Professional Documents
Culture Documents
Elaine Gabovitch - The Healthy People 2020 Roadmap For Massachusetts Children & Youth With ASD/DD: Understanding Needs and Measuring Outcomes
Uploaded by
AUCDOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Elaine Gabovitch - The Healthy People 2020 Roadmap For Massachusetts Children & Youth With ASD/DD: Understanding Needs and Measuring Outcomes
Uploaded by
AUCDCopyright:
Available Formats
The Healthy People 2020 Roadmap for Massachusetts Children & Youth with ASD/DD
Understanding Needs and Measuring Outcomes
Elaine Gabovitch, MPA, Courtney Dutra, MPA & Emily Lauer, MPH
University of Massachusetts-Eunice Kennedy Shriver Center
Wait Time Survey
Background:
The Massachusetts Autism Commission 2012 report identified a critical
need to develop a comprehensive statewide approach to respond to the
needs of the rapidly increasing population of people with autism spectrum
disorder and developmental disabilities (ASD/DD). In response, the
UMMS-Shriver Center has been conducting a needs assessment to inform
efforts to establish a state-level data collection and surveillance plan for
systems of services for children and youth with ASD/DD.
Insurance Utilization
2 to 12 mos.
(median 5 mos.)
>1 to 6 mos.
(median 3 mos.)
>1 to over 12 mos.
>1 to 6 mos.
(median 2 mos.)
(median 3 mos.)
Methods:
>1 to 9 mos.
The projects objectives are to:
(1) Assess state needs of children with ASD and DD that align with six
MCHB core indicators (i.e., early identification, medical home, access
to community-based systems of care, family involvement, transition to
adulthood, and insurance);
(2) Make recommendations to refine the existing Massachusetts Autism
Commission plan and address identified needs; and
(3) Outline an ongoing surveillance strategy to monitor and report on
future state ASD/DD outcomes.
This project has focused on understanding several factors including race,
culture, language, region, level of function, and mental health.
(median 3 mos.)
Top reasons late
referral:
% non-English
speaking patients:
I have access to:
Results
Early Identification
Trends in ASD by age 36 months and identified characteristics
associated with early diagnoses in MA (Manning et al, 2011):
Rate of early diagnoses: Increased 66% from 2001 - 2005
Incidence: 1 in 178 (2001); 1 in 108 (2005); 1 in 85 (2013); 1 in 78
(2015)
Average age of diagnosis for children in EI: 2.56 years old
Cultural/linguistic gap:
Infants of mothers whose primary language was not English or were
foreign-born had lower odds of an early ASD diagnosis
May reflect groups with greater barriers to early screening
Shrinking racial gap:
2001: lower rates of early ASD diagnoses in racial minorities
2005: racial differences substantially lessened.
Suggests screening improved among racial minorities
Diagnosis and treatment of ASD (ABA, speech, etc.); no $ limit, no age limit
Habilitative, rehabilitative, pharmacy, psychiatric, psychological, therapeutic
MassHealth in the process of expanding coverage (<21)
ERISA plans federally regulated and exempt from state law
UMMS-Shriver Autism Insurance Resource Center assists families and
providers with information on insurance coverage in MA (3,000+ contacts)
Home & Community-based Waiver expansion for children with ASD & ID
Accessible community-based service system
Preliminary Findings:
Although Massachusetts is a resource rich state, through a review of
secondary data analysis, key informant interviews, focus groups, and
surveys, the needs assessment has identified certain gaps in services and
coverage. Selected findings are shared here, though much more exists.
Universal healthcare (2006)
96% insured/4% uninsured; however pockets (immigrants, minorities) of
uninsured with sharp contrasts between socio-economic areas
(e.g., East Boston: 23.7%; New Bedford: 22.1%; 10 affluent census tracts in MA: 0%)
Autism-specific coverage:
ARICA law (2011) applies to private, state-regulated plans
I do not have access
to language services:
What do you do
when patients family
does not speak
English?
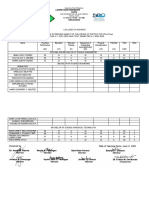
DBP Clinics (n=26)
Pediatricians (n=106)
Parents unaware of
milestones/red flags (77%)
Primary language not English
(59%)
Limited caregiver ability (55%)
Lower SES (44%)
<25% = 81%
25-50% = 12%
51-75% = 4%
Interpreters
= 58%
Translators
= 23%
Cultural liaisons
= 15%
Bilingual providers = 15%
35%
Parents unaware of
milestones/red flags (88%)
Primary language not English
(61%)
Limited caregiver ability (62%)
Lower SES (60%)
<20% = 61%
21-50% = 24%
51-80% = 13%
Interpreters
= 93%
Translators
= n/a
Cultural liaisons = 9%
Bilingual providers = 40%
N/A
Re: Evaluation:
Use translated measure (23%)
Perform w/ interpretation
(62%)
Do not evaluate (35%)
Re: Screening:
Use translated measure (45%)
Perform w/ interpretation
(70%)
Do not screen (20%)
My biggest concern is
the vast difference
money makes. For low
income families, so few
providers take
MassHealth.
In our programs, 50% of
people referred to local
medical centers for an Autism
evaluation dont show up.
With the use of family
navigators, that number
increases to 90%.
In Their
Own Words
The biggest problem is
that the folks doing
transition for your child
have no idea what adult
services look likeAnd
so folks dont really know
what they are going to
get.
80% of the IEPs I
read appear to have
been translated by
Google Translate. The
translation is not very
good or very clear.
We see a lot of homeless
families and they are just
trying to get by. They need
the diagnosis, but where they
are living is horrendous. But
they need that outreach to
prioritize the services they
need.
Psychotropic Medication use
MassHealth recently instituted prior authorization rules for children, based
on recent GAO report, e.g. inter- and intra-class polypharmacy
At least 1/3 children with flagged prescription profiles had utilization claims
with ASD diagnoses
Challenges with coordination of care; talks on strategies with MA Childrens
Behavioral Health Initiative
Transition to Adult Health Care
Transition to Adult Health Care
(NS-CSHCN, 2010)
MA % or #
U.S. % or #
YSHCN who received services to transition
Hispanic
Black, non-Hispanic
Other, non-Hispanic
White, non-Hispanic
47%
35%
20%
35%
51%
40%
25%
28%
40%
46%
Discussion
Through a triangulated data review to examine state strengths and needs in
the six Healthy People 2020 core indicator areas of early identification,
medical home, access to community-based systems, family involvement,
insurance and transition, preliminary findings indicate that while
Massachusetts has done well in such areas as lowering the average age of
identification, instituting universal insurance coverage, and offering resources
and services that support children and youth with ASD/DD and their families,
its challenges now lie in addressing barriers by region, socio-economics,
mental health, and culture, race and language. Old data systems need
updating. Providers may not take Medicaid. Essential therapies like ABA
need more therapists. Access to the All Payer Claims Database, which has just
released its 3.0 version, is needed to better understand healthcare access and
outcomes. The future will lie in sharing our findings with the Commission and
diverse communities to work on the most meaningful solutions together.
Funding: Health Resources & Services Administration-Maternal & Child Health Bureau
You might also like
- Statewide Collaboration To Educate On Developmental and Behavioral Monitoring and ScreeningDocument1 pageStatewide Collaboration To Educate On Developmental and Behavioral Monitoring and ScreeningAUCDNo ratings yet
- The Development and Utility of The Family-Centered Autism Navigation (Family CAN) Semi-Structured InterviewDocument1 pageThe Development and Utility of The Family-Centered Autism Navigation (Family CAN) Semi-Structured InterviewAUCDNo ratings yet
- The Autism Friendly Initiative at Boston Medical Center: Improving The Hospital Experience For Patients With AutismDocument41 pagesThe Autism Friendly Initiative at Boston Medical Center: Improving The Hospital Experience For Patients With AutismAUCDNo ratings yet
- Delaware's Autism Care Team: Autism CARES Meeting July 2019Document66 pagesDelaware's Autism Care Team: Autism CARES Meeting July 2019AUCDNo ratings yet
- Detecting Autism Early - A Pilot To Train Providers, Screen Toddlers, and Support Families With Autism Concerns in Primary CareDocument41 pagesDetecting Autism Early - A Pilot To Train Providers, Screen Toddlers, and Support Families With Autism Concerns in Primary CareAUCDNo ratings yet
- Access To Autism Information and Services in Wisconsin Is Enhanced by LEND Collaboration With State System InitiativeDocument1 pageAccess To Autism Information and Services in Wisconsin Is Enhanced by LEND Collaboration With State System InitiativeAUCDNo ratings yet
- Increasing Access To Autism Spectrum Disorder Assessment Services For Children Under Three Through Part C ClinicsDocument32 pagesIncreasing Access To Autism Spectrum Disorder Assessment Services For Children Under Three Through Part C ClinicsAUCDNo ratings yet
- Test 71 02Document57 pagesTest 71 02AUCDNo ratings yet
- Human-Centered Design For Community-Centered CollaborationDocument17 pagesHuman-Centered Design For Community-Centered CollaborationAUCDNo ratings yet
- "And I Will Tell You This": Single, Black Mothers of Children With ASD/DD Using Cultural Capital in Special EducationDocument20 pages"And I Will Tell You This": Single, Black Mothers of Children With ASD/DD Using Cultural Capital in Special EducationAUCDNo ratings yet
- Evidence For The Use of Age-Based Diagnostic Tracks in Interdisciplinary Team Evaluation For Autism Spectrum DisorderDocument23 pagesEvidence For The Use of Age-Based Diagnostic Tracks in Interdisciplinary Team Evaluation For Autism Spectrum DisorderAUCDNo ratings yet
- Addressing Access and Reach: Implementation of A Group CBT Intervention For Managing Anxiety in Students With ASD in Urban SchoolsDocument36 pagesAddressing Access and Reach: Implementation of A Group CBT Intervention For Managing Anxiety in Students With ASD in Urban SchoolsAUCD0% (1)
- Digital Media Exposure in Young Children With Disabilities, A Population Based SurveyDocument1 pageDigital Media Exposure in Young Children With Disabilities, A Population Based SurveyAUCDNo ratings yet
- Preliminary Validation of The PROMIS® Pediatric Parent-Proxy Anxiety Measure in Children With Autism Spectrum DisorderDocument1 pagePreliminary Validation of The PROMIS® Pediatric Parent-Proxy Anxiety Measure in Children With Autism Spectrum DisorderAUCDNo ratings yet
- Building A Network of Community Leaders To Support Early Developmental Screening: Minnesota Act Early Delegate Network in Diverse Cultural CommunitiesDocument1 pageBuilding A Network of Community Leaders To Support Early Developmental Screening: Minnesota Act Early Delegate Network in Diverse Cultural CommunitiesAUCDNo ratings yet
- Autism Intervention Research Network On Physical Health (AIR-P) Addressing DisparitiesDocument1 pageAutism Intervention Research Network On Physical Health (AIR-P) Addressing DisparitiesAUCDNo ratings yet
- Autism Spectrum Disorder Prevalence in Diverse Communities in MinnesotaDocument1 pageAutism Spectrum Disorder Prevalence in Diverse Communities in MinnesotaAUCDNo ratings yet
- AUTISM 101: A Psychoeducational Intervention For Parents of Newly Diagnosed Children With Autism Spectrum DisorderDocument1 pageAUTISM 101: A Psychoeducational Intervention For Parents of Newly Diagnosed Children With Autism Spectrum DisorderAUCDNo ratings yet
- Association Between Food Insecurity and Developmental Delay and Behavioral Problems in US Children 2-5 Years of AgeDocument1 pageAssociation Between Food Insecurity and Developmental Delay and Behavioral Problems in US Children 2-5 Years of AgeAUCDNo ratings yet
- HRSA MCHB-Funded Autism CARES Programs Promote Equity and Increased Access To CareDocument1 pageHRSA MCHB-Funded Autism CARES Programs Promote Equity and Increased Access To CareAUCDNo ratings yet
- Strengthening Diversity in The Alaska LEND Program: Engaging Faculty From Rural AlaskaDocument1 pageStrengthening Diversity in The Alaska LEND Program: Engaging Faculty From Rural AlaskaAUCDNo ratings yet
- The National Autism Data Center at Drexel University: Population-Level Data To Inform PolicyDocument1 pageThe National Autism Data Center at Drexel University: Population-Level Data To Inform PolicyAUCDNo ratings yet
- Psychotropic Medication Use in Youth With Autism and Attention-Deficit/Hyperactivity DisorderDocument1 pagePsychotropic Medication Use in Youth With Autism and Attention-Deficit/Hyperactivity DisorderAUCDNo ratings yet
- Susan M. Russell, M.S. and Betsy P. Humphreys, Ph.D. SuccessesDocument1 pageSusan M. Russell, M.S. and Betsy P. Humphreys, Ph.D. SuccessesAUCDNo ratings yet
- The Influence of Race and Ethnicity On Vocational Rehabilitation Service Utilization and Outcomes of Transition-Age Young Adults With AutismDocument1 pageThe Influence of Race and Ethnicity On Vocational Rehabilitation Service Utilization and Outcomes of Transition-Age Young Adults With AutismAUCDNo ratings yet
- A Multi-Site Randomized Control Trial of Family Navigation's Effect On Diagnostic Ascertainment Among Children at Risk For Autism: A DBPNet StudyDocument1 pageA Multi-Site Randomized Control Trial of Family Navigation's Effect On Diagnostic Ascertainment Among Children at Risk For Autism: A DBPNet StudyAUCDNo ratings yet
- LEND Training in A Developmental-Behavioral Advanced Practice Nursing Fellowship: Increasing Access To Evaluation and Follow UpDocument1 pageLEND Training in A Developmental-Behavioral Advanced Practice Nursing Fellowship: Increasing Access To Evaluation and Follow UpAUCDNo ratings yet
- Community-Partnered Participatory Research in Autism: Engaging Underresourced African American, Korean and Latino CommunitiesDocument1 pageCommunity-Partnered Participatory Research in Autism: Engaging Underresourced African American, Korean and Latino CommunitiesAUCDNo ratings yet
- Diagnosis of Autism in An Ethnical Diverse, Community Sample: Who Refers and Why?Document1 pageDiagnosis of Autism in An Ethnical Diverse, Community Sample: Who Refers and Why?AUCDNo ratings yet
- Screening of Young Children For Autism Spectrum Disorders: Results From A National Survey of PediatriciansDocument1 pageScreening of Young Children For Autism Spectrum Disorders: Results From A National Survey of PediatriciansAUCDNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Nishan Singh's Education and Career ProfileDocument2 pagesNishan Singh's Education and Career Profileshahid aliNo ratings yet
- Graphic Design - Brochure 2021Document4 pagesGraphic Design - Brochure 2021Siddharth KhuranaNo ratings yet
- The Effect of Peer Pressure To The Grade 10 Students of Colegio San Agustin Makati 2018-2019 That Will Be Choosing Their Respective Strands in The Year 2019-2020Document5 pagesThe Effect of Peer Pressure To The Grade 10 Students of Colegio San Agustin Makati 2018-2019 That Will Be Choosing Their Respective Strands in The Year 2019-2020Lauren SilvinoNo ratings yet
- Hang Out 5 - Unit Test 8Document2 pagesHang Out 5 - Unit Test 8Neila MolinaNo ratings yet
- Jenifer Romualdo Lee ResumeDocument2 pagesJenifer Romualdo Lee ResumeLorilla AlvinNo ratings yet
- Describing Colleagues American English Pre Intermediate GroupDocument2 pagesDescribing Colleagues American English Pre Intermediate GroupJuliana AlzateNo ratings yet
- First Quarter Exam in Reading and Writing SkillsDocument3 pagesFirst Quarter Exam in Reading and Writing SkillsCamille Wu50% (4)
- 4037 w17 Ms 22Document8 pages4037 w17 Ms 22arcanum78No ratings yet
- Unit 1 Vocab. ReadingDocument4 pagesUnit 1 Vocab. ReadingNhật KiênNo ratings yet
- Naval Leadership PrinciplesDocument2 pagesNaval Leadership Principlesdjnet1No ratings yet
- Group CohesivenessDocument26 pagesGroup CohesivenessRaviWadhawanNo ratings yet
- 2023eju Bulletin enDocument35 pages2023eju Bulletin enpokemoknaNo ratings yet
- HIC Partner University DiscountDocument3 pagesHIC Partner University DiscountEzekiel ChoosenNo ratings yet
- Trigonometric Ratios: Find The Value of Each Trigonometric RatioDocument2 pagesTrigonometric Ratios: Find The Value of Each Trigonometric RatioRandom EmailNo ratings yet
- Fasil Andargie Fenta: LecturerDocument2 pagesFasil Andargie Fenta: Lecturerfasil AndargieNo ratings yet
- Faculty Screening J.ODocument2 pagesFaculty Screening J.OIvy CalladaNo ratings yet
- ELECTIVE MATHEMATICS 10 Module Equation of Circle Part 1Document17 pagesELECTIVE MATHEMATICS 10 Module Equation of Circle Part 1Rosuel Aslie ValeNo ratings yet
- Characteristics of Informational TextDocument2 pagesCharacteristics of Informational TextEdwin Trinidad100% (1)
- Zero, First, and Second Conditional SentencesDocument2 pagesZero, First, and Second Conditional SentencesAtzi EspinosaNo ratings yet
- Safe Spaces Act Narrative ReportDocument2 pagesSafe Spaces Act Narrative ReportLian CarrieNo ratings yet
- Veena Kumawat CVDocument1 pageVeena Kumawat CVVeena KumavatNo ratings yet
- Importance of Active ListeningDocument13 pagesImportance of Active ListeningJane Limsan PaglinawanNo ratings yet
- PMP Training 7 2010Document5 pagesPMP Training 7 2010srsakerNo ratings yet
- AssessmentDocument36 pagesAssessmentapi-344737952100% (1)
- Cbse Completed 31TO60AND95TO104Document33 pagesCbse Completed 31TO60AND95TO104tt0% (1)
- Biol 3833 Fa 18Document7 pagesBiol 3833 Fa 18api-263358650No ratings yet
- Cspu 620 Fieldwork Hours Log - Summary SheetDocument2 pagesCspu 620 Fieldwork Hours Log - Summary Sheetapi-553045669No ratings yet
- Architecture Literature Review SampleDocument7 pagesArchitecture Literature Review Samplec5pnw26s100% (1)
- Letterhead Doc in Bright Blue Bright Purple Classic Professional StyleDocument2 pagesLetterhead Doc in Bright Blue Bright Purple Classic Professional StyleKriszzia Janilla ArriesgadoNo ratings yet
- Results of 2011 SMOPS (For Webpage)Document14 pagesResults of 2011 SMOPS (For Webpage)Thích Toán HọcNo ratings yet