handout 2 Sample Adequate Nursing Care Plan-R6SriMathi Kasi Malini ArmugamNo ratings yet
- Gunshot Wound PeritonitisDocument66 pagesGunshot Wound PeritonitisMia Charisse FigueroaNo ratings yet
- Gastrointestinal System Disorders NCLEX Practice - Quiz #2 - 50 Questions - NurseslabsDocument52 pagesGastrointestinal System Disorders NCLEX Practice - Quiz #2 - 50 Questions - NurseslabsGypsy Joan TranceNo ratings yet
- IV FluidsDocument1 pageIV FluidsJhensczy Hazel Maye AlbaNo ratings yet
- Metformin Medication Guide - Uses, Side Effects, DosageDocument5 pagesMetformin Medication Guide - Uses, Side Effects, DosageAgronaSlaughterNo ratings yet
- Clinical Example:: What Additional Assessments Would The Nurse Want To Make To Plan Care For This Client?Document2 pagesClinical Example:: What Additional Assessments Would The Nurse Want To Make To Plan Care For This Client?Kim Kristine D. GuillenNo ratings yet
- Perioperative Risks & InterventionsDocument5 pagesPerioperative Risks & InterventionsJellou MacNo ratings yet
- Hyperosmolar Hyperglycemic State (HHS)Document21 pagesHyperosmolar Hyperglycemic State (HHS)Malueth AnguiNo ratings yet
- Discharge Plan for Stage 4 Lung Cancer and COPDDocument7 pagesDischarge Plan for Stage 4 Lung Cancer and COPDinah krizia lagueNo ratings yet
- DialysisDocument21 pagesDialysisReygie MarsadaNo ratings yet
- Liver Cirrhosis Care PlanDocument3 pagesLiver Cirrhosis Care PlanWendy EscalanteNo ratings yet
- Thoracentesis Reflective EssayDocument2 pagesThoracentesis Reflective EssayAnjae GariandoNo ratings yet
- Operating RoomDocument13 pagesOperating RoomrichardNo ratings yet
- EndocrinedisorderDocument3 pagesEndocrinedisorderDyan LazoNo ratings yet
- Lesson 1 POST TEST Maternal FrameworkDocument1 pageLesson 1 POST TEST Maternal FrameworkAnnalisa TellesNo ratings yet
- Case PresentationDocument138 pagesCase PresentationrinlopenaiNo ratings yet
- Daily Assignment PlanDocument2 pagesDaily Assignment PlanIvanne HisolerNo ratings yet
- Discharge Plan EndoDocument3 pagesDischarge Plan EndoCharlayne AnneNo ratings yet
- Drug Study Case 1Document37 pagesDrug Study Case 1Maria Charis Anne IndananNo ratings yet
- Nursing Management Pancreatic CancerDocument2 pagesNursing Management Pancreatic CancerKit NameKo100% (2)
- Chapter 1 Fundamental Concepts SPSS - Descriptive StatisticsDocument4 pagesChapter 1 Fundamental Concepts SPSS - Descriptive StatisticsAvinash AmbatiNo ratings yet
- Naso & Orogastric Tube Placement, Testing & FeedingDocument10 pagesNaso & Orogastric Tube Placement, Testing & FeedingYwagar Ywagar100% (1)
- Lowers Abnormal Lipid LevelsDocument34 pagesLowers Abnormal Lipid Levelschelle_morales260% (1)
- Fasting Blood Glucose TestDocument10 pagesFasting Blood Glucose TestBrylle ArbasNo ratings yet
- Anaphylaxis (Case)Document4 pagesAnaphylaxis (Case)drkmwaiNo ratings yet
- Nursing Care PlanDocument8 pagesNursing Care PlanVincent QuitorianoNo ratings yet
- NCM 114 RevsDocument8 pagesNCM 114 RevsKryza B. CASTILLONo ratings yet
- Blood GlucoseDocument5 pagesBlood Glucoseediting visualsNo ratings yet
- Laboratory/Diagnostic Exams: WORKSHEET ON Endocrine System DisordersDocument153 pagesLaboratory/Diagnostic Exams: WORKSHEET ON Endocrine System DisorderskdfhjfhfNo ratings yet
- Laboratory Diagnosis and Monitoring Type 2 Diabetes Mellitus - SEKAR EMSDocument29 pagesLaboratory Diagnosis and Monitoring Type 2 Diabetes Mellitus - SEKAR EMSRaja Iqbal Mulya HarahapNo ratings yet
- Blood Glucose MonitoringDocument11 pagesBlood Glucose MonitoringHannaNo ratings yet
- Sistemik CaranzaDocument9 pagesSistemik CaranzawulanNo ratings yet
- Treatment of Sternal Wound Infections After Open-Heart SurgeryDocument6 pagesTreatment of Sternal Wound Infections After Open-Heart SurgeryDennis CobbNo ratings yet
- Managing mediastinitis after cardiac surgeryDocument4 pagesManaging mediastinitis after cardiac surgeryDennis CobbNo ratings yet
- Tugas Individu Anggun PDFDocument6 pagesTugas Individu Anggun PDFAnggun PermatasariNo ratings yet
- Assessment Constipation PDFDocument6 pagesAssessment Constipation PDFDennis CobbNo ratings yet
- APGARDocument1 pageAPGARblazegomezNo ratings yet
- User Training AED ProDocument46 pagesUser Training AED ProDennis CobbNo ratings yet
- Trend Management Patient of Transposition Great ArteryDocument3 pagesTrend Management Patient of Transposition Great ArteryDennis CobbNo ratings yet
- Assessment Constipation PDFDocument6 pagesAssessment Constipation PDFDennis CobbNo ratings yet
- Content 8902 PDFDocument6 pagesContent 8902 PDFabdulNo ratings yet
- Arf Post CabgDocument19 pagesArf Post CabgDennis CobbNo ratings yet
- Fluid Afterload After CabgDocument6 pagesFluid Afterload After CabgDennis CobbNo ratings yet
- Autonomy of Nurse PDFDocument8 pagesAutonomy of Nurse PDFDennis CobbNo ratings yet
- Respiration Disorder PDFDocument14 pagesRespiration Disorder PDFDennis CobbNo ratings yet
- Transient Ischemic PDFDocument8 pagesTransient Ischemic PDFDennis CobbNo ratings yet
- Post Cardiac ComplicationsDocument6 pagesPost Cardiac ComplicationsGull GillNo ratings yet
- CPR Nurse LawDocument6 pagesCPR Nurse LawIpar DayNo ratings yet
- Early Postopcare After Cardiac Surgery PDFDocument23 pagesEarly Postopcare After Cardiac Surgery PDFDennis CobbNo ratings yet
- Liver Cirrhosis PDFDocument9 pagesLiver Cirrhosis PDFDennis CobbNo ratings yet
- Cognitive Impairment PDFDocument4 pagesCognitive Impairment PDFDennis CobbNo ratings yet
- Avian InfluenzaDocument6 pagesAvian InfluenzaDennis CobbNo ratings yet
- Autonomy of Nurse PDFDocument8 pagesAutonomy of Nurse PDFDennis CobbNo ratings yet
- ArdsDocument7 pagesArdsIpar DayNo ratings yet
- Avian InfluenzaDocument6 pagesAvian InfluenzaDennis CobbNo ratings yet
- Best Practice in The Use of SpirometryDocument6 pagesBest Practice in The Use of SpirometryDennis CobbNo ratings yet
- Cardiac ArrhythmiaDocument5 pagesCardiac ArrhythmiaDennis CobbNo ratings yet
- Atrial FibrilationDocument10 pagesAtrial FibrilationDennis CobbNo ratings yet
- Heart NotesDocument13 pagesHeart NotesDennis CobbNo ratings yet
- Marfan's Syndrome Signs and Symptoms: EtiologyDocument3 pagesMarfan's Syndrome Signs and Symptoms: EtiologyDennis CobbNo ratings yet
- Avian InfluenzaDocument6 pagesAvian InfluenzaDennis CobbNo ratings yet
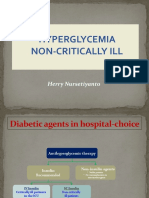
- Non-Critically Ill Hyperglycemia ManagementDocument39 pagesNon-Critically Ill Hyperglycemia ManagementHerry KongkoNo ratings yet
- Impact of Pharmacist Insulin Management On Hemoglobin A1c in Outpatient Hospital Clinic SettingDocument7 pagesImpact of Pharmacist Insulin Management On Hemoglobin A1c in Outpatient Hospital Clinic SettingSabrina JonesNo ratings yet
- Continuous Glucose Monitoring Devices For Patients With Diabeles Mellitus On InsulinDocument25 pagesContinuous Glucose Monitoring Devices For Patients With Diabeles Mellitus On InsulinCalifornia Technology Assessment ForumNo ratings yet
- Insulin Therapy Guide 2Document3 pagesInsulin Therapy Guide 2AimanRiddleNo ratings yet
- DR Bernstein SolutionDocument7 pagesDR Bernstein Solutionev.adilsonNo ratings yet
- Handy Health Guide To DiabetesDocument49 pagesHandy Health Guide To DiabetesDiabetes Care100% (1)
- Hypoglycemia - Prevention - Practi2 NewDocument17 pagesHypoglycemia - Prevention - Practi2 NewfitrianiNo ratings yet
- Management of Diabetic Cats With Long Acting InsulinDocument16 pagesManagement of Diabetic Cats With Long Acting Insulindia_dianneNo ratings yet
- OBAT INJEKSI AmyDocument4 pagesOBAT INJEKSI AmyKlinik MMCNo ratings yet
- Clinical Learning Log 3 Go Solo - Docx-1Document11 pagesClinical Learning Log 3 Go Solo - Docx-1JezraleFame AntoyNo ratings yet
- Quick Reference Guide - Management of Diabetes 1 2022 Version FINALDocument20 pagesQuick Reference Guide - Management of Diabetes 1 2022 Version FINALHigh Class Education (H.C.Education)No ratings yet
- Treatment of Diabetes Mellitus T2 - Samir RaflaDocument35 pagesTreatment of Diabetes Mellitus T2 - Samir Raflasamir raflaNo ratings yet
- Journal Reading Sharon Angelica C (2295015)Document34 pagesJournal Reading Sharon Angelica C (2295015)Sharon Angelica CarolineNo ratings yet
- 852-Article Text-1782-1-10-20221103Document11 pages852-Article Text-1782-1-10-20221103ritaNo ratings yet
- Disclosure: Complex Case: Complications After Cardiac Surgery - Glucose, Sedation and ThrombocytopeniaDocument27 pagesDisclosure: Complex Case: Complications After Cardiac Surgery - Glucose, Sedation and ThrombocytopeniaEnrique SánchezNo ratings yet
- Guidelines and Protocols Of: Diabetes EmergenciesDocument36 pagesGuidelines and Protocols Of: Diabetes Emergenciesyassen hassanNo ratings yet
- Diabetes Mellitus Study GuideDocument5 pagesDiabetes Mellitus Study Guiderr5633No ratings yet
- Addressing Hypoglycemia in Type 1 DiabeticsDocument2 pagesAddressing Hypoglycemia in Type 1 DiabeticsTina WuNo ratings yet
- Media Video Makanan Terhadap Pengetahuan Dan Kepatuhan Diet Serta Pengendalian Kadar Glukosa Darah Pasien Diabetes Melitustipe IIDocument7 pagesMedia Video Makanan Terhadap Pengetahuan Dan Kepatuhan Diet Serta Pengendalian Kadar Glukosa Darah Pasien Diabetes Melitustipe IIpricillia sambekaNo ratings yet
- BMC Endocrine Disorders: Exploring How Patients Understand and Assess Their Diabetes ControlDocument31 pagesBMC Endocrine Disorders: Exploring How Patients Understand and Assess Their Diabetes Controlmaha altweileyNo ratings yet
- (MM2016-3-73) Artur Chwalba, Ewa Otto-Buczkowska: Nowe, Pediatryczne Wskazania Do Stosowania Metforminy - Systematyczny PrzeglądDocument6 pages(MM2016-3-73) Artur Chwalba, Ewa Otto-Buczkowska: Nowe, Pediatryczne Wskazania Do Stosowania Metforminy - Systematyczny PrzeglądTowarzystwo Edukacji TerapeutycznejNo ratings yet
- Farmakologi DMDocument41 pagesFarmakologi DMZainul MuttaqinNo ratings yet
- Diabetic Ketoacidosis Case StudyDocument6 pagesDiabetic Ketoacidosis Case StudyJohn AlcantaraNo ratings yet
- Diabetis 2Document33 pagesDiabetis 2Fercho MedNo ratings yet
- Shaukat Khanum Memorial Cancer Hospital & Research Centre ReportDocument1 pageShaukat Khanum Memorial Cancer Hospital & Research Centre ReportusmannnnNo ratings yet
- A Descriptive Study To Assess The Knowledge and Attitude Regarding Self Administration of Insulin Injection Among Diabetes Mellitus Patients in Rural Area at DehradunDocument5 pagesA Descriptive Study To Assess The Knowledge and Attitude Regarding Self Administration of Insulin Injection Among Diabetes Mellitus Patients in Rural Area at DehradunEditor IJTSRDNo ratings yet
- Jcem 0709Document20 pagesJcem 0709Rao Rizwan ShakoorNo ratings yet
- Diabetes 101 - An Overview of Diabetes and Its Management - Michael SeeDocument88 pagesDiabetes 101 - An Overview of Diabetes and Its Management - Michael SeeSangar MahmoodNo ratings yet
- Carbohydrate To Insulin Ratio - Breakfast-Lunch-DinnerDocument5 pagesCarbohydrate To Insulin Ratio - Breakfast-Lunch-Dinnermario rodriguezNo ratings yet
- Deteksi Dini KomplikasiDocument70 pagesDeteksi Dini KomplikasiWiwik Puji LestariNo ratings yet