Professional Documents
Culture Documents
Neuron-Specific Enolase As A Marker of The Severity and Outcome of Hypoxic Ischemic Encephalopathy
Uploaded by
Agus WijataOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Neuron-Specific Enolase As A Marker of The Severity and Outcome of Hypoxic Ischemic Encephalopathy
Uploaded by
Agus WijataCopyright:
Available Formats
Brain & Development 26 (2004) 398402
www.elsevier.com/locate/braindev
Original article
Neuron-specific enolase as a marker of the severity and outcome
of hypoxic ischemic encephalopathy
ner, O
zer Pala
Coskun Celtik*, Betul Acunas, Naci O
Department of Pediatrics, Trakya University Faculty of Medicine, Edirne, Turkey
Received 7 April 2003; received in revised form 24 December 2003; accepted 24 December 2003
Abstract
The aim of this study was to evaluate serum concentrations of neuron-specific enolase (NSE) as a marker of the severity of hypoxic
ischemic encephalopathy (HIE) and to elucidate the relation among the concentrations of NSE, grade of HIE and short-term outcome. Fortythree asphyxiated full-term newborn infants who developed symptoms and signs of HIE (Group 1) and 29 full-term newborn infants with
meconium-stained amniotic fluid but with normal physical examination (Group 2) were studied with serial neurological examination, Denver
developmental screening test (DDST), electroencephalogram and computerized cerebral tomography (CT) for neurological follow-up. Thirty
healthy infants were selected as the control group. In the patient groups, two blood samples were taken to measure NSE levels, one between 4
and 48 h and the other 5 7 days after birth. Serum NSE levels were significantly higher in infants with HIE compared to those infants in
Group 2 and control group. The mean serum concentrations of the second samples decreased in all groups studied but they were significantly
higher in Group 1 compared to those in Group 2. Serum NSE concentrations of initial samples were significantly higher in patients with stage
III HIE than in those with stages II and I. The sensitivity and specificity values of serum NSE as a predictor of HIE of moderate or severe
degree (cut-off value 40.0 mg/l) were 79 and 70%, respectively, and as a predictor of poor outcome (cut-off value 45.4 mg/l) were calculated
as 84 and 70%, respectively. The predictive capacity of serum NSE concentrations for poor outcome seems to be better than predicting HIE
of moderate or severe degree. However, earlier and/or CSF samples may be required to establish serum NSE as an early marker for the
application of neuroprotective strategies.
q 2004 Elsevier B.V. All rights reserved.
Keywords: Neuron-specific enolase; Perinatal asphyxia; Hypoxic ischemic encephalopathy; Short-term outcome
1. Introduction
Despite advances in medical and technological possibilities, perinatal asphyxia is still a matter of concern due to its
considerably high rate of mortality and morbidity [1,2].
Hypoxic ischemic encephalopathy (HIE) after perinatal
asphyxia is a condition in which cerebrospinal fluid (CSF)
and/or serum concentrations of brain-specific biochemical
markers may be elevated [3 7]. Recent development of
neuroprotective strategies emphasize the need for early and
objective indicators for both diagnosis and outcome of HIE
and studies about biochemical markers may aid neuroprotective studies [8].
niversitesi Tp Fakultesi,
* Corresponding author. Address: Trakya U
Cocuk Saglg ve Hastalklar Anabilim Dal, 22030 Edirne, Turkey. Tel.:
90-284-235-7641; fax: 90-284-235-2338.
E-mail address: cceltik2001@yahoo.com (C. C
eltik).
0387-7604/$ - see front matter q 2004 Elsevier B.V. All rights reserved.
doi:10.1016/j.braindev.2003.12.007
Of those brain-specific proteins, the brain-derived
creatinine kinase (CK-BB), the highly soluble glial protein
S-100, glial fibrillary acidic protein (GFAp), neurofilament
protein (NFp) and the neuron-specific enolase (NSE) have
been found to be released in high concentrations into the
CSF of asphyxiated infants and correlated significantly with
other indicators of long-term prognosis and neurological
impairment at 1 year of age or death [4]. NSE, a dimeric
glycolytic enzyme, containing two gamma subunits,
originates predominantly from the cytoplasm of neurons
and neuroendocrine cells. It is soluble and stable in
biological fluids and its determination is not affected by
hyperbilirubinemia or lipemia. Furthermore it does not elicit
immunological cross-reactivity with non-neuronal enolase
[3 7]. Serum levels of NSE increase in neuroendocrine cell
tumours, medulloblastoma, retinoblastoma, neuroblastoma,
seminoma, small cell cancer of lung, brain hypoxia after
C. Celtik et al. / Brain & Development 26 (2004) 398402
myocardial infarction, cell damage associated with central
and peripheral nervous system as stroke, subarachnoidal
haemorrhage, traumatic brain damage, Guillian Barre
syndrome, bacterial meningitis and encephalitis. NSE has
been established both as a useful and reliable marker of
neuronal damage and prognosis in these various neurological disorders [9 15]. On the other hand there are few
studies about its value in the diagnosis and prognosis of HIE
following perinatal asphyxia most of which have used CSF
values of NSE as an indicator of neurological impairment
[3 7]. However, it is important to have a sufficiently
sensitive marker for brain damage that can be determined in
blood instead of CSF, because blood samples can be taken
more easily and frequently and more independently of
raised intracranial pressure than CSF samples and can be
performed in all conditions even in haemorrhagic diathesis
associated with severe asphyxia.
The aim of this study was to evaluate serum concentrations of NSE as a marker of the severity of HIE and to
elucidate the relation between the concentrations of NSE
and grade of HIE in relation to short-term outcome.
2. Material and methods
The patient group comprised of 43 asphyxiated full-term
newborn infants who developed symptoms and signs of HIE
according to Sarnat and Sarnat [2] and treated at Neonatal
Intensive Care Unit of Trakya University Hospital
(Group 1). Infants were designated as having asphyxia if
they fulfilled the following criteria.
(1) Intrapartum distress indicated by the cardiotocograph
pattern (late decelerations, absence of variability,
persistent bradycardia, etc.) and/or abnormal blood
flow pattern (loss or reversal of end-diastolic velocity)
and/or early passage of thick meconium,
(2) Requirement for resuscitation with positive pressure
ventilation and laryngeal intubation,
(3) Low Apgar score (1st min # 3, 5th min , 6) or
umbilical arterial/first postnatal (pH , 7.1).
Twenty-nine full-term infants with meconium-stained
amniotic fluid but with normal physical examination comprised Group 2. Thirty healthy newborn infants who were
born after spontaneous vaginal delivery with normal physical
findings were included as the control group. Infants with
severe congenital abnormalities, profound anaemia, and history of multiple pregnancies were excluded from the study.
Gender gestational age, mode of delivery, birth weight,
weight for gestational age, Apgar scores at 1st and 5th min,
if present the stage of HIE [mid HIE (stage I), moderate HIE
(stage II) and severe HIE (stage III)] [2], neurological
disabilities of survivors were recorded.
In Group 1, neurological examination was performed
everyday during the hospitalization period, and 1 week, 3, 6
399
and 12 months after discharge. Electroencephalographic
(EEG) and computerized tomography examinations (CT) of
the brain were performed at 1 month and 12 months of age
in all patients in Group 1. During the first year of life, every
month, Denver Developmental Screening Test II (DDST)
adapted for Turkish children [16] was performed in Group 1.
Physical examination and DDST were performed in all
patients in Group 2 and control group at 1 month of age and
repeated every 3 months. Patients were examined by the
same neonatologist (BA) and DDST was performed by
paediatric neurodevelopmental specialist.
Poor outcome was overall determined after 1 year of
delivery. It was defined as death due to HIE or presence of
abnormal neurological findings, that is, abnormalities in
muscular tonus, uncoordinated or absent sucking and
swallowing, the presence of major disabilities such as
spasticity, seizure, hearing loss or neurodevelopmental
delay supported by either persistently abnormal EEG
findings or DDST and/or CT results. EEG findings such as
voltage suppression, burst suppression, isoelectric tracing,
diffuse paroxysmal activity or localized periodic epileptiform discharge, the existence of diffuse hypoxic hypodense
areas and related findings on the brain CT imaging were
accepted as signs of poor prognosis. Besides a child was
identified as having poor outcome by DDST when delays in
development significantly challenged the child in two or
more of the following four developmental areas: personal
social, fine motor adaptive, language, and gross motor.
Normal or good outcome was defined as the absence of
those disabilities mentioned above.
Informed parental consent was obtained for all infants
before the collection of blood samples.
In the patient groups, two blood samples were taken to
measure NSE levels, one between 4 and 48 h (except in one
case at 52 h of age) and the other, between 5 and 7 days after
birth. The blood samples were taken at similar time periods
from all groups. Only one sample has been taken from those
in the control group and those who were lost during followup or died. All blood samples were immediately frozen
(2 70 8C) and haemolysed samples were discarded to
prevent false high value of NSE.
Serum NSE concentrations were measured using the
NSE radioimmunossay kit (Pharmacia AB, Uppsala,
Sweden) and according to the manufacturers instructions.
The method measures concentrations in the range of
2 200 mg/l; the detection limit is less than 2 mg/l.
2.1. Statistics
All values were presented as mean and SD. The
distribution of serum NSE concentrations were assessed
by Kolmogorov Smirnov and Shapiro Wilk tests. x 2 -test
was used to compare gender, place of birth (inborn/outborn), mode or delivery. For comparing three groups in
terms of birth weight and gestational ages which were
parametric data, analysis of variance (ANOVA) test, and to
400
C. C
eltik et al. / Brain & Development 26 (2004) 398402
compare Apgar scores, NSE1 and NSE2 levels which were
non-parametric data, Kruskal Wallis test was used. Kruskal Wallis test was also used to compare HIE subgroups in
terms of serum NSE concentrations. The significance of
differences between groups was analysed by post hoc Tukey
HSD test and Mann Whitney U-test. The specificity,
sensitivity, positive and negative predictive values of NSE
levels in determining diagnosis and prognosis of HIE were
obtained using optimal cut-off levels and were calculated on
the material used in this study. Receiver operating
characteristics (ROC) curves were assessed using the
areas under the curves as indexes of performance. For
statistical analysis Minitab Release 13 (license number: wep
1331.00197) for Windows was used. P , 0:05 was
considered as statistically significant.
3. Results
The demographic data of all groups are shown in Table 1.
There were no differences between patient and control
groups in terms of gestational age, birth weight, gender and
mode of delivery. More patients in Group 1 were outborn
ones (P , 0:05; Group 1 vs Group 2 and control group).
The first and fifth minute Apgar scores of patients in Group 1
were significantly lower than those in Group 2 and the
control group (P , 0:001; Group 1 vs Group 2 and control
group). Eighteen infants in Group 1 (14%) had meconiumstained amniotic fluid. Fourteen patients in the HIE group
were classified as in stage I, 19 as in stage II, 10 as in
stage III. While no morbidity and mortality had been
observed in Group 2 and the control group, 8 patients died
(2 in stage II HIE group and 6 in stage III HIE group; for this
reason second blood samples of these patients are lacking)
and 11 patients were observed to have poor outcome in
Group 1 after 1 year of follow-up. The mean first blood
sampling time was 20 ^ 14 (4 52) h for Group 1; 14 ^ 12
(4 48) h for Group 2; 15 ^ 7 (4 26) h for control group.
The mean second blood sampling time was 6.5 ^ 0.7 and
6.6 ^ 0.9 d for Groups 1 and 2, respectively. There were no
Table 2
Serum concentrations of NSE at different sampling times (NSE1, NSE2) in
the two patient groups and the control group and according to the stage of
HIE
Group
NSE1 (mg/l)
NSE2 (mg/l)
Group 1, stage I HIE n 14
Group 1, stage II HIE n 19
Group 1, stage III HIE n 10
Group 2 n 18
Control group n 30
65.3 ^ 32.4a
64.6 ^ 32.9a
115.7 ^ 60.9a
42.0 ^ 24.00c
21.0 ^ 5.3c
34.6 ^ 13.9b
42.0 ^ 32.7b
70.8 ^ 36.9b
22.1 ^ 8.0
a
b
c
Pstage I vs III and Pstage II vs III , 0:05:
Pstage I vs III and Pstage I II , 0:05:
Pgroup1 vs 2 , 0:05; Pgroup1 vs control , 0:001:
significant differences among the groups in terms of first and
second blood sampling time. The second blood samples
were not taken from the controls.
There were significant differences between Group 1 and
Group 2 and controls in terms of serum NSE concentrations of the first blood samples (Pgroup 1 2 , 0:05;
Pgroup 1 control , 0:001).
Serum concentrations of NSE at different sampling times
(NSE1, NSE2) in the two patient groups and the control
group and according to the stage of HIE are shown in
Table 2. No significant difference was detectable in serum
NSE levels between Group 2 and the Control group. The
mean serum concentrations of the second samples decreased
in all groups studied, however, they were significantly
higher in Group 1 compared with Group 2 P , 0:05:
Serum NSE concentrations of the first blood samples
were significantly higher in patients with stage III HIE than
those with stage I and II HIE (Pstage I III and Pstage II III ,
0:05; Pstage I II , 0:05). Fig. 1 demonstrates the NSE
concentrations in relation to outcome (poor and normal).
Initial NSE levels were evaluated by ROC-curve analysis
in which sensitivity and specificity were calculated for
different cut-off values to distinguish the patients who
Table 1
Characteristics of the study groups and controls
Birth weight (g)
Gestational age (week)
Gender (M/F)
Inborns/outbornsa
Mode of delivery, CS/NSVDb
Apgar score (1 min)c
Apgar score (5 min)c
a
b
c
Group 1
n 43
Group 2
n 29
Control
n 30
3119 ^ 604
39.8 ^ 1.6
28/15
6/37
17/26
1.9 ^ 1.3
4.0 ^ 1.0
3218 ^ 559
39.6 ^ 0.9
16/13
27/2
15/14
6.9 ^ 1.7
8.7 ^ 0.8
3436 ^ 437
39.4 ^ 0.9
12/18
19/11
/30
8.2 ^ 0.4
9.3 ^ 0.5
P , 0:05; Group 1 vs Group 2 and control group.
CS, caesarean section; NSVD, normal spontaneous vaginal delivery.
P , 0:001; Group 1 vs Group 2 and control group.
Fig. 1. Serum concentrations of NSE
poor).
12
in relation to outcome (normal,
C. Celtik et al. / Brain & Development 26 (2004) 398402
401
positive and negative predictive values of serum NSE as a
predictor of HIE of moderate or severe degree were 79, 70,
51 and 89%, respectively, and as a predictor of poor
outcome were calculated as 84, 70, 39 and 95%,
respectively.
4. Discussion
Fig. 2. ROC curves for initial NSE (cut-off point 40.0) as a marker for
distinguishing infants with no or mild HIE from infants with moderate or
severe HIE.
developed HIE of moderate or severe degree from those
with no or mild HIE and those who had poor outcome from
those with good outcome. The cut-off values that maximized the sum of sensitivity plus specificity were 40.0 mg/l
for predictor of HIE and 45.4 mg/l for poor outcome (Figs. 2
and 3). By using these values the sensitivity, specificity,
Fig. 3. ROC curves for initial NSE (cut-off point 45.4) as marker for
distinguishing infants with poor outcome from infants with normal
outcome.
Clinical trials of neuronal rescue therapies need to select
those infants who are most likely to benefit from treatment
and to avoid exposing infants who have a good outcome to
potentially toxic therapies. Therefore, it is very important to
find an early and reliable indicator of the severity degree of
HIE and poor outcome to initiate or end neuroprotective
strategies. In this present study, we have demonstrated that
serum NSE concentrations of infants with stage III HIE
were significantly higher than those in stage I and II HIE.
Several studies measuring NSE and other biochemical
indices in serum and/or CSF of infants with HIE following
perinatal asphyxia showed almost similar results [3 6].
Garcia et al. [3] and Blennow et al. [4] reported higher CSF
NSE levels in newborn babies with grade-II and III HIE than
the ones with grade-I HIE and normal control subjects.
Thornberg et al. [5] found high NSE levels in two cases of
grade-II HIE patients and in all grade-III HIE patients. They
reported that all of these babies had severe neurological
impairment and NSE levels were correlated with cerebral
function. However, Nagdyman et al. [7] reported no
significant difference in serum NSE levels between infants
with no or mild and moderate or severe HIE, 2 and 6 h after
birth but there was a significant difference at 12 and 24 h
age. Yet, in the same study the sensitivity, specificity,
positive and negative predictive values of NSE in predicting
moderate or severe HIE (cut-off value 46 mg/l) were found
to be 83, 65, 42 and 93%, respectively [7], which is not so
different from our results (cut-off value 40.0 mg/l; 79, 70,
51, and 89%, respectively). Besides Nagdyman et al. [7] had
also reported sensitivity, specificity, positive and negative
predictive values at cut-off value 4.6 mg/l for protein S100
as 71, 86, 63, and 90%, and at cut-off value 17.0 U/L for
CK-BB as 86, 77, 55, and 94%, respectively [7], which are
almost similar to those belonging to NSE values obtained in
their study. There were also no clear differences between
ROC curves of different biochemical markers for perinatal
asphyxia.
Optimal blood sampling time for biochemical markers to
indicate neuronal damage is controversial. In different
studies associated with neuronal damage due to perinatal
aspyxia, sampling time shows great variance; in most of
these studies including ours, blood and/or CSF samples
were obtained mostly after 6 h of age; Garcia et al. [3]
obtained samples at 12 and 72 h of age; Thonberg et al. [5]:
between 2 and 64 h after birth, Nagdyman et al. [7] at 2, 6,
12 and 24 h after birth. In our study, the reason for this
delay was the high number of outborn patients especially in
402
C. C
eltik et al. / Brain & Development 26 (2004) 398402
the HIE group. Studies in perinatal animals suggest quick
cellular destruction after hypoxia and a steady decrease in
energy substrates of brain in 48 h [17,18]. Therefore
choosing sampling time as the first 48 h after birth seemed
suitable initially. On the other hand, animal studies indicate
that greater neuroprotection is obtained if hypothermia,
which is the most promising neuroprotective strategy
nowadays, is started soon after the hypoxic insult, possibly
within 6 h of birth [8]. Unfortunately, we could not obtain
blood samples earlier, which shadows the results of this
study. Earlier samples and/or NSE in cerebrospinal fluid can
be more favourable in predicting the severity of HIE and
poor outcome.
The preceding studies associated with NSE about
perinatal asphyxia mostly focused on early diagnosis of
HIE. However, there are few studies investigating the
relation of NSE and HIE outcome in the neonatal period
[3,6]. In this study, both the evaluation of NSE values for
early diagnosis of HIE and the role of NSE for prediction of
HIE outcome were researched and the sensitivity and
specificity of NSE in predicting poor outcome (at cut-off
value 45.4 mg/l: sensitivity 84%; specificity 70%; positive
predictive value 39%; negative predictive value 95%) were
found to be better than predictive values for severity degree
of HIE. Garcia et al. [3] noted that specificity and sensitivity
of initial NSE levels in the assessment of poor outcome, if
cut-off value was 25 ng/ml, were 86 and 90%, respectively.
On the other hand, Verdu Perez et al. [6] noted higher ratios
of sensitivity and specificity for blood NSE as a predictor of
poor outcome (100 and 78%, respectively).
In this study, although sensitivity and specificity rates of
NSE were found to be moderately high for the evaluation of
diagnosis and poor outcome of HIE, positive and negative
predictive values were relatively low. This can be a more
favourable condition if you consider the necessity of having
high sensitivity rate in order to identify those infants with
HIE due to perinatal asphyxia and initiate neuroprotective
therapies. On the other hand in order to prevent unnecessary
intensive follow-up, prediction of HIE outcome, specificity
and negative predictive values that differentiate healthy
infants becomes more important than sensitivity and
positive predictive values. From this point of view,
determination of serum NSE values may be considered as
a reliable assay for detecting and following up neonates with
HIE due to perinatal asphyxia.
In conclusion, the results of this study demonstrate that
the predictive capacity of serum NSE concentrations for
poor outcome seems to be better than predicting HIE of
moderate or severe degree. However, earlier and/or CSF
samples are required to establish serum NSE as an early
predictor for the application of neuroprotective strategies.
References
[1] Costello AM, Manandhar DS. Perinatal Asphyxia in less developed
countries. Arch Dis Child Fetal Neonatal Ed 1994;71:13.
[2] Sarnat HB, Sarnat MS. Neonatal encephalopathy following fetal
distress. Arch Neurol 1976;33:696705.
[3] Garcia-Alix A, Cabanas F, Pellicer A, Hernanz A, Stiris TA, Quero J.
Neuron specific enolase and myelin basic protein: relationship of
cerebrospinal fluid concentrations to the neurological condition of
asphyxiated full-term infants. Pediatrics 1994;93:234 40.
[4] Blennow M, Savman K, Ilves P, Thoresen M, Rosengren L. Brain
specific proteins in the cerebrospinal fluid of severely asphyxiated
newborn infants. Acta Pediatr 2001;90:11715.
[5] Thornberg E, Thiringer K, Hagberg H, Kjellmer I. Neuron specific
enolase in asphyxiated newborns: association with encephalopathy
and cerebral function monitor trace. Arch Dis Child Fetal Neonatal Ed
1995;72:3942.
[6] Verdu Perez A, Falero MP, Arroyos A, Estevez F, Felix V, Lopez Y,
et al. Blood neuroal specific enolase in newborns with perinatal
asphyxia. Rev Neurol 2001;32:7147.
[7] Nagdyman N, Komen W, Ko HK, Muller C, Obladen M. Early
biochemical indicators of hypoxic-ischemic encephalopathy after
birth asphyxia. Pediatr Res 2001;49(4):5026.
[8] Thoresen M. Cooling the newborn after asphyxia-physiological and
experimental background and its clinical use. Semin Neonatol 2000;5:
61 73.
[9] Schaarschmidt H, Prange HW, Reiber H. Neuron-specific enolase
concentrations in blood as a prognostic parameter in cerebrovascular
diseases. Stroke 1994;25:55865.
[10] Nara T, Nozaki H, Nakae Y, Arai T, Ohashi T. Neuron-specific
enolase in comatose children. Am J Dis Child 1988;142:1734.
[11] Cunningham RT, Morrow JI, Johnston CF, Buchanan KD. Serum
neuron-specific enolase concentrations in patients with neurological
disorders. Clin Chim Acta 1994;230:117 24.
[12] van Engelen BG, Lamers KJ, Gabreels FJ, Wevers RA, van Geel WJ,
Borm GF. Age-related changes of neuron-specific enolase, S-100
protein, and myelin basic protein concentrations in cerebrospinal
fluid. Clin Chem 1992;38(6):8136.
[13] Fogel W, Krieger D, Veith M, Adams H-P, Hund E, StorchHagenlocher B, et al. Serum neuron specific enolase as early predictor
of outcome after cardiac arrest. Crit Care Med 1997;25:11338.
[14] Mokuno K, Kiyosawa K, Sugimara K, Yasuda T, Riku S, Murayama
T, et al. Prognostic value of cerebrospinal fluid neuron specific
enolase and S-100b protein in GuillainBarre sydrome. Acta Neurol
Scand 1994;89:2730.
[15] Inoue S, Takahashi H, Kaneko K. The fluctuations of neuron-specific
enolase (NSE) levels of cerebrospinal fluid during bacterial
meningitis: the relationship between the fluctuations of NSE levels
and neurological or outcome. Acta Paediatr Jpn 1994;36:4858.
zturk C, Karagozoglu E, Anlar B. Turkish childrens
[16] Durmazlar N, O
performance on Denver II: effect of sex and mother education. Dev
Med Child Neurol 1998;40:4116.
[17] Vannucci RC, Perlman JM. Interventions for perinatal hypoxic
ischemic encephalopathy. Pediatrics 1997;100:100414.
[18] Lorek A, Takei Y, Cady EB, Wyatt JS, Penrice J, Edwards AD, et al.
Delayed (secondary) cerebral energy failure after acute hypoxiaischemia in the newborn piglet: continuous 48-h studies by
phosphorus magnetic resonance spectroscopy. Pediatr Res 1994;36:
699 706.
You might also like
- Cerebrospinal Fluid in Clinical NeurologyFrom EverandCerebrospinal Fluid in Clinical NeurologyFlorian DeisenhammerNo ratings yet
- The NORSE (New-Onset Refractory Status Epileptic Us) SyndromeDocument4 pagesThe NORSE (New-Onset Refractory Status Epileptic Us) Syndromebenghooi75No ratings yet
- Biochemical markers predict neonatal brain injuryDocument6 pagesBiochemical markers predict neonatal brain injuryrantiadrianiNo ratings yet
- Encephalitis and Aseptic Meningitis: Short-Term and Long-Term Outcome, Quality of Life and Neuropsychological FunctioningDocument9 pagesEncephalitis and Aseptic Meningitis: Short-Term and Long-Term Outcome, Quality of Life and Neuropsychological FunctioningRoberto SoehartonoNo ratings yet
- Early Life Serum Neurofilament Dynamics Predict Neurodevelopmental Outcome of Preterm InfantsDocument8 pagesEarly Life Serum Neurofilament Dynamics Predict Neurodevelopmental Outcome of Preterm InfantsKatharina GoeralNo ratings yet
- Prashant H 2006Document6 pagesPrashant H 2006iradNo ratings yet
- Epilepsia - 2019 - Hanin - Cerebrospinal Fluid and Blood Biomarkers of Status EpilepticusDocument13 pagesEpilepsia - 2019 - Hanin - Cerebrospinal Fluid and Blood Biomarkers of Status EpilepticusAmira GharbiNo ratings yet
- 005Document7 pages005Andreea AvasiloaieiNo ratings yet
- Acute Encephalitis Caused by Intrafamilial Transmission of Enterovirus 71 in AdultDocument7 pagesAcute Encephalitis Caused by Intrafamilial Transmission of Enterovirus 71 in AdultAdhi SyukriNo ratings yet
- Archive of SID: Early Diagnosis of Perinatal Asphyxia by Nucleated Red Blood Cell Count: A Case-Control StudyDocument7 pagesArchive of SID: Early Diagnosis of Perinatal Asphyxia by Nucleated Red Blood Cell Count: A Case-Control Studyeen265No ratings yet
- Pleds 2009 JamaDocument7 pagesPleds 2009 JamaRosiane Da Silva FontanaNo ratings yet
- Clinical Outcomes of Neonatal Hypoxic Ischemic Encephalopathy Evaluated With Diffusion-Weighted Magnetic Resonance ImagingDocument6 pagesClinical Outcomes of Neonatal Hypoxic Ischemic Encephalopathy Evaluated With Diffusion-Weighted Magnetic Resonance ImagingDrsandy SandyNo ratings yet
- Neonatal Seizures : Types, Etiology and Long Term Neurodevelopmental Out-Come at A Tertiary Care HospitalDocument7 pagesNeonatal Seizures : Types, Etiology and Long Term Neurodevelopmental Out-Come at A Tertiary Care HospitalAgung NohuNo ratings yet
- Brucellosis DCDocument6 pagesBrucellosis DCbrahim brahimNo ratings yet
- Cerebrospinal Fluid and Blood Biomarkers of Status Epilepticus - 2020Document40 pagesCerebrospinal Fluid and Blood Biomarkers of Status Epilepticus - 2020Reny Wane Vieira dos SantosNo ratings yet
- Status Epilepticus in Adults: A Study From Nigeria: SciencedirectDocument6 pagesStatus Epilepticus in Adults: A Study From Nigeria: SciencedirectLuther ThengNo ratings yet
- Hearing Loss in Term Newborn Infants With Hypoxic-Ischemic Encephalopathy Treated With Therapeutic Hypothermia PDFDocument8 pagesHearing Loss in Term Newborn Infants With Hypoxic-Ischemic Encephalopathy Treated With Therapeutic Hypothermia PDFstefanp89No ratings yet
- Serum Prolactin Level in Children With Febrile Seizure and Epileptic Seizure Comparative StudyDocument5 pagesSerum Prolactin Level in Children With Febrile Seizure and Epileptic Seizure Comparative StudyjumrainiNo ratings yet
- Telmisartan與失智的發生風險:全人口世代研究Document10 pagesTelmisartan與失智的發生風險:全人口世代研究Hima HuNo ratings yet
- Rabin Stein 2010Document6 pagesRabin Stein 2010luis fermin paredesNo ratings yet
- Seizstroke in ChildDocument6 pagesSeizstroke in ChildDian Isti AngrainiNo ratings yet
- NCC Case StudyDocument4 pagesNCC Case StudyMasego MekgoeNo ratings yet
- Rolul (A) EEG SI NIRS in Diagnosticul, Managmentul Si Prognosticul Convulsiilor NeonataleDocument10 pagesRolul (A) EEG SI NIRS in Diagnosticul, Managmentul Si Prognosticul Convulsiilor Neonataleandreea sfirnaciucNo ratings yet
- Ann Neonatol J 2021 - Effect of Phototherapy On Cardiac Functions in Neonates With Hyperbilirrubinemia. A Prospective Cross-Sectional StudyDocument19 pagesAnn Neonatol J 2021 - Effect of Phototherapy On Cardiac Functions in Neonates With Hyperbilirrubinemia. A Prospective Cross-Sectional StudyCharlie CharcapeNo ratings yet
- International Journal of Developmental NeuroscienceDocument6 pagesInternational Journal of Developmental NeuroscienceFarin MauliaNo ratings yet
- 1536 FullDocument7 pages1536 FullJosue LayedraNo ratings yet
- Leukodystrophies and Genetic Leukoencephalopathies in Children Specified by Exome Sequencing in An Expanded Gene PanelDocument9 pagesLeukodystrophies and Genetic Leukoencephalopathies in Children Specified by Exome Sequencing in An Expanded Gene PanelEduardo Rios DuboisNo ratings yet
- Epilepsy in Children with Cerebral PalsyDocument6 pagesEpilepsy in Children with Cerebral PalsyTiara Renita LestariNo ratings yet
- Importance of Long-Term EEG in Seizure-Free PatienDocument5 pagesImportance of Long-Term EEG in Seizure-Free PatienChu Thị NghiệpNo ratings yet
- Presentation, Etiology, and Outcome of Brain Infections in An Indonesian HospitalDocument15 pagesPresentation, Etiology, and Outcome of Brain Infections in An Indonesian HospitalANISA RIFKA RIDHONo ratings yet
- Case Series: Neuropsychiatric Symptoms With Pediatric Systemic Lupus ErythematosusDocument4 pagesCase Series: Neuropsychiatric Symptoms With Pediatric Systemic Lupus ErythematosusJosue LayedraNo ratings yet
- Ultrasonido Doppler Temprano AMSDocument7 pagesUltrasonido Doppler Temprano AMSKaren Marbelly OrozcoNo ratings yet
- Guillain-Barré Syndrome in Children: Clinic, Laboratorial and Epidemiologic Study of 61 PatientsDocument6 pagesGuillain-Barré Syndrome in Children: Clinic, Laboratorial and Epidemiologic Study of 61 PatientsFarah Basotjatjo KaharNo ratings yet
- Early Biochemical Indicators of Hypoxic-Ischemic Encephalopathy After Birth AsphyxiaDocument5 pagesEarly Biochemical Indicators of Hypoxic-Ischemic Encephalopathy After Birth AsphyxiaAgus WijataNo ratings yet
- 2017 - Differential Diagnosis of AD Using Spectrochemical Analysis of BloodDocument10 pages2017 - Differential Diagnosis of AD Using Spectrochemical Analysis of BloodM JNo ratings yet
- Cei 13095Document6 pagesCei 13095karen rinconNo ratings yet
- NIH Public Access: Management of Pediatric Status EpilepticusDocument16 pagesNIH Public Access: Management of Pediatric Status EpilepticusDiego CedamanosNo ratings yet
- Jurnal ReadingDocument27 pagesJurnal ReadingPatresya LantanNo ratings yet
- EEG - Dynamics - Sevo - Children - Br. J. Anaesth.-2015-Akeju-i66-76Document11 pagesEEG - Dynamics - Sevo - Children - Br. J. Anaesth.-2015-Akeju-i66-76MIRELA MIHALACHINo ratings yet
- ArticleDocument7 pagesArticleLinda RahayueNo ratings yet
- Pilot Study of An Intracranial ElectroencephalographyDocument6 pagesPilot Study of An Intracranial Electroencephalographymisacho82No ratings yet
- Espr Abstracts: Background: Hypoxic-Ischemic Brain Injury (HIE) Is The Most Common Perinatal Cerebral Insult AssociatedDocument1 pageEspr Abstracts: Background: Hypoxic-Ischemic Brain Injury (HIE) Is The Most Common Perinatal Cerebral Insult AssociatedAgus WijataNo ratings yet
- Ene 12372Document7 pagesEne 12372Andres Rojas JerezNo ratings yet
- P300 in Patients With Epilepsy - The DifDocument241 pagesP300 in Patients With Epilepsy - The DifasasakopNo ratings yet
- Use of Human Embryonic Stem Cells in The Treatment of Parkinson's Disease: A Case ReportDocument4 pagesUse of Human Embryonic Stem Cells in The Treatment of Parkinson's Disease: A Case Reportเพียงแค่ แอนโทนี่No ratings yet
- Etiology and Outcome of Non Traumatic Coma in Children Admitted To Pediatric Intensive Care UnitDocument6 pagesEtiology and Outcome of Non Traumatic Coma in Children Admitted To Pediatric Intensive Care Unitcohimif914No ratings yet
- Stroke JounalDocument7 pagesStroke JounalTony HermawanNo ratings yet
- Early Prediction of Severity StrokeDocument11 pagesEarly Prediction of Severity StrokeainihanifiahNo ratings yet
- Biochemical Marker As Predictor of Outcome in Perinatal AsphyxiaDocument4 pagesBiochemical Marker As Predictor of Outcome in Perinatal AsphyxiaAgus WijataNo ratings yet
- Clinical Predictors and Differential Diagnosis of Posterior Reversible Encephalopathy SyndromeDocument7 pagesClinical Predictors and Differential Diagnosis of Posterior Reversible Encephalopathy SyndromekidNo ratings yet
- Nejmc2008597 PDFDocument2 pagesNejmc2008597 PDFAdriana VasilicaNo ratings yet
- Jurnal 1 Ayudita Silvia HasibuanDocument6 pagesJurnal 1 Ayudita Silvia HasibuanParutigapuluh NovemberNo ratings yet
- Journal Full Ayudita Silvia HasibuanDocument29 pagesJournal Full Ayudita Silvia Hasibuanayudita silvia hasibuanNo ratings yet
- Factors predicting mortality in pediatric lupus nephritis patientsDocument6 pagesFactors predicting mortality in pediatric lupus nephritis patientsazwin lubisNo ratings yet
- A Randomized Controlled Clinical Trial To Compare The Safety and Effi Cacy of Edaravone in Acute Ischemic StrokeDocument5 pagesA Randomized Controlled Clinical Trial To Compare The Safety and Effi Cacy of Edaravone in Acute Ischemic StrokeWahyuni SetiawatiNo ratings yet
- Sleep Disorder 3Document7 pagesSleep Disorder 3Dani ursNo ratings yet
- Cardiac Troponin-I As A Marker of Myocardial Dysfunction in Children With Septic ShockDocument5 pagesCardiac Troponin-I As A Marker of Myocardial Dysfunction in Children With Septic ShockjessicaesmrldaNo ratings yet
- Hipo Glice MiaDocument7 pagesHipo Glice MiaRosita Aguirre FloresNo ratings yet
- NLR Bells PalsyDocument4 pagesNLR Bells PalsyIskandar HasanNo ratings yet
- Santoso 2020Document10 pagesSantoso 2020Aldo VictoriaNo ratings yet
- Faktor-Faktor Yang Berhubungan Dengan Kejadian Berat Badan Lahir Rendah (BBLR) Di Kabupaten KudusDocument10 pagesFaktor-Faktor Yang Berhubungan Dengan Kejadian Berat Badan Lahir Rendah (BBLR) Di Kabupaten KudusDellaNo ratings yet
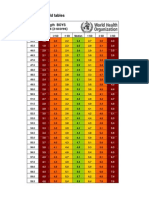
- Boys weight-length z-scores birth to 2 yearsDocument5 pagesBoys weight-length z-scores birth to 2 yearsAgus WijataNo ratings yet
- Link Zoom KONIKA 18-19 OctDocument6 pagesLink Zoom KONIKA 18-19 OctAgus WijataNo ratings yet
- 7869 40826 3 PB PDFDocument8 pages7869 40826 3 PB PDFHendra AjaNo ratings yet
- Espr Abstracts: Background: Hypoxic-Ischemic Brain Injury (HIE) Is The Most Common Perinatal Cerebral Insult AssociatedDocument1 pageEspr Abstracts: Background: Hypoxic-Ischemic Brain Injury (HIE) Is The Most Common Perinatal Cerebral Insult AssociatedAgus WijataNo ratings yet
- Wed SongDocument1 pageWed SongAgus WijataNo ratings yet
- Pediatric Infectious Diseases Conference Focuses on COVID ManagementDocument2 pagesPediatric Infectious Diseases Conference Focuses on COVID ManagementAgus WijataNo ratings yet
- 7869 40826 3 PB PDFDocument8 pages7869 40826 3 PB PDFHendra AjaNo ratings yet
- Drug Doses 2017Document127 pagesDrug Doses 2017Yuliawati HarunaNo ratings yet
- Pone 0026881Document5 pagesPone 0026881Agus WijataNo ratings yet
- Pediatric Infectious Diseases Conference Focuses on COVID ManagementDocument2 pagesPediatric Infectious Diseases Conference Focuses on COVID ManagementAgus WijataNo ratings yet
- Early Biochemical Indicators of Hypoxic-Ischemic Encephalopathy After Birth AsphyxiaDocument5 pagesEarly Biochemical Indicators of Hypoxic-Ischemic Encephalopathy After Birth AsphyxiaAgus WijataNo ratings yet
- Pediatric Infectious Diseases Conference Focuses on COVID ManagementDocument2 pagesPediatric Infectious Diseases Conference Focuses on COVID ManagementAgus WijataNo ratings yet
- Kids Games Powerpoint TemplateDocument26 pagesKids Games Powerpoint TemplateAgus WijataNo ratings yet
- Mile-Stones of Develovment of ChildrenDocument9 pagesMile-Stones of Develovment of ChildrenAgus WijataNo ratings yet
- Nna en November09Document3 pagesNna en November09Agus WijataNo ratings yet
- CC 100Document4 pagesCC 100Agus WijataNo ratings yet
- Biochemical Marker As Predictor of Outcome in Perinatal AsphyxiaDocument4 pagesBiochemical Marker As Predictor of Outcome in Perinatal AsphyxiaAgus WijataNo ratings yet
- Edwin Kim, MD A. Wesley Burks, MD Michael Pistiner, MD, MMSCDocument1 pageEdwin Kim, MD A. Wesley Burks, MD Michael Pistiner, MD, MMSCAgus WijataNo ratings yet
- a732b273a10a012b40c8154c371e732bDocument1 pagea732b273a10a012b40c8154c371e732bAgus WijataNo ratings yet
- Status of Serum Bilirubin, Serum Proteins and Prothrombin Time in Babies With Perinatal AsphyxiaDocument4 pagesStatus of Serum Bilirubin, Serum Proteins and Prothrombin Time in Babies With Perinatal AsphyxiaAgus WijataNo ratings yet
- 0 C 96053 C 581 B 042832000000Document1 page0 C 96053 C 581 B 042832000000Agus WijataNo ratings yet
- Test Definition: NSE: Reporting Title: Neuron Specific Enolase, SDocument1 pageTest Definition: NSE: Reporting Title: Neuron Specific Enolase, SAgus WijataNo ratings yet
- 5211Document7 pages5211Agus WijataNo ratings yet
- SDQ Score Sheet and Instructions For Self ReoprtDocument2 pagesSDQ Score Sheet and Instructions For Self ReoprtAgus WijataNo ratings yet
- Antimicrob. Agents Chemother. 2015 Ramachandran 1162 7Document6 pagesAntimicrob. Agents Chemother. 2015 Ramachandran 1162 7Agus WijataNo ratings yet
- SDQ Score Sheet and Instructions For Self ReoprtDocument2 pagesSDQ Score Sheet and Instructions For Self ReoprtAgus WijataNo ratings yet
- 0 C 96053 C 581 B 042832000000Document1 page0 C 96053 C 581 B 042832000000Agus WijataNo ratings yet
- Apnea NewbornDocument2 pagesApnea NewbornAgus WijataNo ratings yet
- When All They Had Was LoveDocument14 pagesWhen All They Had Was LoveRahul Pinnamaneni100% (1)
- How To Identify Adhd ChildrenDocument6 pagesHow To Identify Adhd ChildrenKUNNAMPALLIL GEJO JOHNNo ratings yet
- Anesthetic Management For Laparoscopic CholecystectomyDocument6 pagesAnesthetic Management For Laparoscopic CholecystectomyibunqumairaNo ratings yet
- Bedside BrochureDocument2 pagesBedside Brochureapi-438607141100% (1)
- Customer Satisfaction - Literature Review - FinalDocument28 pagesCustomer Satisfaction - Literature Review - FinalSaumya SarkarNo ratings yet
- Apollo Hospital Management System SRSDocument14 pagesApollo Hospital Management System SRSVishwa Sourab Brungi100% (2)
- Communication Skills For Doctors PDFDocument2 pagesCommunication Skills For Doctors PDFJenny50% (2)
- A Guide To The Treatment of Pressure UlcersDocument5 pagesA Guide To The Treatment of Pressure UlcersMac Perez LopezNo ratings yet
- ICU-Acquired Weakness and Recovery From Critical IllnessDocument9 pagesICU-Acquired Weakness and Recovery From Critical IllnessFebrian ParuraNo ratings yet
- Expressed Emotion in Eating Disorders Assessed via Self-ReportDocument10 pagesExpressed Emotion in Eating Disorders Assessed via Self-ReportSerbanescu BeatriceNo ratings yet
- Surgery in The Multimodal Mgmt. of Gastric Cancer - G. de Manzoni, Et. Al., (Springer, 2012) WWDocument264 pagesSurgery in The Multimodal Mgmt. of Gastric Cancer - G. de Manzoni, Et. Al., (Springer, 2012) WWAndreea Diana MegaNo ratings yet
- Acute Flaccid ParalysisDocument36 pagesAcute Flaccid ParalysisArun George100% (1)
- Warning Letters - Jubilant Generics Limited 3 - 6 - 19 PDFDocument4 pagesWarning Letters - Jubilant Generics Limited 3 - 6 - 19 PDFsudheerNo ratings yet
- Standard Precautions Hand Hygiene Gloves GownsDocument4 pagesStandard Precautions Hand Hygiene Gloves GownsAjeesh GopidasanNo ratings yet
- Post-Cardiac Arrest SyndromeDocument30 pagesPost-Cardiac Arrest SyndromeAuliaRahmanNo ratings yet
- NCPDocument4 pagesNCPAbegail Abaygar100% (1)
- Discharge advice after coronary proceduresDocument12 pagesDischarge advice after coronary proceduresEmma EmilyNo ratings yet
- Self-Assessment Colour Review of Small Animal Soft Tissue SurgeryDocument194 pagesSelf-Assessment Colour Review of Small Animal Soft Tissue Surgerymiliindianu100% (3)
- 1 Objectives and Classification PD FayadDocument25 pages1 Objectives and Classification PD FayadMostafa FayadNo ratings yet
- Chapter II - Anemia and Hypovolemic Shock Secondary To An Upper Gastrointestinal BleedingDocument3 pagesChapter II - Anemia and Hypovolemic Shock Secondary To An Upper Gastrointestinal BleedingKn VelasquezNo ratings yet
- Menieres DiseaseDocument43 pagesMenieres DiseaseChlodette Eizl M. Laurente100% (4)
- Research On Spaces Related To Doh Level 01 HospitalDocument7 pagesResearch On Spaces Related To Doh Level 01 HospitalDAVID, Jaeron V.No ratings yet
- Ico International Fellowship Program 4089Document94 pagesIco International Fellowship Program 4089Devdutta NayakNo ratings yet
- Worksheets - Isbar Week 4 x1Document3 pagesWorksheets - Isbar Week 4 x1api-631170779No ratings yet
- V 7.1 Breakpoint Tables EUCASTDocument98 pagesV 7.1 Breakpoint Tables EUCASTCarmina LepaNo ratings yet
- Infection in Critical CareDocument34 pagesInfection in Critical CareSuresh Kumar BansalNo ratings yet
- Satelec Tip Book 2011Document9 pagesSatelec Tip Book 2011akash_81087No ratings yet
- Parts of The Body and Health ProblemDocument13 pagesParts of The Body and Health ProblemSonia Tri AgustinaNo ratings yet
- Body MechanicsDocument2 pagesBody MechanicsKarLo TabuzoNo ratings yet
- Recavery After Anasthesia PDFDocument3 pagesRecavery After Anasthesia PDFYudionoNo ratings yet
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (402)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 5 out of 5 stars5/5 (4)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (13)
- The Happiness Trap: How to Stop Struggling and Start LivingFrom EverandThe Happiness Trap: How to Stop Struggling and Start LivingRating: 4 out of 5 stars4/5 (1)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 5 out of 5 stars5/5 (3)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (78)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 3.5 out of 5 stars3.5/5 (2)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsNo ratings yet
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- The Ultimate Guide To Memory Improvement TechniquesFrom EverandThe Ultimate Guide To Memory Improvement TechniquesRating: 5 out of 5 stars5/5 (34)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsFrom EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsNo ratings yet
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 3.5 out of 5 stars3.5/5 (31)
- Techniques Exercises And Tricks For Memory ImprovementFrom EverandTechniques Exercises And Tricks For Memory ImprovementRating: 4.5 out of 5 stars4.5/5 (40)
- Summary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisFrom EverandSummary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisRating: 5 out of 5 stars5/5 (3)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- Secure Love: Create a Relationship That Lasts a LifetimeFrom EverandSecure Love: Create a Relationship That Lasts a LifetimeRating: 5 out of 5 stars5/5 (17)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (327)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (44)