Professional Documents
Culture Documents
Medicine 1 Final Practical Exam Reviewer
Uploaded by
TP RMadCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Medicine 1 Final Practical Exam Reviewer
Uploaded by
TP RMadCopyright:
Available Formats
MEDICINE
1: FINAL PRACTICAL EXAMINATION
REMEMBER:
SEATED
GENERAL SURVEY, VS, SKIN, HEENT, NECK,
PULMO
Patient sitting, examiner in front
Patient sitting, chest exposed, examiner goes in
front then back
SUPINE
CARDIO, GIT, GUT
Patient supine, chest exposed, examiner at right
side of patient
Patient at 30 or 45 degree angle, chest exposed,
examiner at right side
Patient supine, abdomen exposed, examiner at
right
STANDING
NEURO, MUSCULO
Patient standing, examiner in front, then at the side
of the patient
Always state your findings
Height and weight of the patient will be provided to
you
Bring a calculator for BMI calculation
Prepare your materials before starting examination
PREPARATION:
Wash hands before and after the examination
Introduce self to patient
Explains what will be done to the patient
Ask if the patient would like to use the restroom
Ensure privacy and patients comfort throughout the
examination
Ensure adequate lighting and exposure
Materials are complete and prepared beforehand
No borrowing of instruments except for diagnostic
set
Examiner speaks in professional manner
No jargon or inappropriate language
A. GENERAL SURVEY
State of health
Well, acutely ill, chronically ill
Level of consciousness
Conscious, sedated, drowsy
I
Confusion
Inappropriate response to a question
Decreased attention span and memory
II Lethargy
Drowsy, falls asleep quickly
Once aroused, responds appropriately
III Delirium
Confusion with disordered perceptions and
decreased attention span
Marked anxiety with motor and sensory
excitement
Inappropriate reactions to stimuli
IV Stupor
Arousable for short period to verbal,
painful stimuli
Simple motor and moaning responses
Slow responses
V Coma
Neither awake nor aware
Decerebrate posturing to painful stimuli
Eye opening
4
Spontaneous
3
To speech or verbal stimuli
2
To pain
1
None or no response
Best verbal
5
Oriented to appropriate stimuli
response
4
Confused speech
3
Inappropriate words
2
Incomprehensible (incoherent)
1
None
Motor response
6
Obeys commands
(of unaffected limb) 5
Localizes painful stimuli
4
Withdrawn from pain
3
Arm flexion to painful stimuli
2
Arm extension to painful stimuli
1
None
Glasgow coma scale
Habitus
Hyposthenic
Ectomorphic
Sthenic
Mesomorphic
Hypersthenic
Endomorphic
Tall, thin, long neck
Poor muscle dvlpt.
Small bone structure
Appears malnourished
Ultrafast metabolism
Athletic type
Broad shoulders
Great muscle dvlpt.
Large bone structure
Low body fat %
Fast metabolism
Short, stocky
Thick and short neck
Good muscle dvlpt.
Obesity tendencies
Comfort
State if patient is comfortable or in RESPIRATORY
DISTRESS
Abdominal paradox
Central cyanosis
Altered sensorium
Prefers upright or tripod position
Prominent SCM
Retractions
Speaks in phrases
Ambulatory status
Ambulatory
With assistance
Wheel-chair
Stretcher
Bedridden
Mood
Attitude towards the examiner
Cooperative
Guarded
Suspicious
Evasive
Hostile
Seductive
Predominant
mood
Neutral
Anxious
Fearful
Elated
Euphoric
Angry
Depressed
Irritable
Affect
Broad
Restricted
Labile
Intensity
(blunted,
flat,
animated)
Appropriateness
Facies
B.
MENTAL
STATUS
Attention/calculation
Remember 3 words or simple math question
Time: Do you know the current date?
Place: Do you know the name of this hospital?
Person: State full name / birthday.
MEDICINE 1: FINAL PRACTICAL EXAMINATION
C. VITAL SIGNS
Patient needs to be resting for 5 minutes
Ask for intake of caffeinated drinks, smoking, alcohol,
antihypertensive meds, NSAIDs, steroids.
Note time and amount of last intake
Patient is instructed to avoid smoking, drinking for
30 minutes before BP is taken
Reminders:
Patients arm at rest so that the brachial artery is at
heart level (approx. 4th ICS)
If supine, position patient at 30-45 angle
If standing, support the arm at mid chest level
If seated, rest arm on a table a little above the
patients waist
Stay on the RIGHT SIDE of the patient in taking the
blood pressure on the right upper extremity (left
side for left upper extremity)
Use index fingers to palpate for the patients
brachial and radial arteries
Use the proper width of the inflatable bladder
40% or 12-14cm of the upper arm
circumference
Length should be 80% of the upper arm
circumference, along long enough to encircle
the arm
Apply the cuff 2.5 cm above the antecubital fossa
Ensure that the center of the inflatable bladder of
the BP cuff is over the brachial artery
Wrap the cuff snugly
Be able to insert only one finger underneath
the cuff
Measure palpatory BP correctly
Use index and middle fingers to palpate the radial
artery
With the other hand, rapidly inflate cuff while
palpating radial artery pulse
Note when the pulse disappears
State palpatory (SYSTOLIC) BP
Deflate cuff
Measure auscultatory BP correctly
Wait 15-30 seconds after getting the palpatory BP
Palpate for the brachial artery again using index
and middle fingers
Apply the BELL of the stethoscope over the
brachial artery
Inflate BP cuff rapidly 30 mmHg ABOVE the
palpatory (SYSTOLIC) BP
Slowly deflate BP cuff by 2-3 mmHg/sec
First Korotkoff sound = auscultatory (SYSTOLIC)
BP (N.V. 120)
When the Korotkoff sound disappears = DIASTOLIC
BP (N.V. 80)
If elevated measure BP, on other arm and leg
Adult BP classification (ages 18 and older)
Classification
Systolic
Diastolic
(mmHg)
(mmHg)
Normal
<120
<80
Pre-
120-139
80-89
hypertensive
Stage 1
140-159
90-99
Stage 2
>160
>100
Palpate for the patients radial pulse
Use index and middle fingers to palpate for the
patients radial pulse
Count the pulse rate for ONE FULL MINUTE
Note the pattern (rhythm)
Regular, irregular, irregularly irregular
Note the volume
N.V. 60-100 bpm regular +2
No pulse
Absent, not palpable
(-)
Weak pulse
Diminished, barely
(+)
palbable
Normal pulse
Expected
(++)
Strong pulse
Full, increased
(+++)
Very strong
Bounding,
(++++)
pulse
aneurysmal
Pulsus
- Alternation of pulsation
Left ventricular
alternans
of small amplitude with
failure
the pulsation of large
amplitude
(more significant if
- Rhythm is regular
pulse is slow)
Pulsus
- Best detected by
Aortic stenosis
bisferiens
palpation of the carotid
combined with aortic
artery
insufficiency
- Characterized by two
main peaks
- The first is termed
percussion wave which is
believed to be the pulse
pressure and the second
is called the tidal wave
which is the reverberation
from the periphery
Bigeminal
- Result from a normal
Disorder of rhythm
pulse
pulsation followed by a
PVCs
premature contraction
- The amplitude of the
pulsation of the
premature contraction is
less than that of the
normal pulsation
Large,
- Also called hyperkinetic
Exercise
bounding
or strong pulse
Anxiety
pulse
- Readily palpable
Fever
- Does not fade out and
Hyperthyroidism
is not easily obliterated by Aortic rigidity
the examining fingers
Atherosclerosis
PDA
Pulsus
- Characterized by
Premature cardiac
paradoxus exaggerated decrease (>
contraction
10 mmHg) in the
Tracheobronchial
amplitude of pulsation
obstruction
during inspiration and
Bronchial asthma
increased amplitude
Emphysema
during expiration
Pericardial effusion
Constrictive
pericarditis
Water-
- Also known as collapsing Patent ductus
hammer /
pulse
arteriosus
Corrigan
- Has greater amplitude
Aortic regurgutation
pulse
than expected
- A rapid rise to a narrow
summit, and a sudden
descent
Labile
Increase amplitude in
Non-specific
pulse
sitting and standing
compared to supine
MEDICINE 1: FINAL PRACTICAL EXAMINATION
Determine
respiratory
rate
in
a
subtle
way
With the patient unaware, RR is determined in a
subtle way by pretending to continue counting
pulse rate and note the number of rise/fall (cycles)
of the chest for 1 full minute and pattern if any
N.V.
12-20
respirations/breaths
per
minute
The
ratio
of
respirations
to
heartbeats
is
1:4
Expansion
of
the
chest
should
be
bilaterally
symmetric
The
pattern
of
breathing
should
be
even,
neither
too
shallow
or
too
deep
Measure
BMI
BMI = Wt (kg) / Ht (m2)
<18.5
Underweight
18.5 24.9
Healthy
25 29.9
Overweight
>/= 30
Obese
30 34.9
Class 1 Obesity
35 39.9
Class 2 Obesity
>40
Class 3 Obesity
D.
SKIN
Prepare penlight and ruler
Color
Presence of discoloration, (table 8-3, p. 162)
Texture
Smooth, rough?
Moisture
Minimal perspiration, oiliness
Primary lesions (table 8-4, pp. 166-168)
Flat,
non-palpable
Macule:
<1cm
Patch:
>1cm
Just
epidermis,
superficial,
usually
just
discolorations
Elevated,
palpable
Papule:
<1cm
Plaque:
>1cm
Nodule:
>1cm,
deep
on
palpation,
big,
out
Tumor:
>
2cm,
big,
out/in,
deep
palpation
Fluid
filled
Vesicle:
<1cm
Bullae:
>1cm
Pustule:
purulent
material
inside
Secondary lesions (table 8-5, pp. 169-171)
Scales: laminated masses of keratin, dead skin,
corneum
Crust: dried serum, pus or blood mixed epithelial
debris and sometimes bacterial debris
Fissure: linear crack through epidermis or into
dermis
Erosion: loss of all or part of epidermis alone
Ulcer: loss of epidermis and some portion of
dermis, heal with scarring
Scars: connective tissue replaced lost substance in
dermis or deeper keloidal scars
Excoriation: loss of epidermis, linear hallowed-out
crusted area
Keloid: irregularly-shaped, elevated, progressively
enlarging scar, grows beyond the boundaries of the
wound: caused by excessive collagen formation
during healing
Lichenification: rough, thickened epidermis
secondary to persistent rubbing, itching or skin
irritation, involves flexor surface of extremities
Other
respiratory
patterns
Bradypnea
Slower
than
12
breaths
per
minute
Neurologic
or
electrolyte
disturbance,
infection,
response
to
point
of
pleurisy
or
irritative
phenomena,
meidcations,
deep
sleep
Tachypnea
Faster
than
12
breaths
per
minute
Heart
or
lung
disease,
pain
Hyperventilation
Faster
than
20
breaths
per
minute,
deep
Hyperpnea
breathing
Protective
splitting
from
a
broken
rib
or
pleurisy,
massive
liver
enlargement,
abdominal
ascites,
exercise,
anxiety,
CNS
and
metabolic
disease
Sighing
Frequently
interspersed
deeper
breath
Normal
if
occasional,
anxiety
if
frequent
Air
trapping
Increasing
difficulty
in
getting
breath
out
Hypopnea
Shallow
respirations
Cheyne-stokes
Varying
periods
of
increasing
depth
interspersed
with
apnea
Periodic
breathing,
sleep
in
kids
and
elderly,
seriously
ill,
brain
damage
at
cerebral
level,
durgs
Kussmaul
Rapid,
deep,
labored
Metabolic
acidosis
Biot
Irregularly
interspersed
periods
of
apnea
in
a
disorganized
sequence
of
breaths
Severe
&
increased
intracranial
pressure,
respiratory
compromise,
drug
poisoning,
brain
damage
at
the
level
of
medulla
Ataxic
Significant
disorganization
with
irregular
and
varying
depths
of
respiration
Stridor
Harsh,
high-pitched
inspiration
Danger:
airway
obstruction
Take the temperature
Remember
Rectal:
0.4C
>
oral
temperature
Tympanic
membrane:
0.8C
<
rectal
temperature
Axillary:
0.5C
<
oral
temperature
Ergo:
rectal
>
oral
>
axillary
>
tympanic
in
approximating
core
body
temperature
Mean oral temperature: 36.8C + or 0.4C
Normal circadian range: 36.5-37.5C
Normal daily temperature variation: 0.5C
AM: 37.2C
PM: 37.7C
Mild/low grade fever
38.1 39C
Moderate grade fever
39.1 to 40C
High grade fever
40.1 to 41.1C
Hyperpyrexia
>41.5C
Acute fever
<7 days
Subacute fever
>7 days to <2 weeks
Chronic/persistent fever
> 2 weeks
Press on the button, remove clothing from the
axilla, place the tip of the thermometer underneath
the axilla
Instruct patient to firmly appost the medial aspect
of the arm to the lateral surgace of the chest to
keep the thermometer in place
Wait for the alarm and read the temperature
MEDICINE 1: FINAL PRACTICAL EXAMINATION
E. HEENT
Inspect and palpate head and scalp systematically
Head position: tilted, tremor
Size, shape (molding), symmetry, lesions, trauma
Facial features
Associated disorders
Cushings syndrome
Moon-facies, thin erythematous skin,
buffalo hump
Hippocratic facies
Sunken appearance of the eyes, cheeks
(throat cancer)
and temporal areas, sharp nose and dry
rough skin
Myxedema facies
Dull, puffy, yellowed skin, coarse sparse
hair, temporal loss of eyebrows,
periorbital edema, prominent tongue
Hyperthyroid facies
Fine, moist skin, fine hair, prominent
eyes and lid retraction, staring or
startled expression
Systemic lupus
Butterfly-shaped rash over mala
erythematous
surfaces and bridge of the nose
Either a blush with swelling or scaly,
red, maculopapular lesions
Bells palsy
Left facial palsy, asymmetry of one side
of the eyelid not closing completely,
drooping lower eyelid and corner of
mouth, loss of nasolabial fold
Acromegaly
Coarsening of features with broadening
of nasal alae and prominence of the
zygomatic arches
In examining the scalp, systematically part the hair
from frontal to occipital region
Note any lesions, scabs, tenderness, parasites,
nits or scaliness
Pay special attention to the areas behind the
ears, the hairline and at the crown of the haid
Note any loss pattern
Palpate in a gentle rotary movement progressing
systematically from front to back
Inspect for position and alignment of
Eyebrows
Wrinkle
forehead,
raise
your
eyebrows
Loss,
odd
hair,
presence
of
seborrhea
Eyelids
Close
eyes
tightly:
fasiculations
or
tremors
OPEN
EYE:
superior
eyelid
should
cover
a
portion
of
the
iris
but
not
the
pupil
itself
The
average
upper
eyelid
position
is
2mm
below
the
limbus
The
average
lower
eyelid
position
is
at
the
lower
limbus
Note
whether
the
lids
evert
or
invert
Eyes
Symmetry,
size
and
shape
Inspect abnormalities of conjunctivae and sclera
Have the patient look upward while you draw the
lower lid downward
Using a penlight, inspect sclera and conjunctive of
lower eyeball for color, swelling and vascularity
Inspect the upper tarsal conjunctiva only when
there is a suggestion that a foreign body may be
present
Observe the conjunctiva for erythema or exudate
Eythematous / cobblestone: allergic infectious
conjuctivitis
Test for visual acuity (central vision)
Using Snellen chart or pocket card (CNII)
Test one eye at a time initially without correction
(sc) then with correction (cc)
Position patient 20 ft. from Snellen chart or ask
patient to hold pocket card 14 in. away
Instruct patient to cover one eye with card or palm
of the hand
Ask patient to read each line down to the smaller
characters
Record visual acuity as fraction
Check
conjugate
extra
ocular
movements
(CN
III,
IV,
VI)
Instruct patient to follow your index finger with
their eyes only and with the head remaining in one
position
Move your index finger slowly to the extreme
position of each of the 6 cardinal fields of gaze (H-
pattern)
Test
pupils
for
reactivity
to
light
Both directed and consensual as well as
accommodation (CN II, III)
Direct
reaction
Check
for
pupillary
constriction
in
the
eye
that
light
is
shined
into
Consensual
response
Dim
light
in
the
room
Instruct
patient
to
look
into
distance
and
not
to
focus
on
the
light
Shine
a
penlight
into
one
eye
from
a
point
slightly
lateral
to
the
patients
line
of
vision
Note
whether
the
pupil
constricts
Note
the
consensual
response
of
the
opposite
pupil
constricting
simultaneously
with
the
tested
pupil
Repeat
steps
for
the
other
eye
Accommodation
response
Instruct
patient
to
look
at
a
distant
object
and
then
at
the
test
object
(pencil
or
your
finger)
held
10
cm
from
bridge
of
patients
nose
and
check
for
pupillary
constriction
when
changing
focus
from
distance
object
to
test
object
Do
an
ophthalmic
examination
Darken the room
Set ophthalmoscope at correct setting
Use with ease and dexterity
Instruct patient to fix eye on specific point in the
distance and try not to move eyes
Use opthalmoscope in RIGHT HAND and look
through it with RIGHT EYE to examine PATIENTS
RIGHT EYE (if left hand, left eye, patients left eye)
Shine beam into eye from position approximately
12 inches from the patient and about 15 degrees
lateral to patients line of vision
Note orange glow in pupil, red reflex from retina
and opacities interrupting red reflex
Move closer to patients eye to examine retina,
optic disc, retinal vessels, peripheral retina and
macular area
Describe disc margin, cup/disk ratio, A:V ratio,
absence/presence of hemorrhages, exudates,
cotton wool, spots, copper wiring, AV nicking
MEDICINE 1: FINAL PRACTICAL EXAMINATION
Check
hearing
acuity
in
each
ear
Whisper test / watch ticking
Ask patient to occlude each ear one at a time with
his/her finger
Inspect and palpate external ear for deformities and
tenderness
Inspect and palpate auricle and surrounding
tissues for deformities, masses, skin lesions,
tenderness
Gasps top of pinna correctly to straighten canal
(upward and backwards)
Perform otoscopic exam properly
Inspect ear cannal with otoscope speculum for wax,
discharge, foreign bodies, redness and swelling
Inspect nose structure, nostril patency, septum position,
inflammation of nasal mucosa
Visually inspect/palpate nose for deformity,
symmetry, inflammation
Elevate tip of nose with the neck hyperextended
Bilaterally inspects nasal mucosa
Inspect nasal septum
Tilt patients head back slightly and inspect the
inferior and middle turbinates and nasal passage
Palpate for tenderness of the frontal, ethmoid and
maxillary sinuses
If tender, do trans-illumination
Apply digital pressure with the thumb and index
finger over the bony brow sides of the nasal bone
as well as the cheek bone to palpate for tenderness
Inspect mouth
Lips
Color,
symmetry,
inflammation
Gums, teeth, tongue, floor of the mouth and
posterior pharynx
Instruct patient to open mouth
With tongue blade and penlight, visually
inspect teeth, tongue, hard and soft palate,
gums, floor of the mouth and buccal mucosa
Ask patient to protrude tongue and inspect for
deviation and limitation of movement
Using gloves, wrap tongue with a piece of
gauze and gently pulls tongue to each side and
inspect its lateral borders
Check for lumps, nodules and ulcerations
Instruct patient to say ah and inspect
pharynx including soft palate, uvula
Note for deviation of uvula
Touch the posterior wall of the pharynx with a
tongue blade and elicit gag reflex
Neck
Instruct patient to relax, with neck flexed slightly
forward or to side being examined and inspect
neck for symmetry and masses
Examine for palpable lymph nodes at occipital, pre
and post auricular, submandibular, submental,
ant/post cervical and supraclavicular areas
Using pads of first two fingers, move skin over
underlying tissue in a rotary mtion
With patient swallowing, palpate thyroid tissue
correctly for size, symmetry, consistency
Ask patient to gently extend neck
Stand either in front or behind the patient
Bimanually palpate thryroid gland pushing
gently to the right with the first two fingers of
the LEFT HAND
Palpate RIGHT LOBE when the patient
swallows
Auscultate for bruit
Assess whether trachea is midline
Face the patient
Inspect the position of the trachea
Insert index fingers on the spaces on either
side of the trachea
Normal: spaces on either side of the trachea
are equal, trachea is midline
F.
THORAX,
LUNGS
Describe the configuration of anterior chest
Note for deformities of the chest
Symmetry
Chest
asymmetry:
unequal
expansion
and
respiratory
compromise
caused
by
collapsed
lung
or
limitation
of
expansion
by
extrapleural
air,
fluid
or
mass
Masses
Bulges
Unilateral
or
bilateral
bulging
can
be
a
reaction
of
the
ribs
and
interspaces
to
respiratory
obstruction
Scars
Lesions
Compare AP to lateral chest diameter
Normal: AP diameter is less than the lateral
diameter
Identify the sternal angle of Louis and count the spaces
anteriorly
Assess symmetry of lung expansion (inspection and
palpation)
Face the patient
Place thumb along costal margins and xiphoid
processes with palms resting on the anterior chest
Ask patient to take deep breath
Observe for movement of hands
Describe if anterior chest wall movement is
symmetrical or asymmetrical
Move towards back of patient
Locate inferior angle of scapula (7th ICS)
Palpate for the 10th ICS along midscapular line
Puts both palms flush against the chest wall along
the 10th ICS
Grasp the posterior chest and moves both hands
medically (towards the vertebral line) so as to form
a crease along the mid-back
Ask the patient to take a deep breath
Observe for movement of hand
Describe if posterior chest wall movement is
symmetrical or asymmetrical
Palpate for any tenderness in the chest wall and
perform tactile fremiti
Palpate gently across anterior and posterior chest
Describe if there are any points of tenderness,
bulges, masses
Ask patient to cross his arms across his chest
Move toward back of patient
Rest ulnar surface of hand in the upper posterior
chest, medial to the scapula
Ask patient to say ninety-nine or tres-tres
Feel for vibration in the area
Move to other side and do the same procedure
Move hand to the lower position and do the same
procedure
Always compare one side to the other while
moving from upper to mid chest area, initially
always medial to the scapula
Once below the level of T7 or 7th ICS, examine
tactile fremiti along the scapular lines and
posterior axillary lines, always comparing one side
to the other
Normal: tactile fremiti are equal
Percuss anterior lung fields
Remind patient to keep his arms crossed
Beginning at the upper lung field, align finger (of
pleximeter hand) along intercostal space along the
paravertebral line
Make sure it is only the distal 3rd of the finger
resting on the chest wall
Strike
the
distal
3rd
of
the
finger
with
the
tips
of
the
fingers
of
the
free
hand
(plexor)
Listen for percussion sound produced
Do same procedure from upper to the lower lung
fields
MEDICINE 1: FINAL PRACTICAL EXAMINATION
Percussion Tones Heard Over the Chest
Type of Tone
Intensity
Pitch
Duration
Resonant
Loud
Low
Long
Flat
Soft
High
Short
Dull
Medium
Medium Medium
Percussion over
to high
liver
Tympanic
Loud
High
Medium
Percussion over
abdomen
Hyperresonant
Very loud Very low Longer
Hyperinflation,
emphysema,
pneumothorax,
asthma
Breath
sounds
Make
sure
the
patient
still
has
his
arms
crossed
over
his
chest
Ask patient to take slow deep breaths through his
mouth
Auscultate with the diaphragm of the stethoscope in the
same areas used in palpation and percussion
Moving from upper lung field to lower, always
comparing one side to another
Listen to 2-3 respiratory cycles before moving to next
position
State if there are adventitious breath sounds
Characteristics of Normal Breath Sounds
Vesicular
Heard over most of lung fields, low pitch,
breezy, soft and short expirations, more
prominent in a thin person or child,
diminished in overweight and very
muscular patient
Bronchovesciuclar Heard over main bronchus area and over
upper right posterior lung field, medium
pitch, expiration equals inspiration
Bronchial /
Heard only over trachea, high pitch, loud
tracheal (tubular)
and long expirations, sometimes a bit
longer than inspiration, coarse, loud
Adventitious Breath Sounds
Fine Crackles
High pitch, discrete, discontinuous
crackling sound heard during the
end of inspiration, not cleared by a
cough
Medium Crackles
Lower, more moist sound heard
during the midstage of inspiration,
not cleared by cough
Coarse Crackles
Loud, bubbly noise heard during
inspiration, not cleared by cough
Ronchi (Sonorous
Loud, low, coarse sounds like a
Wheeze)
snore most often heard
continuously during inspiration or
expiration, coughing may clear
sound (usually means mucus
accumulation in trachea or large
bronchi), more pronounced during
expiration
Wheeze (Sibilant
Musical noise, sounding like a
Wheeze)
squeak, most often heard
continuously during inspiration or
expiration usually louder during
expiration
Pleural Friction Rub
Dry, rubbing, or gating sound,
usually caused by inflammation of
pleural surfaces, heard during
inspiration or expiration, loudest
over lower lateral anterior surface
Quality
Hollow
Very
dull
Dull
thud
Drum like
Booming
Flat: over heavy
muscles, bones,
scapula, spinous
process
Resonant: upper
lung fields
Dull: viscera,
liver
Auscultate anterior lung
fields
Diaphragm
of
the
stethoscope
is
usually
preferable
to
the
bell
for
listening
to
lungs
because
it
transmits
the
ordinary
high-pitched
sounds
better
and
because
it
provides
broader
area
of
sound
Place the stethoscope firmly on the skin
When the individual breath sound is being
evaluated, there should be no movement of patient
or stethoscope except for the respiratory excursion
To auscultate the back, ask the patient to sit as for
percussion with head bent forward and arms
folded in front to enlarge the listening area
Ask the patient to sit erect with shoulders back for
auscultation of anterior chest
Inspect back, cervical and
lumbar spine
Palpate each vertebral
process from cervical to
sacral
Identify the inferior angle of
the scapula and count the
interspaces posteriorly
Palpate any tenderness in
posterior chest wall
Test for tactile fremiti
Compare one side with another,
Test from top to bottom
Patients arms crossed in front
Perform percussion properly
Compare the percussion notes of both hemithorax
from top to bottom
Patients arms crossed in front
Auscultate the posterior thorax and compare one side
with another, test top to bottom
Check voice transmission
Compare one side with another
Patients arms crossed in front
MEDICINE 1: FINAL PRACTICAL EXAMINATION
G. JUGULAR VENOUS PRESSURE AND CAROTID PULSATION
Inspect neck veins and identify highest undulation of
the RIGHT INTERNAL JUGULAR VEIN and measure JVP
at 30 or 45 degrees angle
Position patient properly
Patient supine in bed, raise the patients head
slightly on a pillow
Raise the head of the bed about 30-45 degree
angle
Turn the patients head slightly towards the
left, exposing the right side of the neck
Use tangential white light over the right side of the
patients neck
Identify the right internal vein pulsation
Identify the highest point of the right jugular
venous pulsation
Measure the JVP
Identify the Sternal Angle of Louis by starting from
the suprasternal notch and slide finger down until
a hump is felt
Place a ruler graduated in cm vertically on top of
the Sternal Angle of Louis and extend another ruler
horizontally from the highest point of the jugular
venous pulsation perpendicular to the ruler on the
sternal angle
Note the vertical distance in cm above the Angle of
Louis at which the rulers intersect
State the JVP in cm water
Note the different waveforms of the JVP
Normal JVP: 3 cm at 30 degrees
Palpate for carotid artery pulse (once at a time) and
describe
Assess the right carotid artery pulse
With the patients head at midline, palpates for
the thyroid cartilage starting from the
submentum
Slide the index and middle fingers until a
prominent midline protrusion of the neck,
anterior to the trachea is felt
Gently slides fingers just below the thyroid
cartilage to the cricoid cartilage
With the other hand, turn the patients head
slightly to the right, and slides fingers laterally
from the cricoid cartilage to the groove
between the trachea and the right
sternocleidomastoid muscle
Feel the pulse, press and gradually releases
the right carotid artery pulse
Note the amplitude, contour and speed of the
upstroke and downstroke of the carotid pulse
Normal: Grade 2, pliable with rapid upstroke
and gradual downstroke
Assess the left carotid artery pulse
Same instructions but in the opposite
direction
Auscultate for carotid artery bruit, one at a time
H.
CARDIOVASCULAR
Inspect the precordium and reports its dynamicity
Adynamic (normal), dynamic, hyperdynamic
At eye level, check for
Precordial bulging
Visible pulsations on the precordium
Look for the most lateral precordial pulsation
(apex beat)
Palpate the precordium and describe the apex beat
Palpates the apex beat by using the tips of the
right index and middle fingers
Describe the location of the apex beat
While palpating the apex beat, palpate for the
Angle of Louis with other hand
From the Angle of Louis, slide fingers laterally
to the left intercostal spaces
Count what intercoastal space the apex beat
is located
Using a graduated ruler (cm), note how far
away from the left midclavicular line and
from the midsternal line is the apex beat
found
Describe the diameter of the apex beat
Apply the tips of the fingers directly on top of
the apex beat
Note the number of fingers needed to cover
the apex beat
Describe the diameter of the apex beat in
fingerbreadths
Another method done by using a ruler
graduated in cm and measure the diameter of
apex beat in cm
Describe the amplitude of the apex beat
With fingertips, feel for the apex beat
Note the height of pulsation of the apex beat
whether normal or hyperdynamic (very
strong)
Describe the duration of the apex beat
While palpating the apex beat, auscultate for
the first and second heart sounds
Note the duration of systole
Note how much of systole does the apex beat
occupy
Normal duration: when the apex beat
occupies only up to half of systole
Sustained duration: when the apex beat
occupies almost the entire systole
Palpate for LV or RV heaves, LA lifts, PA lifts, abnormal
pulsations over 2nd ICS RPSL, and thrills
Palpate for heaves in the precordium
Using the heel of right hand, palpate for
abnormally strong pulsation
Left ventricular heave over the area of the
apex beat
Right ventricular heave over the left side of
the lower sternum
Palpate for lifts in the precordium
Using the fingertips, palpate for abnormal
pulsation over the
2nd ICS LPSL for pulmonary artery lift
2nd ICS RPSL for aortic artery dilatation
3rd and 4th ICS LPSL for left arterial lift
Palpate for thrills in the precordium
Using the ball of the hand, feel for fine vibratory
sensation over the different clinical valves
5th ICS, LMCL for mitral valve thrill, area of
apex beat
Left lower sternum for tricuspid valve thrill
2nd ICS LPSL for pulmonic valve thrill
2nd ICS RPSL for aortic valve thrill
MEDICINE 1: FINAL PRACTICAL EXAMINATION
Auscultate
heart
in
the
following
areas:
mitral,
tricuspid,
pulmonic,
aortic
auscultatory
valve
areas
using
diaphragm
in
an
inching
manner
and
note
character
of
S1
and
S2
and
high
pitch
murmurs
if
any
Using the Angle of Louis, locate and identify the
different auscultatory valve areas
5th ICS LMCL: mitral valve
Left lower parasternum: Tricuspid valve
2nd ICS LPSL: pulmonic valve
2nd ICS RPSL: aortic valve
Using the diaphragm of the stethoscope,
auscultate at the different auscultatory valvular
areas for the different heart sounds (either from
apex to base or base to apex in an inching manner)
1st heart sound in the mitral and tricuspid
area
2nd heart sound in the mitral and tricuspid
area
S1 louder at apex
1st heart sound in the aortic and pulmonic
area
2nd heart sound in the aortic and pulmonic
area
S2 louder at base
Note for the time interval between the 1st and 2nd
heart sounds (systole)
1st heart sound followed by the 2nd heart
sound
Note for the time interval between the 2nd and 1st
heart sounds (diastole)
Note for splitting of the 2nd heart sound especially
at the 2nd ICS LPSL
Inhalation
Maneuvers
Ask
patient
to
assume
a
left
lateral
decubitus
position
to
accentuate
heart
sounds
in
the
apical
area
Ask
patient
to
lean
forward
to
accentuate
heart
sounds
in
the
base
Shift
to
the
bell
and
note
for
S3
and
S4
and
any
low
pitch
murmurs
Use the bell of the stethoscope
Auscultate for 3rd and 4th heart sounds at the
mitral and tricuspid valve areas
Use
the
diaphragm
for
high
pitch
and
bell
for
the
low
pitch
sounds,
auscultate
for
abnormal
sounds
Note
for
turbulent
sounds
(murmurs)
noted
during
systole
and
diastole
over
the
different
valvular
areas
Note
the
character
(high/low
pitch),
duration
of
the
murmur(s)
and
grading
of
the
murmur(s)
Slowly
inch
away
and
note
the
radiation
of
the
murmur
Maneuver
Vasalva
Maneuver
Ask
patient
to
take
deep
breath
then
hold,
pinch
nose,
close
mouth
and
strains
down
Carvallos
Sign
Ask
patient
to
inhale
deeply
while
listening
for
any
change
in
the
heart
sounds
I.
ABDOMEN
Instruct patient to relax, bend knees to relax abdomen if
needed and expose abdomen
Inspect abdomen
Skin
characteristic
Striae,
scars,
spider
angioma,
dilated
veins
Abdominal
contour
Flat,
scaphoid,
protruberant,
rounded
Symmetry
Symmetric,
asymmetric
Pulsations
AAA,
abdominal
aortic
aneurysm
Visible
peristalsis
Thin
person,
obstruction
Umbilicus
Flat,
everted
Hernias
Umbilical,
inguinal
Auscultate abdomen
Bowel
sounds
Use
diaphragm
Normal:
5-35
per
minute,
normoactive
Absent:
if
nothing
is
heard
after
5
minutes
Hypoactive:
peritonitis,
ileus
Hyperactive:
gastroenteritis,
hunger,
early
obstruction
Borborygmi:
loud
and
prlonged
Bruits
Use
bell
Harsh,
musical
intermittent
auscultatory
sound
(turbulence)
Stenosis
Normal:
none
Epigastric
area:
aortic,
renal
iliac,
femoral
arteries
RUQ
LUQ
costovertebral
angles
liver
Friction
rub
Fluid
in
pericardial
activity
Over
liver
and
spleen
High
pitched,
heard
in
association
with
respiration
Inflammation
Percuss abdomen systematically in all 4 quadrants
Areas
of
tympanism
Stomach
Traubes
space
(left
AAL,
9th
ICS)
Areas
of
dullness
Liver
If
there
is
splenomegaly,
traubes
space
is
dull
Percuss for liver dullness
Determine upper and lower border
Upper border: measure liver span along
RIGHT midclavicular line going down until it
changes from resonance to dullness
Lower border: percuss at RUQ below
umbilicus going up: note area of dullness
Percuss from lung resonance down to liver
dullness
Normal
Upper
border
(5th
to
7th
ICS)
Lower
border
(costal
margin)
6-12
cm
at
midclavicular
line
4-8
cm
at
midsternal
line
5th
to
7th
ICD
at
midaxillary
line
Percuss for splenic dullness over Traubes space in the
left AAL on deep inspiration
Percuss left lower anterior chest wall
Traubes space: 6th rib, midaxillary line, left costal
margin
Normal: tympanitic
Enlarged:
dullness
MEDICINE 1: FINAL PRACTICAL EXAMINATION
J.
NEUROLOGIC
AND
MUSCULOSKELETAL
Assessment of GCS
Test for motor coordination
Finger to nose test (full arm extension)
Ask the patient to first touch his nose with his
finger then touch your finger
18 inches away
If not normal, dysmetria
Alternate pronation/supination test
Test for balance/equilibrium
Rombergs
test
Ask
patient
to
stand
with
feet
together,
eyes
open
and
hands
by
the
sides
Ask
patient
to
close
his/her
eyes
then
observe
for
a
full
minute
for
swaying
If
(+),
cerebellar
ataxia
Tandem gait test
Ask patient to walk straight
Heel to toe walking
Examine trigeminal nerve functions: sensation to face
and muscles of mastication
Ask the patient to point to where you touch and ask
him/her to tell you if its light or sharp
Ask the patient to open his/her mouth/ protrude
his/her jaw, clench his/her teeth
Check muscles of facial expression
Eye closure
Forehead wrinkling
Eyebrow elevation
Smiling
CN VII
Test gag reflex and note elevation of palate
Touch the posterior wall of the pharynx with a
tongue blade and elicit gag reflex
CN IX and X
Ask patient to stick tongue and note whether its midline
during protrusion (CN-XII)
Test if shoulders are raised against resistance
Always compare right and left
0
No contraction, no movement
1
Fasciculations, flicker, trace of contractions
but no joint movement
2
Gravity eliminated
3
Against gravity but not against resistance
4
Moderate resistance
5
Maximum resistance, full power
Systematically palpate the entire abdomen
Do light palpation first then deep palpation while
looking at the face of the patient
Note any direct or rebound tenderness and any
masses and describe if present
Fingers together, flat on abdominal surface
Gentle dipping motion
Palpate and describe liver edge
Right hand well below lower border of liver
dullness
Press hand gently in and up
Ask patient to take deep breath and feel liver edge
as it comes down
Evaluate liver edge and surface
Normal: not felt
Thin, smooth, firm, even, nontender
Bimanual palpation of the spleen
Supine or lateral decubitus position for the patient
Left hand around and presses forward the left
lower rib cage
Right hand below the left costal margin towards
the spleen
Ask the patient to take deep breath and feel spleen
go down
Normal: not felt
Bimanual and bilateral palpation of the kidneys
RIGHT side of the patient for RIGHT kidney
Left side for left kidney
Hand behind patient below and parallel to the 12th
rib
Lift hand and displace kidney anteriorly
Other hand at upper quadrant, lateral and parallel
to rectus muscle
Ask patient to take a deep breath, at peak of
inspiration, press firmly and deeply in upper
quadrant below costal margin (capture kidney
between two hands)
Palpate kidney at expiration: slowly release
pressure of hand and feel for the kidney as it slides
back to its expiratory position
Normal: not painful, left kidney is not palpable,
right kidney is smooth, firm and non tender
Rectal examination
Patient in LEFT lateral decubitus position
Stretch the left leg, flex right leg
Inspect perianal area
Skin tags, lesions, external hemorrhoids,
lumps, opening of fistula
Digital
examination
Gloves
on
the
RIGHT
hand,
lubricate
index
finger,
insert
gently
into
anal
canal
point
toward
umbilicus
Note
anal
sphincteric
tone
Palpate
all
4
quadrants
and
note
for
mass,
tenderness,
internal
hemorrhoids,
prostate
(size,
consistency,
tenderness),
cervix,
blood
on
examining
finger
Check motor strength of upper and lower extremities
and compare left and right sides including range of
motion
Tempomandibular
joint
Protrusion,
retrusion,
lateral
deviation
of
the
mandible
Shoulder
joint
Forward
flexion,
extension,
abduction,
adduction,
external
rotation,
internal
rotation
Elbow
join
Flexion,
extension,
supination,
pronation
Forearm, wrist and hand
Wrist flexion, extension
Radial/ulnar deviation of wrist
Finger flextion, extension
Finger abduction, adduction
Make a fist
Cervical
Flexion,
extension,
lateral
flexion,
rotation
Lumbar
spine
Flexion,
extension,
lateral
flexion,
rotation
Hip
joint
Flexion,
extension,
abduction,
adduction,
external
rotation,
internal
rotation
Knee
joint
Flexion,
extension
Ankle joint and foot
Dorsiflexion, inversion, eversion
Toe flexion, extension
MEDICINE 1: FINAL PRACTICAL EXAMINATION
Check
sensory
function
of
upper
and
lower
extremities,
compare
left
and
right
sides
Light touch
Pain
Temperature
Vibration
Position
Check
deep
tendon
reflex
Always compare left and right
Biceps (C5,6)
Triceps (C6, 7)
Patellar / knee jerk (L 2,3,4)
Ankle / Achilles (S2)
H.
BONUS
POINTS
Assessment of orthostatic hypotension
You take blood pressure readings with the patient
laying supine, sitting then standing
Wait three minutes between each reading
(+) any sign of a drop in 20 mm-Hg systolic BP and
10 mm-Hg diastolic BP plus an increase in pulse
rate of about 15 beats per minute
Vasalva maneuver
Ask patient to take deep breath then hold, pinch
nose, close mouth and strains down
Carvallos sign
Ask patient to inhale deeply while listening for any
change in the heart sounds
Murphys sign
Lie the patient supine (as you would during any
other abdominal assessment)
Instruct the patient to breath out
Place your palpating hand just below the costal
margin, approximately mid-clavicularly (this is just
above the gallbladder)
Then instruct the patient to slowly breath in;
(+) when the patient stops breathing in due to pain
Obturator test
(+) if pain is elicited on flexion of the hip and
rotation internally
Iliopsoas sign
Passively extending the thigh of a patient lying on
his side with knees extended, or asking the patient
to actively flex his thigh at the hip
(+) if there is abdominal pain
Shifting dullness
First the midline is percussed eliciting a resonant
note due to gas in the bowel
If there is no area of resonance then the test
cannot be performed
Percussion is then moved progressively more
lateral (away from the examiner) until the note
becomes dull
The examiner's index finger is left on the resonant
side, and the middle finger is left on the dull side
The patient is then asked to lean on their right
lateral side (assuming the examiner used the
traditional right sided approach)
Fluid wave
It is performed by having the patient (or a
colleague) push their hands down on the midline of
the abdomen
The examiner then taps one flank, while feeling on
the other flank for the tap
The pressure on the midline prevents vibrations
through the abdominal wall while the fluid allows
the tap to be felt on the other side
(+) if tap can be felt on the other side
I. SAY THANK YOU
10
You might also like
- Cardiovascular BigDocument37 pagesCardiovascular Bigfaiz nasirNo ratings yet
- أدوية الطوارىءDocument162 pagesأدوية الطوارىءManar22No ratings yet
- Almostadoctor - co.uk-OSCE ChecklistDocument10 pagesAlmostadoctor - co.uk-OSCE ChecklistJonathan YoungNo ratings yet
- Cardiology DR - Ahmed MowafyDocument150 pagesCardiology DR - Ahmed MowafyMohamed AlsaabNo ratings yet
- Blood and Drugs Medicine NotesDocument39 pagesBlood and Drugs Medicine Notesrahuul prasadNo ratings yet
- YEAR 1 and 2 OSCE Revision: Author: DR Thomas PayneDocument30 pagesYEAR 1 and 2 OSCE Revision: Author: DR Thomas Payneminayoki100% (1)
- Part IIDocument64 pagesPart IIhussainNo ratings yet
- Problem-based Approach to Gastroenterology and HepatologyFrom EverandProblem-based Approach to Gastroenterology and HepatologyJohn N. PlevrisNo ratings yet
- Medical MnemonicsDocument256 pagesMedical MnemonicssitalcoolkNo ratings yet
- OSCE Internal MedicineDocument4 pagesOSCE Internal Medicinemohamed mowafeyNo ratings yet
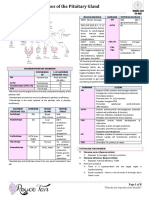
- Diseases of the Pituitary GlandDocument8 pagesDiseases of the Pituitary GlandSheryl Layne Lao-SebrioNo ratings yet
- Clinical ExaminationDocument11 pagesClinical ExaminationMavra zNo ratings yet
- Shivaani (Internal Medicine CWU)Document12 pagesShivaani (Internal Medicine CWU)S.M. Manogaran Shivaani AP S.M. ManogaranNo ratings yet
- FGE Report August/September 2002Document12 pagesFGE Report August/September 2002mnigam64No ratings yet
- Clinical Examination Guide for Oral MedicineDocument123 pagesClinical Examination Guide for Oral MedicineDeepti ChaharNo ratings yet
- History of Fever and DiarrheaDocument4 pagesHistory of Fever and DiarrheaAndréAmistosoNo ratings yet
- ECG ReviewDocument146 pagesECG ReviewThea DinoNo ratings yet
- HyphemaDocument19 pagesHyphemaLiyanti RinceNo ratings yet
- FcpsDocument205 pagesFcpsSoniya DulalNo ratings yet
- Aquifer InternalMedicine09 - 55Document7 pagesAquifer InternalMedicine09 - 55JulieNo ratings yet
- Pediatric OSCEDocument153 pagesPediatric OSCEAtria DewiNo ratings yet
- Skill Labs, Clinical History Taking, and ExaminationDocument84 pagesSkill Labs, Clinical History Taking, and ExaminationJoo Se HyukNo ratings yet
- GI Signs and SymptomsDocument40 pagesGI Signs and SymptomsJohnny BeeNo ratings yet
- Examination of The AbdomenDocument2 pagesExamination of The Abdomenkenners100% (13)
- Aquifer InternalMedicine11 - 45Document8 pagesAquifer InternalMedicine11 - 45JulieNo ratings yet
- Fundamentals of ECGDocument112 pagesFundamentals of ECGadithya polavarapu100% (1)
- HeartMurmursExplained SystolicDiastolicManeuversDocument41 pagesHeartMurmursExplained SystolicDiastolicManeuversurtikikeNo ratings yet
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsNo ratings yet
- A Simple Guide to Circulatory Shock, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Circulatory Shock, Diagnosis, Treatment and Related ConditionsNo ratings yet
- RELOCATE TO THE UK AS A DOCTOR: A STEP-BY-STEP E-GUIDE ON HOW TO MOVE TO THE UNITED KINGDOM AND WORK AS A DOCTOR IN THE NHSFrom EverandRELOCATE TO THE UK AS A DOCTOR: A STEP-BY-STEP E-GUIDE ON HOW TO MOVE TO THE UNITED KINGDOM AND WORK AS A DOCTOR IN THE NHSNo ratings yet
- CLINICAL HISTORY AND DIFFERENTIAL DIAGNOSIS AT YOUR FINGERTIPSFrom EverandCLINICAL HISTORY AND DIFFERENTIAL DIAGNOSIS AT YOUR FINGERTIPSNo ratings yet
- Torsade De Pointes, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandTorsade De Pointes, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- A Simple Guide to Abdominal Aortic Aneurysm, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Abdominal Aortic Aneurysm, Diagnosis, Treatment and Related ConditionsNo ratings yet
- Synovial Chondromatosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandSynovial Chondromatosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Microcirculation as Related to ShockFrom EverandMicrocirculation as Related to ShockDavid SheproNo ratings yet
- Mock Papers for MRCPI, 3rd Edition: Four Mock Tests With 400 BOFsFrom EverandMock Papers for MRCPI, 3rd Edition: Four Mock Tests With 400 BOFsNo ratings yet
- Kochar's Clinical Medicine for Students: Sixth EditionFrom EverandKochar's Clinical Medicine for Students: Sixth EditionNo ratings yet
- Abnormal Slow Heart Beats, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandAbnormal Slow Heart Beats, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- International Medical Graduate and the United States Medical Residency Application: A Guide to Achieving SuccessFrom EverandInternational Medical Graduate and the United States Medical Residency Application: A Guide to Achieving SuccessRaghav GovindarajanNo ratings yet
- Treatment of Minor Thermal BurnsDocument22 pagesTreatment of Minor Thermal BurnsTP RMad100% (1)
- Initial Drugs For HFrEFDocument1 pageInitial Drugs For HFrEFTP RMadNo ratings yet
- Acute Asthma Exacerbations in Children: Emergency Department Management - UpToDateDocument13 pagesAcute Asthma Exacerbations in Children: Emergency Department Management - UpToDateTP RMadNo ratings yet
- Initial Drugs For HFrEFDocument1 pageInitial Drugs For HFrEFTP RMadNo ratings yet
- Blank 2Document5 pagesBlank 2TP RMadNo ratings yet
- Acute Urinary RetentionDocument14 pagesAcute Urinary RetentionTP RMadNo ratings yet
- Approach To The Adult With EpistaxisDocument18 pagesApproach To The Adult With EpistaxisTP RMad100% (1)
- Medical MnemotechnicsDocument149 pagesMedical MnemotechnicsMaja Maja BułkaNo ratings yet
- Glycopeptide and LincosamideDocument8 pagesGlycopeptide and LincosamideTP RMadNo ratings yet
- Behmed Quiz 4 Feb 2010Document2 pagesBehmed Quiz 4 Feb 2010TP RMadNo ratings yet
- 2015 ESC IE Guidelines EHJ 2015Document54 pages2015 ESC IE Guidelines EHJ 2015TP RMadNo ratings yet
- Imaging of Pneumothorax - UpToDateDocument40 pagesImaging of Pneumothorax - UpToDateTP RMadNo ratings yet
- Secondary Spontaneous Pneumothorax in Adults - UpToDateDocument15 pagesSecondary Spontaneous Pneumothorax in Adults - UpToDateTP RMadNo ratings yet
- Primary Spontaneous Pneumothorax in Adults - UpToDateDocument13 pagesPrimary Spontaneous Pneumothorax in Adults - UpToDateTP RMadNo ratings yet
- Pathogen Es IsDocument2 pagesPathogen Es IsTP RMadNo ratings yet
- AuscultogramDocument9 pagesAuscultogramTP RMadNo ratings yet
- CE2 Schedule AY 09-10Document5 pagesCE2 Schedule AY 09-10TP RMadNo ratings yet
- Med 1 Lecture No. 17 - Involuntary Weight Loss, Eating Disorders, ObesityDocument9 pagesMed 1 Lecture No. 17 - Involuntary Weight Loss, Eating Disorders, ObesityTP RMadNo ratings yet
- Surg Samplex Unknown YearDocument4 pagesSurg Samplex Unknown YearTP RMadNo ratings yet
- COT Pathogenesis & Clin Manifestations PDFDocument1 pageCOT Pathogenesis & Clin Manifestations PDFTP RMadNo ratings yet
- PathoPracs SGD HeadNeck ElaineDocument15 pagesPathoPracs SGD HeadNeck ElaineTP RMadNo ratings yet
- Surg Samplex Unknown YearDocument4 pagesSurg Samplex Unknown YearTP RMadNo ratings yet
- Pracs Reviewer - HematopathologyDocument5 pagesPracs Reviewer - HematopathologyTP RMadNo ratings yet
- Clinical Decision Using An Article About Treatment: George G. Lim, MD, FPSGS, FPCS, FpscrsDocument44 pagesClinical Decision Using An Article About Treatment: George G. Lim, MD, FPSGS, FPCS, FpscrsTP RMadNo ratings yet
- Med 1 Lecture No. 24 - Geriatric MedicineDocument1 pageMed 1 Lecture No. 24 - Geriatric MedicineTP RMadNo ratings yet
- Literature SearchDocument3 pagesLiterature SearchTP RMadNo ratings yet
- Principles of Decision Making: Clinical Decision Using An Article About TreatmentDocument8 pagesPrinciples of Decision Making: Clinical Decision Using An Article About TreatmentTP RMadNo ratings yet
- Clinical Decision Using An Article About Treatment: George G. Lim, MD, FPSGS, FPCS, FpscrsDocument44 pagesClinical Decision Using An Article About Treatment: George G. Lim, MD, FPSGS, FPCS, FpscrsTP RMadNo ratings yet
- Ismail's Undergraduate ThesisDocument82 pagesIsmail's Undergraduate ThesisAbiola IbrahimNo ratings yet
- Stay Healthy This WinterDocument4 pagesStay Healthy This WinterMariaNo ratings yet
- Ultimate Reset Cleanse BeachbodyDocument7 pagesUltimate Reset Cleanse BeachbodyJessica CamposNo ratings yet
- Succeed in CAE Practce Tests SamplepagesDocument18 pagesSucceed in CAE Practce Tests SamplepagesEva Rodriguez50% (2)
- PNOE Ergometry Results: Start Time End TimeDocument1 pagePNOE Ergometry Results: Start Time End TimeAlejandroPintoAngelNo ratings yet
- Recommended Weight Gain During Pregnancy ForDocument2 pagesRecommended Weight Gain During Pregnancy Forabdelhamed aliNo ratings yet
- Farmakologi Benincasa Hispida (Kundur)Document11 pagesFarmakologi Benincasa Hispida (Kundur)Syahrir ManaanNo ratings yet
- Don'T Exercise Cellercise!: by Rica E. VillalonDocument21 pagesDon'T Exercise Cellercise!: by Rica E. VillalonMónica SastoqueNo ratings yet
- Diet & Nutrition CounsellingDocument7 pagesDiet & Nutrition Counsellingshilpasheetal0% (1)
- Black AdonisDocument4 pagesBlack Adonisapi-74769985No ratings yet
- Changes in Diet and Lifestyle and Long-Term Weight Gain in Women and MenDocument13 pagesChanges in Diet and Lifestyle and Long-Term Weight Gain in Women and MenemanvitoriaNo ratings yet
- FCD 09-01 Cheese Leader GuideDocument6 pagesFCD 09-01 Cheese Leader GuideAnonymous Zz1XfL5ylNo ratings yet
- 2nd DayDocument13 pages2nd DayMaan Cheska100% (1)
- Effects of Low Versus High Volume High Intensity Interval - 2023 - Journal of EDocument10 pagesEffects of Low Versus High Volume High Intensity Interval - 2023 - Journal of ESherriNo ratings yet
- Family Case Analysis 2Document98 pagesFamily Case Analysis 2Carl Elexer Cuyugan Ano50% (2)
- Track athlete activity and progress with user storiesDocument1 pageTrack athlete activity and progress with user storiesOvopa AcNo ratings yet
- CH 05 Solutions To ProblemsDocument11 pagesCH 05 Solutions To ProblemsrehassanNo ratings yet
- Strength Training Guidelines For Rowers PDFDocument28 pagesStrength Training Guidelines For Rowers PDFmendes67100% (1)
- Benefits of Breast Feeding SummaryDocument3 pagesBenefits of Breast Feeding SummaryMarcus Skookumchuck VanniniNo ratings yet
- Study Questions Chapter 3: Health Risk BehavioursDocument3 pagesStudy Questions Chapter 3: Health Risk BehavioursZakariaNo ratings yet
- Thrombophlebitis 1Document8 pagesThrombophlebitis 1Aya Rugaiyah AlkaffNo ratings yet
- Reader 39 S Digest Int 39 L - May 2016 VK Com StopthepressDocument128 pagesReader 39 S Digest Int 39 L - May 2016 VK Com StopthepressRidwan Mohammed NurNo ratings yet
- Omega-3 6 and 9 Fats PDFDocument4 pagesOmega-3 6 and 9 Fats PDFMohd TaufiqNo ratings yet
- Biology A (Salters Nuffield) : Pearson Edexcel Level 3 GCEDocument36 pagesBiology A (Salters Nuffield) : Pearson Edexcel Level 3 GCEGershonNo ratings yet
- Anatomy and PhysiologyDocument5 pagesAnatomy and Physiologyjohnbech07No ratings yet
- Estimation of Blood GlucoseDocument16 pagesEstimation of Blood GlucoseAhmed MohamadNo ratings yet
- Oral Antidiabetic Glicazide GuideDocument3 pagesOral Antidiabetic Glicazide Guideshe'sgotyouhighNo ratings yet
- Fast Food Industry in Jollibee Tabunoktalisay City and Its Benefits To Working Class PeopleDocument19 pagesFast Food Industry in Jollibee Tabunoktalisay City and Its Benefits To Working Class PeopleLeahNo ratings yet
- Hormones Endocrine Gland: (Clipart Edited From Corel Presentations 8)Document3 pagesHormones Endocrine Gland: (Clipart Edited From Corel Presentations 8)Zheena S. JaroNo ratings yet
- De Thi Mon Tieng Anh Chuyen Ma de 166Document8 pagesDe Thi Mon Tieng Anh Chuyen Ma de 166kuangte0No ratings yet