Professional Documents
Culture Documents
Study: Youth Diabetes 2014
Uploaded by
The Vancouver SunCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Study: Youth Diabetes 2014
Uploaded by
The Vancouver SunCopyright:
Available Formats
DIABETICMedicine
DOI: 10.1111/dme.12657
Research: Epidemiology
Diabetes in the young: a population-based study of South
Asian, Chinese and White people
C. Ke1, P. Sohal2, H. Qian3, H. Quan4 and N. A. Khan1,3
1
Department of Medicine, University of British Columbia, 2Department of Family Medicine, University of British Columbia, 3Center for Health Evaluation and
Outcomes Sciences, University of British Columbia, Vancouver, Canada and 4Department of Community Health Sciences, University of Calgary, Calgary, Canada
Accepted 1 December 2014
Abstract
Aims Rates of diabetes mellitus in the young have not been quantified on a population level, particularly in South Asian
and Chinese populations, which bear high rates of diabetes. We determined the incidence of diabetes (Type 2 diabetes
and diabetes using insulin only) and rates of hospitalizations among South Asian, Chinese and White people aged 5
29 years with newly diagnosed diabetes.
Methods People with newly diagnosed diabetes (19972006) in British Columbia, Canada were identified using
population-based administrative data and pharmacy databases. Age-standardized incidence rates were calculated for
people with diabetes prescribed insulin only and those with Type 2 diabetes. They were followed for up to 8 years for all
hospitalizations and diabetes-related complications.
There were 712 South Asians, 498 Chinese and 6176 White people aged 529 years with diabetes. Most youth
with diabetes had Type 2 diabetes (South Asian 86.4%; Chinese 87.1% and White 61.8%). The incidence of diabetes on
insulin only was highest in White people compared with the other groups. The incidence of Type 2 diabetes was highest
in South Asians, particularly in 2029-year-olds, with rates 2.2 times that of White people and 3.1 times that of Chinese
people. Hospitalization and diabetes-related complications were uncommon in all groups.
Results
The incidence of Type 2 diabetes is higher than previously estimated among youth and is now surpassing
diabetes on insulin only. Significant reductions in Type 2 diabetes screening ages in South Asians need to be considered
and prevention efforts are urgently required in childhood and adolescence. Global estimates need to consider the
epidemic of Type 2 diabetes in the young.
Conclusion
Diabet. Med. 00, 000000 (2015)
Introduction
Type 2 diabetes mellitus had been virtually non-existent in
persons younger than 30 years until recently. Reports suggest
rapid increases in Type 2 diabetes incidence among younger
people, with 45% of newly diagnosed diabetes in adolescents
occurring from Type 2 diabetes, compared with 3% just two
decades ago [1]. The growing incidence of Type 2 diabetes in
the young is thought to be due to urbanization, increased
sedentariness, rapid dietary transitions and population
increases in ethnic groups with a greater propensity for
developing diabetes [2]. The burden of diabetes in the young
is relevant given that over half of the global population is
aged 29 years or less [3]. India and China have disproportionately young population structures with the highest
numbers of young people globally, totalling over 1.2 billion
people aged 29 years and younger. South Asian and Chinese
populations also comprise 62% of the worlds population of
adults with Type 2 diabetes [4]. Despite this burden of
disease, diabetes rates in young South Asian and Chinese
people remain largely unknown. International diabetes
guidelines recommend screening for Type 2 diabetes more
frequently and earlier than age 40 years in Asian populations
[57], but this age cut-off point may be underestimated given
the lack of data on young people outside the scope of existing
paediatric studies.
We sought to evaluate the incidence of diagnosed diabetes,
those prescribed insulin only and those with Type 2 diabetes,
in South Asian, Chinese and White people using a large,
population-based study in people aged 529 years in British
Columbia, Canada. We also characterized care providers by
specialty (i.e. family practice, paediatrics, internal medicine
including endocrinology) and outcomes including all
Correspondence to: Calvin Ke. E-mail: c.ke@alumni.ubc.ca
2014 The Authors.
Diabetic Medicine 2014 Diabetes UK
DIABETICMedicine
Whats new
We have been unable to determine Type 2 diabetes rates
in young populations because previous paediatrician
surveys significantly underestimated rates. The newly
identified Type 2 diabetes rate is much higher, surpassing that of Type 1 diabetes. This has not been reported
previously and is highly relevant for screening.
South Asian people aged 20 years and above had much
higher rates of Type 2 diabetes, suggesting a need to
reduce screening age.
Global Type 2 diabetes rates in people below 29 years
of age may be drastically higher than previously
recognized. Although half the worlds population is
aged less than 29 years, WHO global estimates are
based on people over age 25 years.
hospitalizations and diabetes-related complications including
diabetic ketoacidosis and hyperglycaemic hyperosmolar state.
Methods
Data sources
Administrative data from the Canadian Province of British
Columbia (19972006) were used. British Columbia includes
22% of Canadas South Asian population (210 400) and
34% of Canadas Chinese population (373 800) [8,9].
British Columbia has a total population of 4.6 million
people with over 1.5 million at risk for diabetes aged 5
29 years. The administrative data included physician claims
for all inpatient and outpatient encounters (Medical Services
Plan Payment Information; http://www.popdata.bc.ca/data),
and International Classification of Diseases (IICD9 and
IICD10) codes were extracted for each encounter. Inpatient
data are collected from hospital discharge abstracts, which
contain primary and secondary discharge diagnosis codes
(Discharge Abstract Database; http://www.popdata.bc.ca/
data). Under the universal healthcare system, these comprehensive data include virtually all British Columbia residents.
Medication data were obtained from a provincial electronic
database (PharmaNet; http://www.popdata.bc.ca/data),
which contains a record of all dispensed prescriptions and
date of dispensation regardless of age. Population denominators were determined from a population registry data file
that provides annual population counts.
Study population
The study population was restricted to people aged
529 years at the time of diagnosis. People with diabetes
were identified with an IICD9 or IICD10 code for diabetes
for at least one hospital discharge abstract or two physician
Diabetes in the young: a population-based study ! C. Ke et al.
claims within 2 years (IICD9-CM: 250.x; IICD10: E109,
E119, E139, E149, E101, E111, E131, E141, E105, E115,
E135, E145). Date of diabetes incidence was defined as the
date of the first IICD9 or IICD10 code. This algorithm has
been extensively validated in those aged under 20 years
(sensitivity 94.2100%, specificity 93.599.9%) [10,11] and
in those aged 35 years and over (sensitivity 92.3%, specificity 96.9%) [2,12,13]. We excluded women with an obstetrical event (IICD9 code 650669 or IICD10 code O1314,
O29, O4748, O6075, O8084) within 5 months of
diabetes diagnosis to exclude gestational diabetes mellitus.
Categorizing diabetes on insulin only and Type 2 diabetes
We identified people with diabetes who take insulin only as
those with a diabetes diagnosis having a prescription for
insulin and no other diabetes medication aside from insulin
at any time during the study period. Use of insulin only
captures two major categories of people: those with Type 1
diabetes and those with Type 2 diabetes treated with only
insulin at all times during the study period. Notably, use of
insulin only has a 96.8% sensitivity for identifying Type 1
diabetes [10]. Therefore, the remaining study population was
categorized as having Type 2 diabetes. This group included
people on non-insulin diabetes medication with or without
adjunctive insulin therapy, as well as people with a diabetes
diagnosis not prescribed any diabetes medications.
Categorizing ethnic group
Administrative health data in Canada is not linked to
self-reported ethnicity. To identify people of South Asian
and Chinese descent, we performed surname analysis using
the validated Nam Pehchan and Quan surname algorithms,
which have a 7894% sensitivity, 99.499.7% specificity
and 6396% positive predictive value [1417]. In Canada,
93.2% of South Asians and 90.5% of Chinese marry people
of the same ethnocultural background, minimizing misclassification due to mixed marriages [18]. The rest of the
population consists mainly of Caucasians (93.2%) with very
few from Aboriginal and visible minority groups [19].
Therefore, we characterized this group as White.
Procedures
Incident cases of diabetes were determined for the years
19972004. To exclude people with pre-existing diabetes, we
removed those with a diabetes diagnosis within 3 years prior
to 1997. We included only people with health insurance
registration 3 years prior to diabetes diagnosis to avoid
falsely identifying new immigrants with pre-existing diabetes
as incident cases. Population totals were obtained from the
provincial population registry with surname algorithms
applied to minimize denominator bias. Medical specialty of
care providers (family medicine, paediatrics, internal medi 2014 The Authors.
Diabetic Medicine 2014 Diabetes UK
DIABETICMedicine
Research article
cine) were identified by physician visits within 2 years of
diagnosis.
The following conditions were defined from the Charlson
comorbidities list [20]: hypertension (IICD9 401404,
IICD10 I1013), asthma (IICD9 493, IICD10 J45), renal
disease (IICD9 580586, IICD10 N00-N19), cancer
(IICD9 140239, IICD10 C0097 and D00D48) and
polycystic ovarian syndrome (IICD9 256.4, IICD10
E28.2). We estimated socio-economic status using the
chronologically closest census data by assigning median
income derived from postal code. We assigned a missing
value for missing post codes (566 people: 3.6% Chinese,
6.7% South Asian, 8.5% White).
Statistical analysis
Baseline data were described as mean and standard deviation (SD) if continuous, and as counts and percentage if
categorical. Comparisons between ethnic groups were
performed using the analysis of variance (ANOVA) for
continuous variables. For categorical variables, we used the
v2 test.
Age-standardized incidence rates were calculated using a
direct method with the British Columbia 2001 population as
the reference population. Confidence intervals for age-standardized rate estimates were calculated according to the
method based on gamma distribution [21].
We measured the following outcomes: time to first
hospitalization for any cause and time to first occurrence of
diabetic ketoacidosis or hyperglycaemic hyperosmolar state
(IICD9 codes 250.1250.3; IICD10 codes E10.0E10.1).
To evaluate the association between ethnic groups with
outcomes within each diabetes subtype, separate Cox
proportional hazards models were constructed with adjusting pre-specified confounding variables (age, sex, socio-economic status, and baseline comorbidities). The observation
time started at time of diagnosis and ended on the date of
occurrence of outcomes. People with no occurrence of
outcomes of interest in the study were censored at the time
of death or until the last available date within the study
period that the patient was confirmed to be registered under
the provincial healthcare plan. The proportional hazards
assumption was tested by scaled Sch
oenfeld residuals. Firth
correction methods were applied in the models in case of
monotone likelihood with infinite estimates [22]. Cox
proportional hazards models were also performed within
each age group.
A two-tailed P-value < 0.05 was considered as statistically
significant. All analysis was conducted using SAS software
v. 9.3 (SAS Institute Inc., Cary, NC, USA) and R 2.15 (R
Foundation for Statistical Computing, Vienna, Austria).
Graphs were plotted using Microsoft Excel 2002 (Microsoft
Corporation, Redmond, WA, USA). This study was
approved by the University of British Columbia Providence
research ethics board.
2014 The Authors.
Diabetic Medicine 2014 Diabetes UK
Results
There were 7388 incident cases of diabetes detected, with
712 South Asians (9.64%), 498 Chinese (6.74%) and 6176
White people (83.62%). Most South Asian and Chinese
people with diabetes had Type 2 diabetes (86.4% and
87.1%, respectively), compared with 61.8% in White
people. People using insulin only were younger than those
with Type 2 diabetes (Table 1). Among females, polycystic
ovarian syndrome was rare.
Diabetes incidence
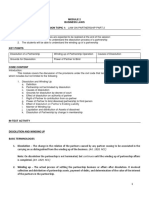
For the insulin-only cohort, the age-standardized average
incidence of diabetes was 1.7 times higher in White people
than in South Asians and 5.6 times higher than in Chinese
people in the age groups under 20 years and 2029 years (see
Table 2, Figs 1a and 2a). Over half (57.1%) of those in the 5
9 years age group were taking insulin only. Age-standardized
average incidence of Type 2 diabetes was 2.2 times higher in
South Asians than in White people and 3.1 times higher
compared with Chinese people in those aged 2029 years.
Although the majority of Type 2 diabetes cases in South Asian
people were in those aged 20 years and above, the incidence
rate in South Asians is slightly higher than in the White and
Chinese groups up to age 19 years (see Fig. 1b). Rates of
Type 2 diabetes were higher in the 2029 years age group
than in the 519 years age group, regardless of ethnicity.
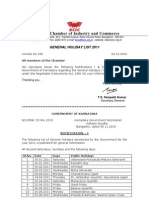
Time trends
The age-standardized incidence showed no grossly observable changes over time for people on insulin only (Fig. 2a).
Incidence of Type 2 diabetes appeared to be stable in all
ethnic groups (Fig. 2b).
Medical specialty of the care providers
Over 80% of people with diabetes were seen by family
physicians within 2 years of diagnosis (Table 3). The majority
of people aged 519 years on insulin only were seen by
paediatricians (81.7%), compared with only 26.9% of those
with Type 2 diabetes in this age group. People aged 2029 years
on insulin only were more likely to be seen by internal medicine
specialists (67.2%) compared with all other groups.
Medication use
Among people with Type 2 diabetes, a consistent majority
across all ethnicities (56.558.1%) were treated without
diabetes medication. Mean follow-up time was 4.73 years.
Among those treated with medication, Chinese people were
more commonly treated using non-insulin agents only,
whereas White people were most commonly treated using a
combination of insulin and non-insulin agents.
DIABETICMedicine
Diabetes in the young: a population-based study ! C. Ke et al.
Table 1 Baseline characteristics among people with diabetes aged 529 years in British Columbia
South Asian (n = 712)
Characteristics
Diabetes on insulin only (%)
13.6
Type 2 diabetes (%)
86.4
Age at diagnosis, mean (years) " SD or %
All
22.8 " 6.2
Diabetes on insulin only
15.9 " 7.0
Type 2 diabetes
23.9 " 5.4
59 years
7.9
1014 years
7.1
1519 years
11.1
2029 years
73.9
Female (%)
54.8
Socio-economic euintile (%)
1st (low)
28.9
2nd
27.5
3rd
20.4
4th
13.1
5th (high)
3.4
Unknown
6.7
Comorbidities (%)
Hypertension
5.6
Asthma
5.6
Renal disease
0.6
Cancer
1.1
Polycystic ovarian syndrome*
0.8
Medication use among popel with Type 2 diabetes (%)
Non-insulin hypoglycaemic agents only
29.4
Non-insulin agents and insulin
12.5
No diabetes medications
58.1
Chinese (n = 498)
White (n = 6176)
12.8
87.2
38.3
61.7
< 0.0001
21.9 " 5.7
17.2 " 7.6
22.6 " 5.0
4.4
11.4
20.3
63.9
52.2
19.8 " 7.2
15.6 " 7.2
22.4 " 5.9
14.7
15.8
16.3
53.2
51.7
< 0.0001
0.21
< 0.0001
< 0.0001
26.7
24.3
16.3
17.1
12.0
3.6
21.0
18.8
18.0
16.8
17.0
8.5
< 0.0001
4.8
4.0
0.4
2.0
0.4
3.7
6.0
0.6
1.3
0.7
0.03
0.17
0.95
0.31
0.85
33.0
10.6
56.5
25.2
17.8
57.0
< 0.0001
0.29
*Among females with Type 2 diabetes only.
Table 2 Age-standardized average incidence of diabetes mellitus by ethnicity and treatment regimen in people aged 529 years for 19972004
inclusive (per 100 000 patient-years)
Age-standardized average incidence [95% CI]
Patient subgroup
Ethnicity
Age 519
Age 2029
All ages
Diabetes on insulin only
South Asian
Chinese
White
South Asian
Chinese
White
16.77 [12.64, 21.87]
4.7 [3.30, 6.52]
26.64 [25.26, 28.08]
22.88 [18.09, 28.60]
11.47 [9.33, 14.00]
17.48 [16.36, 18.65]
9.61
3.54
18.98
147.15
46.92
67.07
13.83
4.23
23.50
73.90
26.03
37.84
Type 2 diabetes
Risk of complications and hospitalization
All-cause hospitalization, diabetic ketoacidosis and hyperglycaemic hyperosmolar state were uncommon across all
ethnic groups. For people on insulin only, South Asians aged
2029 years were significantly more likely to be hospitalized
for any reason (P = 0.007; Table 4). There were no significant differences in hospitalization observed between Chinese
and White people, and no significant difference in diabetes-related complications among South Asian and Chinese
people.
For the Type 2 diabetes cohort, Chinese people were
significantly less likely to be hospitalized for any reason
[6.48, 13.76]
[2.19, 5.42]
[17.58, 20.46]
[133.77, 161.51]
[41.57, 52.77]
[64.41, 69.81]
[11.02, 17.18]
[3.20, 5.49]
[22.50, 24.53]
[67.67, 80.61]
[23.47, 28.81]
[36.56, 39.15]
compared with White people. South Asians were less likely to
have diabetes-related complications compared with White
people, but there was no significant difference in total
hospitalizations.
Discussion
This population-based analysis found high rates of Type 2
diabetes in all groups, but substantially higher rates among
South Asian youth aged 2029 years than White or Chinese
people. Conversely, White youth had high rates of diabetes
using insulin only compared with the other ethnic groups.
Time trends revealed stable rates of diagnosis over the 8-year
2014 The Authors.
Diabetic Medicine 2014 Diabetes UK
DIABETICMedicine
Research article
(a) 35
Incidence Rate
30
25
South
Asian
20
Chinese
15
White
10
5
0
5-9
10-14
15-19
20-24
25-30
Age Group
(b)
250
Incidence Rate
200
South
Asian
150
Chinese
100
White
50
0
5-9
10-14
15-19
20-24
25-30
Age Group
FIGURE 1 (a) Crude age-specific incidence of diabetes on insulin only according to ethnicity (not age adjusted; incidence rates per 100 000). Based
on Poisson regression, White people had a significantly higher crude incidence rate versus Chinese people in all age groups (P < 0.0001). White
people also had a significantly higher crude incidence rate versus South Asian people in the 1014 years age group (P = 0.02) and in the 2030 years
age group (P = 0.01). (b) Crude age-specific incidence of Type 2 diabetes according to ethnicity (not age adjusted; incidence rates per 100 000).
Based on Poisson regression, South Asian people had a significantly higher crude incidence rate in the 2024 years age group compared with Chinese
(P < 0.0001) and White people (P = 0.001). In the 2530 years age group, South Asian people also had a significantly higher crude incidence rate
compared with both Chinese and White people (P < 0.0001).
observation period and low rates of diabetes-related hospitalizations, especially among Chinese people.
Until recently, diabetes in youth has been predominantly
and almost exclusively due to Type 1 diabetes [1]. Our study
found high proportions of Type 2 diabetes in adolescents and
young adults aged 2029 years in all ethnic groups. This
rapid increase in Type 2 diabetes in youth is thought to
correlate with the rising rates of obesity and inactivity in
young people. Previous estimates of the magnitude of this
Type 2 diabetes epidemic have been based on national
surveys of paediatric specialists [23,24]. We found that only
a quarter of people with Type 2 diabetes aged 519 years
were seen by paediatricians compared with 81.7% for people
on insulin only. This finding suggests that Type 2 diabetes
rates have been significantly underestimated by previous
studies because the majority of people with Type 2 diabetes
being treated by family physicians would have been excluded
from these studies that utilized a paediatrician survey
methodology. Specifically, a Canadian survey reported a
Type 2 diabetes minimum incidence rate of 2.34 per
2014 The Authors.
Diabetic Medicine 2014 Diabetes UK
100 000 [24], whereas a UK survey reported an incidence
rate of 1.3 for children under 17 [23]. In the landmark US
SEARCH cohort study of participants with diagnosed
diabetes, the incidence rate of Type 2 diabetes in the
non-Hispanic White population aged 519 years of age
was 3.0 per 100 000 [25]. By contrast, we found drastically
higher rates of Type 2 diabetes in White people aged
519 years (17.48 per 100 000). Although the SEARCH
study included data from multiple sources including hospitals, health plans and recruited physicians, in a non-universal
healthcare setting potential cases may have been missed using
this methodology.
It is well-recognized that the South Asian adult population
aged > 35 years bears a large burden of Type 2 diabetes [13].
Type 2 diabetes incidence appears to be slightly higher in
South Asians under age 20 years, with the majority of the
increase in incidence observed in the 2029 years age group.
Our study suggests that this increased risk of Type 2 diabetes
in South Asians starts much earlier in life than previously
known and the cumulative incidence magnifies with age.
DIABETICMedicine
Diabetes in the young: a population-based study ! C. Ke et al.
(a) 35
Incidence Rate
30
25
South
Asian
20
Chinese
15
White
10
5
0
1997
1998
1999
2000
2001
2002
2003
2004
Year
(b)
140
Incidence Rate
120
South
Asian
100
80
Chinese
60
White
40
20
0
1997
1998
1999
2000
2001
2002
2003
2004
Year
FIGURE 2 Age-standardized incidence of diabetes for (a) diabetes on insulin only, and (b) Type 2 diabetes (incidence rates per 100 000).
Table 3 Medical specialty of care providers for people on insulin only
and people with Type 2 diabetes, categorized by age group
Age group
Care provider
519 years
Family practice
Paediatrics
Internal medicine,
endocrinology
Family practice
Internal medicine,
endocrinology
2029 years
Diabetes
on insulin
only (%)
Type 2
diabetes (%)
90.7
81.7
21.4
81.4
26.9
20.0
90.0
67.2
89.2
28.3
Chinese people had the lowest rates of Type 2 diabetes at
young ages. The incidence rates of Type 2 diabetes previously reported vary from 7.7 to 9.4 per 100 000 in South
Asian, Chinese or Asian Pacific Islander populations aged
019 years [24,25]. Our results extend the findings from
county-based, single-hospital studies and paediatrician surveys in the UK, Canada, USA and India that have shown
increased Type 2 diabetes rates in South Asians and
Asian-Pacific Islanders among those aged less than 20 years
[23,24,2628]. However, previous studies combined South
Asian and East Asian populations, likely attenuating the
effect of South Asian ethnicity on diabetes incidence. For the
first time, we are able to demonstrate the comparatively
increased incidence of early-onset Type 2 diabetes specifically in South Asians.
For people with diabetes on insulin only, incidence appears
to be higher among White people across all age groups. This
elevated incidence rate in White people (26.64 in the 5
19 years age group) is consistent with other paediatric studies
(24.427.4 in those aged less than 20 years) [25,29]. Among
Chinese people, observed diabetes incidence among those
using insulin only was 4.7 in those aged 519 years, and this
is comparable with Type 1 diabetes rates reported in China of
up to 4.6 in children under age 15 years [30]. The observed
incidence of diabetes for South Asian people using insulin
only was 16.77 among those under age 15 years. Although
accurate population-level incidence data on Type 1 diabetes
incidence in South Asian countries are lacking, a small UK
county-based study reported a similar incidence rate of 14.7
among South Asian people under age 15 years [31]. Genetic
haplotypes conferring a greater predisposition to developing
Type 1 diabetes are less common in Asian populations,
potentially explaining lower Type 1 diabetes rates among
Asians [32].
2014 The Authors.
Diabetic Medicine 2014 Diabetes UK
DIABETICMedicine
0.24 [0.05, 0.69]
P = 0.03
0.21 [0.02, 0.76]
P = 0.06
0.99 [0.83, 1.18]
P = 0.92
0.42 [0.31, 0.56]
P < 0.0001
0.24 [0.03, 0.91]
P = 0.10
0.44 [0.05, 1.65]
P = 0.33
1.05 [0.87, 1.26]
P = 0.63
0.47 [0.34, 0.64]
P < 0.0001
1.47]
1.86]
1.75]
2.91]
3.47]
3.79]
0.81 [0.33,
P = 0.59
0.77 [0.26,
P = 0.59
1.28 [0.84,
P = 0.23
0.89 [0.49,
P = 0.68
2014 The Authors.
Diabetic Medicine 2014 Diabetes UK
DKA, diabetic ketoacidosis; HHS, hyperglycaemic hyperosmolar state.
1.37]
1.4]
Any
hospitalization
0.78 [0.28,
P = 0.60
0.60 [0.14,
P = 0.34
0.82 [0.43,
P = 0.51
0.73 [0.34,
P = 0.38
South Asian
vs. White
Chinese
vs. White
South Asian
vs. White
Chinese
vs. White
Diabetes-related
complications
(DKA or HHS)
1.52]
0.57 [0.03,
P = 0.58
0.80 [0.05,
P = 0.83
2.10 [1.18,
P = 0.007
1.35 [0.50,
P = 0.50
Age 519
Ethnicity
Outcome
1.74]
Age 2029
2.67]
Total
1.64]
0.35 [0.04, 1.36]
P = 0.24
0.16 [0.001, 1.17]
P = 0.21
0.65 [0.34, 1.13]
P = 0.15
0.25 [0.11, 0.50]
P = 0.0004
Total
Age 2029
Age 519
Type 2 diabetes
Diabetes on insulin only
Table 4 Hazard ratios for hospitalization outcomes for South Asian and Chinese compared with White populations, adjusted using Cox proportional hazards models with bias correction [95% CI]
Research article
The reason for this substantial ethnic difference in the
development of early-onset Type 2 diabetes is likely multifactorial. Significant environmental influences may include
rapid transitions to high-fat, high-carbohydrate diets;
inadequate maternal nutrition; and decreased physical
activity among South Asian youth [33,34]. Some have
suggested in utero effects given that South Asian newborns
have increased cord leptin and insulin levels that are
associated with increased diabetes. By infancy, South
Asians are observed to have a thinfat phenotype characterized by thin muscles, central obesity and decreased
synthesis of adiponectin [35]. This biochemical change
increases insulin resistance, Type 2 diabetes, metabolic
syndrome and polycystic ovarian syndrome. Consequently,
South Asian children have significantly higher levels of
obesity, insulin and inflammatory markers compared with
White children [36]. Evidence is emerging that Indian
populations have variants of the ADIPOQ gene associated
with altered adiponectin synthesis and increased Type 2
diabetes susceptibility [37].
This study found that more than half of all people with
Type 2 diabetes across all ethnic groups were managed with
no medication. This proportion is greater than findings from
a diabetes registry in Manitoba, Canada reporting that
36.4% of youth were left untreated, although a substantially
higher Aboriginal population in Manitoba may have altered
prescribing patterns in that Province [10]. Our findings are
highly concerning given that Type 2 diabetes in young
people was shown to have increased risk of complications
[39]. Although lifestyle therapy has been recommended by
major guidelines as first-line therapy in children with Type 2
diabetes [6,40], pharmacological therapy has been less
clearly defined due to the relative lack of studies in this
population. Emerging evidence suggests that lifestyle therapy may have limited efficacy, and that the majority of
young people with Type 2 diabetes would require insulin
within a few years from time of diagnosis [41]. Given the
findings of our study, efforts are required to understand and
address the apparent lack of pharmacological management
of diabetes in British Columbia. Moreover, there needs to be
a significant impetus to promote more aggressive pharmacological therapy in young people with diabetes, especially
among family physicians who care for the majority of these
people. Further studies are also important to examine the
use of pharmacological agents for treating diabetes in the
young, considering that oral hypoglycaemic agents still lack
regulatory approval for use in children and adolescents [6,
40].
Our results also showed that hospitalization among those
with newly diagnosed DM was low in all ethnic groups and
lowest in Chinese people with Type 2 diabetes. This finding
is in keeping with similar studies in the adult population [13].
Evidence suggests that diabetes self-management behaviours
and outcomes are predicted by psychosocial mediators such
as social support and education [42]. We speculate that
DIABETICMedicine
Chinese people may have enhanced diabetes self-management abilities considering the contribution of strong familial
social networks and higher than average education levels [9].
The results of the present study generate several important
contributions in regard to diabetes screening and determining
population estimates of Type 2 diabetes. Currently, international guidelines suggest initiating screening for Type 2
diabetes for people with high-risk characteristics at ages less
than 40 years, including being of Asian descent [57].
Although Chinese and South Asian people are often inappropriately grouped together in this category, our data
support consideration for much earlier population screening
for people of South Asian ethnicity and not those of Chinese
descent. Our findings also suggest that significantly lower age
thresholds need to be considered for Type 2 diabetes.
Notably, the latest WHO world estimates of Type 2 diabetes
rates largely consider adult populations beginning at age
25 years and as such, likely underestimate the true global
burden of Type 2 diabetes [43] Although Type 2 diabetes
rates in youth are still less than those of people aged 30 years
and older [43], half of the worlds population is aged
29 years or below. Estimates of Type 2 diabetes are considerably higher in younger people than previously reported
especially in South Asian populations that also have a
disproportionately young population structure.
Limitations
This study was a large population-based study of diagnosed
diabetes incidence in a multiethnic population with extensive
information on diabetes medication prescribing and validated measures of diabetes. However, there are several
limitations to note. With administrative data, we were
unable to measure levels of Cpeptide, anti-GAD antibodies
and HbA1c to confirm Type 1 diabetes diagnoses among the
people using insulin only. Further studies with biochemical
characterization would be necessary to confirm these diagnoses. We were also unable to characterize clinical signs of
insulin resistance such as acanthosis nigricans in people with
Type 2 diabetes. Accordingly, we were not able to verify
diagnoses of polycystic ovarian syndrome. Prevalence of
polycystic ovarian syndrome may have been significantly
higher than observed in this study due to underdiagnosis
among primary care providers [44]. Because some people
with Type 2 diabetes may be treated with insulin only, our
rates of Type 2 diabetes are likely conservative. For people
up to age 18 years, prescription for insulin only has an
excellent sensitivity of 96.8% [10,11]. Based on this statistic,
sensitivity analysis confirms that our results would not have
differed substantially. Another limitation is that we were not
able to exclude people with other forms of diabetes, such as
steroid-induced diabetes and monogenic diabetes. However,
our validated methodology has previously been shown to
have an excellent specificity for identifying diabetes (93.5
99.9%) [2,1012]. Considering the very low prevalence of
Diabetes in the young: a population-based study ! C. Ke et al.
other forms of diabetes [24] (i.e. 0.20.4 cases per 100 000),
our results are unlikely to be different. The surname
algorithms we used to identify ethnicity were reasonably
accurate, but this methodology did not allow us to capture
data such as place of birth or age at immigration to Canada.
Our analysis was therefore unable to distinguish new
immigrants from later-generation Canadians of Asian
descent.
Conclusion
This study found disturbingly high rates of Type 2 diabetes
at ages 529 years in South Asian people and considerably
higher than previously reported. These data argue for a
significant reduction in the screening age for Type 2 diabetes
in South Asian people. Future international diabetes guidelines should incorporate data from such studies to recommend screening South Asians at a much younger age. The
occurrence of Type 2 diabetes in people under age 20 years
may be drastically higher than previously recognized, and
global population estimates for Type 2 diabetes should
consider including younger people given the global population structure. Interventions required to prevent the onset of
Type 2 diabetes will also likely need to occur in childhood
and adolescence to address the diabetes epidemic in this
population. Further research is required to determine why
South Asian people have such a proclivity to develop diabetes
at very young ages, why other immigrant groups (i.e.
Chinese) have much lower rates of developing Type 2
diabetes and why White youth have higher rates of diabetes
using insulin only.
Funding sources
This study was funded by the Canadian Institutes of Health
Research (CIHR). The study sponsors had no role in the
design and conduct of the study; collection, management,
analysis, and interpretation of the data; and preparation,
review, or approval of the manuscript. NAK is funded by a
Michael Smith Foundation for Health Research Career
Scientist award. HQ receives salary support from the Alberta
Heritage Foundation for Medical Research Senior Population Investigator award. This study was funded by the
Canadian Institutes for Health Research. We thank the
Ministry of Health for British Columbia for providing access
to the research data.
Competing interests
There are no potential conflicts of interest involving the work
under consideration for publication (during the time involving the work, from initial conception and planning to
present), no relevant financial activities outside the submitted
work (over the 3 years prior to submission), and no other
relationships or activities that readers could perceive to have
2014 The Authors.
Diabetic Medicine 2014 Diabetes UK
Research article
influenced, or that give the appearance of potentially
influencing what is written in the submitted work (based
on all relationships that were present during the 3 years prior
to submission) for any of the co-authors.
References
1 Pinhas-Hamiel O, Zeitler P. The global spread of type 2
diabetes mellitus in children and adolescents. J Pediatr 2005; 146:
693700.
2 Lipscombe LL, Hux JE. Trends in diabetes prevalence, incidence,
and mortality in Ontario, Canada 19952005: a population-based
study. The Lancet 2007; 369: 750756.
3 Population Division of the Department of Economic and Social
Affairs of the United Nations Secretariat. World Population
Prospects: The 2012 Revision. New York: United Nations Population Division, 2012. Available at http://esa.un.org/unpd/wpp/
index.htm Last accessed 19 June 2013.
4 International Diabetes Federation. IDF Diabetes Atlas. International Diabetes Atlas, 2012. Available at http://www.idf.org/
diabetesatlas/5e/ Last accessed 19 June 2013.
5 American Diabetes Association. Standards of medical care in
diabetes2013. Diabetes Care 2012; 36(Suppl 1): S11S66.
6 Canadian Diabetes Association Clinical Practice Guidelines Expert
Committee . Canadian Diabetes Association 2013 clinical practice
guidelines for the prevention and management of diabetes in
Canada. Can J Diabetes 2013; 37(Suppl 1): S1S212.
7 Chatterton H, Younger T, Fischer A, Khunti K. Risk identification
and interventions to prevent type 2 diabetes in adults at high risk:
summary of NICE guidance. BMJ 2012; 345: e4624.
8 Lindsay C. The South Asian Community in Canada. Ottawa: Social
and Aboriginal Statistics Division, Statistics Canada, 2001. Report
No: 89-621-XIE. Available at http://www.statcan.gc.ca/pub/
89-621-x/89-621-x2007006-eng.htm#4 Last accessed 19 June 2013.
9 Lindsay C. The Chinese Community in Canada. Ottawa: Social and
Aboriginal Statistics Division, Statistics Canada, 2001. Report No.:
89-621-XIE. Available at http://www.statcan.gc.ca/pub/89-621-x/
89-621-x2006001-eng.htm Last accessed 19 June 2013.
10 Dart AB, Martens PJ, Sellers EA, Brownell MD, Rigatto C, Dean
HJ. Validation of a pediatric diabetes case definition using
administrative health data in Manitoba. Canada. Diabetes Care
2011; 34: 898903.
11 Guttmann A, Nakhla M, Henderson M, To T, Daneman D,
Cauch-Dudek K et al. Validation of a health administrative data
algorithm for assessing the epidemiology of diabetes in Canadian
children. Pediatr Diabetes 2010; 11: 122128.
12 Chen G, Khan N, Walker R, Quan H. Validating ICD coding
algorithms for diabetes mellitus from administrative data. Diabetes
Res Clin Pract 2010; 89: 189195.
13 Khan NA, Wang H, Anand S, Jin Y, Campbell NRC, Pilote L et al.
Ethnicity and sex affect diabetes incidence and outcomes. Diabetes
Care 2011; 34: 96101.
14 Quan H, Wang F, Schopflocher D, Norris C, Galbraith PD, Faris P
et al. Development and validation of a surname list to define
Chinese ethnicity. Med Care 2006; 44: 328333.
15 Computer Services, Bradford Council. Nam Penchan News. Bradford, UK: Bradford Council, 1998. Summer.
16 Cummins C, Winter H, Cheng KK, Maric R, Silcocks P, Varghese
C. An assessment of the Nam Pehchan computer program for the
identification of names of south Asian ethnic origin. J Public Health
Med 1999; 21: 401406.
17 Harding S, Dews H, Simpson SL. The potential to identify South
Asians using a computerised algorithm to classify names. Popul
Trends 1999; 97: 4649.
2014 The Authors.
Diabetic Medicine 2014 Diabetes UK
DIABETICMedicine
18 Milan A, Maheux H, Chui T. A portrait of couples in mixed
unions. Can Soc Trends 2010 April 20; 89. Available at http://
www.statcan.gc.ca/pub/11-008-x/2010001/article/111
43-eng.htm Last accessed 9 May 2013.
19 Government of Canada SC. Tables by subject: Ethnic diversity and
immigration. Available at http://www.statcan.gc.ca/tables-tableaux/
sum-som/l01/ind01/l2_30000-eng.htm Last accessed 27 February
2013.
20 Monami M, Lambertucci L, Lamanna C, Lotti E, Marsili A,
Masotti G et al. Are comorbidity indices useful in predicting
all-cause mortality in Type 2 diabetic patients? Comparison
between Charlson index and disease count. Aging Clin Exp Res
2007; 19: 492496.
21 Fay MP, Feuer EJ. Confidence intervals for directly standardized
rates: a method based on the gamma distribution. Stat Med 1997;
16: 791801.
22 Heinze G, Schemper M. A solution to the problem of monotone
likelihood in Cox regression. Biometrics 2001; 57: 114119.
23 Haines L, Wan KC, Lynn R, Barrett TG, Shield JPH. Rising
incidence of type 2 diabetes in children in the U.K. Diabetes Care
2007; 30: 10971101.
24 Amed S, Dean HJ, Panagiotopoulos C, Sellers EAC, Hadjiyannakis
S, Laubscher TA et al. Type 2 diabetes, medication-induced
diabetes, and monogenic diabetes in Canadian children: a
prospective national surveillance study. Diabetes Care 2010; 33:
786791.
25 Dabelea D, Bell RA, DAgostino RB Jr, Imperatore G, Johansen
JM, Linder B et al. Incidence of diabetes in youth in the United
States. JAMA 2007; 297: 27162724.
26 Ehtisham S, Hattersley A, Dunger D, Barrett T. First UK survey of
paediatric type 2 diabetes and MODY. Arch Dis Child 2004; 89:
526529.
27 Amutha A, Datta M, Unnikrishnan IR, Anjana RM, Rema M,
Narayan KMV et al. Clinical profile of diabetes in the young seen
between 1992 and 2009 at a specialist diabetes centre in south
India. Prim Care Diabetes 2011; 5: 223229.
28 Amutha A, Datta M, Unnikrishnan R, Anjana RM, Mohan V.
Clinical profile and complications of childhood- and adolescent-onset type 2 diabetes seen at a diabetes center in south India.
Diabetes Technol Ther 2012; 14: 497504.
29 Lawrence JM, Imperatore G, Dabelea D, Mayer-Davis EJ, Linder
B, Saydah S et al. Trends in incidence of Type 1 diabetes among
non-Hispanic White youth in the United States 20022009,
Diabetes 2014; DB_131891.
30 World Health Organization DIAMOND Project Group. Incidence
and trends of childhood Type 1 diabetes worldwide 19901999.
Diabet Med J Br Diabet Assoc 2006; 23: 857866.
31 Harron KL, McKinney PA, Feltbower RG, Bodansky HJ, Norman
PD, Campbell FM et al. Incidence rate trends in childhood type 1
diabetes in Yorkshire, UK 19782007: effects of deprivation and
age at diagnosis in the South Asian and non-South Asian populations. Diabet Med J Br Diabet Assoc 2011; 28: 15081513.
32 Park Y. Why is type 1 diabetes uncommon in Asia? Ann NY Acad
Sci 2006; 1079: 3140.
33 Holmboe-Ottesen G, Wandel M. Changes in dietary habits after
migration and consequences for health: a focus on South Asians in
Europe. Food Nutr Res 2012; 56: 10.3402/fnr.v56i0.18891.
doi:10.3402/fnr.v56i0.18891. Available at http://www.ncbi.nlm.
nih.gov/pmc/articles/PMC3492807/ Last accessed 12 July 2013.
34 Yajnik CS, Lubree HG, Rege SS, Naik SS, Deshpande JA,
Deshpande SS et al. Adiposity and hyperinsulinemia in
Indians are present at birth. J Clin Endocrinol Metab 2002; 87:
55755580.
35 Mente A, Razak F, Blankenberg S, Vuksan V, Davis AD, Miller R
et al. Ethnic variation in adiponectin and leptin levels and their
DIABETICMedicine
36
37
38
39
10
association with adiposity and insulin resistance. Diabetes Care
2010; 33: 16291634.
Nightingale CM, Rudnicka AR, Owen CG, Cook DG, Whincup
PH. Patterns of body size and adiposity among UK children of
South Asian, black African-Caribbean and white European origin:
Child Heart and Health Study in England (CHASE Study). Int J
Epidemiol 2011; 40: 3344.
Saxena M, Srivastava N, Banerjee M. Genetic association of
adiponectin gene polymorphisms (+45T/G and +10211T/G) with
type 2 diabetes in North Indians. Diabetes Metab Syndr Clin Res
Rev 2012; 6: 6569.
Mohan S, Chen G, Campbell NR, Hemmelgarn BR. Regional
variations in not treating diagnosed hypertension in Canada. Can J
Cardiol 2010; 26: 409413.
Wong J, Molyneaux L, Constantino M, Twigg SM, Yue DK.
Timing is everything: age of onset influences long-term retinopathy
risk in type 2 diabetes, independent of traditional risk factors.
Diabetes Care 2008; 31: 19851990.
Diabetes in the young: a population-based study ! C. Ke et al.
40 American Diabetes Association. Standards of medical care in
diabetes2014. Diabetes Care 2013; 37(Suppl 1): S14S80.
41 TODAY Study Group, Zeitler P, Hirst K, Pyle L, Linder B,
Copeland K et al. A clinical trial to maintain glycemic control in
youth with type 2 diabetes. N Engl J Med 2012; 366: 22472256.
42 Brown AF, Ettner SL, Piette J, Weinberger M, Gregg E, Shapiro MF
et al. Socioeconomic position and health among persons with
diabetes mellitus: a conceptual framework and review of the
literature. Epidemiol Rev 2004; 26: 6377.
43 Danaei G, Finucane MM, Lu Y, Singh GM, Cowan MJ, Paciorek
CJ et al. National, regional, and global trends in fasting plasma
glucose and diabetes prevalence since 1980: systematic analysis of
health examination surveys and epidemiological studies with 370
country-years and 2.7 million participants. The Lancet 2011; 378:
3140.
44 Fingert SB, Shah B, Kessler M, Pawelczak M, David R. Evaluation
of adolescents for polycystic ovary syndrome in an urban population. J Clin Res Pediatr Endocrinol 2009; 1: 188193.
2014 The Authors.
Diabetic Medicine 2014 Diabetes UK
You might also like
- B.C. Public Safety Minister Mike Farnworth Letter To Surrey Re: Police Information Sharing (June 13, 2023)Document2 pagesB.C. Public Safety Minister Mike Farnworth Letter To Surrey Re: Police Information Sharing (June 13, 2023)The Vancouver SunNo ratings yet
- B.C. Emergency Health Services: External ReviewDocument37 pagesB.C. Emergency Health Services: External ReviewThe Vancouver SunNo ratings yet
- B.C. Emergency Health Services: External ReviewDocument37 pagesB.C. Emergency Health Services: External ReviewThe Vancouver SunNo ratings yet
- Rising To The Challenge Full ReportDocument92 pagesRising To The Challenge Full ReportThe Vancouver SunNo ratings yet
- Special Committee On Reforming The Police ActDocument96 pagesSpecial Committee On Reforming The Police ActChristopherFouldsNo ratings yet
- Vancouver International Wine Festival ChecklistDocument1 pageVancouver International Wine Festival ChecklistThe Vancouver Sun100% (1)
- Letter From B.C. Public Safety Minister Mike FarnworthDocument3 pagesLetter From B.C. Public Safety Minister Mike FarnworthThe Vancouver SunNo ratings yet
- 26 E Hastings - The Only - Structural Safety Assessment ReportDocument15 pages26 E Hastings - The Only - Structural Safety Assessment ReportThe Vancouver SunNo ratings yet
- Vancouver Sun - 2020 Mammoth Crossword ANSWERSDocument1 pageVancouver Sun - 2020 Mammoth Crossword ANSWERSThe Vancouver SunNo ratings yet
- 01/25/2021 - Ernst & Young BC LTC COVID-19 Response ReviewDocument28 pages01/25/2021 - Ernst & Young BC LTC COVID-19 Response ReviewThe Vancouver SunNo ratings yet
- Feb 25 2021 - Postmedia / Leger StudyDocument20 pagesFeb 25 2021 - Postmedia / Leger StudyThe Vancouver SunNo ratings yet
- 01/21/2021 - Rod and Ekaterina BakerDocument3 pages01/21/2021 - Rod and Ekaterina BakerThe Vancouver SunNo ratings yet
- 01/28/2021 - Leger BC Survey On COVID-19 Rule BreakingDocument30 pages01/28/2021 - Leger BC Survey On COVID-19 Rule BreakingThe Vancouver SunNo ratings yet
- Letter From Superintendent To NVSD CommunityDocument1 pageLetter From Superintendent To NVSD CommunityThe Vancouver SunNo ratings yet
- Vancouver Sun - 2020 Mammoth CrosswordDocument1 pageVancouver Sun - 2020 Mammoth CrosswordThe Vancouver SunNo ratings yet
- Nov. 23, 2020 - Maxwell Johnson - 911 Transcript REDACTEDDocument7 pagesNov. 23, 2020 - Maxwell Johnson - 911 Transcript REDACTEDThe Vancouver Sun100% (1)
- NHL Phased Return To Sport Protocol-COMBINED-FINALDocument22 pagesNHL Phased Return To Sport Protocol-COMBINED-FINALThe Vancouver SunNo ratings yet
- Vancouver COVID-19 Impacts Report Economy + RestartDocument18 pagesVancouver COVID-19 Impacts Report Economy + RestartThe Vancouver SunNo ratings yet
- TransLink Releases Results of Burnaby Mountain Gondola EngagementDocument80 pagesTransLink Releases Results of Burnaby Mountain Gondola EngagementThe Vancouver SunNo ratings yet
- Liquor Consumption in Parks By-Law & Pilot ProgramDocument27 pagesLiquor Consumption in Parks By-Law & Pilot ProgramThe Vancouver SunNo ratings yet
- Go Forward Tech BriefingDocument36 pagesGo Forward Tech BriefingThe Vancouver Sun100% (2)
- Vancouver Park Board Liquor Consumption Parks Bylaw Pilot ProgramDocument15 pagesVancouver Park Board Liquor Consumption Parks Bylaw Pilot ProgramThe Vancouver SunNo ratings yet
- July 2020. Open Letter Ban On Street Checks.Document10 pagesJuly 2020. Open Letter Ban On Street Checks.The Vancouver SunNo ratings yet
- VPD Police ReportDocument11 pagesVPD Police ReportThe Vancouver SunNo ratings yet
- RCMP - Valerie Little.Document31 pagesRCMP - Valerie Little.The Vancouver SunNo ratings yet
- City of Vancouver: Mobility and Public Life ResponseDocument60 pagesCity of Vancouver: Mobility and Public Life ResponseThe Vancouver SunNo ratings yet
- Kids & COVID-19: Canadian Children Are Done With School From Home, Fear Falling Behind, and Miss Their FriendsDocument11 pagesKids & COVID-19: Canadian Children Are Done With School From Home, Fear Falling Behind, and Miss Their FriendsThe Vancouver SunNo ratings yet
- BC Hydro Report: COVID19 Demand DilemmaDocument6 pagesBC Hydro Report: COVID19 Demand DilemmaThe Vancouver SunNo ratings yet
- Leger National Weekly Pandemic Tracker June 22nd 2020Document63 pagesLeger National Weekly Pandemic Tracker June 22nd 2020The Vancouver SunNo ratings yet
- National Sick-Day LetterDocument3 pagesNational Sick-Day LetterThe Vancouver SunNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5784)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Bianchi Size Chart for Mountain BikesDocument1 pageBianchi Size Chart for Mountain BikesSyafiq IshakNo ratings yet
- Detailed Lesson PlanDocument5 pagesDetailed Lesson PlanHazel Mae HerreraNo ratings yet
- February / March 2010Document16 pagesFebruary / March 2010Instrulife OostkampNo ratings yet
- Communication Tourism PDFDocument2 pagesCommunication Tourism PDFShane0% (1)
- Business Law Module No. 2Document10 pagesBusiness Law Module No. 2Yolly DiazNo ratings yet
- Belonging Through A Psychoanalytic LensDocument237 pagesBelonging Through A Psychoanalytic LensFelicity Spyder100% (1)
- (Class 8) MicroorganismsDocument3 pages(Class 8) MicroorganismsSnigdha GoelNo ratings yet
- Sangam ReportDocument37 pagesSangam ReportSagar ShriNo ratings yet
- Consumer Behavior Paper PLDTDocument6 pagesConsumer Behavior Paper PLDTAngeline Santiago100% (2)
- McLeod Architecture or RevolutionDocument17 pagesMcLeod Architecture or RevolutionBen Tucker100% (1)
- The Awesome Life Force 1984Document8 pagesThe Awesome Life Force 1984Roman PetersonNo ratings yet
- Ultramat 2 instructions for useDocument2 pagesUltramat 2 instructions for useBalaji BalasubramanianNo ratings yet
- RumpelstiltskinDocument7 pagesRumpelstiltskinAndreia PintoNo ratings yet
- Introduction To Computing (COMP-01102) Telecom 1 Semester: Lab Experiment No.05Document7 pagesIntroduction To Computing (COMP-01102) Telecom 1 Semester: Lab Experiment No.05ASISNo ratings yet
- BCIC General Holiday List 2011Document4 pagesBCIC General Holiday List 2011Srikanth DLNo ratings yet
- TITLE 28 United States Code Sec. 3002Document77 pagesTITLE 28 United States Code Sec. 3002Vincent J. Cataldi91% (11)
- R19 MPMC Lab Manual SVEC-Revanth-III-IIDocument135 pagesR19 MPMC Lab Manual SVEC-Revanth-III-IIDarshan BysaniNo ratings yet
- The Insanity DefenseDocument3 pagesThe Insanity DefenseDr. Celeste Fabrie100% (2)
- Bpoc Creation Ex-OrderDocument4 pagesBpoc Creation Ex-OrderGalileo Tampus Roma Jr.100% (7)
- Irony in Language and ThoughtDocument2 pagesIrony in Language and Thoughtsilviapoli2No ratings yet
- Preparation For Exercise1-1 CompleteDocument28 pagesPreparation For Exercise1-1 CompleteSimon GranNo ratings yet
- CP ON PUD (1) ADocument20 pagesCP ON PUD (1) ADeekshitha DanthuluriNo ratings yet
- Training Effectiveness ISO 9001Document50 pagesTraining Effectiveness ISO 9001jaiswalsk1No ratings yet
- Obtaining Workplace InformationDocument4 pagesObtaining Workplace InformationJessica CarismaNo ratings yet
- EAPP Q2 Module 2Document24 pagesEAPP Q2 Module 2archiviansfilesNo ratings yet
- Surah 25. Al-Furqan, Ayat 63-69 PDFDocument1 pageSurah 25. Al-Furqan, Ayat 63-69 PDFMusaab MustaphaNo ratings yet
- Skin Yale University Protein: Where Does Collagen Come From?Document2 pagesSkin Yale University Protein: Where Does Collagen Come From?Ellaine Pearl AlmillaNo ratings yet
- MC-SUZUKI@LS 650 (F) (P) @G J K L M R@601-750cc@175Document103 pagesMC-SUZUKI@LS 650 (F) (P) @G J K L M R@601-750cc@175Lanz Silva100% (1)
- Classification of Boreal Forest Ecosystem Goods and Services in FinlandDocument197 pagesClassification of Boreal Forest Ecosystem Goods and Services in FinlandSivamani SelvarajuNo ratings yet
- EE-LEC-6 - Air PollutionDocument52 pagesEE-LEC-6 - Air PollutionVijendraNo ratings yet