Professional Documents
Culture Documents
tmp6FA8 TMP
Uploaded by
FrontiersOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
tmp6FA8 TMP
Uploaded by
FrontiersCopyright:
Available Formats
Med. Eng. Phys. Vol. 18, No. 4, pp.
336-338,
1996
Copyright
0 1996 Elsevier Science Ltd for IPEMB
Printed
in Great Britain.
All rights reserved
1350-4533/96
$15.00 + 0.00
1350-4533(95)00049-6
ELSEVIER
Reply to Professor Burattinis
comments on
Exponentially
tapered t-tube model of systemic
arterial system in dogs
Kuo-Chu Chang
Department
of Phvsiolow.
College
Set. 1, Jen-Ai Rd, Taipec Taiwan
Received
Med.
8 March
Eng.
Phys.,
1995, accepted
1996,
Vol.
25 July
of Medicine,
National
Taiwan
University,
No. 1,
1995
18, 336-338, June
There is no argument
to say that the geometric
and elastic tapering of the arterial system is the
rule of nature and any assumption
to describe the
mechanical
and anatomical
properties
of blood
vessels in a uniform fashion deviates considerably
from the reality.
Diameter
tapering is evident as lumen radius
and wall thickness become
progressively
small
toward the peripheral.
The wall stiffness and
pulse wave velocity are increasing
with the distance from the heart. There are many reports suggesting that the reflection
phenomena
in the
arterial system are low-pass filteredz4.
This lowpass filtering
is presumed
to be due to the geometric and elastic differences,
such as tapering,
between the proximal
and distal portions of the
arterial tree. Both diameter
and elastic tapering
cause a smooth change of the arterial impedance
and will have a substantial impact on the magnitude and/or sequence of pulse wave reflection.
In studies of Wave travel in arteries and the
design of the cardiovascular
system, Taylor summarized the main effects of non-uniformity
of the
arterial system 5. These found that the efficiency of
the system will be enhanced if the system is made
progressively
less distensible
in its peripheral
extensions.
If the heart frequency
be suitably
chosen, such a non-uniform
distensibility
will
result in minimal
reflected components
from the
periphery
and a functional
isolation of the input
impedance,
thus both reducing cardiac work and
keeping
it relatively
constant
at different
frequencies. It was concluded
that the experimental
evidence is all in favour of the existence of such
suitable non-uniformity
in the mammalian
arterial
system. Consequently,
making use of a uniform
transmission
line to relate pulsatile pressure and
flow waveforms in the ascending aorta is indeed
improper.
Burattinis
contribution
on the uniform model is well recognized.
However, from a
scientific point of view, the important
thing is how
to advance the uniform
model to describe the
non-uniform
nature of the arterial system.
The main issue remained
to be unravelled
is
how to incorporate
the non-uniform
geometrical
and mechanical
properties
of the vasculature to
analyse the measured pulsatile aortic pressure and
flow signals. We start our approach by using an
exponentially
tapered
transmission
line
to
describe the non-uniformity
of the tube6. In the
process of our non-uniform
T-tube model formulation, each tsbe terminates
in a normalized
lo&d
impedance,
&. Burattini
et al. criticize
that &
must be a real and frequency independent
load
to result in our equation
(4). We disagree with
that comment
because the arterial impedance
is
complex
and frequency-dependent,
even at the
distal of the tube. In both formulation
of uniform
line and non-uniform
line, it is not necessary to
concrete that Z, has to be real resistor. Therefore,
r (0,) equals 0 if the arterial impedance
at the
distal of the tube equals the terminal
load at the
termination
of the tube.
In our report6, we a ologize for missing to mention the assumption
1F I<< 1, when the approximation
equation,
our equation
(2), is used to
resolve the problem.
Burattini
et al. question that
under the assumption
ll?<<
1 we still have a
result in relatively
big amplitude
of reflected
waves with respect to forward waves as displayed
in our Figure 4. In fact, the magnitude
of pulse
reflection
is 0.48 calculated by our non-uniform
T-tube model and this value is smaller than that,
0.55, estimated by the uniform T-tube model proposed by Burattini
et aZ.,s, when the same dog
data were analysed. Although
the shape of these
forward and reflected waves are similiar to those
calculated
by Burattini
et al. using their uniform
T-tube, the impedance
spectra at the inlet of each
tube are significantly
different
when the uniform
and non-uniform
T-tube models are adopted to
relate the same pulsatile aortic pressure and flow
fkpownl~a~~y
signals. It is obvious to notice that at high frequency portion the input impedance
at the inlet
of head circulation
is considerably
smaller than
that at the entrance of body circulation
when
their uniform
T-tube is used to analyse the data
(see Figure I). When our data are analysed with
the uniform T-tube model, the result is similiar to
that obtained
by Burattini
et aZ.,. However, this
is in contradiction
with the general finding that
the blood vessels in the head circulation,
brachiocephalic
and left subclavian arteries, are stiffer
and narrower than those in the body circulation,
descending
thoracic aorta and large arteries in
the abdomen.
The phase velocity is a function
of both pulsation, o, and position, z, along the paths (&~re
9.7 and Fi re 9.5 in the book of Milnor,
respectively) $-I. This is the characterstic
of the
arterial system no matter whether the arterial system is modelled
or not. Burattini
et al. argue that
the phase velocity in a uniform transmission
tube
is independent
of pulsation and the phase velocity
must be a function
of pulsation
in an exponentially tapered transmission
line. They conclude
tapred
t-tube
model
of systemic
arterial
syslrm
in dqp:
KuoChu
Chang
that our equation
(9) is incorrect
because the
dependence
of the phase velocity on o is not
taken into consideration.
We wonder very much
why there should be a discrepancy between these
two models. The general findings are the fact that
apparent phase velocity calculated
from Fourier
series of pressures in the ascending aorta of the
dog is frequencydependenP.
The dilemma
our
non-uniform
model
encounters
is also the
dilemma
that the uniform model has to face. We
take the assumption
that the phase velocity in an
exponentially
tapered transmission
line is independent
of o as in the uniform
tube. The
important
fact is that wave front velocity of the
pressure wave is in progressive
increase with
increasing distance from the heart. Our non-uniform T-tube mode takes into account that the
phase velocity is positiondependent.
The disadvantage of the uniform model is that the influence
of elastic tapering is not taken into consideration.
Therefore,
the uniform
T-tube model is insufficient to relate pulsatile pressure and flow signals
measured in the ascending aorta.
We acknowledge
that our non-uniform
T-tube
model has a drawback in our equation
(14). This
is the high frequency adaptation
between the tube
and the terminal
load. We assume that the normalizedarterial
impedance
at the distal of the
tube, &, equals the normalized
complex terminal
load, &. At the termination
of each tube, the following result holds as w - cc:
(1)
0
Frcqlrciay
(lb)
100
200
Frequency
300
400
(Hz)
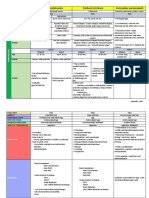
Figure 1 The uniform
T-tube model proposed
by Burattini
et al.,*
is used to relate pulsatile aortic pressure and flow waveforms
that is
the same as the example
in Changs report.
In the upper panel, the
solid lines show the pressure and flow signals measured
in the ascencing aorta, and the predicted
pressure is represented
as a dashed line.
Model-estimated
forward
and backward
pressure components
at the
inlet of the head circulation
(dashed lines), body circulation
(dotted
lines). and in the ascending
aorta (solid lines) are shown in the
middle panel. In the lower panel, the input impedance
spectra of
the head circulation
(dashed lines), body circulation
(dotted lines),
and whole systemic vasculature
(solid lines) are shown. Circles are
data points obtained
from the ratio of the ascending
aortic pressure
harmonics
to the corresponding
flow harmonics
& is the arterial impedance
at the distal of the
tube, and 4 is the peripheral
vascular resistance.
&,, is the load resistor chosen to adapt the load
with the tube at high frequency. There is little
information
about the exact value in end-tube
characteristic
impedance
at very high frequencies.
However, we learn the fact that the apparent
phase velocity should be higher
at lower frequencies where reflections
prevail, and lower at
higher frequencies where reflections
are less significant.
According
to Lathams
report),
at
locations immediately
proximal
and distal to the
renal branches, the difference
between the two
corresponding
apparent
velocities
at high frequency is small while the difference
at low frequency is relatively large. So, we speculated that
at very high frequencies the characteristic
impedance at the distal of the tube approximates
the
characteristic
impedance
at the entrance of the
transmission
tube, Z,. This assumption
leads to
high frequency adaptation
between the tube and
the terminal
load that is expressed by our equation (14):
(2)
However, the exact connection
between ( Zd),=
remains to be determined.
and (&),x
In the process of parameter
estimation,
the
number
of six free model parameters
estimated
by our non-uniform
T-tube model is the same as
337
&$onatially
tapered t-tube model of
systaic arterial system in dogs: KueChu
1 System parameters estimated by making use of the uniform
T-tube model. Proposed by Burattini er al.
Table
(N= 10)
Mean 251 9.75 0.0528
+SD f41 24.82 f0.0269
0.0634
344 22.42 0.0888
0.1549
f0.0166 f78 f7.31 f0.0323 f0.0879
Subscript
h = head
circulation;
b = body
circulation.
Z, = characteristic inpedance at the inlet of the tube (dyne s cmm5);
r = tube-end transmission time
(ms);
(I&= tube
compliance
(ml mmHg-); Cr= load compliance (ml mmHg-).
the number of free parameters estimated by Burattini
et al. in their
uniform
T-tube
model.
Although
we do not introduce
any more parameters, it cannot be judged, based on this point,
that the use of the exponentially
tapered transmission line theory for the description
of the vasculature is incorrect. Now, I would raise a question: What kind of model is a good, useful, and
correct model for the description
of the arterial
system? Indeed,
modelling
is very much an art.
Mathematical
models, however, are limited in having a finite number of variables and a finite arithmetical precision.
A really good, useful, and
correct
model should identify regularities
in a
system and then create a mathematic
process that
could emulate, to a limited degree, the behaviour
of the actual system. It not only has a goodness of
model-fit,
but also has the model-generated
parameters capable of representing
and interpreting
the biological
system. Table I lists some model-estimated
parameters
when the uniform
T-tube
model proposed by Burattini
et al. is used to analyse our experimental
data. The results are in contrast to the general expectations
because Z, is
27% larger than Zh, where h and b represent the
head and body circulation
respectively. These are
close to the reports by Burattini
et aZ.s. On the
other hand, our non-uniform
T-tube model gives
the estimate of Z., that is, on the average, 88.25%
of the estimate of Z,,. This is in agreement
with
the findings of Cox and Pace who found that &,
was 12% less than Zh. Since the non-uniform
Ttube model has spatial tapering of the tube for
which the phase constant is a function of the path
length, the calculation
of tube compliance
from
the knowledge of characteristic
impedance
at the
inlet of the tube, 2, and tube-end transmission
time, T, seems to be meaningless.
However, for the
uniform
T-tube model, tube compliance
can be
calculated
by having model-estimated
Z, and T:
C, = T/Z,~. Surprisingly,
the calculated tube compliance is significantly
smaller than the estimated
load compliance
in each tube (see Table I). The
results are similar to those obtained by Burattini
et
338
Chang
aPp8**. These are in contradiction
with the general
expectations
that there is more compliance
in
proximal
than distal arteries. All unexpected
results mentioned
above originate
from the use
of the uniformtransmissionline to represent the
arterial system when non-uniformity
is the rule of
nature in this system.
The unexpected
results obtained
by the uniform T-tube model proposed by Burattini
et al.
prompt
as to conclude
that the uniform
T-tube
model is incorrect to relate pulsatile pressure and
flow waveforms measured in the ascending aorta. On
the other hand, our non-uniform
T-tube model
gives reasonable
estimates in representing
and
interpreting
the mechanical
properties of the vasculature. The important
aspect of the exponentially tapered transmission line theory is that it can
reflect the behaviour of the arterial diameter and
elastic tapering.
However, our non-uniform
Ttube model still has a drawback as mentioned
earlier. More studies are needed to resolve the problem, in the formulation
of the arterial non-uniformity, to construct a model in more reality.
REFERENCES
1. McDonald
DA. Blood flow in Arteries. London: Arnold,
1974.
of an assembly of ran2. Taylor MC. The input impedance
domly branching elastic tube. BiophysJ 1966; 6: 29-51.
3. Westerhof N, Sipkema P, Van Den Bos GC, Elzinga G.
Forward and backward waves in the arterial system. Curdiovas Res 1972, 6: 648-56.
4. Latson TW, Hunter WC, Katoh N, Sagawa K. Effect of
nitroglycerin
on aortic impedance, diameter, and pulse
wave velocity. Circ Res 1988; 62: 884-90.
5. Taylor MG. Wave travel in arteries and the design of the
cardiovascular system. In Pulsatik Blow FZow (Attinger EO,
Editor), McGraw-Hill,
Inc., 1964.
6. Chang KC, Tseng YZ, Lin YJ, Kuo TS, Chen HI. Exponentially tapered t-tube model of systemic arterial system in
dogs. Med Eng Phys 1994; 16: 370-S.
R, Campbell KB. Modified asymmetric T-tube
7. Burattini
model to infer arterial wave reflection at the aortic root.
IEEE Trans Biomed Eng 1989; 36: 805-14.
8. Burattini
R, Knowlen GG, Campbell KB. Two arterial
effective reflecting sites may appear as one to the heart.
Circ I2es 1991; 68: 85-99.
9. Milnor
WR. Hemodynamics.
Baltimore: Williams & Wilkins, 1989.
10. Lathm RD, Westerhof N, Sipkema P, Rubal BJ, Reuderink P, Murgo JP. Regional wave travel and reflections
along the human aorta: a study with six simultaneous
micromanometric
pressures. Circulation
1985; 72(6):
1257-69.
11. Cox RH, Pace JB. Pressure-flow relations in the vessels of
the canine aortic arch. AmJPhysiol
1975; 228: l-10.
R, Bell DL, Kirkpatrick
RD,
12. Campbell KB, Burattini
Knowlen GG. Time-domain
formulation
of asymmetric
T-tube model of arterial system. AmJ Physiol 1990; 258:
H1761-74.
You might also like
- tmpB83D TMPDocument9 pagestmpB83D TMPFrontiersNo ratings yet
- Central Venous Pressure: Its Clinical Use and Role in Cardiovascular DynamicsFrom EverandCentral Venous Pressure: Its Clinical Use and Role in Cardiovascular DynamicsNo ratings yet
- Aw of OiseuilleDocument4 pagesAw of OiseuilleVinay GuptaNo ratings yet
- Thoracic Electrical Bioimpedance Theory and Clinical Possibilities in Perioperative MedicineDocument6 pagesThoracic Electrical Bioimpedance Theory and Clinical Possibilities in Perioperative MedicinebusagaNo ratings yet
- ECG/EKG Interpretation: An Easy Approach to Read a 12-Lead ECG and How to Diagnose and Treat ArrhythmiasFrom EverandECG/EKG Interpretation: An Easy Approach to Read a 12-Lead ECG and How to Diagnose and Treat ArrhythmiasRating: 5 out of 5 stars5/5 (2)
- Notes and Discussions: Department of Natural Sciences, University of Wisconsin-Superior, Superior, Wisconsin 54880Document4 pagesNotes and Discussions: Department of Natural Sciences, University of Wisconsin-Superior, Superior, Wisconsin 54880garridolopezNo ratings yet
- ScienceDocument12 pagesScienceMohammed Al-AzawyNo ratings yet
- Morgan 1974Document15 pagesMorgan 1974mintillaNo ratings yet
- Revisiting The Simplified Bernoulli EquationDocument6 pagesRevisiting The Simplified Bernoulli Equationgu1000No ratings yet
- Articol 4Document16 pagesArticol 4POPESCU LUCIANNo ratings yet
- Arterial Doppler Waveforms: Understanding Hemodynamic PrinciplesDocument21 pagesArterial Doppler Waveforms: Understanding Hemodynamic PrinciplesL0v3B00k5100% (6)
- 040Document14 pages040Assacd AasdedNo ratings yet
- Detecting Cardio-Vascular Acoustics in An Incipient TurbulenceDocument14 pagesDetecting Cardio-Vascular Acoustics in An Incipient TurbulenceMJBAS JournalNo ratings yet
- Schiller Etal 2008Document28 pagesSchiller Etal 2008ramsis321No ratings yet
- Flow InstabilityDocument30 pagesFlow InstabilityGiriNo ratings yet
- 383 - Pre-Lab 4 - Laminar Flow in ArteriesDocument2 pages383 - Pre-Lab 4 - Laminar Flow in Arterieshelloceline1No ratings yet
- Lec. 1 Selected TopicsDocument30 pagesLec. 1 Selected TopicsMustafa KamelNo ratings yet
- Lab 3 - Wind Tunnel and Boundary LayerDocument9 pagesLab 3 - Wind Tunnel and Boundary LayerameershamiehNo ratings yet
- Straatman2002 PDFDocument8 pagesStraatman2002 PDFmintillaNo ratings yet
- Ce (Ra1) F (T) PF1 (Bmak) Pfa (Ak) PF2 (Pag)Document4 pagesCe (Ra1) F (T) PF1 (Bmak) Pfa (Ak) PF2 (Pag)Jozhy Nugraha MahmudaNo ratings yet
- Ageing of The Conduit Arteries: Review ArticleDocument16 pagesAgeing of The Conduit Arteries: Review ArticlehoplalaNo ratings yet
- Physics of Live Systems (10 Points) : TheoryDocument4 pagesPhysics of Live Systems (10 Points) : TheoryFishNo ratings yet
- Arterial DopplerDocument29 pagesArterial DopplerAudrey100% (20)
- Andritos & HanrattyDocument21 pagesAndritos & HanrattyMohit KulkarniNo ratings yet
- Hyrtl AnastomosisDocument6 pagesHyrtl AnastomosisMiguel SantosNo ratings yet
- Applications of Partial DerivativesDocument17 pagesApplications of Partial DerivativesK BhargavramNo ratings yet
- 7 ImpedanceDocument7 pages7 Impedancewx8vnnnzjhNo ratings yet
- Hagen Poiseuille FlowDocument7 pagesHagen Poiseuille FlowRocky Tran100% (1)
- Amm 31 (2007) 1847 - 1864Document18 pagesAmm 31 (2007) 1847 - 1864Duraisamy Sambasiavm SankarNo ratings yet
- Laminar and Turbulent Flows in Bounded SystemsDocument11 pagesLaminar and Turbulent Flows in Bounded SystemsRamy Abd Elkhalek Shahin100% (1)
- Interference Test Case StudyDocument41 pagesInterference Test Case StudyEdgar ChiquitoNo ratings yet
- Water Hammer EquationsDocument11 pagesWater Hammer Equationsmostafa shahrabiNo ratings yet
- Prevent pulsation problemsDocument10 pagesPrevent pulsation problemsfathim1356No ratings yet
- Application of Basic Science To Anesthesia Case FileDocument4 pagesApplication of Basic Science To Anesthesia Case Filehttps://medical-phd.blogspot.comNo ratings yet
- Hypertension: A Comparative Review Based On Fractal Wave Theory of ContinuumDocument8 pagesHypertension: A Comparative Review Based On Fractal Wave Theory of ContinuumAdaptive MedicineNo ratings yet
- Viscous and turbulent flow conceptsDocument9 pagesViscous and turbulent flow conceptsjassimjaz_327682348No ratings yet
- A Study On Two-Layered Model (Casson-Newtonian) For Blood Ow Through An Arterial Stenosis: Axially Variable Slip Velocity at The WallDocument14 pagesA Study On Two-Layered Model (Casson-Newtonian) For Blood Ow Through An Arterial Stenosis: Axially Variable Slip Velocity at The WallRicardoNo ratings yet
- Blood vessel layer in direct contact with red blood cellsDocument9 pagesBlood vessel layer in direct contact with red blood cellsAsp Corp SlaveNo ratings yet
- Numerical Analysis of Stent Design for Intra-saccular Aneurysmal FlowDocument4 pagesNumerical Analysis of Stent Design for Intra-saccular Aneurysmal FlowSupriya RaniNo ratings yet
- Diagnosis of The Preterm Patent DuctusDocument9 pagesDiagnosis of The Preterm Patent DuctusHelenaFalconeNo ratings yet
- 1 s2.0 014154259190100L MainDocument9 pages1 s2.0 014154259190100L MainMetehan AgacaNo ratings yet
- 1974 ARahman, FHStilllingerDocument11 pages1974 ARahman, FHStilllingerDaniel ArismendiNo ratings yet
- Lin e Hanratty 1986 Prediction PDFDocument20 pagesLin e Hanratty 1986 Prediction PDFFrancisco OppsNo ratings yet
- Formal ReportxDocument7 pagesFormal ReportxDarshan ShaarmaNo ratings yet
- Physics of flowLR PDFDocument7 pagesPhysics of flowLR PDFAshwin SheriefNo ratings yet
- Tmpa252 TMPDocument10 pagesTmpa252 TMPFrontiersNo ratings yet
- Surge Analysis Using Transient Pressure TheoryDocument8 pagesSurge Analysis Using Transient Pressure TheoryMaqsood Ibn Shaikhul ArfeenNo ratings yet
- Lab1 Continuity Equation and Bernoullis PrincipalDocument22 pagesLab1 Continuity Equation and Bernoullis Principaljon382k0% (1)
- Fluid_Mechanics_4.pdfDocument7 pagesFluid_Mechanics_4.pdfDesmond OwusuNo ratings yet
- Venous Function and Central Venous Pressure: A Physiologic StoryDocument14 pagesVenous Function and Central Venous Pressure: A Physiologic StoryMarzuki Panji WijayaNo ratings yet
- Probe Methods For Direct MeasurementsDocument17 pagesProbe Methods For Direct MeasurementsMuhammad UsmanNo ratings yet
- Emodinamik: Muhammad Yusuf Fathoni Yudhish ResiDocument23 pagesEmodinamik: Muhammad Yusuf Fathoni Yudhish Resiyusuf fathoniNo ratings yet
- Basic concepts of viscosity and blood flowDocument3 pagesBasic concepts of viscosity and blood flowtahera aqeelNo ratings yet
- 1 s2.0 0735109795005986 MainDocument6 pages1 s2.0 0735109795005986 MainDiana BonteanNo ratings yet
- Poiseuille's Law of Blood FlowDocument13 pagesPoiseuille's Law of Blood Flownadim_tabassum9760No ratings yet
- Wang and Gleason, 2010Document11 pagesWang and Gleason, 2010Ανδρεας ΜπομπαςNo ratings yet
- Ultrasound in Vascular DiseaseDocument10 pagesUltrasound in Vascular Diseaseospinu6780100% (1)
- j124 Cmame CardDocument7 pagesj124 Cmame CardmkbNo ratings yet
- tmp3CAB TMPDocument16 pagestmp3CAB TMPFrontiersNo ratings yet
- tmpCE8C TMPDocument19 pagestmpCE8C TMPFrontiersNo ratings yet
- tmpFFE0 TMPDocument6 pagestmpFFE0 TMPFrontiersNo ratings yet
- tmpE7E9 TMPDocument14 pagestmpE7E9 TMPFrontiersNo ratings yet
- tmp6F0E TMPDocument12 pagestmp6F0E TMPFrontiersNo ratings yet
- tmpE3C0 TMPDocument17 pagestmpE3C0 TMPFrontiersNo ratings yet
- tmpF178 TMPDocument15 pagestmpF178 TMPFrontiersNo ratings yet
- tmp80F6 TMPDocument24 pagestmp80F6 TMPFrontiersNo ratings yet
- tmpEFCC TMPDocument6 pagestmpEFCC TMPFrontiersNo ratings yet
- Tmp1a96 TMPDocument80 pagesTmp1a96 TMPFrontiersNo ratings yet
- tmpF3B5 TMPDocument15 pagestmpF3B5 TMPFrontiersNo ratings yet
- Tmpa077 TMPDocument15 pagesTmpa077 TMPFrontiersNo ratings yet
- tmp72FE TMPDocument8 pagestmp72FE TMPFrontiersNo ratings yet
- tmpF407 TMPDocument17 pagestmpF407 TMPFrontiersNo ratings yet
- tmpC0A TMPDocument9 pagestmpC0A TMPFrontiersNo ratings yet
- tmp60EF TMPDocument20 pagestmp60EF TMPFrontiersNo ratings yet
- tmp8B94 TMPDocument9 pagestmp8B94 TMPFrontiersNo ratings yet
- tmp6382 TMPDocument8 pagestmp6382 TMPFrontiersNo ratings yet
- tmp998 TMPDocument9 pagestmp998 TMPFrontiersNo ratings yet
- tmp4B57 TMPDocument9 pagestmp4B57 TMPFrontiersNo ratings yet
- tmp9D75 TMPDocument9 pagestmp9D75 TMPFrontiersNo ratings yet
- tmp37B8 TMPDocument9 pagestmp37B8 TMPFrontiersNo ratings yet
- tmpC30A TMPDocument10 pagestmpC30A TMPFrontiersNo ratings yet
- tmpD1FE TMPDocument6 pagestmpD1FE TMPFrontiersNo ratings yet
- tmpB1BE TMPDocument9 pagestmpB1BE TMPFrontiersNo ratings yet
- tmp3656 TMPDocument14 pagestmp3656 TMPFrontiersNo ratings yet
- tmpA0D TMPDocument9 pagestmpA0D TMPFrontiersNo ratings yet
- Tmp75a7 TMPDocument8 pagesTmp75a7 TMPFrontiersNo ratings yet
- tmp27C1 TMPDocument5 pagestmp27C1 TMPFrontiersNo ratings yet
- tmp2F3F TMPDocument10 pagestmp2F3F TMPFrontiersNo ratings yet
- Histology of Small Intestine 3Document17 pagesHistology of Small Intestine 3ShizraNo ratings yet
- Pathophysiology of Postpartum Hemorrhage and Third Stage of LaborDocument7 pagesPathophysiology of Postpartum Hemorrhage and Third Stage of Labornouval_iqbalNo ratings yet
- Erythropoiesis: Presented by DR Etu-Efeotor T. PDocument88 pagesErythropoiesis: Presented by DR Etu-Efeotor T. PPrincewill SeiyefaNo ratings yet
- Rat Catchers PDFDocument8 pagesRat Catchers PDFDavid FrostNo ratings yet
- Characteristics of Vibrio: Vibrio Cholera Vibrio Mimicus Vibrio FluvialisDocument4 pagesCharacteristics of Vibrio: Vibrio Cholera Vibrio Mimicus Vibrio FluvialisnurulnydaNo ratings yet
- FE ImbalanceDocument6 pagesFE ImbalanceDonna CortezNo ratings yet
- Foreign Bodies in The EarDocument6 pagesForeign Bodies in The EarGlorina KumarNo ratings yet
- CannulaDocument4 pagesCannulaAnonymous m0vrFqAsNo ratings yet
- Semen AnalysisDocument3 pagesSemen Analysisameerabest80% (5)
- Annotated Reading Dengue FeverDocument1 pageAnnotated Reading Dengue FeverGoRbz SarmientoNo ratings yet
- 5090 - w22 - QP - 12 Biology O-Level PypDocument20 pages5090 - w22 - QP - 12 Biology O-Level Pypmuiz phiNo ratings yet
- Rabbit Breeds Management and ClassificationDocument37 pagesRabbit Breeds Management and ClassificationAÿâñ Jitéñdrä Yãdáv100% (1)
- Plant Innate Immunity: Sub. - Biochem-506, IMMUNO CHEMISTRYDocument22 pagesPlant Innate Immunity: Sub. - Biochem-506, IMMUNO CHEMISTRYviralnanobio_4150420No ratings yet
- Chapter 8 MariebDocument5 pagesChapter 8 MariebmjhenkeNo ratings yet
- Anaesthesia For Paediatric Dentistry: Lola Adewale MBCHB DCH FrcaDocument8 pagesAnaesthesia For Paediatric Dentistry: Lola Adewale MBCHB DCH FrcaJavier Farias VeraNo ratings yet
- NCERT BookDocument10 pagesNCERT Bookkaushikray06No ratings yet
- CDC - Fasciola - BiologyDocument2 pagesCDC - Fasciola - BiologypecopecochanNo ratings yet
- Finding An Apartment Project: Background - Answer These Questions in Complete SentencesDocument4 pagesFinding An Apartment Project: Background - Answer These Questions in Complete Sentencesapi-288310744No ratings yet
- امتحان تجريبي للصف الحادي عشر -فترة رابعة-ورقة ثانيةDocument5 pagesامتحان تجريبي للصف الحادي عشر -فترة رابعة-ورقة ثانيةshehabedenNo ratings yet
- CRI Annual Report 2006Document10 pagesCRI Annual Report 2006aptureincNo ratings yet
- Assignment 1Document4 pagesAssignment 1Ashish YadavNo ratings yet
- Periodontal LigamentDocument3 pagesPeriodontal LigamentCzarina DavidNo ratings yet
- Dental Caries Booklet PDFDocument10 pagesDental Caries Booklet PDFIon BondariNo ratings yet
- TABLE (Ascaris, Trichuris, and Enterobius)Document3 pagesTABLE (Ascaris, Trichuris, and Enterobius)TRISHA MAE ORDONANo ratings yet
- SchistosomaDocument5 pagesSchistosomasarguss14100% (1)
- Vector - and Rodent-Borne Diseases in Europe and North America 2gfshDocument411 pagesVector - and Rodent-Borne Diseases in Europe and North America 2gfshRhyan ArfanNo ratings yet
- Scoliosis: Review of Diagnosis and Treatment: Janusz Popko, Michał Kwiatkowski, Monika GałczykDocument5 pagesScoliosis: Review of Diagnosis and Treatment: Janusz Popko, Michał Kwiatkowski, Monika Gałczykandi dirhanNo ratings yet
- 8.3.2 SPEAKING - Oral Presentation Rubric NAMEDocument4 pages8.3.2 SPEAKING - Oral Presentation Rubric NAMEapi-197465646No ratings yet
- Hand Foot Mouth Disease (HFMD) For TeachersDocument2 pagesHand Foot Mouth Disease (HFMD) For Teachersalbeny j.pNo ratings yet
- Group discusses case of heart failure in elderly womanDocument14 pagesGroup discusses case of heart failure in elderly womangalih suharnoNo ratings yet
- NO More Heart Disease: How Nitric Oxide Can Prevent--Even Reverse--Heart Disease and StrokesFrom EverandNO More Heart Disease: How Nitric Oxide Can Prevent--Even Reverse--Heart Disease and StrokesRating: 4 out of 5 stars4/5 (5)
- Sick Sinus Syndrome, (Sinus Nodal Disorder) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandSick Sinus Syndrome, (Sinus Nodal Disorder) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- The Pathophysiology and Pharmacotherapy of Myocardial InfarctionFrom EverandThe Pathophysiology and Pharmacotherapy of Myocardial InfarctionNabil El-SherifNo ratings yet
- Syncope, A Simple Guide to the Condition, Treatment and Related DiseasesFrom EverandSyncope, A Simple Guide to the Condition, Treatment and Related DiseasesNo ratings yet
- Atrial Fibrillation A Simple Guide to The Condition, Treatment And Related DiseasesFrom EverandAtrial Fibrillation A Simple Guide to The Condition, Treatment And Related DiseasesRating: 4 out of 5 stars4/5 (1)
- Essential Cardiac Electrophysiology: The Self-Assessment ApproachFrom EverandEssential Cardiac Electrophysiology: The Self-Assessment ApproachNo ratings yet
- Hemodynamic Rounds: Interpretation of Cardiac Pathophysiology from Pressure Waveform AnalysisFrom EverandHemodynamic Rounds: Interpretation of Cardiac Pathophysiology from Pressure Waveform AnalysisNo ratings yet
- Cardiac PharmacologyFrom EverandCardiac PharmacologyR. Douglas WilkersonRating: 5 out of 5 stars5/5 (1)
- Impedance Spectroscopy: Theory, Experiment, and ApplicationsFrom EverandImpedance Spectroscopy: Theory, Experiment, and ApplicationsEvgenij BarsoukovNo ratings yet
- Cardioversion, A Simple Guide To The Condition, Types, Treatment of Arrhythmias And Related ConditionsFrom EverandCardioversion, A Simple Guide To The Condition, Types, Treatment of Arrhythmias And Related ConditionsNo ratings yet
- Building Wellness with DMG: How A Breakthrough Nutrient Gives Cancer, Autism & Cardiovascular Patients A Second Chance at HealtFrom EverandBuilding Wellness with DMG: How A Breakthrough Nutrient Gives Cancer, Autism & Cardiovascular Patients A Second Chance at HealtRating: 5 out of 5 stars5/5 (1)
- Put Your Heart in Your Mouth: Natural Treatment for Atherosclerosis, Angina, Heart Attack, High Blood Pressure, Stroke, Arrhythmia, Peripheral Vascular DiseaseFrom EverandPut Your Heart in Your Mouth: Natural Treatment for Atherosclerosis, Angina, Heart Attack, High Blood Pressure, Stroke, Arrhythmia, Peripheral Vascular DiseaseRating: 4.5 out of 5 stars4.5/5 (5)
- Case Presentations in Arterial DiseaseFrom EverandCase Presentations in Arterial DiseaseRating: 5 out of 5 stars5/5 (1)
- Predicting Forex and Stock Market with Fractal PatternFrom EverandPredicting Forex and Stock Market with Fractal PatternRating: 4 out of 5 stars4/5 (4)
- Quantum Mechanics 2: Reality, Uncertainty, & Schrödinger’s CatFrom EverandQuantum Mechanics 2: Reality, Uncertainty, & Schrödinger’s CatRating: 5 out of 5 stars5/5 (4)