Professional Documents
Culture Documents
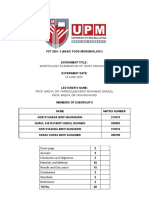
Vaginal Candidiasis 1
Uploaded by
Leanyn Andini0 ratings0% found this document useful (0 votes)
106 views7 pagesCandida colonization is common in women's vaginas. While often asymptomatic, it can sometimes lead to vaginal candidiasis (CVV). Recurrent CVV appears to be increasing and is often caused by non-albicans Candida species. For a colonization to cause symptoms, Candida must adhere to vaginal cells, germinate into invasive hyphal forms, and penetrate the epithelium. Estrogen increases adhesion by upregulating epithelial receptors. Lactobacilli normally block adhesion sites and prevent overgrowth.
Original Description:
about vaginal candidiasis
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCandida colonization is common in women's vaginas. While often asymptomatic, it can sometimes lead to vaginal candidiasis (CVV). Recurrent CVV appears to be increasing and is often caused by non-albicans Candida species. For a colonization to cause symptoms, Candida must adhere to vaginal cells, germinate into invasive hyphal forms, and penetrate the epithelium. Estrogen increases adhesion by upregulating epithelial receptors. Lactobacilli normally block adhesion sites and prevent overgrowth.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
106 views7 pagesVaginal Candidiasis 1
Uploaded by
Leanyn AndiniCandida colonization is common in women's vaginas. While often asymptomatic, it can sometimes lead to vaginal candidiasis (CVV). Recurrent CVV appears to be increasing and is often caused by non-albicans Candida species. For a colonization to cause symptoms, Candida must adhere to vaginal cells, germinate into invasive hyphal forms, and penetrate the epithelium. Estrogen increases adhesion by upregulating epithelial receptors. Lactobacilli normally block adhesion sites and prevent overgrowth.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 7
.
International Journal of Gynecology & Obstetrics 71 2000 S21S27
Vaginal candidosis: epidemiological and
etiological factors
J. Ferrer
U
Chair and Serice of Obstetrics and Gynecology, Hospital Central de Asturias, Uniersidad de Oiedo, Oiedo, Spain
Abstract
A review is presented of the emerging problem of candidal colonization regarding epidemiological and etiological
factors. In recent years a change in epidemiological trends has been observed. Vaginal candidosis seems to show a
higher frequency to recur and a signicant increase in infections caused by non albicans species of candidas has been
stated. The three stage mechanisms of adhesion, blastopore germination and epithelium invasion are emphasized.
There is a balance between candidal organisms and vaginal defense factors lactobacilli, cellular and humoral
. immunity controlling and limiting fungal growth. Vaginitis appears because of an increased number or an enhanced
virulence of candidas. In some other patients, a decreased vaginal defense mechanism is a determinant factor. There
are still a number of factors involved in clinical candidal vulvovaginitis that need to be claried. 2000 International
Federation of Gynecology and Obstetrics. All rights reserved.
Keywords: Vaginal candidosis; Host factors; Microbiology; Pathogenesis
Candida isolation from samples of vaginal exu-
date is a very frequent nding. It has been esti-
mated that it can be found in some 20% of
healthy symptomless women during their repro-
ductive premenopausal years. This rate shows a
w x
dramatic decrease after menopause 1 . There-
fore, Candida may be isolated from vaginal sam-
ples in approximately one-fourth of symptom-free
women.
U
Corresponding author. Fax: q34-985-277-573.
. E-mail address: javier.ferrer@ovd.servicom.es J. Ferrer .
Due to the high frequency of Candida in child-
bearing age, an understanding of pathogenic
mechanisms that can transform a symptomless
.
colonization into a candidal vulvovaginitis CVV
appears to be very important.
In fact, the scourge of CVV has important
implications. Some 75% of women will have a
CVV during their life span, and approximately
w x
half of them will suffer a second CVV event 2,3 .
Approximately 5% of cases will develop a recur-
rent CVV, showing frequent and refractory
w x
episodes 4 .
Global assessments of its importance have
0020-7292r00r$20.00 2000 International Federation of Gynecology and Obstetrics. All rights reserved.
. PII: S 0 0 2 0 - 7 2 9 2 0 0 0 0 3 5 0 - 7
( ) J. Ferrer rInternational Journal of Gynecology & Obstetrics 71 2000 S21S27 S22
Table 1
Factors predisposing to an increased colonization by candida
and to candidal vulvovaginitis
Pregnancy
Uncontrolled diabetes
Oral contraceptives containing high estrogen doses
Systemic or local antibiotics
IUD
Increased frequency of sexual intercourse
shown that CVV is the leading cause of colpitis
w x
worldwide 5 . In the United States, only bacterial
w x
vaginitis is slightly more common than CVV 6 .
Regarding incidence, some characteristics
should be mentioned that can double its fre-
quency. During pregnancy, Candida can be
isolated from 30 to 40% of women, and the
infection is particularly virulent in the last
w x .
trimester 7 Table 1 .
Candidosis can be likened to an iceberg. All
these data suggest that candidal colonization is
extremely important in women; clinical cases are
just the visible portion of the iceberg.
In recent years a new trend has appeared.
Vaginal candidosis seems to show a higher trend
to recur. Approximately 50% of CVV have a
w x
second episode 8,9 . In some 5% of cases, the
w x
disease has a chronic course 9,10 . Recurrent
vaginal candidosis is dened by four or more
mycologically-diagnosed episodes during a year.
Sometimes, recurrences have a great impact on
the patient; they can cause some kind of phobic
w x
state or even anxiety 11 .
1. Microbiology
There are approximately 150 Candida species,
belonging to genus 4 in blastomycetes. Nowadays
DNA makeup is very important to classify these
species.
Candida albicans is by far the most common
species in gynecology; it can be found in approxi-
w x
mately 8090% of cases 3,7,9,11 .
Candida glabrata is the second most common
species, causing approximately 515% of cases of
vaginal candidosis. Other species that can also be
found are: Candida tropicalis in approx. 5% of
Table 2
Pathogenesis of recurrent candidosis
Source
Vaginal inoculation: most common
Intestinal reservoir theory
Sexual transmission
Vaginal recurrence
Mechanisms
Increased candidal virulence
Candida non-albicans
Host factors
Decreased secretory local immunity
IgE-mediated hypersensitivity reaction
Loss of lactobacille protective effect
. w x
cases 1115 , C. pseudotropicalis, and C. krusei.
Other species, such as C. parapsilosis and C.
w x
guilliermondi, are rarely isolated 11,15,16 .
In recent years, a change in epidemiological
trends has been observed. There has been a sig-
nicant increase in infections caused by non-
albicans species of candida, particularly C.
w x
glabrata and C. tropicalis 1719 .
An increase of non-albicans species has been
observed, particularly in recurrent cases. At pre-
sent, these species are found in approximately
2030% of cases of recurrent vaginal candidosis
w x
20 . Among them, Candida glabrata is the most
w x .
common type 18,21 Table 2 .
The increasing detection of non-albicans spe-
cies has been related to the widespread and inap-
propriate use of antimycotic treatments self-
medication, long-term maintenance treatments,
.
repeated treatments for candidosis episodes . C.
albicans eradication causes a selection of species
.
such as C. glabrata that are resistant to com-
w x
monly used agents 18,22 .
Candida is a dimorphic fungus that can be
found in two different states. Blastopores or
Table 3
Mycological differences between colonization and candidal
vaginitis
Colonization Vaginitis
Phenotype Blastopore Mycelium
Titer )1000rml )10 000rml
Proteolysis qrqq qqqrqqqq
Colony opacity Faint More opaque
( ) J. Ferrer rInternational Journal of Gynecology & Obstetrics 71 2000 S21S27 S23
spores are the phenotype for extension, dissemi-
nation and transmission. They are also a resis-
tance form of the fungus, that can be associated
with a symptomless colonization.
On the other hand, mycelia are germinative
forms; this phenotype can invade tissues and cause
.
symptoms Table 3 .
2. Pathogenesis
To be invasive, candida must follow a three-
stage mechanism.
2.1. Adhesion
Adhesion is crucial for blastopore survival. Ad-
hesion of Candida albicans is higher than adhe-
sion of C. glabrata, C. tropicalis, C. pseudotropi-
calis, and C. krusei, and this can explain its higher
w x
frequency in clinical settings 23 .
Candidal organisms are able to recognize a
true receptor on cell membranes of vaginal epi-
thelium; they can adhere to this phospholipid-
w x
and bronectin-containing receptor 24,25 .
Blastopore adherence seems to be based on a
mannoprotein in fungal membrane, previously
known as adhesin, similar to integrins. This pro-
tein is able to anchor itself on the receptor on
w x
surface cells in vaginal epithelium 24,25 .
In laboratory assays, a great individual variabil-
w x
ity has been shown in candidal adherence 26 .
This nding suggests that a great variation could
exist in susceptibility to fungal adherence, which
is the rst step in symptomatic vaginitis. Thus,
some women could be much more susceptible
than others to CVV, due to their susceptibility to
spore adherence.
Adherence is enhanced by estrogen impregna-
tion in vaginal epithelium. Estrogen increases
surface exposure of glycoprotein complexes acting
w x
as receptors for blastopore adherence 27 .
Thus, candidal vaginitis is uncommon during
hypoestrogenic periods, such as premenarche and
postmenopause. On the other hand, pregnancy
as well as use of oral contraceptives containing a
high estrogen dose causes an increased blasto-
pore adhesion and, so, a higher symptomatic in-
.
fection rate Table 1 .
Based on all these data, we can state that
symptomatic vaginal candidosis is a hormone-
dependent and more specically, estrogen-de-
.
pendent disorder.
Another factor affecting candidal adhesion is
competition with vaginal lactobacilli. Lactobacilli,
through their co-aggregation, prevent and block
spore adhesion to surface receptors on vaginal
epithelium cells. They simply block such loci,
preventing candidal organisms to adhere to them
w x
26 .
Thus, a reduction in normal lactobacilli ora
can cause an imbalance and provoke a candidal
vaginitis. In fact, a low number of lactic bacilli has
been reported in vaginal exudate samples from
patients with CVV.
2.2. Blastopore germination. mycelium or hyphae
deelopment
Blastopore forms are not able to penetrate into
w x
epithelial tissues and cause colpitis 28 . In fact,
some mutant forms of Candida albicans have
been found that are not able to develop their
mycelia; these mutant forms do not cause VCC
w x
6 .
Exogenous factors promoting spore germina-
tion can trigger candidal vaginitis in women.
Again, estrogen promotes mycelium development
w x
in candida 27 . On the other hand, ketoconazole
administration prevents germination and can be
w x .
useful in colpitis prophylaxis 29 Table 3 .
2.3. Epithelium inasion
Once its mycelium has been developed, can-
dida is able to penetrate and invade vaginal sur-
face cells. Electron microscopy studies have shown
w x
intracellular penetration holes 3032 .
From a biochemical point of view, epithelial
cell penetration has been related to production of
w x
several proteases by hyphae 25 .
Epithelium invasion also causes a release of
several other substances, such as prostaglandins
and bradykinin, inducing inammatory changes in
tissues. This process can lead to edema, ery-
thema, exudate increase, and cell shedding. These
changes can be detected occasionally with a col-
( ) J. Ferrer rInternational Journal of Gynecology & Obstetrics 71 2000 S21S27 S24
poscopic exam, showing diffuse or focal colpitis
features.
Candidal leucorrhea consists of a mix of hy-
phae, non-viable exfoliated vaginal cells, as well
w x
as some polymorphonuclear cells 30 .
Another factor involved in epithelial invasion is
blastopore load. An increase in the number of
spores in vaginal environment triggers invasion
and candidal colpitis. The increase in number of
spores is related to an increase in sexual inter-
course frequency exogenous blastopore acquisi-
. w x
tion 33 or has an intestinal reservoir source
. w x
inappropriate personal hygiene 34 Tables 1
.
and 2 .
Although CVV can by no means be considered
a sexually-transmitted disease, it has some associ-
ation with an increased frequency of sexual inter-
course. This can be explained by the increased
.
blastopore vaginal load Table 1 . Also, although
intestinal reservoir has a minor role in CVV,
inappropriate personal hygiene can cause an in-
crease in the number of spores in vagina.
3. Defense factors against candida in vagina
3.1. Vaginal ora. Lactobacilli
This is the most important barrier to candidal
infections. Lactobacilli are involved in three de-
fense mechanisms. Firstly, they compete with can-
dida for nutrients; this is not, however, the most
effective mechanism. In fact, a shoulder-to-
shoulder survival has been shown for lactobacilli
w x
and candida on an experimental basis 35,36 .
Secondly, and more importantly, they cause a
co-aggregation process that blocks epithelial re-
ceptors for blastopore. Thus, adhesion cannot take
place.
Thirdly, lactobacilli produce some substances
. w x
the so-called bacteriocins 37 that hamper
mycelia germination.
These mechanisms can explain that clinical
candidosis can be triggered in some patients when
antibiotic agents causing a depletion of lacto-
w x
bacilli ora are administered 38,39 Tables 1
.
and 2 .
3.2. Humoral immunity. Antibodies
Immunodepressed patients show severe recur-
rent candidosis. Antibodies must undoubtedly play
a major role in preventing growth and develop-
ment of a number of saprophytic organisms.
Protective effects of systemic humoral anti-
bodies are not well known. Undoubtedly, local
secretory IgA-type antibodies must be more im-
portant; a low level of these antibodies has been
w x
reported in active candidal infections 40 . They
are, however, difcult to measure in secretions,
and their values have no clinical use. Neverthe-
less, local secretory immunity variation can be the
cause of a higher susceptibility to candidal infec-
.
tion Table 2 .
In some cases, high levels of IgE in serum and
vaginal samples have been observed, particularly
in patients with recurrent candidosis. This nding
implies some allergic sensitization, and sometimes
a major inammatory response to low candidal
w x
antigen loads 41,42 . These patients could show a
true allergic sensitization to candidal antigens
.
Table 2 .
3.3. Cellular immunity
Oral and vaginal candidosis are associated with
T-cell immunodepression. Up to 5070% of
patients infected with HIV show vulvaroral
vaginal candidosis.
Cellular immunity plays a major role in host
defense mechanisms against candida. A low inter-
feron- production by lymphocytes is believed to
w x .
prevent mycelia germination 43 Table 2 .
Overall, these ndings suggest that a decrease
in cellular immunity not detectable by clinical or
.
laboratory means could be a key factor in some
individual cases with a high susceptibility to CVV.
In patients with recurrent vulvovaginitis
sometimes difcult to treat a failure to pre-
vent candidal growth due to immune changes
.
could be the main cause Table 2 .
( ) J. Ferrer rInternational Journal of Gynecology & Obstetrics 71 2000 S21S27 S25
4. Host predisposing factors
4.1. Pregnancy
During pregnancy there is an increased vaginal
susceptibility to infection, with a high rate of
w x
colonization and symptomless vaginitis 6 .
High estrogen levels cause an increased glyco-
gen load in epithelium, which, in turn, is a nutri-
tional source for candida growth and germination
w x
36 .
Secondly, gestational hyperestrogenism pro-
motes fungal adhesion and germination; as a con-
sequence, fungi are more capable to penetrate
w x
vaginal wall 27 .
Thus, candidal vaginitis incidence is very high
in pregnancy. Additionally, cure rates are lower
during pregnancy. Therapy must be careful and
appropriate in these patients.
4.2. Contraception
An increased candidal colonization has been
shown in several studies in patients using oral
contraceptives containing a high estrogen dose
w x
8 . The mechanisms for this effect are the same
.
as in pregnancy Table 1 .
Even an association of oral contraception with
recurrent vulvovaginitis has been reported by
w x
some workers 21 , although other studies have
failed to conrm such an association. No synergic
action has ever been shown, of course, for low-
estrogen contraceptives regarding candidal growth
w x
9,33,44 .
On the other hand, an association of IUD with
recurrences has been reported, because the thread
w x
could act as a candidal reservoir 36 .
4.3. Diabetes
Vaginal colonization and CVV are more com-
mon in diabetic women. Metabolic disturbances
w x .
predispose to clinical vaginitis 36,46 Table 1 .
This factor can be, however, minimized by means
of an appropriate diabetic control.
4.4. Antibiotic agents
Candidal vulvovaginitis is a common occur-
rence after systemic or vaginal antibiotic drug
treatment.
Antibiotic agents not only trigger CVV, but can
w x
also increase vaginal colonization 38,39,45 Ta-
.
ble 1 .
These drugs, either systemically or locally, sup-
press lactobacilli ora. Candidal organisms are
then free to grow, adhere and germinate. How-
ever, several case-control studies have failed to
show this causal association of antibiotic agents
w x
with clinical candidosis 44 .
5. Symptomatic vaginitis development
Transformation of vaginal colonization into
vaginitis is a critical step in the pathogenic mech-
anism of candidal vaginitis.
During colonization stage, candidal organisms
are present basically in lamentous forms, and
.
their number is not very high Table 3 .
There is balance between candidal organisms
and vaginal defense factors lactobacilli, cellular
.
and humoral immunity, etc. controlling and limit-
ing fungal growth.
Vaginitis appears because of an increased num-
ber or an enhanced virulence of candidal organ-
isms. In some other patients, a decreased or
abolished vaginal defense mechanism is a de-
terminant factor.
When this occurs, blastopores adhere to vagi-
nal epithelium and germinate; mycelium devel-
ops, and nally invades mucous membrane, pro-
ducing vaginitis.
There are still a number of mechanisms in-
volved in clinical candidal vulvovaginitis develop-
ment and its recurrence that need to be claried.
In the near future there will be new advances in
Candida biology and in vaginal immune defense
mechanisms understanding, that will allow us to
better understand candidal infections and to op-
timize their treatment.
( ) J. Ferrer rInternational Journal of Gynecology & Obstetrics 71 2000 S21S27 S26
References
w x 1 Sobel JD. Epidemiology and pathogenesis of recurrent
vulvovaginal candidiasis. Am J Obstet Gynecol
1985;152:924935.
w x 2 Hurley R, De Luvois J. Candida vaginitis. Postrgrad
Med J 1979;55:645647.
w x 3 Hurley R. Trends in candidal vaginitis. Proc R Soc Med
70 suppl 1977;4:18.
w x 4 Hurley R. Recurrent candida infection. Clin Obstet
Gynecol 1981;8:209213.
w x 5 Annual Report of Chief Medical Ofcer. Department of
Health and Social Security, 19761984 England and
. Wales .
w x 6 Sobel JD. Candidal vulvovaginitis. Clin Obstet Gynecol
1993;36:153165.
w x 7 Odds F.C. eds. Candida and candidiasis. Baltimore: Uni-
versity Park Press, 1979: 104110.
w x 8 Denning DW, Evan EGB, Kibbler CC, Richardson MD,
Roberts MM, Rogers TR et al. Working group of the
British Society for Medical Mycology. Management of
genital candidiasis. Br Med J 1995;310:12411244.
w x 9 Sobel JD. Candida vulvovaginits. Sem Dermatol.
1996;15:1728.
w x 10 Geiger AM, Foxman B, Sobel JD. Chronic vulvovaginal
candidiasis: characteristics of women with Candida albi-
cans, C. glabrata and no candida. Genitourin Med
1975;71:304330.
w x 11 Grillot R. Mycoses genitales. Les mycoses humaines:
demarche diagnostique. Elsevier, Paris, 1996:116124.
w x 12 Sobel JD, Chaim W. Treatment of torulopsis glabrata
vaginitis: retrospective review of boric acid therapy. Clin
Infect Dis 1997;24:649652.
w x 13 Sobel JD. Vulvovaginitis due to Candida glabrata. An
emerging problem. Mycoses Problem, 41 suppl
1998;2:1822.
w x 14 Redondo-Lopez V, Lynch M, Schmitt C, Cook R, Sobel
JD. Torulopsis glabrata vaginitis: clinical aspects and
susceptibility to antifungal agents. Obstet Gynecol
1990;76:651655.
w x 15 Spinillo A, Capuzzo E, Egbe TO, Baltaro F, Nicola S,
Piazi G. Torulopsis glabrata vaginitis. Obstet Gynecol
1995;85:993998.
w x 16 Moyal Barraco M. Candidosis vulvo.vaginales recidi-
vants. Manifestations cliniques, diagnostic mycologique,
facteurs favorisants, traitement. Reprod Hum Horm
1996;9:5361.
w x 17 Horowitz BJ, Giaquinta D, Ito S. Evolving pathogens in
vulvovaginal candidasis: implications for patient care. J
Clin Pharmacol 1992;32:248255.
w x 18 Spinillo A, Nicola S, Colonna L, Marangoni F, Cavanna
C, Michelone G. Frequency and signicance of drug
resistance in vulvovaginal candidiasis. Gynecol Obstet
Invest 1994;38:130133.
w x 19 Horwitz BJ, Edelstein SW, Lippman L. Candida topi-
calis vulvovaginitis. Obstet Gynecol 1985;66:229232.
w x 20 Nyirjesy P, Seeney SM, Grody MHT, Jordan CA, Buck-
ley HR. Chronic fungal vaginitis: the value of cultures.
Am J Obstet Gynecol 1995;173:820823.
w x 21 Spinillo A, Pizzoli G, Colonna L, Nicola S, De Seta F,
Guaschino S. Epidemiologic characteristics of women
with idiopathic vulvovaginal candidiasis. Obstet Gynecol
1993;81:721727.
w x 22 Fidel P, Vazquez JA, Sobel JD. Candida glabrata: re-
view of epidemiology pathogenesis and clinical disease
with comparison to candida albicans. Clin Microb Rev;
1999;12:8096.
w x 23 King RD, Lee JC, Morris AL. Adherence of Candida
albicans and other candida species to mucosal epithelial
cells. Infect Immun 1980;27:667674.
w x 24 Krivan HC. Microbial adhesion: glycolipids as possible
receptors for vaginal pathogens. Orlando, FL: Second
International Conference on Vaginitis, March Abstract
1989;29:P3.
w x 25 Bohbot JM. Acquisitions recentes sur la physio-
pathologie des candidosis vulvovaginales. Gyn Obs
1996;354:2528.
w x 26 Sobel JD, Myer P, Levison ME. Candida albicans adher-
ence to vaginal epithelial cells. J Infect Dis
1981;143:7682.
w x 27 Powell BL, Drutz DI. Estrogen receptor in Candida
albicans. A possible explanation for hormonal inuences
in vaginal candidiasis. Twenty third Interscience Confer-
ence on Antimicrobial Agents and Chemotherapy. Abs-
tract 1983;751:222.
w x 28 Fidel PL, Sobel JD. Immunopathogenesis of recurrent
vulvovaginal candidiasis. Clin Microbiol Rev
1996;9:335348.
w x 29 Sobel JD, Muller G. Ketoconazole prophylaxis in experi-
mental vaginal candidiasis. Antimicrob Agents
Chemother 1984;25:281282.
w x 30 Sobel JD, Muller G, Mc Cormick E. Experimental
chronic vaginal candidiasis in rats. Suabouraudia
. 1998;5 23 :199206.
w x 31 Farrell SM, Hawkins DF, Ryder TA. Scanning electron
microscope study of Candida albicans invasion of cul-
tured human cervical cells. Sabouraudia 1983;21:
151154.
w x 32 Garca T, Castello E, Martinez AJ. Human genital can-
didosis. Histochemistry, scanning and transmission elec-
. tron microscopy. Acta Cytol Baltimor 1982;26:711.
w x 33 Foxman B. The epidemiology of vulvovaginal candidia-
sis: risk factors. Am J Public Health 1990;80:329331.
w x 34 Fong IV. The value of treating the sexual partner of
women with recurrent vaginal candidiasis with ketocona-
zol. Genotourin Med 1992;68:174176.
w x 35 Savage DC. Microbial interference between indigenous
yeast and lactobacilli in the rodent stomach. J Bacteriol
1969;98:12781285.
w x 36 Bohbot JM. Les mycoses genitales chroniques. Physio-
pathologie, traitement: jusquou aller? Realites en
Ginecologie-Obstetrique 1995;5:2938.
w x 37 Narayanan TK, Tao GR. Beta-indole-ethanol and beta-
indolel-acid production by Candida species: their
( ) J. Ferrer rInternational Journal of Gynecology & Obstetrics 71 2000 S21S27 S27
antibacterial and autoantibiotic action. Antimicrob
Agents Chemoter 1976;9:375380.
w x 38 Caruso LJ. Vaginal moniliasis after teracycline therapy.
Am J Obstet Gynecol 1964;90:374380.
w x 39 Oriel JD, Waterworth PM. Effect of mynocicline and
tetacycline on the vaginal yeast ora. J Clin Pathol
1975;28:403409.
w x 40 Gough PM, Warnock DV, Richardson MD. IgA and IgI
antibodies to Candida albicans in the genital tract secre-
tions of women with and without vaginal candidiasis.
. Sabouradis 1989;4 22 :265271.
w x 41 Mathur S, Goust JM, Horger EO. Immunoglobulin E
anti-Candida antibodies and candidiasis. Infect Immun
1977;8:257261.
w x 42 Witkin S.S. IgE antibodies to Candida albicans in vagi-
nal uids of with recurrent vaginitis. Palm Spring,CA:
American Society for Microbiology Meeting 1987; 10:
abstract 9.
w x 43 Morton RS, Rashid S. Candidal vaginitis: natural his-
tory, predisposing factors and prevention. Proc R Soc
Med, 70 suppl 1977;4:312.
w x 44 Geiger AM, Foxman B. Risk factors for vulvovaginal
candidiasis. A case control study among university stu-
dents. Epidemiology 1996;7:182187.
w x 45 Bluestein D, Rutledge C, Lumsden I. Predicting the
occurrence of antibiotic induced candidal vaginitis. Fam
Pract Res 1991;11:319326.
w x 46 Reed B. Risk factors for candida vulvovaginits. Obstet
Gynecol Survey 1992;47:551560.
You might also like
- Fast Facts: Complex Perianal Fistulas in Crohn's Disease: A multidisciplinary approach to a clinical challengeFrom EverandFast Facts: Complex Perianal Fistulas in Crohn's Disease: A multidisciplinary approach to a clinical challengeNo ratings yet
- An overview of Candida vaginitisDocument3 pagesAn overview of Candida vaginitisRicha SharmaNo ratings yet
- Practical Guide To Diagnosing and Treating Vaginitis (Medscape)Document16 pagesPractical Guide To Diagnosing and Treating Vaginitis (Medscape)Nur Ilmi SofiahNo ratings yet
- Vulvovaginal Candidiasis in Pregnancy: Causes, Risks, and TreatmentDocument6 pagesVulvovaginal Candidiasis in Pregnancy: Causes, Risks, and TreatmentMitre AttkNo ratings yet
- B04801007013 PDFDocument7 pagesB04801007013 PDFrismahNo ratings yet
- B04801007013 PDFDocument7 pagesB04801007013 PDFrismahNo ratings yet
- B04801007013 PDFDocument7 pagesB04801007013 PDFrismahNo ratings yet
- Vaginal CandidiasisDocument29 pagesVaginal CandidiasisMike Serge RazafiNo ratings yet
- Treatment of Vulvovaginal Candidiasis: A Review of The LiteratureDocument3 pagesTreatment of Vulvovaginal Candidiasis: A Review of The LiteraturePatresya LantanNo ratings yet
- Sindrome Duh Genital Non GODocument15 pagesSindrome Duh Genital Non GOIntan PermataNo ratings yet
- Candida vulvovaginitis clinical manifestationsDocument18 pagesCandida vulvovaginitis clinical manifestationsCindyNo ratings yet
- Selecting Anti-Microbial Treatment of Aerobic Vaginitis: Genitourinary Infections (J Sobel, Section Editor)Document7 pagesSelecting Anti-Microbial Treatment of Aerobic Vaginitis: Genitourinary Infections (J Sobel, Section Editor)eva yustianaNo ratings yet
- Vulvovaginal Candidiasis: Understanding Epidemiology and PathogenesisDocument11 pagesVulvovaginal Candidiasis: Understanding Epidemiology and PathogenesisJoshua RuntuweneNo ratings yet
- 8042 28586 1 PBDocument6 pages8042 28586 1 PBRasika de SilvaNo ratings yet
- Acute VulvovaginitisDocument8 pagesAcute VulvovaginitisKagek BheNo ratings yet
- Diagnosis and Management of Fungal Urinary Tract InfectionDocument14 pagesDiagnosis and Management of Fungal Urinary Tract InfectionIvan SanchezNo ratings yet
- Candida vulvovaginitis: Current ReviewDocument20 pagesCandida vulvovaginitis: Current ReviewVicobeingoNo ratings yet
- Calzolari 2000Document6 pagesCalzolari 2000Rika Yulizah GobelNo ratings yet
- Pathogenesis, diagnosis and treatment of vaginitis and cervicitisDocument7 pagesPathogenesis, diagnosis and treatment of vaginitis and cervicitisNisaNo ratings yet
- Bacterial VaginalDocument5 pagesBacterial VaginalYuliana DaisongNo ratings yet
- N00159 South Africa Vulvovaginal Candidiasis SEP2016 Rev000Document2 pagesN00159 South Africa Vulvovaginal Candidiasis SEP2016 Rev000Endy SitumbekoNo ratings yet
- Acute Vulvovaginitis: Clinical Prac TiceDocument9 pagesAcute Vulvovaginitis: Clinical Prac TicewiwiknovitasariNo ratings yet
- Prevalence of Vulvovaginal Candidiasis (VCC) Among Secondary School Girls at Katunguru Seed School in Rubirizi DistrictDocument17 pagesPrevalence of Vulvovaginal Candidiasis (VCC) Among Secondary School Girls at Katunguru Seed School in Rubirizi DistrictKIU PUBLICATION AND EXTENSIONNo ratings yet
- Bacterial Vaginosis and Its Association With Infertility, Endometritis, and Pelvic Inflammatory DiseaseDocument7 pagesBacterial Vaginosis and Its Association With Infertility, Endometritis, and Pelvic Inflammatory DiseasePraneeth PaletiNo ratings yet
- Recurrent Vulvovaginal Candidiasis: Clinical UpdateDocument4 pagesRecurrent Vulvovaginal Candidiasis: Clinical UpdateErihka Silvia SiregarNo ratings yet
- CMV in Pregnancy GuideDocument24 pagesCMV in Pregnancy GuideLearta Asani VeliuNo ratings yet
- Pelvic Infections in Women: Belgian Guidelines: OutlineDocument35 pagesPelvic Infections in Women: Belgian Guidelines: OutlineJose mauricio PalenciaNo ratings yet
- Tugas Kukel WulanDocument15 pagesTugas Kukel WulanDonny Ardika NovanandaNo ratings yet
- Infeksi Genitalia Interna & ExternaDocument63 pagesInfeksi Genitalia Interna & ExternaPoetri IermayaniNo ratings yet
- 2018 - DR Soffin - FLUOR ALBUS KULIAHDocument24 pages2018 - DR Soffin - FLUOR ALBUS KULIAHYoggaNo ratings yet
- Practical Diabetes International - November December 1991 - Scott - Genito Urinary Disorders and DiabetesDocument3 pagesPractical Diabetes International - November December 1991 - Scott - Genito Urinary Disorders and Diabetescsedmonds1503No ratings yet
- Candida VulvovaginitisDocument29 pagesCandida VulvovaginitisPepe VizcarraNo ratings yet
- Vaginal Discharge Causes and ManagementDocument5 pagesVaginal Discharge Causes and ManagementHassan Abdullah AL-balushiNo ratings yet
- Candidiasis (Hasznalt)Document4 pagesCandidiasis (Hasznalt)Ilyes FerenczNo ratings yet
- Bacterial Vaginosis PaperDocument4 pagesBacterial Vaginosis Paperobakhit91No ratings yet
- 2013 Fluconazole Resistant Candida Albicans.22Document8 pages2013 Fluconazole Resistant Candida Albicans.22Kala SuvarnaNo ratings yet
- Recurrent Vaginal Candidiasis GuideDocument5 pagesRecurrent Vaginal Candidiasis Guideamo94No ratings yet
- Vaginal Discharge: Clinical ReviewDocument5 pagesVaginal Discharge: Clinical ReviewOktari Dwi YantiNo ratings yet
- Vaginitis ACOG 2006Document17 pagesVaginitis ACOG 2006xiomara andrea rios coquecoNo ratings yet
- Pertemuan Ke-3 REPRODocument29 pagesPertemuan Ke-3 REPROAdi Joyo NegoroNo ratings yet
- Sobel Et Al. 2011 Infecções UrináriasDocument4 pagesSobel Et Al. 2011 Infecções UrináriasLeandro FigueiraNo ratings yet
- Jurnal AborsiDocument6 pagesJurnal Aborsimakiyatul madaniaNo ratings yet
- Bacterial VaginosisDocument11 pagesBacterial VaginosisMuh. Idham RahmanNo ratings yet
- Vaginal Fungal InfectionsDocument15 pagesVaginal Fungal InfectionsBalsc Bals BalscNo ratings yet
- Prior Pelvic Inflammatory Disease, Endometriosis and Ectopic PregnancyDocument16 pagesPrior Pelvic Inflammatory Disease, Endometriosis and Ectopic PregnancyLinda Ratna12No ratings yet
- Idog 03 210Document7 pagesIdog 03 210jwmeadow2401No ratings yet
- Jurnal VaginitisDocument8 pagesJurnal VaginitisKariina Indah PrayogiNo ratings yet
- Risk Factors & Species of Invasive Fungal Infections in ICUsDocument7 pagesRisk Factors & Species of Invasive Fungal Infections in ICUsquaisherhossainNo ratings yet
- Gynaecology: Gum, Fertility, Contraception, and UrogynaecologyDocument46 pagesGynaecology: Gum, Fertility, Contraception, and UrogynaecologyOccamsRazorNo ratings yet
- Vulvovaginal Candidiasis and Bacterial VaginosisDocument16 pagesVulvovaginal Candidiasis and Bacterial VaginosisAdnanda Maulan100% (1)
- Pelvic Inflammatory DiseaseDocument43 pagesPelvic Inflammatory DiseaseFauzia Jamiri - Abdurasid100% (2)
- Vaginitis EmedicineDocument17 pagesVaginitis EmedicineIndah HaneNo ratings yet
- PM 02 53Document7 pagesPM 02 53الشاطر المصرىNo ratings yet
- Incidence of Candidiasis Amongst Female Students of A Tertiary Institution in Rivers State NigeriaDocument6 pagesIncidence of Candidiasis Amongst Female Students of A Tertiary Institution in Rivers State NigeriaUbali Ibrahim HashimuNo ratings yet
- Infectious Diseases of The Female Genital TractDocument1,111 pagesInfectious Diseases of The Female Genital TractJohn Ntokos100% (2)
- Session9-Gynecologic InfectionsDocument81 pagesSession9-Gynecologic InfectionsCHALIE MEQUNo ratings yet
- 2018 - DR Soffin - FLUOR ALBUS KULIAHDocument24 pages2018 - DR Soffin - FLUOR ALBUS KULIAHZakaha RachmadhaniNo ratings yet
- PreventionDocument6 pagesPreventionBipin PatelNo ratings yet
- Review ArticleDocument12 pagesReview ArticleThallita Rahma ZiharviardyNo ratings yet
- Prevalence of Vaginitis Among Women Attending Antenatal Care Centre of Wudil General Hospital, Kano State NigeriaDocument6 pagesPrevalence of Vaginitis Among Women Attending Antenatal Care Centre of Wudil General Hospital, Kano State NigeriaUMYU Journal of Microbiology Research (UJMR)No ratings yet
- Dwnload Full Janeways Immunobiology 9th Edition Murphy Test Bank PDFDocument35 pagesDwnload Full Janeways Immunobiology 9th Edition Murphy Test Bank PDFsiennaclimatal1bk6t6100% (13)
- Pharmacological Activities of Coccinia GrandisDocument6 pagesPharmacological Activities of Coccinia GrandisSatya NandaNo ratings yet
- 00A 097 Comprehensive Microbial Identification With OdinDocument5 pages00A 097 Comprehensive Microbial Identification With OdingombasgNo ratings yet
- Fluconazole - Herrera - 2013Document104 pagesFluconazole - Herrera - 2013Ferney Alexis Cortes ZapataNo ratings yet
- Corn MealDocument2 pagesCorn MealSantosh YeleNo ratings yet
- ResearchDocument31 pagesResearchAlexa BarnNo ratings yet
- Management and Treatment of Fungal Infection in The Oral CavityDocument4 pagesManagement and Treatment of Fungal Infection in The Oral CavityKIU PUBLICATION AND EXTENSIONNo ratings yet
- Environmental PH Modulation Bypathogenic Fungi As A Strategy To Conquer The HostDocument6 pagesEnvironmental PH Modulation Bypathogenic Fungi As A Strategy To Conquer The HostMano RatyiNo ratings yet
- Oxoid - SdaDocument1 pageOxoid - SdaDidik PrasetyaNo ratings yet
- Antifungal Catheter Lock Therapy 1Document8 pagesAntifungal Catheter Lock Therapy 1Dakota YamashitaNo ratings yet
- Candida Research and Resources - Intestinal Health InstituteDocument19 pagesCandida Research and Resources - Intestinal Health InstituteKátia SiqueiraNo ratings yet
- Pathogenesis of Fungal InfectionsDocument70 pagesPathogenesis of Fungal Infectionsማላያላም ማላያላም100% (15)
- A Review On Traditional Uses, Phytochemistry and Pharmacological Properties of Eclipta Alba (Linn.) Hassk - An Innumerable Medicinal Plant.Document15 pagesA Review On Traditional Uses, Phytochemistry and Pharmacological Properties of Eclipta Alba (Linn.) Hassk - An Innumerable Medicinal Plant.anithaNo ratings yet
- Candidiasis Pathogenesis and TypesDocument10 pagesCandidiasis Pathogenesis and TypesBunny OzuNo ratings yet
- Borges, K. Et Al. (2018)Document7 pagesBorges, K. Et Al. (2018)Paulina Bermudez ValenzuelaNo ratings yet
- Caspofungin: InvitedarticleDocument13 pagesCaspofungin: InvitedarticleIris GalvánNo ratings yet
- The Borax ConspiracyDocument18 pagesThe Borax ConspiracybartNo ratings yet
- Articulo Cientifico Derivado Del FenilpropanoDocument23 pagesArticulo Cientifico Derivado Del FenilpropanoKaren GonzalezNo ratings yet
- Candiduria: Evidence-Based Approach To Management, Are We There Yet?Document10 pagesCandiduria: Evidence-Based Approach To Management, Are We There Yet?ntnquynhproNo ratings yet
- Staphylococcus-Candida Interaction Models: Antibiotic Resistance Testing and Host InteractionsDocument9 pagesStaphylococcus-Candida Interaction Models: Antibiotic Resistance Testing and Host InteractionsNorman BilliNo ratings yet
- A Clinical Study of Lodhra Kalka Paan With Nyagrodh Twak Kashaya and Panchavalkaladi Varti in Shweta Pradara (W.S.R To Leucorrhoea)Document12 pagesA Clinical Study of Lodhra Kalka Paan With Nyagrodh Twak Kashaya and Panchavalkaladi Varti in Shweta Pradara (W.S.R To Leucorrhoea)IJAR JOURNALNo ratings yet
- C - Albicans - Cellular and Molecular Biology - Prasad - R - PDFDocument552 pagesC - Albicans - Cellular and Molecular Biology - Prasad - R - PDFRodolfo Jonathan DelevauxNo ratings yet
- Anti-Candidal Activity of Homoeopathic Drugs: An In-Vitro EvaluationDocument6 pagesAnti-Candidal Activity of Homoeopathic Drugs: An In-Vitro EvaluationSk Saklin MustakNo ratings yet
- Morphology Examination of Yeast and MouldDocument17 pagesMorphology Examination of Yeast and MouldNOR SYUHADA BINTI BAHARUDIN / UPMNo ratings yet
- The Candida Treatment Revolution - Candida Cleanser (PDFDrive)Document50 pagesThe Candida Treatment Revolution - Candida Cleanser (PDFDrive)Sandra Milena BelloNo ratings yet
- Memoria Del Congreso PDFDocument197 pagesMemoria Del Congreso PDFRebeca Bibriesca SanchezNo ratings yet
- Sobue Et Al-2018-Molecular Oral MicrobiologyDocument12 pagesSobue Et Al-2018-Molecular Oral MicrobiologyLouise Dornelas FigueiraNo ratings yet
- Rogosa SL AgarDocument2 pagesRogosa SL AgarSubhajit GiriNo ratings yet
- Opportunistic MycosesDocument6 pagesOpportunistic MycosesJullana Rondina EscondeNo ratings yet