Professional Documents
Culture Documents
tmp269F TMP
Uploaded by
FrontiersOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
tmp269F TMP
Uploaded by
FrontiersCopyright:
Available Formats
European Journal of Clinical Investigation (2006) 36, 1 7
Arterial stiffening and cardiac hypertrophy in a new rat model
of type 2 diabetes
Blackwell Publishing Ltd
K.-C. Chang*, C.-D. Tseng, T.-F. Chou, Y.-L. Cho*, T.-C. Chi*, M.-J. Su* and Y.-Z. Tseng*
*
National Taiwan University, National Taiwan University Hospital, and Municipal Jen-Ai Hospital, Taipei, Taiwan
Abstract
Background We determined the effects of NIDDM on haemodynamic parameters
describing arterial wall elasticity and cardiac hypertrophy in rats administered streptozotocin
(STZ) and nicotinamide (NA), using the aortic impedance analysis.
Methods Male Wistar rats at 2 months were administered intraperitoneally 180 mg kg1 of NA,
30 min before an intravenous injection of 50 mg kg1 STZ, to induce type 2 diabetes. The STZNA rats were divided into two groups, 4 weeks and 8 weeks after induction of diabetes, and
compared with untreated age-matched controls. Pulsatile aortic pressure and flow signals were
measured by a high-fidelity pressure sensor and electromagnetic flow probe, respectively,
and were then subjected to Fourier transformation for the analysis of aortic input impedance.
Results In each diabetic group, the experimental syndrome was characterized by a moderate
and stable hyperglycaemia and a relative deficiency of insulin secretion. However, the 8week but not the 4-week STZ-NA diabetic rats showed a decrease in cardiac output in the
absence of any significant changes in mean aortic pressure, having increased total peripheral
resistance. The diabetic syndrome at 8 weeks also contributed to an increase in aortic
characteristic impedance, from 149 033 (mean SD) to 195 028 mmHg s mL1
(P < 005), suggesting a detriment to the aortic distensibility in NIDDM. Meanwhile, the
STZ-NA diabetic animals after 8 weeks had an increased wave reflection factor (046 009
vs. 061 013, P < 005) and decreased wave transit time (258 38 vs. 206 28 ms,
P < 005). Ratio of the left ventricular weight to body weight was also enhanced in the
8-week STZ-NA diabetic rats.
Conclusion The heavy intensity with early return of the pulse wave reflection may augment
systolic load of the left ventricle coupled to the arterial system, leading to cardiac hypertrophy
in the rats at 8 weeks after following STZ and NA administration.
Keywords Aortic distensibility, aortic input impedance, diabetes mellitus type 2, pulse wave
reflection, streptozotocin-nicotinamide diabetic rats.
Eur J Clin Invest 2006; 36 (1): 17
Introduction
Type 2 diabetes mellitus or noninsulin-dependent diabetes
mellitus (NIDDM) is a complex metabolic disorder
Department of Physiology, College of Medicine, National Taiwan
University (K.-C. Chang, Y.-L. Cho, Y.-Z. Tseng); Internal
Medicine, National Taiwan University Hospital (C.-D. Tseng,
Y.-Z. Tseng); Department of Surgery, Municipal Jen-Ai Hospital
(T.-F. Chou); Pharmacological Institute, College of Medicine,
National Taiwan University (T.-C. Chi, M.-J. Su), Taipei, Taiwan.
Correspondence to: K.-C. Chang, Department of Physiology,
College of Medicine, National Taiwan University, No. 1, Sec. 1,
Jen-Ai Road, Taipei, Taiwan. Tel.: 886-2-2312-3456 (ext. 8243);
fax: 886-2-2396-4350; e-mail: kcchang@ha.mc.ntu.edu.tw
Received 25 August 2005; accepted 31 October 2005
2006 Blackwell Publishing Ltd
characterized by hyperglycaemia and associated with a
relative deficiency of insulin secretion, along with a reduced
response of target tissues to insulin (insulin resistance).
These features of the disease may negatively modulate a
wide array of cardiovascular risk factors, including redox
imbalance and increased oxidative stress [1]. In type 2 diabetes, the formation of advanced glycation endproducts
(AGEs) on collagen is also enhanced within the arterial wall
and may contribute to vascular injury [2].
In 1998, Masiello et al. [3] described a new rat model of
type 2 diabetes that shares a number of features with human
NIDDM. This experimental syndrome was induced in adult
rats administered streptozotocin (STZ) and partially protected with a suitable dose of nicotinamide (NA). Its pathophysiological alterations could be mainly attributed to a
quantitative reduction of cells (40%) and the residual
cells appear to remain well differentiated and maintain most
K.-C. Chang et al.
of their metabolic functions [4]. The diabetic syndrome is
characterized by moderate stable hyperglycaemia, glucose
intolerance, altered but significant glucose-stimulated
insulin secretion, and in vivo and in vitro responsiveness to
tolbutamide.
Long-term complications of diabetes on the cardiovascular
system consist of macro and microvascular disease. Compared with nondiabetic individuals, patients with diabetes
manifest premature development of both arterial stiffness
[5] and diminished left ventricular compliance [6], contributing to increased risk for congestive heart failure. Although
the rat model of type 2 diabetes proposed by Masiello et al.
is helpful for understanding most aspects of the pathogenesis,
little attention has been given to the changes in the pulsatile
nature of blood flows in arteries. Hence, this study focused
on investigating the effects of NIDDM on haemodynamic
parameters describing arterial wall elasticity and cardiac
hypertrophy in rats after being administered STZ and NA,
using the aortic impedance analysis [7,8]. Our data suggest
that the heavy intensity with early return of the pulse wave
reflection may augment systolic load of the left ventricle
coupled to the arterial system, leading to cardiac hypertrophy
in rats with prolonged hyperglycaemia.
Methods
Animals and catheterization
Male Wistar rats at 2 months were administered intraperitoneally 180 mg kg1 of NA (Sigma, St. Louis, MO)
dissolved in saline, 30 min before an intravenous injection
of 50 mg kg1 STZ (Sigma) dissolved in 01 citrate buffer
(pH 45) [3]. The STZ-NA rats were divided into two
groups, 4 weeks (STZ-NA4) (n = 10) and 8 weeks (STZNA8) (n = 10) after induction of DM type 2, and compared
with untreated age-matched controls (n = 10). Insulin concentrations in plasma were measured by the ELISA method
(Mercodia AB, Uppsala, Sweden). The development of
hyperglycaemia was confirmed by blood glucose determination using a SURESTEP Test Strip (Lifescan Inc., Milpitas,
CA). All animals were allowed free access to the Purina
chow and water and housed two to three per cage in a 12-h
light/dark cycle animal room. The animal experiments were
conducted according to the Guide for the Care and Use of
Laboratory Animals, and were approved by the Animal Care
and Use Committee of the National Taiwan University.
General surgical procedures and measurement of the
haemodynamic variables in anaesthetized rats have been
described in our previous work [9]. In brief, rats were anaesthetized with sodium pentobarbital (50 mg kg1, i.p.), placed
on a heating pad, intubated, and ventilated with a rodent
respirator (Model 131, New England Medical Instruments,
Medway, MA). The chest was opened through the second
intercostal space of the right side. An electromagnetic flow
probe (model 100 series, internal circumference 8 mm,
Carolina Medical Electronics, King, NC) was positioned
around the ascending aorta to measure the pulsatile aortic
flow. A high-fidelity pressure catheter (model SPC 320, size
2F, Millar Instruments, Houston, TX) was used to measure
the pulsatile aortic pressure via isolated carotid artery of the
right side. The electrocardiogram (ECG) of lead II was
recorded with a Gould ECG/Biotach amplifier (Cleveland,
OH). The selective pressure and flow signals of 510 beats
were averaged in the time domain, using the peak R wave
of ECG as a fiducial point. Timing between the pressure
and flow signals, owing to spatial distance between the flow
probe and proximal aortic pressure transducer, was corrected by a time-domain approach, in which the foot of the
pressure waveform was realigned with that of the flow [10].
The resulting pressure and flow signals were subjected to
further aortic impedance analysis.
Aortic input impedance spectra
Aortic input impedance (Zi ) can be obtained from the ratio
of ascending aortic pressure harmonics to the corresponding
flow harmonics, using a standard Fourier series expansion
technique (Fig. 1) [79]. Total peripheral resistance of the
systemic circulation (Rp) was calculated as the mean aortic
pressure divided by mean aortic flow. The aortic characteristic
impedance (Zc) was computed by averaging high-frequency
moduli of the aortic input impedance data points (4 10th
harmonics) [11,12]. Taking Zc into consideration, we calculated the systemic arterial compliance C at mean aortic
pressure Pm by expanding the two-element [13] into the
three-element Windkessel model, which accounts for a
nonlinear exponential pressure-volume relationship:
bP
SV b
e m
,
bP
bP
K + Z c SV / Ad
e i e d
where SV is the stroke volume, K is the ratio of total area
under the aortic pressure curve to the diastolic area (Ad), b
is the coefficient in the pressure-volume relation (00131
0009 in aortic arch), Pi is the pressure at the time of incisura
and Pd is the end-diastolic pressure.
The wave transit time () can be computed by the impulse
response of the filtered aortic input impedance (Fig. 2).
This was accomplished by the inverse transformation of Zi
after multiplication of the first 12 harmonics by a DolphChebychev weighting function with the order 24 [14].
Meanwhile, the time domain reflection factor (Rf) can be
derived as the amplitude ratio of backward-to-forward peak
pressure wave by the method Westerhof et al. [15] proposed.
Therefore, both the wave transit time and the wave reflection factor may characterize the wave reflection phenomenon
in the vasculature.
C( Pm ) =
Gel electrophoresis
Method for measuring collagen glycation has been proposed
by Turk et al. [16]. Collagen samples from aortic walls, previously digested by pepsin, proteinase K and collagenase,
were investigated by sodium dodecyl sulphate polyacrylamide gel electrophoresis (SDS-PAGE) on Mini PROTEAN
2006 Blackwell Publishing Ltd, European Journal of Clinical Investigation, 36, 17
Aortic impedance in rats with type 2 diabetes
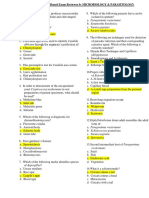
Figure 1 Aortic input impedance spectra derived from the
ascending aortic pressure and flow signals. The modulus of
impedance spectra at 8 but not 4 weeks after induction of diabetes
was displaced upward because of the impaired wall elastic
properties and shifted to the right owing to diminished aortic
distensibility. NC, normal controls; STZ-NA4, rats at 4 weeks after
being administered STZ and NA; STZ-NA8, rats at 8 weeks after
being administered STZ and NA; Rp, total peripheral resistance;
Zc, aortic characteristic impedance.
3 System (Bio-Rad Laboratory, Hercules, CA). This
was carried out using a 4% stacking and a 10% separating
gel, running buffer system (Tris-HCl, Ph 83 /SDS/glycine),
and Coomassie blue staining (Fig. 3). Each lane was loaded
with 20 g protein from two to three rats. Protein blotting analysis was carried on PVDF membrane, using
anti-AGE antibody 6D12 (Trans Genic Inc., Kumamoto,
Japan).
Statistics
Results are expressed as means SD. No differences in all
haemodynamic parameters studied were observed between
untreated 3- and 4-month control rats, and then all control
data were consolidated. Differences between the two STZ-NA
diabetic and the consolidated control groups were detected
using one-way analysis of variance (). Where differences
were found, significance was determined with Dunnetts
Figure 2 Impulse response function curve derived from the
filtered aortic input impedance spectra shown in Figure 1.
One-half of the time difference between the appearance of the
reflected peak from the body circulation (long arrow) and the initial
peak as a reference (short arrow) approximates the wave transit time
in the lower body circulation. It is evident that the 8- but not the
4-week STZ-NA diabetic rat had shortened wave transit time,
indicating an early return of pulse wave reflection from the
peripheral circulation. NC, normal controls; STZ-NA4, rats
at 4 weeks after being administered STZ and NA; STZ-NA8,
rats at 8 weeks after being administered STZ and NA;
, wave transit time.
test for multiple comparisons with a single control. Statistical significance is defined as P < 005.
Results
Table 1 shows the main metabolic features and aortic pressure profiles of the STZ-NA diabetic rats used in this study.
This experimental syndrome yielded a moderate and stable
hyperglycaemia and prevented STZ-induced hypoinsulinaemia and body weight loss. In comparison with controls,
both the 4- and the 8-week STZ-NA diabetic rats exhibited
no significant changes in systolic, diastolic and mean aortic
pressure. By contrast, the 8- but not the 4-week diabetic
rats had higher left ventricular weight and ratio of the left
ventricular weight to body weight.
2006 Blackwell Publishing Ltd, European Journal of Clinical Investigation, 36, 17
K.-C. Chang et al.
Table 1 Effects of NIDDM on body weight, left ventricular weight,
plasma glucose and insulin level, and aortic pressure profile in male
Wistar rats (n = 10 in each group)
Figure 3 SDS-PAGE electrophoretic profiles of aortic collagen
from the STZ-NA diabetic rats and normal controls. Diabetic
collagen samples at 8 weeks display molecular weight fragments
between 27 and 41 kDa which are much greater in amount than
those from normal controls. Protein blotting analysis on PVDF
membrane is shown in the right column, using anti-AGE antibody
6D12. NC, normal controls; STZ-NA4, rats at 4 weeks after being
administered STZ and NA; STZ-NA8, rats at 8 weeks after being
administered STZ and NA.
Figure 1 depicts abnormalities in the aortic input impedance spectra from a STZ-NA8 diabetic rat. The modulus
of impedance spectra at 8 but not 4 weeks after induction
of diabetes was displaced upward and shifted to the right.
Figure 2 describes impulse response function curve derived
from the filtered aortic input impedance spectra shown in
Fig. 1. It is evident that the 8- but not the 4-week STZ-NA
diabetic rat had shortened wave transit time. Figure 3 shows
the representative SDS-PAGE electrophoretic profiles of
aortic collagen from the experimental animals. There was
a 62% increase in collagen AGE content at 8 weeks after
induction of diabetes and little change after 4 weeks.
Figure 4 shows the effects of the experimental NIDDM
on the static haemodynamic data, including basal heart
rate (HR), cardiac output (CO), stroke volume (SV ), and
Variable
NC
STZ-NA4
STZ-NA8
BW (g)
LVW (mg)
LVW/BW (mg g1)
Glucose (mg dL1)
Insulin (IU mL1)
Ps (mmHg)
Pd (mmHg)
Pm (mmHg)
Pf (mmHg)
Pb (mmHg)
Z1 (mmHg s mL1)
4475 318
8068 627
180 008
1048 153
715 300
1190 92
950 82
1088 87
926 069
459 055
265 024
4220 239
7900 713
187 015
1552 115*
632 250
1159 174
896 167
1041 174
1020 048
486 028
281 013
4180 297
8330 622*
205 019*
1584 242
687 272
1191 181
929 170
1074 172
1020 044
610 032*
367 018*
All values are expressed as means SD.
No differences in these basic data were observed between
untreated 3- and 4-month control rats, and then all control data
were consolidated. All data collected from STZ-NA-diabetic rats
were compared with those of untreated controls.
*
P < 005 compared with controls. P < 001 compared with
controls.
BW, body weight; LVW, left ventricular weight; Ps, systolic aortic
pressure; Pd , diastolic aortic pressure; Pm, mean aortic pressure;
Pf , magnitude of the forward pressure; Pb, magnitude of the
backward; Z1, fundamental impedance modulus; NC, age-matched
controls; STZ-NA4, diabetic rats at 4 weeks after being
administered STZ and NA; STZ-NA8, diabetic rats at 8 weeks
after being administered STZ and NA.
total peripheral resistance (Rp); HR exhibited a significant
decrease in the diabetic rats at 8 but not 4 weeks after STZ
and NA administration (Fig. 4a). Although producing a fall
in CO (Fig. 4b) and SV (Fig. 4c) in the 8-week diabetic
animals, the experimental syndrome showed no significant
changes in these variables in the rats 4 weeks after induction of
diabetes. A decrease in CO in the absence of any significant
Figure 4 Effects of NIDDM on basal heart
rate (HR in a), cardiac output (CO in b),
stroke volume (SV in c), and total peripheral
resistance (Rp in d). No differences in those
static haemodynamic data were observed
between untreated 3- and 4-month control
rats, and then all control data were
consolidated. NC, normal controls;
STZ-NA4, rats at 4 weeks after being
administered STZ and NA; STZ-NA8,
rats at 8 weeks after being administered
STZ and NA.
2006 Blackwell Publishing Ltd, European Journal of Clinical Investigation, 36, 17
Aortic impedance in rats with type 2 diabetes
Figure 5 Effects of NIDDM on aortic
characteristic impedance (Zc in a), arterial
compliance at mean aortic pressure (Cm in
b), wave reflection factor (Rf in c), and wave
transit time ( in d). No differences in those
pulsatile haemodynamic data were observed
between untreated 3- and 4-month control
rats, and then all control data were
consolidated. NC, normal controls;
STZ-NA4, rats at 4 weeks after being
administered STZ and NA; STZ-NA8,
rats at 8 weeks after being administered
STZ and NA.
changes in Pm (Table 1) caused an increase in R p in the
STZ-NA8 diabetic rats, from 549 78 to 658 87
mmHg s mL1 (P < 005) (Fig. 4d).
Figure 5 depicts the effects of the experimental NIDDM
on the pulsatile nature of blood flows in arteries using aortic
characteristic impedance (Zc), arterial compliance (Cm),
wave transit time (), and wave reflection factor (Rf ). No
significant changes in Zc and Cm were detected in the rats
at 4 weeks after induction of diabetes. However, the STZNA8 diabetic rats showed a marked increase in Zc, from
149 033 to 195 028 mmHg s mL1 (P < 005) (Fig. 5a),
and a decrease in Cm, from 101 12 to 81 17 L
mmHg1 (P < 005) (Fig. 5b). The 8-week diabetic animals
also had increased fundamental impedance modulus (Z1)
at 265 024 vs. 367 018 mmHg s mL1 (P < 005)
(Table 1). Meanwhile, the experimental syndrome at 8
weeks elicited an increase in magnitude of the backward
pressure (Pb), but exerted no effect on magnitude of the forward pressure (Pf) (Table 1), causing an increase in Rf , from
046 009 to 061 013 (P < 005) (Fig. 5c). In addition,
the STZ-NA8 diabetic rats had decreased , at 258 38
vs. 206 28 ms (P < 005) (Fig. 5d).
Discussion
The major findings of this study are that in the absence of
hypertension only in the rats at 8 weeks after STZ and NA
administration does diabetes produces a detriment to the
aortic distensibility and impairs wave reflection phenomena.
The results indicate that type 2 diabetes influences elastic
arteries (characteristic impedance), muscular arteries (wave
reflection factor) and arterioles (peripheral resistance).
Herein, the combined administration of STZ with a suitable protective dose of NA used to rats leads to the development of DM type 2 as reported by Masiello et al. [3]. The
experimental syndrome at both 4 and 8 weeks was charac-
terized by a moderate and stable hyperglycaemia and associated with a relative deficiency of insulin secretion (Table 1).
No significant alterations in aortic pressure profile were
found in each diabetic group compared with controls. By
contrast, a decline in cardiac output occurred in the absence
of any significant changes in mean aortic pressure, causing
an increase of 199% in total peripheral resistance (Rp) in
the 8- but not the 4-week STZ-NA diabetic animals.
Diabetes mellitus is a complex metabolic disorder, which
involves redox imbalance and increased oxidative stress [1].
Various potential cardiovascular risk factors such as homocysteine may increase levels of superoxide anion radical in
subjects with type 2 diabetes [2,17,18]. Even at low concentrations, nitric oxide (NO) can react rapidly with the
superoxide under conditions of oxidative stress to form the
very harmful peroxynitrite anion [19]. Meanwhile, nonenzymatic glycation of proteins, formation of advanced glycation endproducts, has the potential to quench NO and then
diminish the vasodilatory capacity of the peripheral muscular arteries [20,21]. However, Pieper [22] has reported a
triphasic response of increased, unaltered and impaired
NO-mediated relaxation in the diabetic blood vessels,
depending on the duration of 1, 2 and 8 weeks of the
disease, respectively. Herein, the increased vascular smooth
muscle tone of the resistance vessels occurred in the diabetic
rats at 8 but not 4 weeks after being administered STZ and
NA. Probably, reduced NO availability and increased peroxynitrite production may cause vasoconstriction, alter
growth of vascular muscle, as well as producing cellular
injury in the rats with prolonged hyperglycaemia.
As for the pulsatile components of the arterial load, the
aortic characteristic impedance increased (Zc in Fig. 5a) and
the arterial compliance decreased (Cm in Fig. 5b) in the 8but not the 4-week STZ-NA diabetic rats. In a hydraulic
system, Zc is directly related to pulse wave velocity (PWV ),
and then has an inverse relation to the aortic distensibility:
the higher the aortic characteristic impedance, the stiffer
the aortic wall [7,8]. In addition, animal studies using a
2006 Blackwell Publishing Ltd, European Journal of Clinical Investigation, 36, 17
K.-C. Chang et al.
three-element Windkessel model suggest that an increase in
the low-frequency harmonic of impedance may indicate
a decrease in systemic arterial compliance [23]. Herein, we
used the fundamental impedance modulus as an index of
the low-frequency portion of the impedance spectrum and
found that the moduli of the lower harmonics increase
in the rats after 8 weeks of type 2 diabetes (Table 1). The
change of lower harmonics of the aortic input impedance
supported the likelihood that NIDDM decreased the
systemic arterial compliance in the animals treated with
STZ and NA. Both the augmented Zc and the diminished Cm
suggest that a decline in aortic distensibility may occur in
the rats that were induced with diabetes at 8 weeks after
the injection of STZ and NA.
It has been shown that inhibition of the synthesis of NO
may induce an endothelium-dependent constriction of aortic
rings, leading to an increase in Zc [11]. As NO production
varies with duration of diabetes [22,24], reduced NO availability may be one of the factors responsible for arterial
stiffening in the STZ-NA8 diabetic rats. Moreover, tissue
collagen modified by advanced glycation is reported to be
related to the duration of diabetes mellitus [16]. Thus, prolonged hyperglycaemia may enhance AGE formation and
accumulation in the arterial wall with changes in the biomechanical properties of collagen [25 27]. Herein, there
was a 62% increase in collagen AGE content at 8 weeks after
induction of diabetes and little change after 4 weeks. The
AGE-modulated collagen crosslinks in the elastic reservoir
could function as one of the several factors to increase
the aortic stiffness in the STZ-NA8 diabetic rats. Viewed
together, reduced NO availability and enhanced AGEmodulated collagen crosslinks in Windkessel vessels could
be considered potential roles in regulating the development of
arterial stiffening in animals with prolonged hyperglycaemia.
Changes in timing and/or magnitude of the pulse wave
reflection do impair the loading condition for the left
ventricle coupled to its arterial system [28]. As mentioned
earlier, a decline in aortic distensibility could be reflected
in the increased PWV and in the reduced along the path.
The shorter observed in the STZ-NA8 diabetic rats (Fig. 5d)
suggests that prolonged hyperglycaemia may cause an early
return of pulse wave reflection from the peripheral circulation. Meanwhile, the experimental syndrome at 8 weeks
contributed to a significant increase in magnitude of the
backward pressure, whereas the magnitude of the forward
pressure remained unchanged (Table 1). The elevated Pb
associated with the unaltered Pf was responsible for the
increase in R f (Fig. 5c), suggesting the heavy reflection
intensity in the STZ-NA8 diabetic rats. Thus, the enhanced
Rf with shortened indicates that prolonged hyperglycaemia
can modify the timing and magnitude of the pulse wave
reflection to augment systolic load of the left ventricle. That
may increase the ratio of left ventricular weight to body
weight, an indicator of cardiac hypertrophy, in the STZNA8 diabetic animals.
Herein, the augmented wave reflection factor in the STZNA8 diabetic rats was not in accordance with that of human
with diabetes reported by Lacy et al. [29]. They found that
pulse wave velocity but not augmentation index (wave
reflection index) is increased in patients with diabetes, and
this might be attributed to a higher heart rate in the diabetic
group. The lower HR in the 8-week diabetic rats may be the
factor responsible for the higher Rf because of the inverse,
linear relationship between wave reflection index and heart
rate [30]. By contrast, the shorter wave transit time with
prolonged hyperglycaemia was in accordance with that
observed in human with diabetes [29]. As is generally recognized, is inversely related to PWV, which is modulated
by arterial blood pressure. Several studies also found a positive correlation between PWV and resting HR [3133]. It
is inferred that the lower HR associated with the unchanged
aortic pressure might cause a decline in PWV and then an
increase in in the STZ-NA8 diabetic animals. However,
the shorter was observed in the rats after 8 weeks of type
2 diabetes in this report. This suggests that the increased
oxidative stress and protein glycation rather than HR may
be the main factors responsible for arterial stiffening in the
animals with prolonged hyperglycaemia.
In this report, no significant changes in systolic blood
pressure and pulse pressure were observed in the STZ-NA8
diabetic rats with the increased arterial stiffness. Several factors importantly affect the magnitude of the pulse pressure,
including the stroke volume and the aortic compliance [34].
The arterial pulse pressure varies directly with the stroke
volume but inversely with the arterial compliance. Thus, the
decrease in SV (Fig. 4c) with diabetes may blunt the effect
of arterial stiffness (e.g. the diminished Cm in Fig. 5b) on
the systolic blood pressure and arterial pulse pressure in the
rats at 8 weeks after following STZ and NA administration.
In conclusion, we have demonstrated that in the absence
of hypertension only in rats at 8 weeks after streptozotocin
and nicotinamide administration does type 2 diabetes produce a detriment to the physical properties of the resistance
vessels and the Windkessel vessels. The heavy intensity with
early return of the pulse wave reflection indicates that the
prolonged hyperglycaemia can augment systolic load of the
left ventricle coupled to its arterial system. The impaired
systolic loading condition of the left ventricle may cause
the heart to adapt to muscular hypertrophy when rats are
administered streptozotocin and nicotinamide after 8 weeks.
Acknowledgements
This study was supported by grants from the National
Taiwan University (NTUH 94-S017) and from the National
Science Council of Taiwan (NSC 942320-B-002058).
References
1 Oberley LW. Free radicals and diabetes. Free Rad Biol Med
1988;5:11324.
2 Hayden JM, Reaven PD. Cardiovascular disease in diabetes
mellitus type 2: a potential role for novel cardiovascular risk
factors. Curr Opin Lipidol 2000;11:51928.
2006 Blackwell Publishing Ltd, European Journal of Clinical Investigation, 36, 17
Aortic impedance in rats with type 2 diabetes
3 Masiello P, Broca C, Gross R, Roye M, Manteghetti M,
Hillaire-Buys D et al. Experimental NIDDM. Development of
a new model in adult rats administered streptozotocin and
nicotinamide. Diabetes 1998;47:224 9.
4 Novelli M, Fabregat ME, Fernandez-Alvarez J, Gomis R,
Masiello P. Metabolic and functional studies on isolated islets
in a new rat model of type 2 diabetes. Mol Cell Endocrinol
2001;175:57 66.
5 Lehmann ED, Riley WA, Clarkson P, Gosling RG.
Non-invasive assessment of cardiovascular disease in diabetes
mellitus. Lancet 1997; 350:SI14 9.
6 Poirier P, Bogaty P, Garneau C, Marois L, Dumesnil JG.
Diastolic dysfunction in normotensive men with well-controlled
type 2 diabetes: importance of maneuvers in echocardiographic
screening for preclinical diabetic cardiomyopathy. Diabetes Care
2001;24:5 10.
7 Milnor WR. Hemodynamics. Baltimore: Williams & Wilkins Co.:
1989.
8 Nichols WW, ORourke MF. Mcdonalds Blood Flow in Arteries.
Arnold: London: 1998.
9 Chang KC, Hsu KL, Tseng YZ. Effects of diabetes and gender
on mechanical properties of the arterial system in rats: aortic
impedance analysis. Exp Biol Med 2003;228:70 8.
10 Mitchell GF, Pfeffer MA, Westerhof N, Pfeffer JM.
Measurement of aortic input impedance in rats. Am J Physiol
1994;267 (Heart Circ. Physiol., 36):H1907 15.
11 Gaballa MA, Raya TE, Hoover CA, Goldman S. Effects of
endothelial and inducible nitric oxide synthases inhibition on
circulatory function in rats after myocardial infarction.
Cardiovasc Res 1999;42:627 35.
12 Huijberts MS, Wolffenbuttel BH, Boudier HA, Crijns FR,
Kruseman AC, Poitevin P et al. Aminoguanidine treatment
increases elasticity and decreases fluid filtration of large arteries
from diabetic rats. J Clin Invest 1993;92:140711.
13 Liu A, Brin KP, Yin FCP. Estimation of total arterial
compliance: An improved method and evaluation of current
methods. Am J Physiol 1986;251 (Heart Circ. Physiol.,
20):H588 600.
14 Laxminarayan S, Sipkema P, Westerhof N. Characterization of
the arterial system in the time domain. IEEE Trans Biomed Eng
1978;25:177 84.
15 Westerhof N, Sipkema P, VanDen Bos GC, Elzinga G. Forward
and backward waves in the arterial system. Cardiovasc Res
1972;6:648 56.
16 Turk Z, Misur I, Turk N, Benko B. Rat tissue collagen modified
by advanced glycation: correlation with duration of diabetes and
glycemic control. Clin Chem Lab Med 1999;37:813 20.
17 Drzewoski J, Czupryniak L, Chwatko G, Bald E.
Hyperhomocysteinemia in pooly controlled type 2 diabetes
patients. Diabetes Nutr Metab 2000;13:319 24.
18 Lang D, Kredan MB, Moat SJ, Hussain SA, Powell CA,
Bellamy MF et al. Homocysteine-induced inhibition of
endothelium-dependent relaxation in rabbit aorta:
role foe superoxide anions. Arterioscl Throm Vas Biol
2000;20:422 7.
19 Blough NV, Zafiriou OC. Reaction of superoxide with nitric
oxide to form peroxynitrite in alkaline aqueous solution. Inorg
Chem 1985;24:35045.
20 McCance DR, Dyer DG, Dunn JA, Bailie KE, Thorpe SR,
Baynes JW et al. Maillard reaction products and their relation
to complications in insulin dependent diabetes mellitus. J Clin
Invest 1993;91:24708.
21 Li YM, Steffes M, Donnelly T, Liu C, Fuh H, Basgen J et al.
Prevention of cardiovascular and renal pathology of aging by
the advanced glycation inhibitor aminoguanidine. Proc Natl
Acad Sci USA 1996;93:39027.
22 Pieper GM. Enhanced, unaltered and impaired nitric
oxide-mediated endothelium-dependent relaxation in
experimental diabetes mellitus: importance of disease duration.
Diabetologia 1999;42:20413.
23 Westerhof N, Van den Bos GC, Elzinga G. Influence of central
and peripheral changes on the hydraulic input impedance of the
systemic arterial tree. Med Biol Eng 1973;11:71023.
24 Pieper GM. Review of alterations in endothelial nitric oxide
production in diabetes: protective role of arginine on
endothelial dysfunction. Hypertension 1998;31:104760.
25 Brownlee M, Cerami A, Vlassara H. Advanced glycosylation
end products in tissue and the biochemical basis of diabetic
complications. N Engl J Med 1988;318:131521.
26 Bucula R, Cerami A. Advanced glycosylation: chemical,
biology, and implications for diabetes and aging. Adv Pharmacol
1992;23:134.
27 Vlassara H, Bucala R, Striker L. Pathogenic effects of advanced
glycosylation: biochemical, biological, and clinical implications
for diabetes and aging. Lab Invest 1994;70:13851.
28 ORourke MF, Avolio AP, Nichols WW. Left ventricularsystemic arterial coupling in humans and strategies to improve
coupling in disease states. In: Yin FCP, editor. Ventricular/
Vascular Coupling. New York: Springer-Verlag;1987,pp. 119.
29 Lacy PS, OBrien DG, Stanley AG, Dewar MM, Swales PR,
Williams B. Increased pulse wave velocity is not associated with
elevated augmentation index in patients with diabetes.
J Hypertens 2004;22:193744.
30 Wilkinson IB, MacCallum H, Flint L, Cockcroft JR,
Newby DE, Webb DJ. The influence of heart rate on
augmentation index and central arterial pressure in humans.
J Physiol 2000;525:26370.
31 Sa Cunha CR, Pannier B, Benetos A, Siche JP, London GM,
Mallion JM et al. Association between high heart rate and high
arterial rigidity in normotensive and hypertensive subjects.
J Hypertens 1997;15:142330.
32 Asmar R, Rudnichi A, Blacher J, London GM, Safar ME. Pulse
pressure and aortic pulse wave are markers of cardiovascular
risk in hypertensive populations. Am J Hypertens 2001;14:917.
33 Haesler E, Lyon X, Pruvot E, Kappenberger L, Hayoz D.
Confounding effects of heart rate on pulse wave velocity in
paced patients with a low degree of atherosclerosis. J Hypertens
2004;22:131722.
34 West JB. BEST and TAYLORS Physiological Basis of Med
Practice. Baltimore: Williams & Wilkins;1991,pp. 1479.
2006 Blackwell Publishing Ltd, European Journal of Clinical Investigation, 36, 17
You might also like
- tmpCD4A TMPDocument8 pagestmpCD4A TMPFrontiersNo ratings yet
- Robert D. Foreman Et Al - Modulation of Intrinsic Cardiac Neurons by Spinal Cord Stimulation: Implications For Its Therapeutic Use in Angina PectorisDocument9 pagesRobert D. Foreman Et Al - Modulation of Intrinsic Cardiac Neurons by Spinal Cord Stimulation: Implications For Its Therapeutic Use in Angina PectorisLuammmNo ratings yet
- hr2008109 PDFDocument10 pageshr2008109 PDFKumarsai DurusojuNo ratings yet
- Effect Garlic ExtractDocument6 pagesEffect Garlic ExtractSubhadra LaimayumNo ratings yet
- Beneficial Role of Telmisartan On Cardiovascular Complications Associated With STZ-induced Type 2 Diabetes in RatsDocument11 pagesBeneficial Role of Telmisartan On Cardiovascular Complications Associated With STZ-induced Type 2 Diabetes in RatsAuthor Nauman ShadNo ratings yet
- Regional Alterations After Brief Coronary Artery Occlusion in Conscious DogsDocument8 pagesRegional Alterations After Brief Coronary Artery Occlusion in Conscious DogsFranco Fabricio CarpioNo ratings yet
- Effect of Coenzyme Q10 On Risk of AtheroDocument8 pagesEffect of Coenzyme Q10 On Risk of AtheroKumar KartikeyNo ratings yet
- The Effect of Combined Aerobic and Resistance Exercise Training On Vascular Function in Type 2 DiabetesDocument7 pagesThe Effect of Combined Aerobic and Resistance Exercise Training On Vascular Function in Type 2 DiabetesZINATUL WIDADNo ratings yet
- Anti-Inflammatory and Metabolic Effects of Candesartan in Hypertensive PatientsDocument5 pagesAnti-Inflammatory and Metabolic Effects of Candesartan in Hypertensive PatientsBarbara Sakura RiawanNo ratings yet
- Detection of Myocardial Infraction Monisha C M - 17bei0092: Select, Vit VelloreDocument8 pagesDetection of Myocardial Infraction Monisha C M - 17bei0092: Select, Vit VelloresubramanianNo ratings yet
- Study For MCB CardioDocument12 pagesStudy For MCB Cardiolavanya.aNo ratings yet
- AT2 Receptor AgonistsDocument5 pagesAT2 Receptor Agonistsfer123wizNo ratings yet
- Salt Sensitivity of Blood Pressure in NKCC1-deficient MiceDocument9 pagesSalt Sensitivity of Blood Pressure in NKCC1-deficient MiceHongyu LiNo ratings yet
- The Year in Cardiology 2015Document13 pagesThe Year in Cardiology 2015SyafniYuliaSistriNo ratings yet
- Novel Strategy For Measuring Creatine Kinase Reaction Rate in The in Vivo HeartDocument10 pagesNovel Strategy For Measuring Creatine Kinase Reaction Rate in The in Vivo HeartYoung-Hoon SungNo ratings yet
- Jurnal HeartDocument9 pagesJurnal HeartHe RhaNo ratings yet
- Reljanovic Et Al. - 1999 - Treatment of Diabetic Polyneuropathy With The Antioxidant Thioctic Acid (Alpha-Lipoic Acid) A Two Year Multi Center Randomized DoubleDocument9 pagesReljanovic Et Al. - 1999 - Treatment of Diabetic Polyneuropathy With The Antioxidant Thioctic Acid (Alpha-Lipoic Acid) A Two Year Multi Center Randomized DoubleJay LawNo ratings yet
- Bern Jak 2021Document6 pagesBern Jak 2021Meirina KhairatNo ratings yet
- Dynamics of The QT Interval During and After Exercise in Healthy ChildrenDocument6 pagesDynamics of The QT Interval During and After Exercise in Healthy ChildrenNITACORDEIRONo ratings yet
- Status Epilepticus Induces Cardiac Myofilament Damage and Increased Susceptibility To Arrhythmias in RatsDocument8 pagesStatus Epilepticus Induces Cardiac Myofilament Damage and Increased Susceptibility To Arrhythmias in Ratsricky hutagalungNo ratings yet
- Progressive Aortic Stiffness in Aging C57Bl-6 Mice Displays Altered Contractile Behaviour and Extracellular Matrix ChangesDocument11 pagesProgressive Aortic Stiffness in Aging C57Bl-6 Mice Displays Altered Contractile Behaviour and Extracellular Matrix Changesender000No ratings yet
- Qualitative and Quantitative Comparison of Tgrappa and Tsense Real Time Cine Techniques During Deep BreathingDocument316 pagesQualitative and Quantitative Comparison of Tgrappa and Tsense Real Time Cine Techniques During Deep BreathingRadhaRajasekaranNo ratings yet
- FluidDocument190 pagesFluidAndrias OzNo ratings yet
- AbstractDocument12 pagesAbstractMunir AlshameeryNo ratings yet
- Jvms 83 997Document7 pagesJvms 83 997Blanca A SerranoNo ratings yet
- Short-Term Effects of Methylene Blue On Hemodynamics and Gas Exchange in Humans With Septic ShockDocument5 pagesShort-Term Effects of Methylene Blue On Hemodynamics and Gas Exchange in Humans With Septic ShockMahtosurup GodavarthyNo ratings yet
- Stimulation of Acupuncture LociDocument12 pagesStimulation of Acupuncture LociThais LimaNo ratings yet
- Tmpa252 TMPDocument10 pagesTmpa252 TMPFrontiersNo ratings yet
- Gastric distension causes peripheral vasoconstriction in anaesthetized pigsDocument12 pagesGastric distension causes peripheral vasoconstriction in anaesthetized pigsHimanshu SharmaNo ratings yet
- Torsades de Pointes in 3 Patients With Leukemia Treated With Arsenic TrioxideDocument4 pagesTorsades de Pointes in 3 Patients With Leukemia Treated With Arsenic TrioxideStanley PhanNo ratings yet
- Tsalikakis Clinical ScienceDocument7 pagesTsalikakis Clinical SciencetsalikakisNo ratings yet
- Adverse Diastolic Remodeling After Reperfused ST-elevation Myocardial Infarction: An Important Prognostic IndicatorDocument11 pagesAdverse Diastolic Remodeling After Reperfused ST-elevation Myocardial Infarction: An Important Prognostic IndicatorCatia MoraesNo ratings yet
- EMPA REG OUTCOME The Cardiologist S Point 2017 The American Journal of MedDocument6 pagesEMPA REG OUTCOME The Cardiologist S Point 2017 The American Journal of MedAlina PopaNo ratings yet
- Dong 2022Document8 pagesDong 2022Olivia LimNo ratings yet
- Krunoslav Fuckar, Nenad Lakusic, Hrvoje Stipic: Case ReportDocument8 pagesKrunoslav Fuckar, Nenad Lakusic, Hrvoje Stipic: Case ReportFariz DwikyNo ratings yet
- 2015-Acta PhysiologicaDocument19 pages2015-Acta PhysiologicaFatima Ezzahra ZahrouNo ratings yet
- The Angiotensin AT Receptor in Myocardial Infarction: Elena KaschinaDocument7 pagesThe Angiotensin AT Receptor in Myocardial Infarction: Elena KaschinaIrina Luciana DumitriuNo ratings yet
- 6_aphresis, + statinDocument7 pages6_aphresis, + statinjef5525No ratings yet
- 2000 - Reactions of The Heart Rate and Carotid Artery Pulse Wave Components To The Nitroglycerine UptakeDocument1 page2000 - Reactions of The Heart Rate and Carotid Artery Pulse Wave Components To The Nitroglycerine UptakesuknatsNo ratings yet
- Arrhythmia risks after thrombolytic therapyDocument5 pagesArrhythmia risks after thrombolytic therapyTaniaNo ratings yet
- Takeda 2007 Spironolakton Pada MI TikusDocument11 pagesTakeda 2007 Spironolakton Pada MI TikusauliaNo ratings yet
- Metformin Attenuates Early-Stage Atherosclerosis in Mildly Hyperglycemic Oikawa-Nagao MiceDocument9 pagesMetformin Attenuates Early-Stage Atherosclerosis in Mildly Hyperglycemic Oikawa-Nagao Micegandik danu pramigaNo ratings yet
- Stress-Related Cardiomyopathy or Tako-Tsubo Syndrome: Current ConceptsDocument6 pagesStress-Related Cardiomyopathy or Tako-Tsubo Syndrome: Current ConceptslivroinglesNo ratings yet
- International Journal of Neurology and Neurotherapy Ijnn 2 030Document2 pagesInternational Journal of Neurology and Neurotherapy Ijnn 2 030Anis Rita PratiwiNo ratings yet
- Beneficial Effect of Cyclosporine A On Traumatic Hemorrhagic ShockDocument12 pagesBeneficial Effect of Cyclosporine A On Traumatic Hemorrhagic ShockJoecoNo ratings yet
- Overview of StressDocument32 pagesOverview of Stressjennifer benavideSNo ratings yet
- 3636 1 7556 1 10 20230505Document8 pages3636 1 7556 1 10 20230505WellemNo ratings yet
- Lanza - Diagnostic and Prognostic Value of ST Segment Depression Limited To The Recovery Phase of Exercise Stress TestDocument5 pagesLanza - Diagnostic and Prognostic Value of ST Segment Depression Limited To The Recovery Phase of Exercise Stress TestM. PurnomoNo ratings yet
- Irreversible ShockDocument50 pagesIrreversible ShockAnonymous YWmEwCNo ratings yet
- Beta-Block The Septic Heart 2010Document5 pagesBeta-Block The Septic Heart 2010Ivann FloresNo ratings yet
- A Clinical Evaluation of Statin Pleiotropy: Statins Selectively and Dose-Dependently Reduce Vascular InflammationDocument9 pagesA Clinical Evaluation of Statin Pleiotropy: Statins Selectively and Dose-Dependently Reduce Vascular InflammationzzakieNo ratings yet
- Evaluation of Morphological Changes in Experimental Models of Myocardial Infarction: Electron and Light Microscopical EvidenceDocument11 pagesEvaluation of Morphological Changes in Experimental Models of Myocardial Infarction: Electron and Light Microscopical EvidenceRania QhalisyaNo ratings yet
- Insulin Resistance Is Not Associated With Myocardial Steatosis in WomenDocument8 pagesInsulin Resistance Is Not Associated With Myocardial Steatosis in WomenAstriUtamaNo ratings yet
- Skeletal Muscle Deoxygenation Abnormalities in Early Post-Myocardial InfarctionDocument8 pagesSkeletal Muscle Deoxygenation Abnormalities in Early Post-Myocardial Infarctionmehdi.chlif4374No ratings yet
- Lapkas VT RevisiDocument13 pagesLapkas VT RevisiRannyNo ratings yet
- Clinchem 2013 203778 FullDocument9 pagesClinchem 2013 203778 FullHarnadi WonogiriNo ratings yet
- Reciprocal Communication of Pericoronary Adipose TDocument7 pagesReciprocal Communication of Pericoronary Adipose TeugeniaNo ratings yet
- Pi Is 0140673605601146Document1 pagePi Is 0140673605601146Novita Dewi LestariNo ratings yet
- PletismografiaDocument10 pagesPletismografiamaxifamous6No ratings yet
- Antiarrhythmic DrugsFrom EverandAntiarrhythmic DrugsAntoni Martínez-RubioNo ratings yet
- tmp80F6 TMPDocument24 pagestmp80F6 TMPFrontiersNo ratings yet
- tmpCE8C TMPDocument19 pagestmpCE8C TMPFrontiersNo ratings yet
- tmp3CAB TMPDocument16 pagestmp3CAB TMPFrontiersNo ratings yet
- Tmpa077 TMPDocument15 pagesTmpa077 TMPFrontiersNo ratings yet
- tmpF178 TMPDocument15 pagestmpF178 TMPFrontiersNo ratings yet
- tmp6F0E TMPDocument12 pagestmp6F0E TMPFrontiersNo ratings yet
- tmpEFCC TMPDocument6 pagestmpEFCC TMPFrontiersNo ratings yet
- Tmp1a96 TMPDocument80 pagesTmp1a96 TMPFrontiersNo ratings yet
- tmp72FE TMPDocument8 pagestmp72FE TMPFrontiersNo ratings yet
- tmpF407 TMPDocument17 pagestmpF407 TMPFrontiersNo ratings yet
- tmpF3B5 TMPDocument15 pagestmpF3B5 TMPFrontiersNo ratings yet
- tmpE3C0 TMPDocument17 pagestmpE3C0 TMPFrontiersNo ratings yet
- tmpE7E9 TMPDocument14 pagestmpE7E9 TMPFrontiersNo ratings yet
- tmpFFE0 TMPDocument6 pagestmpFFE0 TMPFrontiersNo ratings yet
- tmp6382 TMPDocument8 pagestmp6382 TMPFrontiersNo ratings yet
- tmp60EF TMPDocument20 pagestmp60EF TMPFrontiersNo ratings yet
- tmpB1BE TMPDocument9 pagestmpB1BE TMPFrontiersNo ratings yet
- tmpC30A TMPDocument10 pagestmpC30A TMPFrontiersNo ratings yet
- tmp8B94 TMPDocument9 pagestmp8B94 TMPFrontiersNo ratings yet
- tmp998 TMPDocument9 pagestmp998 TMPFrontiersNo ratings yet
- tmp3656 TMPDocument14 pagestmp3656 TMPFrontiersNo ratings yet
- tmp37B8 TMPDocument9 pagestmp37B8 TMPFrontiersNo ratings yet
- tmpD1FE TMPDocument6 pagestmpD1FE TMPFrontiersNo ratings yet
- tmpC0A TMPDocument9 pagestmpC0A TMPFrontiersNo ratings yet
- tmp4B57 TMPDocument9 pagestmp4B57 TMPFrontiersNo ratings yet
- tmp9D75 TMPDocument9 pagestmp9D75 TMPFrontiersNo ratings yet
- tmp27C1 TMPDocument5 pagestmp27C1 TMPFrontiersNo ratings yet
- tmp2F3F TMPDocument10 pagestmp2F3F TMPFrontiersNo ratings yet
- tmpA0D TMPDocument9 pagestmpA0D TMPFrontiersNo ratings yet
- Tmp75a7 TMPDocument8 pagesTmp75a7 TMPFrontiersNo ratings yet
- Yoga y AyurvedaDocument50 pagesYoga y AyurvedaManuel100% (1)
- Mu 089Document4 pagesMu 089Rahul RaiNo ratings yet
- MSDS Berkat Saintifindo PDFDocument27 pagesMSDS Berkat Saintifindo PDFDianSelviaNo ratings yet
- 10 0000@Www Quintpub Com@ejed@18638Document23 pages10 0000@Www Quintpub Com@ejed@18638Víctor Rodríguez67% (3)
- RX Int Festival PlanGuideDocument8 pagesRX Int Festival PlanGuideIke1234567No ratings yet
- Acute Lymphoblastic LeukaemiaDocument3 pagesAcute Lymphoblastic LeukaemiamelpaniNo ratings yet
- Levodopa in The Treatment of Parkinson's DiseaseDocument15 pagesLevodopa in The Treatment of Parkinson's Diseasewisni damayantiNo ratings yet
- Enriched Air Diver Knowledge ReviewDocument2 pagesEnriched Air Diver Knowledge Reviewgabriele belmonte100% (1)
- 2021-2022 Sem 2 Lecture 2 Basic Tests in Vision Screenings - Student VersionDocument123 pages2021-2022 Sem 2 Lecture 2 Basic Tests in Vision Screenings - Student Versionpi55aNo ratings yet
- Medical services tariffs starting 2016 and on-request servicesDocument16 pagesMedical services tariffs starting 2016 and on-request servicesIonutNo ratings yet
- A Comparison of Muscle Strength and Flexibility Between The Preferred and Non Preferred Leg in English Soccer PlayersDocument10 pagesA Comparison of Muscle Strength and Flexibility Between The Preferred and Non Preferred Leg in English Soccer PlayersMalikiNo ratings yet
- Scalp Acupuncture BasicsDocument27 pagesScalp Acupuncture BasicsGanga SinghNo ratings yet
- BSMT Review For BoardsDocument3 pagesBSMT Review For BoardsLyudmyla GillegoNo ratings yet
- 504 Vs IEP Power PointDocument11 pages504 Vs IEP Power Pointbmorgan5No ratings yet
- Botany Vol-2 - EMDocument232 pagesBotany Vol-2 - EMVandanaNo ratings yet
- WeeFIM Score Sheet (MS Word)Document4 pagesWeeFIM Score Sheet (MS Word)Siti Maryam Rosyidah0% (2)
- Medicine BOF 2017 OctoberDocument7 pagesMedicine BOF 2017 Octoberweerawarna fernandoNo ratings yet
- Positioning: The Battle For Your MindDocument30 pagesPositioning: The Battle For Your Mindjayson RebeiroNo ratings yet
- Tonus MuscularDocument12 pagesTonus MuscularRadu Cristian StuparNo ratings yet
- Genetic Polymorphism of Cyp2d6Document23 pagesGenetic Polymorphism of Cyp2d6Oscar Velasco0% (1)
- PHMB-Silver Sulfadiazine - HCDT-20-019Document7 pagesPHMB-Silver Sulfadiazine - HCDT-20-019gloriaNo ratings yet
- Modern Wound Care Practical Aspects of Non Interventional Topical Treatment of Patients With Chronic WoundsDocument14 pagesModern Wound Care Practical Aspects of Non Interventional Topical Treatment of Patients With Chronic WoundsDauz ArashNo ratings yet
- World03 30 16Document40 pagesWorld03 30 16The WorldNo ratings yet
- Hospital Waste Management in Kathmandu Valley Power Point FinalDocument30 pagesHospital Waste Management in Kathmandu Valley Power Point FinalSamzana0% (1)
- Pes WesDocument12 pagesPes WesjotapintorNo ratings yet
- Oral Physio FinalDocument34 pagesOral Physio FinaldraggarwalNo ratings yet
- Health and its failure: Causes, Types, and Prevention of DiseasesDocument9 pagesHealth and its failure: Causes, Types, and Prevention of DiseasesAbhimanyu BahreeNo ratings yet
- Management of Intravascular Devices To Prevent Infection: LinicalDocument5 pagesManagement of Intravascular Devices To Prevent Infection: LinicalCristianMedranoVargasNo ratings yet
- Research Background: (Budget 2016: Chapter 5 - An Inclusive and Fair Canada, 2021)Document4 pagesResearch Background: (Budget 2016: Chapter 5 - An Inclusive and Fair Canada, 2021)Talha NaseemNo ratings yet
- Red Cross Blood Donation CaseDocument12 pagesRed Cross Blood Donation CaseYajuvender SinghNo ratings yet