Professional Documents
Culture Documents
Bme464 Notes
Uploaded by
James BrooksCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Bme464 Notes
Uploaded by
James BrooksCopyright:
Available Formats
BME464: Medical Imaging
John DiCecco, PhD
Department of Electrical, Computer, and Biomedical Engineering
University of Rhode Island
Kingston, RI USA
diceccoj@ele.uri.edu
September 25, 2014
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 1 / 89
Introduction
Medical Imaging Systems (The Physics of Medical Imaging,
Webb)
Conventional X-rays
Nuclear Medicine
Imaging of radiopharmaceuticals
Diagnostic Ultrasound
Magnetic Resonance Imaging (MRI)
Medical Image Processing
Backprojection, Radon Transform, Convolution, ltering, etc.
Computer Requirements
Student Image Processing Project (More later)
Grading Exam 1, Exam 2, Exam 3 (nal), and Project
25% each
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 2 / 89
Why Imaging?
Heart disease: 597,689
Cancer: 574,743
Chronic lower respiratory diseases: 138,080
Stroke (cerebrovascular diseases): 129,476
Accidents (unintentional injuries): 120,859
Alzheimers disease: 83,494
Diabetes: 69,071
Nephritis, nephrotic syndrome, and nephrosis: 50,476
Inuenza and Pneumonia: 50,097
Intentional self-harm (suicide): 38,364
Septicemia: 35,539
Chronic liver disease: 33,539
Essential hypertension and hypertensive renal disease: 27,477
Parkinsons disease: 23,107
Pneumonitis due to solids and liquids: 18,090
All other causes: 512,723
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 3 / 89
History of Medical Imaging
1895 - Discovery of x-rays (Wilhelm Rontgen)
1905 - Subtraction Radiogram (DSA)
1917 - Radon Transform
1937 - Xeroradiograhpy (patent)
1946 - NMR principle
1950 - Scintillation imaging (-camera)
1952 - 2D Ultrasound Imaging
1953 - Positron Tomography
1957 - Anger () camera using Sodium Iodide Crystals
1958 - X-ray CT
1961 - Oldendorf - laboratory X-ray CT
1963 - SPET (analog)
1971 - SPECT
1972 - First commercial X-ray CT (Ambrose and Hounseld)
1979 - Nobel prize to Hounseld and Cormack
1976 - MRI (Manseld & Maudsley) - ex-vivo nger
1978 - Commercial version
1982 - Impedance Tomography
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 4 / 89
Cardiology
Cardiac Ultrasound Images - Echo and Doppler
Non-invasive but poor resolution
Mitral (bicuspid), tricuspid valve regurgitation, ow
Angiogram - Catheterization
Percutaneous Transluminal Coronary Angioplasty (PTCA)
AKA Balloon Angioplasty
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 5 / 89
3D
CT Scan (Computed Tomography, or Computer Axial
Tomography (CAT))
MRI (with/without contrast, typically varying paramagnetism)
Dynamic Spatial Reconstructor (Mayo Clinic)
14 image intensied X-ray tubes
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 6 / 89
Photons (EM waves)
Media to make human body semi-opaque
Visible light (3800
A- 7600
A) human body is opaque
400 800 THz
1.6 3.28 eV
Recall:
E = hv =
hc
(1)
h = 6.626 10
34
J s = 4.14 10
15
eV s (2)
c = 3 10
8
m/s(speedoight) (3)
E(eV) =
1.24 10
6
(m)
eV (4)
1.24 10
6
(m)
=
1240
(nm)
eV (5)
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 7 / 89
Photons (EM waves) (cont.)
Recall human body is opaque to visible light
Cosmic Rays (10
11
Ato 10
16
A) human
body is transparent
Energy is 10
15
10
20
eV
1 eV = 1.6 10
12
erg = 1.6 10
19
joules
Charge on an electron is 1.6 10
19
C
X-rays (energy 0.1 123 keV, 0.1
A 100
A) human body is semi-opaque
Trade-o between X-ray dose and SNR
radioactive isotope (Tc - 140 keV, Ga - 511
keV after positron electron annihilation)
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 8 / 89
Chapter Two - Diagnostic Radiology with X-ray
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 9 / 89
Three Types of Interactions Between X-ray and Tissue
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 10 / 89
Three Types of Interactions Between X-ray and Tissue
Photoelectric interaction - ionization eect (photoionization)
Transmitted - passes through unaected (Primary)
Scattered - interacts with tissue or bone and passes through
(Secondary)
Absorbed - this is the delivery dose and is responsible for the
damage
The characteristic x-ray may not be always be absorbed but
the ionized electron almost always will be
Mean free path of electron in water is 0.03 cm
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 11 / 89
Dose Versus Contrast Trade-o
Low Energy Photons - Only a few get through
Good contrast but to get enough photons to the detector,
HIGH DOSE
In case youre not sure, high dose is BAD
High Energy Photons - Most get through
Poor contrast
Good news is low dose to patient
Bad news is unusable image - colossal waste of time
X-ray energy determined by
X-ray target material, W(high), Mo(low)
X-ray tube potential (how much voltage is supplied)
Filtration (screening) - typically Al or Cu, with Al preferred for
medical imaging (lower atomic number, control with thickness)
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 12 / 89
Dose Versus Contrast Trade-o
For CT scan, can take advantage
of redundant information
Image processing can lter low
contrast images
Image at right current GE
algorithm developed at Purdue
University
Left, ltered back projection (we
will cover)
Right, Veo
TM
iterative
reconstruction (we will not cover)
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 13 / 89
Image Receptors
Film, though much less now than historical use
Screen lm (copper, aluminum, etc)
Xeroradiogram
Image intensier tube (IIT) and Photomultipliers (PMT)
Charge-Coupled Device (CCD - often used with IIT)
Other receptors include ionography chamber and stimulable
phosphor, though the prevalence of other modalities (CT, PET,
MRI, etc.) have made the development of these modalities
somewhat moot
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 14 / 89
Film
Speed: Low
Dose: High
Resolution: High
Photographic emulsion is AgBr
suspended in gelatin (lime, I think)
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 15 / 89
Expose-Develop-Fix-Stop-Wash
sensitized grains incident photons and the # unsensitized
grains
dg = (G g)bdN, where
G: # grains of AgBr per unit area
b: cross-sectional area of a single AgBr grain
g: # sensitized grains per unit area
N: # photons(i.e. the dose)
Boundary condition: N = 0, g = 0 (G is a constant)
g = G(1 e
(bN)
) + g
0
g is now the optical density (sort of, more later), N is the
exposure, and g
0
is the fog level
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 16 / 89
Optical Density (Darkening)
D = log
10
I
0
I
I
0
: incident light intensity
I : exit light intensity
Near the maximum contrast point
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 17 / 89
Graphical Representation of Scatter at I(x,y)
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 18 / 89
Lambert-Beer Law of Photon Absorption
I (x, y) = NE(E, 0)Ee
(x,y,z)dz
+
E(E
s
, )E
s
S(x, y, E
s
, )ddE
s
(6)
I(x,y): image at the receptor
N: # of incident x-ray photons per unit area
(assumed single energy E)
(x, y, z): attenuation coecient (i.e. YOU)
S(x, y, E
s
, ): # scatter photons arrived at (x,y) from
solid angle (i.e. d = sin d d)
with energy range dE
s
E(E, ): energy absorption coecient
for energy E, solid angle
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 19 / 89
Lambert-Beer Law of Photon Absorption
I (x, y) NE(E, 0)Ee
(x,y,z)dz
+
S
E(E)E = NE(E, 0)Ee
(x,y,z)dz
(1+R)
(7)
R: Scattered to primary ratio
If we now make the substitution
C =
I
1
I
2
I
1
(8)
where C is the contrast, we have
I
1
= NE(E, 0)Ee
1
t
1
+
S
E(E)E (9)
I
2
= NE(E, 0)Ee
[
1
(t
1
t
2
)
2
t
2
]
+
S
E(E)E (10)
C =
e
1
t
1
e
[
1
(t
1
t
2
)
2
t
2
]
e
1
t
1
(1 + R)
(11)
=
1 e
(
2
1
)t
2
1 + R
(12)
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 20 / 89
Contrast Integral
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 21 / 89
Contrast and SNR
So, when scatter R C
The change in intensity between two regions is given by
I = I
1
I
2
= CI
1
So, the signal over area A = I A = I
1
C A
Signal
area
= C A N E E e
1
t
1
(1 + R) (13)
But what is the noise over the adjacent area?
Assume E is the same for primary and secondary photons and a
Poisson process for X-Ray photon arrival at area A.
Noise
area
= E
I
1
A
E
= E
NEAe
1
t
1
(1 + R) (14)
So
SNR
area
= C
NEAe
1
t
1
(1 + R) = [1e
(
2
1
)t
2
]
NEAe
1
t
1
1 + R
(15)
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 22 / 89
Dose
Given the minimal acceptable SNR (typically 5 (units are dB but
more on this later)), what is the required dose to see a cube of
t
2
t
2
t
2
? The required # of incident X-Ray photons is derived
from
SNR = k = [1 e
(
2
1
)t
2
]
NEAe
1
t
1
1 + R
(16)
which is approximately equal to
SNR = k = [1 [1 (
2
1
)t
2
]]
NEAe
1
t
1
1 + R
(17)
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 23 / 89
Dose
Rearrange terms and clear the radical
(1 + R)k
2
(
2
1
)
2
= NEAt
2
2
e
1
t
1
(18)
N =
k
2
(1 + R)e
1
t
1
E(
2
1
)
2
t
4
2
(19)
This is the number of photons per unit area (thats why the A
went away). To get surface dose, we have
Dose
surf
= N(
EN
)E =
EN
Ek
2
(1 + R)e
1
t
1
E(
2
1
)
2
t
4
2
(20)
Where N is the number of incident photons per unit area,
EN
is
the mass energy absorption coecient for tissue, and E is the
photon energy.
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 24 / 89
Quantum Mottle
Exposure (X) due to scatter
AEN, but total exposure is
AEN
x
x
= (AEN)
1
2
.
Recall, D = 0.434
x
x
D
Q
= 0.434(AEN)
1
2
, which is the
optical density due to quantum mottle (*proportional to lm
gamma)
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 25 / 89
Film Granularity
Recall, D
G
= 0.434
gA
A
, where is the cross-sectional area of a
silver speck resulting from a sensitized AgBr grain.
Nuttings Law gives D = 0.434g D
G
=
0.434D
A
(*proportional to
D)
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 26 / 89
Film Granularity
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 27 / 89
Detective Quantum Eciency
DQE =
SNR
out
SNR
in
2
DQE
total
= DQE
1
DQE
2
. . . DQE
n
In other words, the total DQE is the
product of each individual DQE
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 28 / 89
Geometric Unsharpness
Image blurring B =
ad
2
d
1
= a(m 1), where m is the image
magnication, i.e. m =
d
1
+d
2
d
1
(divide both sides by m)
U
g
=
B
m
= a(1
1
m
) (21)
Directly proportional to focal spot size, a, i.e. m U
g
.
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 29 / 89
Receptor Unsharpness
Caused by lateral spread of photons. Let F be the intrinsic receptor
unsharpness, i.e. the thickness of the image of an object which has
NO thickness. Imagine a photograph. The reason you can hold it is
because the paper and the ink have thickness - the image has zero
thickness. The receptor has thickness, but the image does not.
U
r
=
F
m
(22)
Inversely proportional to magnication, m, i.e. m U
r
.
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 30 / 89
Total Unsharpness
Ignore motion unsharpness (patient movement), making total
unsharpness the geometric mean of U
g
and U
r
U =
U
2
g
+ U
2
r
(23)
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 31 / 89
General Radiography
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 32 / 89
Xeroradiogram
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 33 / 89
Image Intensier
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 34 / 89
Photo Multiplier Tube
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 35 / 89
Digital Angiography
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 36 / 89
Digital Angiography
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 37 / 89
Four Generations of CT
Actually 5, though the fth is just a derivative of the fourth
All modern CT scans can be traced to the rst 1973 model
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 38 / 89
First Generation CT
Single X-Ray source,
single detector (180
rotate and shift)
Parallel beam
4 minutes per slice
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 39 / 89
Second Generation CT
Single X-Ray source,
multiple (3-60)
detectors (180
rotate
and shift)
Small angle fan beam
(10
)
20 seconds per slice
(240 seconds per
slice/average 12
detectors)
Wedge size
determines the
eciency of the slice
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 40 / 89
Third Generation CT (Fan beam reconstruction)
Single X-Ray source,
multiple (128-600)
detectors (360
rotation only)
Wide angle fan beam
(pulsed)
5 seconds per slice
(240 seconds per
slice/average 48
detectors)
Zenon gas detector
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 41 / 89
Fourth Generation CT
Single X-Ray source,
multiple ( 1000)
detectors (360
rotation only)
Wide angle fan beam
(continuous)
2 seconds per slice
(240 seconds per
slice/average 120
detectors)
Zenon gas detector
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 42 / 89
Fifth Generation
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 43 / 89
Classical Tomography
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 44 / 89
Computed Tomography
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 45 / 89
Computed Tomography
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 46 / 89
Projection
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 47 / 89
Back Projection
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 48 / 89
Back Projection
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 49 / 89
Algebraic Reconstruction Technique
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 50 / 89
Convolution, Backprojection, and Radon Transform
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 51 / 89
Dose vs. Resolution
Recall N =
SNR
2
(1+R)e
1
t
(
2
1
)t
4
2
Now
=
k
1
(SNR)
2
t
3
(k
2
t)
, where
: DQE
: x-ray dose (related to N)
k
1
: constant related to E
t: dimension of the smallest object
visible
k
2
t: thickness of the slice
(k
2
= 2 5 t)
dose
1
(spatial resolution)
4
Values for diagnostic CT
resolution: less than 1
mm
discrimination: 1% in
image density (related
to SNR)
dose: 10 100mGy
(compare to 1 mGy for
mammogram)
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 52 / 89
Beam Hardening
Low energy x-rays are attenuated
rst
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 53 / 89
Radioisotope Imaging
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 54 / 89
Ways to Detect -rays
Scintillation Crystal
NaI (Tl doping)
-ray visible light voltage (NaI PMT)
Gas-lled, multi-wire chamber
Xe
-ray charge voltage (wires)
Semiconductor
Si, Ge with doping (HPGe, CdTe, HgI
2
-ray charge voltage
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 55 / 89
Radioisotope Imaging
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 56 / 89
Gamma Camera
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 57 / 89
Gamma Camera
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 58 / 89
Position Determination
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 59 / 89
Spatial Resolution
Geometric Unsharpness: determined by the -ray energy and
the collimator design (R
c
< 10mm)
Intrinsic Unsharpness: determined by the thickness of the NaI
crystal, the number of PMTs and the position calculation
network (R
i
< 4mm)
Total Unsharpness (Spatial Resolution): R =
R
2
c
+ R
2
i
(R < 10mm)
At least an order of magnitude LESS than other modalities (CT,
MRI) Advantage of radioactive isotopes
Functional Imaging: Not just anatomical but physiological
information (metabolism)
Strong signal from small amount of tracer (nanograms)
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 60 / 89
Production of Radionuclides
Neutron Capture: Place target in a eld of thermal neutrons
(nuclear reactor)
98
42
Mo + n
99
42
Mo +
Nuclear Fission (nuclear reactor)
235
92
U + n
236
92
U
99
42
Mo +
99
42
Sn+
Charged Particle Bombardment: H
+
(p), H
, D
+
,
He
+
,
3
He
++
,
4
He
++
() (Cyclotron)
68
30
Zn + p
67
31
Mo + n
Radioactive Decay: Metastable
99
42
Mo
99
43
Tc
Isomeric Trans
99
43
Tc + (140 keV)
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 61 / 89
Decay of Radionuclides
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 62 / 89
Two Most Used Decays
Single Photon Emission
(
99
Mo
2.7 day
)
99
43
Tc
m
99
43
Tc + (140 keV) (Technetium
half-life 6.02 hours)
Positron Emission
(
68
Ge ) +
68
31
Ga
68
30
Zn+e
+
+ (Gallium half-life 68 minutes)
Annihilation produces two photons, each with energy 511 keV
(E = mc
2
)
Detect both, reduces scatter, increases spatial resolution ( 5
mm)
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 63 / 89
Compton -Camera Refraction
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 64 / 89
Dynamic Imaging
MUGA - Multiple Uptake Gate Acquisition
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 65 / 89
Dodges Area Length Formula
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 66 / 89
Diagnostic Ultrasound
Pulse Echo Imaging
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 67 / 89
Diagnostic Ultrasound
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 68 / 89
Pulse Echo Display Modes
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 69 / 89
Sound Speed (velocity), Bulk Modulus, Density, and
Impedance
Sound Velocity (speed): c =
=
dP
d
=
dP
d
(pressure per unit change of percent density)
K: Bulk modulus
dyn
cm
2
=
g
cms
2
, where
dyn
cm
2
is pressure
dyne =
gcm
s
2
Elastance =
1
capacitance
Recall Bulk modulus measures resistance to compression,
related to elastic modulus
Sound velocity (speed) in tissue: 1540
m
s
K
(g cm
1
s
1
) (g
1
cm
3
) =
cm
2
s
2
cm
s
, i.e. velocity
Acoustic characteristic impedance: z = c =
K
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 70 / 89
Fluid Mechanical Analogue
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 71 / 89
Reection/Refraction of Sound Waves at Interface
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 72 / 89
Pulsed Doppler System
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 73 / 89
Beamforming, Dynamic and Geometric Focusing
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 74 / 89
Duplex Scanning
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 75 / 89
Future Directions
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 76 / 89
Magnetic Resonance Imaging
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 77 / 89
Magnetic Resonance Imaging
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 78 / 89
Magnetic Resonance Imaging
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 79 / 89
Magnetic Resonance Imaging
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 80 / 89
RF Sequences
Saturation Recovery
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 81 / 89
RF Sequences
Inversion Recovery
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 82 / 89
RF Sequences
Spin Echo
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 83 / 89
RF Sequences
180 Rephasing
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 84 / 89
RF Sequences
Carr-Purcell and Carr-Purcell-Meiboom-Gill
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 85 / 89
Coils
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 86 / 89
Coils
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 87 / 89
Coils
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 88 / 89
References
[1]
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 89 / 89
S. Webb, The Physics of Medical Imaging.
Taylor and Francis, 1988.
John DiCecco, PhD BME464: Medical Imaging September 25, 2014 89 / 89
You might also like
- Assignment 2Document10 pagesAssignment 2James Brooks100% (3)
- CELTA Assignment 1Document12 pagesCELTA Assignment 1James Brooks100% (1)
- Equivalency Between Emulated Disc Electrodes and Conventional Disc Electrode Human EncephalographyDocument4 pagesEquivalency Between Emulated Disc Electrodes and Conventional Disc Electrode Human EncephalographyJames BrooksNo ratings yet
- NLF-MEDDocument9 pagesNLF-MEDJames BrooksNo ratings yet
- On The Detection of Independent Finger Movements Through Two Forearm MyoelectrodesDocument2 pagesOn The Detection of Independent Finger Movements Through Two Forearm MyoelectrodesJames BrooksNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Adobe Scan 12 Aug 2022Document3 pagesAdobe Scan 12 Aug 2022surabhi kalitaNo ratings yet
- Durango GS 6-7 Helitack OutreachDocument4 pagesDurango GS 6-7 Helitack OutreachdcgmNo ratings yet
- Lisa - Add New Front: Process Matching/Installation and Qualification (IQ)Document62 pagesLisa - Add New Front: Process Matching/Installation and Qualification (IQ)Thanh Vũ NguyễnNo ratings yet
- Experimental Design and Optimization MethodsDocument38 pagesExperimental Design and Optimization MethodssudalaiyandiNo ratings yet
- LP Pressure TestingDocument34 pagesLP Pressure TestinglisaNo ratings yet
- Meditations on Ancient Astrology Principles from Brihat Parashari HorāDocument87 pagesMeditations on Ancient Astrology Principles from Brihat Parashari HorāPrasanna KumarNo ratings yet
- Name: Amir Bin Rossaifuddin Id: 2016307153 Group: Emd2M2ADocument2 pagesName: Amir Bin Rossaifuddin Id: 2016307153 Group: Emd2M2AamirossaifuddinNo ratings yet
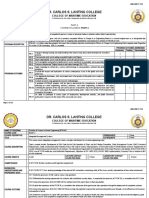
- Dr. Carlos S. Lanting College: College of Maritime EducationDocument14 pagesDr. Carlos S. Lanting College: College of Maritime EducationJeynard Moler J. TanNo ratings yet
- Maize Package of Practices in BriefDocument3 pagesMaize Package of Practices in Briefkomandla venkatkiran reddyNo ratings yet
- Starter Unit Basic Vocabulary: Smart Planet 3Document21 pagesStarter Unit Basic Vocabulary: Smart Planet 3Rober SanzNo ratings yet
- Educ 211 Ancient EgyptDocument27 pagesEduc 211 Ancient Egyptapi-207262700No ratings yet
- Minicargador Cat 246Document22 pagesMinicargador Cat 246Juanca FerroNo ratings yet
- How To Use Dr. Foster's Essentials: Essential Oils and BlendsDocument5 pagesHow To Use Dr. Foster's Essentials: Essential Oils and BlendsemanvitoriaNo ratings yet
- Advanced Technologies of CDQ Plant Advanced Technologies of CDQ PlantDocument12 pagesAdvanced Technologies of CDQ Plant Advanced Technologies of CDQ Plant조기현No ratings yet
- LearnEnglish Video Zone How These Women Changed Science ForeverDocument3 pagesLearnEnglish Video Zone How These Women Changed Science ForeverDaniella MensatoNo ratings yet
- 2nd Semester All Courses-100Document194 pages2nd Semester All Courses-100Ejiade PeterNo ratings yet
- Painting, DrawingDocument22 pagesPainting, DrawingMithilesh_Kuma_7083No ratings yet
- Unit 5 Project ManagementDocument19 pagesUnit 5 Project ManagementYashu RajNo ratings yet
- Telemark PulloverDocument2 pagesTelemark Pulloverkidknits100% (1)
- Chefs at HomeDocument4 pagesChefs at Homezbdv2kyzv7No ratings yet
- Kathrein 80010375Document2 pagesKathrein 80010375klamar5No ratings yet
- The Focus Shooting Method CourseDocument48 pagesThe Focus Shooting Method CourseKobiXDNo ratings yet
- Automatic Transaxle PDFDocument50 pagesAutomatic Transaxle PDFdemos70100% (1)
- Copeland CompressorDocument135 pagesCopeland CompressorsugirinNo ratings yet
- DEF File DescriptionDocument5 pagesDEF File Descriptionchompink6900No ratings yet
- Specimen 1 ValuationDocument17 pagesSpecimen 1 ValuationLight BearerNo ratings yet
- STC Ratings PDFDocument3 pagesSTC Ratings PDFDiseño SonidoNo ratings yet
- ArduinoDocument15 pagesArduinoAlvarez TomasNo ratings yet
- Spcr-TagbayaganDocument76 pagesSpcr-TagbayaganReycia Vic QuintanaNo ratings yet
- MR 20 Nissan PDFDocument1,639 pagesMR 20 Nissan PDFFREDYRUFO AZA MORALES83% (6)