Professional Documents
Culture Documents
How To Write A Global Health Case Report
Uploaded by
pranabchatterjee0 ratings0% found this document useful (0 votes)
12 views5 pagesThis document provides guidance on how to write a case report for a global health journal. It outlines the key sections that should be included such as the title, summary, case presentation, global health problem list, and global health problem analysis. The summary should be 150 words and give an overview of the case or global health issue. The case presentation section should provide clinical details of the patient's presentation and outcomes. The global health problem list identifies the issues raised by the case, which are then analyzed in more detail in the global health problem analysis section through a literature review. This section examines each problem and potential solutions through medical, epidemiological and sociopolitical research.
Original Description:
How to write a Global Health Case Report, a resource from the BMJ Case Reports website. For those who are interested in submitting their Global Health cases to the BMJ.
Original Title
How to Write a GH CR
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document provides guidance on how to write a case report for a global health journal. It outlines the key sections that should be included such as the title, summary, case presentation, global health problem list, and global health problem analysis. The summary should be 150 words and give an overview of the case or global health issue. The case presentation section should provide clinical details of the patient's presentation and outcomes. The global health problem list identifies the issues raised by the case, which are then analyzed in more detail in the global health problem analysis section through a literature review. This section examines each problem and potential solutions through medical, epidemiological and sociopolitical research.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
12 views5 pagesHow To Write A Global Health Case Report
Uploaded by
pranabchatterjeeThis document provides guidance on how to write a case report for a global health journal. It outlines the key sections that should be included such as the title, summary, case presentation, global health problem list, and global health problem analysis. The summary should be 150 words and give an overview of the case or global health issue. The case presentation section should provide clinical details of the patient's presentation and outcomes. The global health problem list identifies the issues raised by the case, which are then analyzed in more detail in the global health problem analysis section through a literature review. This section examines each problem and potential solutions through medical, epidemiological and sociopolitical research.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 5
How to write a Global Health case report
The title should be straight
forward nothing cryptic
The summary is the only part of
the manuscript that has a word
limit. It appears on PubMed just
as an abstract might, so it should
give a good overview of your
paper.
This may be further anonymised.
Exact age and ethnic origin are
not essential.
Describe the clinical reason that
the patient first presented and
give the clinical details in the
usual way, as per a standard
clinical case report.
TITLE OF CASE Do not include a case report
Ramifications of minority populations with poor medical
education and screening: an extensive acral melanoma
150 WORD SUMMARY Focus the summary on the case or
the Global Health problem that you want to discuss. You
may wish to give an indication of the severity of the case
or the scale of the problem
An elderly Samoan man presented, after a two year
holistic self-treatment period on his home island, with a
painful, hyperpigmented mass on his left heel. Physical
exam revealed a black, friable tumor with necrotic tissue
and superficial ulcerations with no other associated
symptoms. Further work up revealed that the mass was
invasive and treated with resection. A final diagnosis of
acral-lentiginous melanoma; stage T4b was made. Poor
access to care and screening services are large barriers to
care for minorities and patients of low socioeconomic
status. Once access is obtained, however, it does not
guarantee patient compliance. Healthcare practices often
clashes with societal beliefs, therefore, patient education
regarding their disease and its possible progression,
along with treatment options are important.
Furthermore, lack in the ethnic diversity of physicians
contributes to low cultural competency amongst their
patients resulting in poor communication and low patient
satisfaction of care.
CASE PRESENTATION Explain the relevant features of the
case in sufficient detail so that someone in another
country would have a good understanding of who you are
describing. Go back to the history of the problem, and
forward to the outcomes that have resulted
An 82 year old Samoan man, skin phototype V, presented
with left heel pain due to a large, exophytic,
hyperpigmented, polypoid mass. His initial presentation to
the Dermatology Clinic was two years prior and was seen for a
small, dark macule; but the patient elected to self-medicate
holistically over this time on his home island until his heel pain
caused his return. Physical exam revealed a lesion consisting of
black, necrotic nodules and friable granulation tissue along with
ulcerations and purulent/serosanguinous drainage. At the base
of the lesion was a hyperpigmented, asymmetrical macule with
nodularity (figure 1). The man had no other associated
symptoms and no lymphadenopathy.
An MRI noted a 9x7cm lobulated; exophytic left heel soft tissue
mass with invasion into the fat pad, but no other tissue invasion
or bone erosion. Biopsies from the medial and plantar surface of
the macular lesion showed marked pigment deposition
throughout all levels of the epidermis and into the superficial
dermis (figure 2). The histopathologic findings also
demonstrated lentiginous proliferation of atypical melanocytes
associated with irregular epidermal acanthosis along with
prominent pagetoid spread of atypical intraepidermal
melanocytes (figure 3). Atypical melanocytes were noted at
dermal papillae tips, but it was difficult to discern any definitive
invasion into the dermis. These initial findings suggested a
diagnosis of malignant melanoma in-situ, acral lentiginous-type
along with a vertical growth phase resulting in an extensive
nodule. Although definitive features of invasive melanoma were
not identified, given the patients history, small sample size of
tissue, and lack of biopsies from the fungating mass itself; it was
felt that tumor excision was the most appropriate treatment.
Simply list the social
determinants of your
patients health. These
may be anything from
access to health services,
education, transport
facilities and where they
live to socioeconomic
status, employment,
political stability of their
country or cultural aspects
that affect health.
Each of these is discussed
in more detail in the
section below.
This section requires a
comprehensive literature review
and is NOT a summary of the
literature.
Global Health problems are
difficult to solve. Solutions must
be prioritised and be appropriate
to the context of the patient. This
requires real analysis of the
problems, not simply a summary
of the evidence.
The problem you describe in the
case presentation is a global one.
Therefore, the literature must
reflect the global incidence, global
significance, global evidence and
potential global solutions.
A sentinel node biopsy was negative and a below the knee
amputation was completed. Gross examination of the prosection
revealed clear margins and findings of a variably pigmented
(white to jet black) lesion with a focal area of fungating tumor
measuring about 9x7x3cm overall. Adjacent to this fungating
mass, covering approximately half of the lateral aspect of the
foot, was an ill-defined, gray-blue discoloration measuring
11x8cm. Finally, located 0.4cm medially from the variably
pigmented lesion and grossly separate from the main lesion, was
a well-demarcated, slightly firm, jet black lesion measuring
0.5x0.5x0.2cm. Microscopic findings of the fungating mass
revealed superficial ulceration and an underlying multinodular,
heavily pigmented mass with gross extension into the adjacent
adipose tissue that measured 3.2cm Breslow depth. Additional
histopathologic findings of the mass and lesions were consistent
with biopsy results as well as demonstrating invasion into the
dermis and subcutaneous tissues. Midway through the dermis,
there was prominent regression that was indicated by tumoral
melanosis and fibrosis. Deeper to this, the tumor extended into
the subcutaneous tissue without pigmentation supported by
findings of marked cytologic atypia that included pleomorphism,
abnormal chromatin patterns, and atypical mitotic figures (figure
4). The mitotic count was 15 per square millimeter with hot spot
method. There was no definitive lymphovascular invasion or
perineural invasion identified. Acral lentiginous melanoma,
stage T4b, was the final diagnosis (figure 5).
GLOBAL HEALTH PROBLEM LIST Just list the problems
raised in the case. These will be discussed more precisely
in the section below
- Minorities with darker skin tones are at higher risk
for acral melanomas.
- Minorities and those of low socioeconomic status
(SES) usually present with advanced disease.
- Minority patients and those of low SES have
decreased access to care due to multifactorial
barriers.
- Poor secondary preventative medicine in low SES
populations.
- Poor diversity among healthcare providers results
in decreased cultural competency
GLOBAL HEALTH PROBLEM ANALYSIS The problem
analysis directly addresses each problem in your case that
needs attention to achieve a better health outcome for the
patient. This should be a well-researched and balanced
account. Find and appraise all the relevant medical,
epidemiological and socio-political literature. Explaining
missing epidemiological data is important in the appraisal
of the literature. Make sure you discuss all the relevant
aspects of the case, including important anthropological,
cultural and community issues
According to a report done in California, Native Hawaiians and
Pacific Islanders (NHPI) were one of only two racial groups
where the leading cause of death was cancer and above the
national average.[1] Acral lentiginous melanomas make up the
most common form of melanoma in dark-skinned individuals,
ranging from 29%-72%, with a median age of onset of 65, and
often result in a higher lethality rate due to misdiagnoses in
favor of diagnosing more common diseases.[2] Minorities with
darker skin tones places them at a higher risk for acral
melanomas.[3] Additionally, minorities and those of low
socioeconomic status (SES) usually present with thicker lesions
and more advanced disease leading to a higher mortality
rate.[3-5]
Poorer health outcomes in low SES populations are likely due to
poor secondary prevention in low SES populations, such as
access to physician skin screening services and patient education
of harmful melanocytic lesions.[3,4] One study found that
women and younger patients tend to seek out medical screening
services more often than their counterparts.[6] Another study
revealed that low-SES patients generally have inadequate
knowledge of their own medical condition, tend to have a high
school education or less, and have difficulties arranging
transportation; contributing to care barriers.[7] Meanwhile,
those of high SES are generally more educated with a larger
fund of medical knowledge, i.e. skin changes can be an
indication of skin cancer.[5] With this knowledge, patients of
high SES tend to recognize any skin changes when they selfscreen and obtain medical treatment earlier than lower SES
patients.[5]
Our patient, being an elderly gentleman from a remote Pacific
island, supports this notion of increased wait time in seeking
preventative services in addition to incurring barriers to his own
care, to include proper understanding and knowledge of his
disease and the vast distance traveled in order to obtain proper,
specialty care. Rural and isolated populations have very similar
characteristics when speaking about access to care. Several
studies show that, historically, these areas have poor access to
care mainly due to the vast travel distance, time, lack of
specialty care, and financial burden to obtain healthcare
services; with larger distances correlating to infrequent doctor
visits, decreased use of preventative services and decreased
routine medical follow ups.[8-10]
Multiple studies have shown that having a usual source of care
(person or place where one receives healthcare) improves
preventative medical screening services and decreases health
disparities; however, this is often not available to
minorities.[7,11-13] Language proficiency, insurance
availability, time away from work, low income combined with
out-of-pocket expenses, and even lack of citizenship are some
barriers experienced by minorities that prevent them from
obtaining a usual source of care; thus creating health disparities
and poorer overall health.[1,14,15]
Of these, insurance availability is likely the biggest barrier.
Having health insurance decreases health disparities among high
and low SES groups by opening doors to preventative and
primary care while lowering the overall cost.[13,15,16] Though
many uninsured minorities are eligible for insurance, they do no
sign up for it often due to lack of awareness about the benefit or
have limited English proficiencies;[11] though a California study
showed a high, 88%, English proficiency among NHPI.[1]
Another patient barrier to care is the lack of cultural
understanding or competency by the physician. Generally,
physicians withhold more clinical information from minority
patients, which often leads the patient to a feeling of being left
out of the medical decision-making process of their own
care.[11] Typically, the ethnic makeup of physicians does not
reflect the diversity of their patients.[1] Due to this asymmetry,
there is a strong sense within each ethnic community that the
physician is not aware of popular cultural alternative/holistic
medicine therapies.[11] It is plausible that a Samoan provider
would have been able to relate better to our patient at an earlier
point of care, understand his concerns and desires to try a
homeopathic treatment, and further educate the patient about
his advanced disease and need for modern medical treatments,
thus leading to a better outcome.
This section requires a
comprehensive literature review
and is NOT a summary of the
literature.
Global Health problems are
difficult to solve. Solutions must
be prioritised and be appropriate
to the context of the patient. This
requires real analysis of the
problems, not simply a summary
of the evidence.
The problem you describe in the
case presentation is a global one.
Therefore, the literature must
reflect the global incidence, global
significance, global evidence and
potential global solutions.
Please use relevant and
contemporary references where
appropriate.
Often with differences in cultural background along with
language comprehension, there is a breakdown in
communication that strains the physician-patient relationship
that leads to decreased trust in the physician, poor quality of
care due to patients lack of following physician
recommendations, and poor interactions and misunderstandings
that lead to decreased primary care visits and decreased use of
preventative services.[11] A more diverse and/or engaged
healthcare team builds greater cultural competency and provides
high-quality care to all patients; there is better communication
between the two parties which leads the patient to a more
comprehensive understanding of their particular condition and
treatment options which creates a stronger, patient-centered
interaction that lowers discriminatory perceptions and increases
patient care satisfaction.[1,11]
LEARNING POINTS/TAKE HOME MESSAGES 3 to 5 bullet
points this is a required field and should be directly
relevant to the Global Health issues being discussed
- Acral melanoma rates are increased in minority
populations.
- The most important prognostic factor for patients
with localized melanoma is tumor thickness.
- Patient education, access to care, and early
intervention are primary tools used to detect early
melanoma that can be treated, preventing
advanced disease, and, thereby decrease mortality.
- A usual source of care enhances preventative and
screening medical services; often provided by
insurance, however, benefits unlikely known or
difficult to obtain due to language barriers and
work constraints.
- Healthcare providers increased cultural
competency leads to improved health outcomes in
minority patients and higher patient satisfaction
scores.
REFERENCES Vancouver style
1. Ponce N, Tseng W, Ong P, et al. California Asian Pacific
Islander Joint Legislative Caucus. The State of Asian
American, Native Hawaiian and Pacific Islander Health in
California Report. California: California Program on
Access to Care, California Program on Opportunity and
Equity, and Kaiser Permanente, 2009. Print.
2. Bailey EC, Sober AJ, Tsao H, et al. Chapter 124.
Cutaneous Melanoma. In: Goldsmith LA, Katz SI,
Gilchrest BA, editors. Fitzpatrick's Dermatology in General
Medicine, 8th ed. New York, NY: McGraw-Hill; 2012.
This is Vancouver style. Please
use this. Do not simply cut and
paste online sources
All figures must be clearly
annotated. Use arrows if
necessary.
3. Ortiz CA, Goodwin JS, Freeman JL. The effect of
socioeconomic factors on incidence, stage at
diagnosis and survival of cutaneous melanoma.
Med Sci Monit 2005; 11:RA16372.
4. Linos E, Swetter SM, Cockburn MG, et al. Increasing
burden of melanoma in the United States. J Invest
Dermatol 2009; 129:1666-74.
5. Idorn LW, Wulf HC. Socioeconomic status and cutaneous
malignant melanoma in Northern Europe. Brit J Derm
2014; 170:787-93.
6. Reyes-Ortiz CA, Goodwin JS, Freeman JL, et al.
Socioeconomic Status and Survival in Older Patients with
Melanoma. J Am Geriatr Soc 2006; 54(11):1758-64.
7. Starfield B, Shi L. The Medical Home, Access to Care, and
Insurance: A Review of Evidence. Pediatrics 2004;
113:1493-8.
8. Nemet GF, Bailey AJ. Distance and health care utilization
among the rural elderly. Soc Sci Med 2000; 50:1197-208.
9. Person DA. Pacific Island Health Care Project: early
experiences with a web-based consultation and referral
network. Pac Health Dialog 2000; 7(2):29-35.
This is often the most valuable
part of the case report. The
patient should write in their own
words. A good time to do this is
after the case report is written, so
that the patient may give
informed consent and their
perspective at the same time.
FIGURE/VIDEO CAPTIONS Figures should NOT be
embedded in this document
Figure 1: Large, exophytic, hyperpigmented, polypoid,
acral mass.
Figure 2: Marked pigment deposition throughout the basal
layer on the lower magnification, H&E, 4X.
Figure 3: Lentiginous proliferation of atypical melanocytes
on the basal layer of the epidermis, and a few scattered
pagetoid spread, H&E, 20X.
Figure 4: Large, pigmented, pleomorphic cells with
nucleoli and chromatin irregularities. Multiple mitotic
figures, some atypical, are present, H&E, 20X.
Figure 5: Amputation of affected limb and dissection of
acral mass.
PATIENTS PERSPECTIVE Optional but strongly
encouraged this has to be written by the patient or next
of kin
The patients family declined to provide a written statement.
You might also like
- Lookingbill and Marksâ Principles of Dermatology (PDFDrive)Document320 pagesLookingbill and Marksâ Principles of Dermatology (PDFDrive)Alexander Hartono100% (5)
- Hematology SOPsDocument99 pagesHematology SOPssalamon2t100% (1)
- Ws - Mea Millennium Ecosystem AssessmentDocument3 pagesWs - Mea Millennium Ecosystem Assessmentapi-305791685No ratings yet
- All About Ocean Life-Rachel BladonDocument6 pagesAll About Ocean Life-Rachel BladonRichard TekulaNo ratings yet
- Fire Alarm SymbolsDocument6 pagesFire Alarm Symbolscarlos vasquezNo ratings yet
- Epidemiiology SeminarDocument15 pagesEpidemiiology SeminarMugu 123No ratings yet
- An Update On The Diagnosis and Treatment of LeprosyDocument10 pagesAn Update On The Diagnosis and Treatment of LeprosyChlarissa WahabNo ratings yet
- Concept BuildingDocument1,586 pagesConcept BuildingMUWANGUZI ALEXANDERNo ratings yet
- Adenoid Cystic Carcinoma of Hard Palate: A Case ReportDocument5 pagesAdenoid Cystic Carcinoma of Hard Palate: A Case ReportHemant GuptaNo ratings yet
- M CAD Ermatol CtoberDocument1 pageM CAD Ermatol CtoberFerdie YuzonNo ratings yet
- Liceo de Cagayan University College of NursingDocument29 pagesLiceo de Cagayan University College of Nursingchin41686No ratings yet
- Epidemiology MCH 101Document96 pagesEpidemiology MCH 101Christiaan Gaye B. PilayNo ratings yet
- What We Know About Cancer AmericaDocument68 pagesWhat We Know About Cancer AmericaErdemNo ratings yet
- Managing The Risk of Cancer in Cowden Syndrome: A Case ReportDocument4 pagesManaging The Risk of Cancer in Cowden Syndrome: A Case ReportKaisun TeoNo ratings yet
- Squamous Cell Carcinoma of The Lung Presenting As A Fungating Ulcerated Skin Lesion: A Case ReportDocument7 pagesSquamous Cell Carcinoma of The Lung Presenting As A Fungating Ulcerated Skin Lesion: A Case ReportwonderNo ratings yet
- Research Paper On Skin BleachingDocument4 pagesResearch Paper On Skin Bleachingefeq3hd0100% (1)
- 10.1007@s12094 019 02107 WDocument6 pages10.1007@s12094 019 02107 WUzi SuruziNo ratings yet
- Fetch ObjectDocument12 pagesFetch ObjectJoel FlosanNo ratings yet
- Lethal Midline Granuloma Importance of Early Diagnosis: A Case ReportDocument0 pagesLethal Midline Granuloma Importance of Early Diagnosis: A Case ReportdeolukmanaNo ratings yet
- Pediatric Cancer in Perspective: Cure NOT: IS EnoughDocument5 pagesPediatric Cancer in Perspective: Cure NOT: IS EnoughKaren MacDonaldNo ratings yet
- TB NewDocument6 pagesTB NewTirza StevanyNo ratings yet
- Value of Epi Research in Clinical PracticeDocument6 pagesValue of Epi Research in Clinical PracticeFouzia ShariqNo ratings yet
- Jcad 2 8 30Document3 pagesJcad 2 8 30Mariana ValerianoNo ratings yet
- International Journal of Pediatric OtorhinolaryngologyDocument22 pagesInternational Journal of Pediatric OtorhinolaryngologyDear Farah SielmaNo ratings yet
- v1 CoveredDocument9 pagesv1 CoveredIdmNo ratings yet
- Cancer Screening in the Developing World: Case Studies and Strategies from the FieldFrom EverandCancer Screening in the Developing World: Case Studies and Strategies from the FieldMadelon L. FinkelNo ratings yet
- Symposium Article: Cultural Beliefs and Values in Cancer PatientsDocument4 pagesSymposium Article: Cultural Beliefs and Values in Cancer PatientsDiānë Spëncēr LÿnčhNo ratings yet
- 3descriptive EpidemiologyDocument49 pages3descriptive EpidemiologyAnusha VergheseNo ratings yet
- Ingles Datos de Aumento de Cancer en Niños y Adolescentes EeuuDocument11 pagesIngles Datos de Aumento de Cancer en Niños y Adolescentes EeuuMildred RiofrioNo ratings yet
- Principii Psiho OncologieDocument16 pagesPrincipii Psiho OncologieCristina Tulba100% (1)
- Research Paper Topics About HivDocument8 pagesResearch Paper Topics About Hivlrqylwznd100% (1)
- 6703 23736 1 PBDocument3 pages6703 23736 1 PBReski Harlianty HarliNo ratings yet
- SPIKES Six-Step Protocol For Delivering Bad News - Application To The Patient With CancerDocument15 pagesSPIKES Six-Step Protocol For Delivering Bad News - Application To The Patient With Cancerdudubloom007No ratings yet
- An International Survey of Physician Attitudes and Practice in Regard To Revealing The Diagnosis of CancerDocument4 pagesAn International Survey of Physician Attitudes and Practice in Regard To Revealing The Diagnosis of Cancerm.pernetasNo ratings yet
- Advance Epi & Direct Acyclic GraphDocument14 pagesAdvance Epi & Direct Acyclic GraphPurnima VermaNo ratings yet
- Epidemiology and Prevention of Cancer: LearningDocument20 pagesEpidemiology and Prevention of Cancer: LearningWeiLinNo ratings yet
- Spikes PDFDocument11 pagesSpikes PDFMona LisaNo ratings yet
- Non Experimental EpidemologyDocument16 pagesNon Experimental EpidemologyKrishnaveni MurugeshNo ratings yet
- Dermatologic Emergencies Diagnosing and Managing Life-Threatening RashesDocument28 pagesDermatologic Emergencies Diagnosing and Managing Life-Threatening RashesWva RalphNo ratings yet
- Melanoma in Clinical PracticeFrom EverandMelanoma in Clinical PracticeRhoda M. AlaniNo ratings yet
- Module 1 Epidemiology Anatomy and Physiology of The Cell CarcinogenesisDocument38 pagesModule 1 Epidemiology Anatomy and Physiology of The Cell CarcinogenesisAlessandra MercadoNo ratings yet
- Randall 1996Document21 pagesRandall 1996agita kartika sariNo ratings yet
- Pure Vulvar Langerhans Cell Histiocytosis A Case Report and Literature ReviewDocument8 pagesPure Vulvar Langerhans Cell Histiocytosis A Case Report and Literature ReviewqdvtairifNo ratings yet
- Case ReportDocument12 pagesCase ReportRimueng GhuenNo ratings yet
- Postgrad Med J 1989 Crisp 150 5Document7 pagesPostgrad Med J 1989 Crisp 150 5Octavian Alexandru BoghiciNo ratings yet
- Factitious in Children and AdolescentsDocument8 pagesFactitious in Children and Adolescentslors93No ratings yet
- Descriptive Epidemiology: Submitted by Nirmal Varghese KDocument26 pagesDescriptive Epidemiology: Submitted by Nirmal Varghese KHAMID100% (1)
- Research On CancerDocument11 pagesResearch On Cancerrubyshah886No ratings yet
- Unequal Quality in Cancer Pain ManagementDocument9 pagesUnequal Quality in Cancer Pain Managementapi-244230664No ratings yet
- Cancers: New Developments in The Pathogenesis, Therapeutic Targeting, and Treatment of Pediatric MedulloblastomaDocument15 pagesCancers: New Developments in The Pathogenesis, Therapeutic Targeting, and Treatment of Pediatric MedulloblastomaSebastian SalvadorNo ratings yet
- Descriptive EpidemiologyDocument7 pagesDescriptive EpidemiologyVineeta JoseNo ratings yet
- Final Project Work of English: Topic: Breast CancerDocument8 pagesFinal Project Work of English: Topic: Breast CancerLeidy AguileraNo ratings yet
- Melanocytic Lesions: A Case Based ApproachFrom EverandMelanocytic Lesions: A Case Based ApproachMai P. HoangNo ratings yet
- Epidemiology of Leprosy. in Book - Textbook of Clinical Leprosy Chapter 1.1 ITL - 1 - 1FINALDocument29 pagesEpidemiology of Leprosy. in Book - Textbook of Clinical Leprosy Chapter 1.1 ITL - 1 - 1FINALNaeNo ratings yet
- Evaluation of Neck MassDocument17 pagesEvaluation of Neck MassMuammar Aqib MuftiNo ratings yet
- Basal Cell CarcinomaDocument20 pagesBasal Cell CarcinomaJordan CoronadoNo ratings yet
- Nursing Care of Black AdultsDocument65 pagesNursing Care of Black AdultsSherilNo ratings yet
- Dematos 1997Document6 pagesDematos 1997Ali AmokraneNo ratings yet
- Uses of EpidemiologyDocument28 pagesUses of EpidemiologyBinita Shakya0% (1)
- Case Report: Xanthoma Disseminatum With Tumor-Like Lesion On FaceDocument5 pagesCase Report: Xanthoma Disseminatum With Tumor-Like Lesion On FaceAgus SyaifudinNo ratings yet
- The Pathomorphology of Bartholin's Gland. Analysis of Surgical DataDocument5 pagesThe Pathomorphology of Bartholin's Gland. Analysis of Surgical DataYuliana Eka SintaNo ratings yet
- Journal Reading SEMIFIDocument3 pagesJournal Reading SEMIFIJanNo ratings yet
- Final Case StudyDocument13 pagesFinal Case StudyJen Gacula OsinNo ratings yet
- Types of Business OwnershipDocument2 pagesTypes of Business Ownershipprelovedseller bnNo ratings yet
- Reclaimer Inspection ReportDocument51 pagesReclaimer Inspection ReportThiru Malpathi100% (1)
- WAUZZZ8K0BA159120Document10 pagesWAUZZZ8K0BA159120Vedad VedaddNo ratings yet
- Streptococcus Pneumoniae Staphylococci Faculty: Dr. Alvin FoxDocument32 pagesStreptococcus Pneumoniae Staphylococci Faculty: Dr. Alvin Foxdanish sultan100% (1)
- Moody's Financial Metrics 2007Document35 pagesMoody's Financial Metrics 2007Adrian IlieNo ratings yet
- New-DLP Phase2 Assignment-3 Module-B Final-9.8.18Document6 pagesNew-DLP Phase2 Assignment-3 Module-B Final-9.8.18PNo ratings yet
- Teoria Do Campo Ligante - Part IIDocument25 pagesTeoria Do Campo Ligante - Part IIArthurGrafdeSousaNo ratings yet
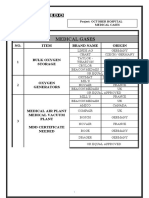
- Medical Gases: NO. Item Brand Name OriginDocument4 pagesMedical Gases: NO. Item Brand Name OriginMahmoud AnwerNo ratings yet
- Baseline Capacity Assessment For OVC Grantee CSOsDocument49 pagesBaseline Capacity Assessment For OVC Grantee CSOsShahid NadeemNo ratings yet
- Pipe TobaccoDocument6 pagesPipe TobaccoVictorIoncuNo ratings yet
- Neurology and Special Senses: High-Yield SystemsDocument72 pagesNeurology and Special Senses: High-Yield SystemsMahmoud Abu MayalehNo ratings yet
- Impact of Odor From A Landfill Site On Surrounding Areas: A Case Study in Ho Chi Minh City, VietnamDocument11 pagesImpact of Odor From A Landfill Site On Surrounding Areas: A Case Study in Ho Chi Minh City, VietnamNgọc HảiNo ratings yet
- Wetted Wall Gas AbsorptionDocument9 pagesWetted Wall Gas AbsorptionSiraj AL sharifNo ratings yet
- AAA V Edgardo SalazarDocument2 pagesAAA V Edgardo SalazarNiajhan PalattaoNo ratings yet
- Technical Reference For Water Conservation in Cooling TowersDocument41 pagesTechnical Reference For Water Conservation in Cooling TowersDorn GalamarNo ratings yet
- People v. Jerry BugnaDocument1 pagePeople v. Jerry BugnaRey Malvin SG PallominaNo ratings yet
- From Crème Fraîche To Sour Cream: What's The Difference?Document14 pagesFrom Crème Fraîche To Sour Cream: What's The Difference?Maricel BautistaNo ratings yet
- ComFlor 80 Load Span Tables PDFDocument4 pagesComFlor 80 Load Span Tables PDFAkhil VNNo ratings yet
- Trash Chute-Compliance Sheet Sangir)Document5 pagesTrash Chute-Compliance Sheet Sangir)Li LiuNo ratings yet
- Les Essences D'amelie BrochureDocument8 pagesLes Essences D'amelie BrochuresayonarasNo ratings yet
- JAMB Biology Past Questions 1983 - 2004Document55 pagesJAMB Biology Past Questions 1983 - 2004Keith MooreNo ratings yet
- Msds M-Toluoyl ChlorideDocument4 pagesMsds M-Toluoyl ChloridecrisNo ratings yet
- SM Electrical Guidelines: General Notes:: Site HereDocument1 pageSM Electrical Guidelines: General Notes:: Site HereNathaniel DreuNo ratings yet
- Urie BronfenbrennerDocument27 pagesUrie Bronfenbrennerapi-300862520100% (1)
- Pediatric Medication Dosing GuildelinesDocument2 pagesPediatric Medication Dosing GuildelinesMuhammad ZeeshanNo ratings yet
- X FEDEX EIDocument13 pagesX FEDEX EINISREEN WAYANo ratings yet