Professional Documents
Culture Documents
Recurrent Vaginal Candidiasis Guide
Uploaded by
amo94Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Recurrent Vaginal Candidiasis Guide
Uploaded by
amo94Copyright:
Available Formats
CONTINUING MEDICAL EDUCATION
Recurrent Vaginal Candidiasis
il
.,1/jJJJ!!IIi lI/JlfJ!iiUIl
K Y Loh, MMed(FamMed)*, N Sivalingam, FRCOG**
Department of Family Medicine, **Department of 0 & G, International Medical University, Jalan Rasah, 70300 Seremban, Negeri
Sembilan
Introduction
Vaginal candidiasis is one of the most common
gynecological problems seen in primary care.
Candida albicans account for 90% of the infection. It
is reported that all women will suffer at least one
episode of vaginal candidiasis during their life time and
up to 40-55% of them having recurrent vaginal
candidiasis'. Recurrent vaginal candidiasis is defined as
at least four discrete episodes of symptomatic infection
occurring in a year2". It is estimated that 5% of all
women who have a single episode of vaginal
candidiasis will experience chronic or recurrent
infection2
Recurrent vaginal candidiasis must be
distinguished from persistent infection in which there
is a symptom-free period in between the episodes of
infection. Up to 33% of recurrent vaginal candidiasis
is caused by non-albican species, which include C.
glabrata, C.tropicalis and Cparapsilosis.4.
Clinical features
Women with recurrent vaginal candidiasis often present
with intense vaginal discomfort. Common symptoms
include odourless whitish discharge, pruritus vulvae,
dyspareunia and dysuria. However, these symptoms
are not specific for candidiasis 2.'.4. The itch of pruritus
vulvae usually occurs in either mid-cycle or shortly
after menstruation. Severity of pruritus and vaginal
discharge positively correlate to higher yeast counts in
their culture'. Vaginal examination will usually reveal
erythema of vulva or vagina, presence of flaky vaginal
thrush and swelling of labia minora4 . Vaginal secretion
sent for microscopic examination with 10% potassium
hydroxide will demonstrate presence of yeast and
pseudohyphae. Typical budding yeast of candida is
seen in less than 30% of culture-positive cases.
Sensitivity and specificity of direct microscopy increases
to 70-100% if Gram's stain is performed. The yeast will
appear as gram-positive grape-like structure with grampositive germinating tubes of peudohyphae. Vaginal
swab for fungal culture is the gold standard for
diagnosis when a patient has persistent and recurrent
symptoms despite antimicrobial treatment"'.
Causes of recurrent candidiasis
Three primary theories have been proposed to explain
why women develop recurrent vaginal candidiasis.
First the intestinal reservoir theory suggest that
persistence of the organism in gastrointestinal tract later
This article was accepted: 11 November 2003
.
.
Corresponding Author: K Y Loh, Department of Family Medicine, IMU, Jolon Rasah 70300 Seremban, Negen Sembdan
788
Med J Malaysia Vol 58 No 5 December 2003
Recurrent Vaginal Candidiasis
reinfect the vagina.
This theory is based on
observation in uncontrolled data in the late 1970s in
which a concordance of almost 100% was observed
between rectal and vaginal cultures in women with
recurrent vaginal candidiasis. However, subsequent
studies failed to sustain this theory!,4.
The second hypothesis put forward is the sexual
transmission theory in which it is believed that the
sexual partner is the reservoir or source for recurrent
infection in the women.
Again subsequent studies
showed that in a majority of the cases the partner is
culture negative. One longitudinal study indicates that
the higher colonization rate in the man is reflective of
his exposure to chronically infected women rather than
he be the source. Treatment of the partner has no
effect on the women's risk of recurrence!4.
The third hypothesis is the vaginal relapse theory,
which states that even with treatment, some women
will remain colonized with the organism. The recurrent
symptoms is not caused by new infection but that the
organism increases in number and cause a new clinical
episode when the environment permits. This include
exogenous factors and also possibility of lowered local
vaginal immune response. Some of these well known
exogenous factors predisposing to recurrent vaginal
candidiasis are shown in Table I. It is important to
control these factors in managing recurrent vaginal
candidiasis ' '4.
may be misdiagnosed as recurrence. It was reported
that 15-20% of women with negative cultures after
treatment present again with positive culture within 3
months. If the infection occurs after a period free
period of 3 months follOWing the previous treated
episode, then it is more likely to be caused by a
different strain of candida'.
Differential diagnosis
Due to the availability of over the counter anti-fungal
medications, self-medication is common. In one study
it was found that up to 73% of women self treated with
over counter medications and 42 percent used
alternative medicines for self-treatment of recurrent
vaginal candidiasis.
However, when they were
evaluated at specialist centers, only 28% were actually
having vaginal candidiasis 4 It is therefore important to
take note of possibility of wrong diagnosis and
inappropriate use of medications.
Table II shows
some of the skin conditions may be misdiagnosed as
recurrent vaginal candidiasis.
Women taking oral contraceptive pills were found to
have higher rate of vaginal candidiasis. According to
one theory, candida cells have estrogen and
progesterone receptors which when stimulated can
cause fungal proliferation. Use of spermicidal jellies
and creams also increases susceptibility to infection by
altering the vaginal flora and increasing the adhesions
of candida species.
In patients using intrauterine
contraceptive devices, budding cells on the IUCD
threads could be a source reinfection.
Diabetes
mellitus stimulates formation of budding candida cells
and aids in transition from colonization to infection.
Cell mediated immunity also is less effective in killing
the yeasts in diabetic patients. Prolonged used of
broad spectrum antibiotics inhibit antibody synthesis
and phagocytic activity and lead to lower resistance to
yeast infection. One example is tetracycline shown to
cause faster detachment of young budding yeast from
the old blastoconidia.
Treatment
There are many treatment options for recurrent vaginal
candidiasis. Whichever regime is chosen, treatment
must always be individualized. The treating physician
must consider cost-effectiveness, convenience, possible
side effects and the availability of the medication. It is
also reminded that controlling underlying medical
conditions such as diabetes mellitus is absolutely
important and helpful. When recurrent infection' is
caused by C. albicans, it is best managed by using an
initial 14-day course of oral azoles antifungal. This will
induce clinical remission and negative fungal culture.
It is then followed" by 6. rponths maintenance regime'4.
Azoles drugs has broad~anti-fungalspectrum of efficacy
and high intensity of antimycotic activity. Effective
azoles medications include ketoconazole, itraconazole
and fluconazole.
Maintenance therapy using
clotrimazole vaginal pessary is an alternative to oral
maintenance therapy.
Most studies recommend
maintenance for six months after which the patient is
re-evaluated. For those who have recurrences once the
maintenance is over, they may need to be put on
medication for a longer period. However, the optimal
dosing interval in maintenance therapy is still not clear.
Table III shows the common recommended treatment
regime for acute infection and maintenance therapy.
Non-compliance with a treatment regime may result in
persistent infection by the similar strain and species and
C. albicans resistance to treatment is rare. However,
for infections caused by non-albican candida species,
Med J Malaysia Vol 58 No 5 December 2003
789
CONTINUING MEDICAL EDUCATION
clinical evidence of resistance seems common. In this
group of patients, terconazole vaginal cream is the drug
of choice'. This drug interferes with cytochrome P450
isoenzymes and is particularly effective against
G.tropicalis and G. glabrata'.
Boric acid vaginal
suppositories and topical flucytosine cream have also
been used successfully in non-albicans candidiasis'.
Nystatin vaginal pessary is one of the cheapest
antifungal agents but it is less effective than topical or
oral azoles in the treatment of candidiasis. Its use
usually requires up to 14 days. It is particularly useful
in patients who develop allergies to azoles and also in
the first trimester of pregnancy.
Alternative therapy
One study looked at the association between ingestion
of yogurt containing Lactobacillus acidophilus and the
prevention of recurrent vaginal candidiasis.
It was
found that ingestion of 80z of yogurt containing
Lactobacillus acidophilus decreases the rate of candidal
infection. However, subsequent studies fail to show any
significant results.
Other measures recommended
include wearing loose fitting cotton clothing and avoid
wearing tights altogether.
Again, little available
evidence on the efficacy of these measures is available'.
Similarly, use of substances such as vinegar and garlic
by some patients remains a fallacy.
Complications
Failure to treat recurrent vaginal candidiasis can lead to
various bio-psycho-social consequences. Patients may
present with recurrent dysparenia, which may lead to
unhappy sexual life. Some patients feel frustrated with
the sYJ;llptoms and suffer from reactive depression ,,4,5.
Besides depression, women with recurrent vaginal
candidiasis also complain of less satisfaction with life,
poor self esteem, anxiety and perceive life as more
stressful.
Table I: Risk factors for recurrent vaginal candidiasis
Host factors
Impaired glucose tolerance
Diabetes mellitus
Broad spectrum antibiotics
Contraceptive pills
Pregnancy
Use of spermicidal, jelly
Steroid therapy
Immunodeficiency
Mechanical irritation
Yeast Factors
Virulence: ability to adhere to vaginal epithelium.
Protease production: Increased invasiveness.
Germ tube formation: increase adherence.
Table II: Skin conditions misdiagnosed as recurrent vaginal candidiasis
Irritant contact dermatitis
Vulvar vestibulitis
Bacterial vaginosis
Genital herpes
Physiological discharge
Tinea cruris
Psoriasis
Lichen planus
790
Med J Malaysia Vol 58 No 5 December 2003
Recurrent Vaginal Candidiasis
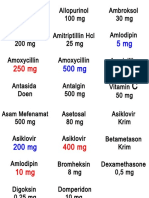
Table III: Recommended drug regime for recurrent vaginal candidiasis
Agent
Treatment for acute episode
Clotrimazole
Fluconazole
Ketoconazole
Terconazole cream
Maintenance
Clotrimazole
Ketoconazole
Fluconazole
Itraconazole
Dosing Regime
100mg vaginal pessary for 7 days
150mg orally single dose
200mg orally daily for 14 days
5g intravaginal for 3 days
Two 100mg vaginal pessary twice weekly for six months
Two 200mg oral tablets for 5 days after menses for six months
150mg orally once a month
200mg orally once a month
Recurrent vaginal candidiasis is a common problem in
clinical practice and can be frustrating for patients.
Proper diagnosis and prompt treatment will reduce
both the physical and psychological morbidity for the
patients.
Controlling of risk factors and underlying
medical disease such as diabetes mellitus and impaired
glucose tolerance helps in preventing recurrent vaginal
candidiasis.
Use of maintenance therapy following
treatment of acute symptoms has a role in preventing
recurrent vaginal candidiasis.
1.
Denning D W. Fortnightly review: Management of genital
candidiasis. BM] 1995; 310: 1241-44.
5.
2.
Ringdahl E N. Treatment of recurrent vulvovaginal
candidiasis. Am Fam Physician 2000; 61: 3306-312.
Irving G,Miller D, Robinson A, Reynolds S, Copas A].
Psychological factors associated with recurrent vaginal
candidiasis: a preliminary stu.dy. Sex Transm Infect 1998;
74: 334-38.
3.
Tanaka, Diane. Management of vaginal candidiasis: A
review. Pediatr Infect Dis] 1998; 17: 746-47.
6.
4.
Nyirjesy P. Chronic vulvovaginal candidiasis. Am Fam
Physician 2001; 63: 697-702.
Donders GG, Prenen H, Verbeke G, reybrouck R.
Impaired tolerance for glucose in women with recurrent
vaginal candidiasis. Am] Obstet Gynecol 2002; 184: 98993.
7.
Marrazzo]. Valvovaginal candidiasis. BM] 2002; 325: 58687.
Conclusion
Med J Malaysia Vol 58 No 5 December 2003
791
CONTINUING MEDICAL EDUCATION
Recurrent Vaginal Candidiasis:
Multiple Choice Questions (MCQs)
1.
A.
B.
C.
D.
E.
The following are features of recurrent vaginal candidiasis.
Persistent greenish vaginal discharge.
Pruritus vulvae
Dyspareunia
Dysuria
Vaginal bleeding
2. Risk factors for recurrent vaginal candidiasis include:
A. Steroid therapy
B. Broad spectrum antibiotics
C. Oral contraceptive pills
D. Impaired glucose tolerance
E. Hypertension
3. The following vulva conditions may be misdiagnosed as recurrent candidiasis:
A. Psoriasis
B. Contact dermatitis
C. Lichen planus
D. Vulvar vestibulitis
E. Tinea cruris
4. the following drugs are effective in treating recurrent vaginal candidiasis:
A. Oral itraconazole
B. Clotrimazole vaginal pessary
C. Oral tetracycline
D. Oral fluconazole
E. Oral terbinafine
5. Psychosocial complications of recurrent vaginal candidiasis include:
A. Reactive depression
B. Low self esteem
C. Unsatisfaction with sexual life
D. Increase medical cost
E. Anxiety
792
Med J Malaysia Vol 58 No 5 December 2003
You might also like
- Acute Vulvovaginitis: Clinical Prac TiceDocument9 pagesAcute Vulvovaginitis: Clinical Prac TicewiwiknovitasariNo ratings yet
- Vaginal Discharge Causes and ManagementDocument5 pagesVaginal Discharge Causes and ManagementHassan Abdullah AL-balushiNo ratings yet
- 2014 Diagnosis of Pelvic Inflammatory Disease (PID) Intra Operative Findings and ComparisonDocument7 pages2014 Diagnosis of Pelvic Inflammatory Disease (PID) Intra Operative Findings and ComparisonUrología GinecológicaNo ratings yet
- Clinical Trial - Use of Oral Probiotics As An Adjunctive Therapy To Fluconazole in The Treatment of Yeast VaginitisDocument3 pagesClinical Trial - Use of Oral Probiotics As An Adjunctive Therapy To Fluconazole in The Treatment of Yeast VaginitisneleatucicovshiiNo ratings yet
- Urinary Tract Infections During PregnancyDocument8 pagesUrinary Tract Infections During PregnancyGloria SaldivarNo ratings yet
- An Update On The Management of Acute Pelvic Inflammatory DiseaseDocument3 pagesAn Update On The Management of Acute Pelvic Inflammatory DiseaseVinnyRevinaAdrianiNo ratings yet
- 33 - 4 - 07-Dr - KhademDocument5 pages33 - 4 - 07-Dr - Khademedy744No ratings yet
- United Kingdom National Guideline On The Management of Vulvovaginal Candidiasis (2007)Document5 pagesUnited Kingdom National Guideline On The Management of Vulvovaginal Candidiasis (2007)Anonymous Tzn8RGBZ4No ratings yet
- Prevalence of Vaginal Candidiasis in Pregnancy Among Coastal South Indian Women HnYuDocument3 pagesPrevalence of Vaginal Candidiasis in Pregnancy Among Coastal South Indian Women HnYuEdogawa RakhmanNo ratings yet
- Vaginal Discharge: Clinical ReviewDocument5 pagesVaginal Discharge: Clinical ReviewOktari Dwi YantiNo ratings yet
- N00159 South Africa Vulvovaginal Candidiasis SEP2016 Rev000Document2 pagesN00159 South Africa Vulvovaginal Candidiasis SEP2016 Rev000Endy SitumbekoNo ratings yet
- 05 N037 38983Document22 pages05 N037 38983MeghaNo ratings yet
- Vulvovaginitis: by James Holencik, DODocument70 pagesVulvovaginitis: by James Holencik, DOSyarifa YuliaNo ratings yet
- Vaginal CandidiasisDocument29 pagesVaginal CandidiasisMike Serge RazafiNo ratings yet
- Chlamydia and Nonspecific UrethritisDocument4 pagesChlamydia and Nonspecific UrethritisErfina BasriNo ratings yet
- Pelvic Inflammatory DiseaseDocument43 pagesPelvic Inflammatory DiseaseFauzia Jamiri - Abdurasid100% (2)
- Vaginal Infections Update: Original ReviewDocument6 pagesVaginal Infections Update: Original ReviewEpi PanjaitanNo ratings yet
- 72 2006 VaginitisDocument12 pages72 2006 VaginitisEdwin AtencioNo ratings yet
- PresusDocument6 pagesPresusFrishia DidaNo ratings yet
- NEJMoa033114 KulitDocument8 pagesNEJMoa033114 KulitelsyamelindaNo ratings yet
- Jurnal Pubmed EndoDocument6 pagesJurnal Pubmed EndoSofyanNo ratings yet
- Gyne - (Section B) PID-STI-1Document45 pagesGyne - (Section B) PID-STI-1Kailash KhatriNo ratings yet
- Treatment of Asymptomatic Vaginal Candidiasis in Pregnancy To Prevent Preterm Birth An Openlabel Pilot Randomized ContrDocument7 pagesTreatment of Asymptomatic Vaginal Candidiasis in Pregnancy To Prevent Preterm Birth An Openlabel Pilot Randomized ContrariestianiNo ratings yet
- Effect of Probiotic in Treatment of Recurrent Vulvovaginal CandidiasisDocument8 pagesEffect of Probiotic in Treatment of Recurrent Vulvovaginal CandidiasisRizka Hidya Tiffani IINo ratings yet
- 51 Vaginal Discharge & PIDDocument45 pages51 Vaginal Discharge & PIDcollinsmagNo ratings yet
- Pelvic Infections in Women: Belgian Guidelines: OutlineDocument35 pagesPelvic Infections in Women: Belgian Guidelines: OutlineJose mauricio PalenciaNo ratings yet
- Gupta Bowman 2012 Managing Sexually Transmitted Infections in Pregnant WomenDocument9 pagesGupta Bowman 2012 Managing Sexually Transmitted Infections in Pregnant WomenNaresh Babu.TNo ratings yet
- Vaginal CandidiasisDocument31 pagesVaginal CandidiasisMutabazi Sharif100% (1)
- Metronidazole Vaginal Gel 075Document6 pagesMetronidazole Vaginal Gel 075neleatucicovshiiNo ratings yet
- Real-World Data of Helicobacter Pylori Prevalence, Eradicationregimens, and Antibiotic Resistance in Thailand, 2013-201Document5 pagesReal-World Data of Helicobacter Pylori Prevalence, Eradicationregimens, and Antibiotic Resistance in Thailand, 2013-201andi kulokNo ratings yet
- EndometritisDocument6 pagesEndometritisandriansyah2110% (1)
- Management of Persistent Vaginitis .99281 PDFDocument12 pagesManagement of Persistent Vaginitis .99281 PDFWinna Eka PNo ratings yet
- Cdi and FMT Risks and BenefitsDocument5 pagesCdi and FMT Risks and Benefitsapi-426734065No ratings yet
- Kandidiasis Vulvovaginalis Pada Pasien SLEDocument7 pagesKandidiasis Vulvovaginalis Pada Pasien SLEkika byunNo ratings yet
- National Guideline on Managing Vulvovaginal CandidiasisDocument5 pagesNational Guideline on Managing Vulvovaginal CandidiasisLeanyn AndiniNo ratings yet
- Ef Cacy and Safety of A Single Oral 150 MG Dose of Uconazole For The Treatment of Vulvovaginal Candidiasis in JapanDocument7 pagesEf Cacy and Safety of A Single Oral 150 MG Dose of Uconazole For The Treatment of Vulvovaginal Candidiasis in JapanMuhammad IkbarNo ratings yet
- CandidaDocument56 pagesCandidasaraabolghasemi1No ratings yet
- Pelvic Inflammatory DiseaseDocument34 pagesPelvic Inflammatory DiseaseOhunakin AfolabiNo ratings yet
- Infestation of Endometrium by Mycobacterium Tuberculosis Bacilli-Cause of Reproductive FailureDocument10 pagesInfestation of Endometrium by Mycobacterium Tuberculosis Bacilli-Cause of Reproductive FailureMathivanan AnbazhaganNo ratings yet
- Enteric Fever 2013Document3 pagesEnteric Fever 2013aminceloNo ratings yet
- Asymptomatic Trichomonas & Candida Colonization Impact on PregnancyDocument7 pagesAsymptomatic Trichomonas & Candida Colonization Impact on PregnancyalvilNo ratings yet
- Congenital Syphilis Causes and TreatmentDocument4 pagesCongenital Syphilis Causes and TreatmentAlya Putri Khairani100% (1)
- Candida vulvovaginitis clinical manifestationsDocument18 pagesCandida vulvovaginitis clinical manifestationsCindyNo ratings yet
- 1756 0500 5 197Document7 pages1756 0500 5 197El tren del MameNo ratings yet
- Gynaecology: Gum, Fertility, Contraception, and UrogynaecologyDocument46 pagesGynaecology: Gum, Fertility, Contraception, and UrogynaecologyOccamsRazorNo ratings yet
- Tuberculosis and Pregnancy ManduaDocument16 pagesTuberculosis and Pregnancy ManduaMinorC3No ratings yet
- Management of Urinary Tract Infection in Women A Practical Approach For Everyday PracticeDocument23 pagesManagement of Urinary Tract Infection in Women A Practical Approach For Everyday PracticeKeysha AbigailNo ratings yet
- Iaat 12 I 9 P 187Document8 pagesIaat 12 I 9 P 187Maniak LuckNo ratings yet
- Treatment of Chlamydia Trachomatis InfectionDocument9 pagesTreatment of Chlamydia Trachomatis InfectioneeeeewwwwwNo ratings yet
- Vaginitis - ACOG 2019Document12 pagesVaginitis - ACOG 2019J RNo ratings yet
- 43 Pukar EtalDocument3 pages43 Pukar EtaleditorijmrhsNo ratings yet
- Urethritis in FemaleDocument7 pagesUrethritis in FemaleRika SuryanaNo ratings yet
- Acute VulvovaginitisDocument8 pagesAcute VulvovaginitisKagek BheNo ratings yet
- 1 Gynecologic Infections 2Document109 pages1 Gynecologic Infections 2Girum SolomonNo ratings yet
- Clostridium Difficile: Isolation of The Hospitalized Patient: Control MeasuresDocument5 pagesClostridium Difficile: Isolation of The Hospitalized Patient: Control MeasuresSizi DiazNo ratings yet
- Sexually Transmitted Diseases: Jasmin P. EgargueDocument33 pagesSexually Transmitted Diseases: Jasmin P. EgargueLiza AingelicaNo ratings yet
- 1b BV ReviewDocument5 pages1b BV Reviewrisda aulia putriNo ratings yet
- USMLE Step 3 Lecture Notes 2021-2022: Internal Medicine, Psychiatry, EthicsFrom EverandUSMLE Step 3 Lecture Notes 2021-2022: Internal Medicine, Psychiatry, EthicsRating: 5 out of 5 stars5/5 (9)
- G-Ranitidine: Commonly used medicines for acid reflux and ulcersDocument4 pagesG-Ranitidine: Commonly used medicines for acid reflux and ulcersHoney Grace L LemorenasNo ratings yet
- Puskesmas: Kaibon: NO Nama BMHP Kemasan Total Harga 1 2 3 4 5 6 7 8 RP 9.00 Dau + Dak: Harga SatuanDocument12 pagesPuskesmas: Kaibon: NO Nama BMHP Kemasan Total Harga 1 2 3 4 5 6 7 8 RP 9.00 Dau + Dak: Harga SatuanyunitacahyaniiNo ratings yet
- Sambungan Data Persediaan Obat PuskesmasDocument7 pagesSambungan Data Persediaan Obat PuskesmasMerry OctafiaNo ratings yet
- Ccs Tips Step 3Document18 pagesCcs Tips Step 3JMi Grca Pbla100% (6)
- CVS MCQsDocument36 pagesCVS MCQsskNo ratings yet
- Kasus 1 HIVDocument78 pagesKasus 1 HIVDina0% (1)
- Label OBATDocument22 pagesLabel OBATal13zaNo ratings yet
- Daftar Harga ObatDocument4 pagesDaftar Harga ObatKadek Soga Prayaditya PutraNo ratings yet
- EPI Schedule Malawi COM 2017Document2 pagesEPI Schedule Malawi COM 2017INNOCENT KHULIWANo ratings yet
- DR / Osama Ahmed: Contact UsDocument20 pagesDR / Osama Ahmed: Contact UsAhmed AliNo ratings yet
- Diabetes QuestionsDocument8 pagesDiabetes QuestionsJohn Osborne100% (1)
- Clinical Pathways for Appendicitis PerforationDocument4 pagesClinical Pathways for Appendicitis PerforationAnton Trihartanto100% (2)
- Soap Note 4 (CPII)Document5 pagesSoap Note 4 (CPII)Flor OM89% (37)
- DDD Consumption Report TemplateDocument14 pagesDDD Consumption Report TemplatenicoletagenovevaNo ratings yet
- Diffrent Types of IVFDocument2 pagesDiffrent Types of IVFGail SantosNo ratings yet
- Overview of Measles DiseaseDocument3 pagesOverview of Measles DiseaseLighto RyusakiNo ratings yet
- Septicemia PresentationDocument23 pagesSepticemia Presentationapi-548307464No ratings yet
- Golongan Obat Casemix1Document31 pagesGolongan Obat Casemix1FiniNo ratings yet
- IDBDocument2 pagesIDByondaime15No ratings yet
- PHARMACOTHERAPEUTICS - II CASE PRESENTATION ON PSORIASIS by SRIRAM ADocument21 pagesPHARMACOTHERAPEUTICS - II CASE PRESENTATION ON PSORIASIS by SRIRAM ASriram Surya100% (1)
- CH 38 Cardiotonic and InotropicDocument2 pagesCH 38 Cardiotonic and InotropicHannaNo ratings yet
- Cagayan Valley Medical Center: 2017 List of Procured and Consigned MedicinesDocument15 pagesCagayan Valley Medical Center: 2017 List of Procured and Consigned MedicinesJZik SibalNo ratings yet
- Prefix, Suffix of DrugsDocument6 pagesPrefix, Suffix of DrugsBriel Jake CabusasNo ratings yet
- Rash FeverDocument1 pageRash FeverSyima MnnNo ratings yet
- OrchitisDocument5 pagesOrchitisNader SmadiNo ratings yet
- Drug Study CeftriaxoneDocument2 pagesDrug Study CeftriaxoneBianca Freya Porral94% (17)
- Health Data Vision ResponesDocument12 pagesHealth Data Vision ResponesSmruti RanjanNo ratings yet
- Febrile Seizures Epilepsy OSCE Counselling PaediatricsDocument6 pagesFebrile Seizures Epilepsy OSCE Counselling PaediatricsJJ Lim100% (1)
- Neonatal SeizuresDocument22 pagesNeonatal SeizuresKatrin Marcelina SihombingNo ratings yet
- Tetanus BrochureDocument2 pagesTetanus BrochureOpuntia PclNo ratings yet