Professional Documents
Culture Documents
DIVERSE Study
Uploaded by
yashubyatappaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
DIVERSE Study
Uploaded by
yashubyatappaCopyright:
Available Formats
38
Journal of The Association of Physicians of India Vol. 64 April 2016
Original Article
DemographIc Assessment and EValuation of
DEgree of Lipid Control in High Risk Indian
DySlipidemia PatiEnts (DIVERSE Study)
Naresh Malhotra1, MK Keshan2, Avinash Agarwal3, R Anil Kumar4, Abhijit Trailokya5,
Kalpesh Dalvi 6, Suhas Talele7
Abstract
Editorial Viewpoint
Background: Cardiovascular diseases (CVDs) are the major cause of
morbidity and mortality in both developed and developing countries.
Many clinical trials have demonstrated that low-density lipoprotein
cholesterol (LDL-C) lowering, reduces the incidence of coronary and
cerebrovascular events across a broad spectrum of patients at risk.
Guidelines for the management of patients at risk have been established in
Europe and North America. The guidelines have advocated progressively
lower LDL-C targets and more aggressive use of statin therapy. In Indian
patients, comprehensive data on dyslipidemia management and its
treatment outcomes are inadequate. There is lack of information on
existing treatment patterns, the patients profile being treated, and
factors that determine treatment success or failure in achieving desired
goals.
High risk dyslipidemic
patients need intensive
lipid lowering therapy.
Purpose: The present study was planned to determine the lipid control
status in high-risk dyslipidemic patients treated with lipid-lowering
therapy in India.
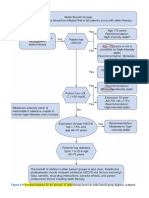
Methods: This cross-sectional, non-interventional, single visit program
was conducted across 483 sites in India where male and female patients
with high-risk dyslipidemia aged 18 to 65 years who had visited for a
routine health check-up to their respective physician at hospital or a
healthcare center. Percentage of high-risk dyslipidemic patients achieving
adequate LDL-C level (< 70 mg/dL) on lipid-lowering therapy and the
association of lipid parameters with patient characteristics, comorbid
conditions, and lipid lowering drugs were analysed.
Results: 3089 patients were enrolled in the study; of which 64% were
males. LDL-C data was available for 95.2% of the patients; only 7.7%
of these patients achieved LDL-C levels < 70 mg/dL on lipid-lowering
therapy, which may be due to inability to follow therapeutic plans, poor
compliance, or inadequate counselling by physician. The physicians lack
of awareness about recent treatment guidelines also might contribute
to patients poor adherence, not explaining adequately the benefit and
risks of a medication, not giving consideration to the patients life style
M o s t o f t h e h i g h r i s k
dyslipidemic Indian
patients are on suboptimal
dosage of statin.
Aggressive counselling
a n d
i n t e n s i v e
management are required
for appropriate lipid
management.
Introduction
ardiovascular diseases
(CVDs) are the major cause
of morbidity and mortality in
both developed and developing
countries. Dyslipidemia has been
identified as an independent risk
f a c t o r f o r t h e d e ve l o p m e n t o f
CVD. It may occur due to elevated
production or low clearance of
lipoproteins, apolipoproteins
defects or enzyme deficiencies,
or due to environmental factors
(such as saturated fat diet or
sedentary lifestyle), diseases (such
as diabetes, hypothyroidism, liver
disease), and medications (such as
thiazide diuretics, progestins, or
anabolic steroids).1 As per European
Society of Cardiology (ESC) and the
European Atherosclerosis Society
Aditya Hospital, Ahmedabad, Gujarat; 2MK Keshan Clinic, Guwahati, Assam; 3Agarwal Poly Clinic, Jaipur, Rajasthan; 4Vismaya Diabetes Care Centre, Bangalore, Karnataka;
Chief Manager Cardiology, 6Medical Adviser, 7Manager-Clinical Research, Abbott Healthcare Private Limited, Mumbai, Maharashtra
Received: 09.11.2015; Accepted: 02.03.2016
1
5
Journal of The Association of Physicians of India Vol. 64 April 2016
and the cost of medication. Statin was the most commonly used antidyslipidemic drug across population. The higher proportion of patients
had the comorbid condition of CVD and diabetes mellitus across all
dyslipidemic patients.
Conclusion: As per the European Society of Cardiology guidelines the
ideal LDL-C levels in high risk dyslipidemic patients should be less than
70 mg/dL. In the present study, 7.7% of the patients achieved LDL-C levels
< 70 mg/dL on lipid lowering therapy which is very less. Most of high risk
dyslipidemic patients in India are on suboptimal dosage of statin. So more
aggressive and high dosage statin therapy may be required to achieve
target LDLC levels in high risk Indian dyslipidemic patients.
Guidelines (EAS), a high-risk
dyslipidemic patient is defined as
a person with known CVD, and
type 2 or type 1 diabetes mellitus
(DM) with microalbuminuria and
chronic kidney disease (CKD).
Pa t i e n t s i n h i g h - r i s k c a t e g o r y
have CVD or DM plus one or more
coronary heart disease risk factors
in addition to dyslipidemia. 2 There
exist an independent and strongly
p o s i t i ve r e l a t i o n s h i p b e t we e n
dyslipidemia and risk of CV death.3
Every individuals LDL-C treatment
goal is determined by his or her
absolute CVD risk. Elevated LDL-C
level suggests a higher risk of CVD,
hypertension, DM and obesity. 4,5
Dietary improvements (saturated
fat <7% of calories, cholesterol
<200 mg/day; soluble fiber 10-25
g/day and plant stanols/sterols 2g/
day) and lifestyle changes (weight
reduction and increased physical
activity) constitute the therapeutic
options to enhance LDL lowering. 6
In cases where these efforts fail
to achieve the target LDL-C goal,
the patients are treated by lipidlowering therapy with/without
lifestyle modification.7 Many
clinical trials have demonstrated
t h a t L D L - C l o we r i n g , r e d u c e s
th e i n c i de n c e of c oronary an d
cerebrovascular events across a
broad spectrum of patients at risk.
Statins have been recommended
as the first-line treatment and
considered as the most effective
p h a r m a c o t h e r a p y f o r e l e va t e d
LDL-C; their use has been associated
with significant improvement in
CVD outcomes. In cases where
the target goal is not achieved,
the LDL-lowering therapies are
intensified by either increasing
the dose or by combination with
other lipid lowering therapies (e.g.
Fibrates, bile acid sequestrants,
ezetimibe, nicotinic acid etc)
along with diet optimization and
aggressive physical activity. The
major reasons for patients not
able to achieve LDL-C goal may
be due to their inability to follow
their therapeutic plan, poor or low
treatment adherence/compliance,
not able to tolerate prescribed dose
of medication, or genetic causes. In
addition, physicians do not have
enough time for extensive patient
counselling or schedule a training
session to explain the role of
treatment compliance, lifestyle, and
diet in achieving the LDL-C goals.
If the LDL-C goal is not attained by
standard lipid-lowering therapy,
consideration should be given to
seeking consultation from a lipid
specialist. 6 In addition to LDL-C,
some guidelines also highlight high
density lipoprotein cholesterol
(HDL-C)/total cholesterol (TC) and
non-HDL-C as secondary goals
of the therapy as their abnormal
levels are associated with increased
chronic heart disease risk.
Reference guidelines
(American Association of Clinical
Endocrinologists; ESC/EAS) for the
management of patients at risk have
been established in Europe and
North America. These guidelines
h a ve a d v o c a t e d p r o g r e s s i ve l y
lower LDL-C targets and more
aggressive use of statin therapy.
In Indian patients, comprehensive
39
data on dyslipidemia management
and its treatment outcomes are
inadequate. There is lack of
information on existing treatment
patterns, the patients profile
being treated, and factors that
determine treatment success
or failure in achieving desired
goals. In addition, there is poor
awareness of treatment strategies
in physicians with respect to
treatment of high risk dyslipidemic
patients in India. The therapeutic
goals for patients with very high
cardiovascular risk include LDL-C
levels less than 70 mg/dL or at
least a 50% relative reduction in
LDL-C when target level cannot
be achieved. 8 However, despite
guideline recommendations, there
is a growing evidence of suboptimal
use of lipid-lowering treatment. 9
T h e f a i l u r e t o a c h i e ve L D L - C
goal is most commonly attributed
to patient non-compliance with
Table 1: Patient characteristics
Category
Gender, n (%)1
Female, age groups
18-25
26-35
36-45
46-55
56-65
Male, age groups
18-25
26-35
36-45
46-55
56-65
Life style
Non-sedentary
Sedentary
Diet
Non-vegetarian
Vegetarian
Age (years)
Height (cm)
Weight (kg)
Body mass index (kg/m2)
Waist circumference (cm)
Laboratory test
HbA1c (%)
FPG (mg/dL)
PPG (mg/dL)
No. of pts.
(N = 3089)
1116 (36.1)
2 (0.2)
26 (2.3)
202 (18.1)
380 (34.1)
506 (45.3)
1973 (63.9)
3 (0.2)
36 (1.8)
269 (13.6)
758 (38.4)
907 (45.1)
1411 (45.7)
1677 (54.3)
1455 (47.1)
1634 (52.9)
53.57.7
163.98.5
72.89.6
27.24.0
92.98.9
7.41.73
126.035.4
186.562.6
Values as: No. of patients (%), mean SD
40
Journal of The Association of Physicians of India Vol. 64 April 2016
900
768
(24.9%)
662
(21.4%)
700
600
500
36-45 46-55 46-55
Normal
18-25 26-35 26-35
36-45 36-45 46-55
Female
Male
Male
132
(4.3%)
89
(2.9%)
17
(0.6%)
Female
Male
56-65
Female
56-65
Female
Male
26-35 26-35 36-45
18
2
2
(0.1%) (0.6%) (0.1%)
Female
18-25
123
(4%)
Female
Female
34
8
3
(1.1%)
(0.1%) (0.3%)
Male
100
139
(4.5%)
76
(2.5%)
Female
200
Male
300
306
(9.9%)
239
(7.7%)
46-55 56-65
Male
250
(8.1%)
Female
400
Male
No. of subjects (percentage)
800
56-65
Above normal
Waist circumference (cm)
Fig. 1: Age and gender-wise distribution of waist circumference
250
214.5
(1063)
209.5
(1926)
211.3
(2989)
187.7
(994)
Mean (No. of subjects)
200
132.9
(1098)
150
128
(1981)
185.5
(1867)
186.3
(2861)
Male
Overall
129.7
(3079)
100
50
43.8
(984)
44.5
(1860)
44.3
(2844)
1.7
(1033)
Female
Male
Overall Female
HDL-C (mg/dl)
Male
Overall Female
LDL-C (mg/dl)
1.7
(1857)
1.7
(2890)
Male
Overall Female
TC/LDL ratio
Male
Overall Female
Total cholesterol (mg/dl)
Triglycerides (mg/dl)
Lipid prole prameters
Fig. 2: Gender-wise mean values of lipid profile parameters
drug treatment regimen and poor
physician adherence to treatment
guidelines. 10 Other reasons for
poor achievement of LDL-C goal
include insufficient dosing, failure
to adequately up titrate the dose,
not switching to a more potent drug
when essential, and lack of follow-up
after initiation of treatment. In
Indian patients, comprehensive
data on dyslipidemia management
and its treatment outcomes are
inadequate. There is lack of
information on existing treatment
patterns, the patients profile being
treated, and factors that determine
treatment success or failure in
achieving desired LDL-C goals.
H e n c e , t h e p r e s e n t s t u d y wa s
designed to determine the lipid
control in high-risk dyslipidemic
Indian patients treated with lipidlowering therapy.
Methods
This cross-sectional, noninterventional, single visit study
was conducted between January
2014 to September 2014 at 483 sites
all-over India. Patients diagnosed
for high-risk dyslipidemia aged
n (%)
1 (100.0)
507 (18.7)
453 (19.4)
2 (11.1)
1 (50.0)
50 (14.9)
1 (33.3)
1 (33.3)
9 (29.0)
7 (28.0)
2 (33.3)
27 (8.1)
27 (8.3)
1 (20.0)
1 (20.0)
1 (100.0)
1 (100.0)
1 (50.0)
-
1 (50.0)
-
1861 (68.5) 972 (35.8) 1171 (43.1) 232 (8.5)
1626 (69.5) 840 (35.9) 1023 (43.8) 183 (7.8)
16 (88.9)
9 (50.0)
1 (5.6)
3 (16.7)
18 (100.0)
9 (50.0)
3 (16.7)
1 (50.0)
1 (50.0)
1 (50.0)
198 (58.9) 121 (36.0) 136 (40.5) 43 (12.8)
2 (66.7)
1 (33.3)
1 (33.3)
1 (33.3)
1 (33.3)
1 (33.3)
-
14 (4.2)
13 (4.0)
1 (10.0)
-
HDL-C (mg/dL)
<40
40-59
60
1 (100.0)
-
19 (61.3) 16 (51.6)
8 (25.8)
18 (72.0) 14 (56.0)
5 (20.0)
1 (16.7)
2 (33.3)
3 (50.0)
284 (85.0) 128 (38.3) 164 (49.1)
277 (85.5) 125 (38.6) 161 (49.7)
7 (70.0)
3 (30.0)
3 (30.0)
4 (80.0)
1 (20.0)
4 (80.0)
1 (20.0)
-
1 (100.0)
LDL-C (mg/dL)
<70
70-100
>100
1 (100.0)
Ezetimibe w/
1 (0.03)
Fibrates w/ Statins
Atorvastatin, Ezetimibe,
1 (0.03)
Fenofibrate
Fibrates
31 (1.00)
2 (6.5)
Clofibrate
25 (0.8)
Fenofibrate
6 (0.2)
2 (33.3)
Fibrates w/ Statins
334 (10.8) 11 (3.3)
Atorvastatin, Fenofibrate 324 (10.5) 11 (3.4)
Fenofibrate, Rosuvastatin 10 (0.3)
Nicotinic acid w/ Statins
5 (0.2)
Atorvastatin,
5 (0.2)
Nicotinic acid
Statins
2715 (87.9) 213 (7.8)
Atorvastatin
2338 (75.7) 143 (6.1)
Fluvastatin
18 (0.6)
Lovastatin
18 (0.6)
Pitavastatin
2 (0.1)
Rosuvastatin
336 (10.9) 70 (20.8)
Simvastatin
3 (0.1)
Statins w/
3 (0.1)
other combinations
Acetylsalicylic acid,
2 (0.1)
Atorvastatin
Acetylsalicylic acid,
1 (0.03)
Atorvastatin,
Atorvastatin calcium
No. of patients (%); $Mean SD
Classification /
generic name
Table 2: Association of lipid lowering drugs with lipid parameters
19 (61.3)
18 (72.0)
1 (16.7)
54 (16.2)
51 (15.7)
3 (30.0)
1 (20.0)
1 (20.0)
1 (100.0)
6 (19.4)
2 (8.0)
4 (66.7)
219 (65.6)
216 (66.7)
3 (30.0)
-
1 (100.0)
1 (50.0)
752 (27.7) 959 (35.3) 676 (24.9)
639 (27.3) 838 (35.8) 582 (24.9)
1 (5.6)
5 (27.8)
8 (44.4)
3 (16.7)
7 (38.9)
2 (11.1)
1 (50.0)
109 (32.4) 106 (31.5) 84 (25.0)
2 (66.7)
2 (66.7)
1 (3.2)
1 (4.0)
29 (8.7)
28 (8.6)
1 (10.0)
1 (20.0)
1 (20.0)
<150
-
TGs (mg/dL)
150-199
200-499
1 (100.0)
-
3 (0.1)
3 (0.1)
-
5 (1.5)
5 (1.5)
-
500
-
8 (25.8)
7 (28.0)
1 (16.7)
78 (23.4)
76 (23.5)
2 (20.0)
-
7 (22.6)
7 (28.0)
169 (50.6)
167 (51.5)
2 (20.0)
2 (40.0)
2 (40.0)
1.89 (0.6)
1.77 (0.4)
2.49 (0.9)
1.77 (0.5)
1.77 (0.5)
1.70 (0.2)
1.37 (0.2)
1.37 (0.2)
1.12 (-)
1.12 (-)
TC/LDL
ratio$
1 (100.0)
1 (50.0)
2.14 (-)
1.43 (-)
1132 (41.7) 669 (24.6) 708 (26.1) 1.72 (0.6)
959 (41.0) 590 (25.2) 602 (25.7) 1.71 (0.6)
2 (11.1)
9 (50.0)
7 (38.9) 1.50 (0.3)
9 (50.0)
4 (22.2)
5 (27.8) 1.47 (0.2)
1 (50.0)
1 (50.0) 2.14 (1.4)
159 (47.3) 65 (19.3) 93 (27.7) 1.82 (0.7)
2 (66.7)
1 (33.3)
1.64 (0.4)
1 (33.3)
1 (33.3) 1.79 (0.5)
15 (48.4)
11 (44.0)
4 (66.7)
65 (19.5)
62 (19.1)
3 (30.0)
3 (60.0)
3 (60.0)
1 (100.0)
Total cholesterol (mg/dL)
<200
200-239
240
1 (100.0)
-
Journal of The Association of Physicians of India Vol. 64 April 2016
41
18 to 65 years and prescribed
lipid-lowering therapy for at
least 3 months with no dose
adjustments for at least 6 weeks
prior to study enrollment were
enrolled in the study. Patients
who did not have their recent
lipid profile (within 15 days)
a n d / o r we r e n o t w i l l i n g t o
provide lipid profile; pregnant
or lactating; or were currently
participating in other trial
or had participated in any of
the clinical trial in the past 3
months were excluded from the
study. The primary objective
of the study was to determine
the lipid control in high-risk
dyslipidaemic Indian patients
t r e a t e d w i t h l i p i d - l o we r i n g
therapy. The secondary
objectives of the study were to
understand the demographic
profile, treatment modalities,
co-morbidities, and to identify
potential determinants in
achieving defined LDL-C levels
in patients with high-risk
dyslipidemia. The protocol was
approved by the independent/
institutional ethics committee.
The study was conducted in
accordance with the Declaration
of Helsinki and International
Conference on Harmonization
of Good Clinical Practice
guidelines with Cardiologists/
Consulting Physicians with
e x t e n s i ve e x p e r i e n c e i n t h e
management of dyslipidemia.
For each patient, the
investigator recorded the
following information in
web based case report form:
patients demographics
(age, gender, height, weight,
body mass index, and waist
circumference), lifestyle
(sedentary and non-sedentary),
dietary patterns (vegetarian and
non-vegetarian), risk categories
(CVD, cerebrovascular disease,
CKD, and DM), medical history,
lipid profile (LDL-C, HDL-C,
triglycerides [TGs], TC, and
TC/LDL ratio), lipid lowering
therapy (statins, fibrate, nicotinic
42
Journal of The Association of Physicians of India Vol. 64 April 2016
654
(30.1%)
700
530
(24.4%)
500
361
(16.6%)
400
286
(13.2%)
300
26-35
36-45
46-55
56-65
18-25
26-35
<70
36-45
46-55
56-65
18-25
26-35
36-45
Male
Female
Male
Female
Male
Female
Male
Female
Male
Female
18
16
1
1
(0.8%) (0.7%)
(0%) (0%)
Male
Female
Male
Female
Male
Female
Male
Female
Male
Female
Male
Female
Male
Female
Male
Female
79
(14.5%)
70
57
59
36 (12.8%) 44
31 (26.1%) 39 (25.2%)
15
16
11 (6.6%)
(8.1%)
7
(17.3%)
2
4
2
1
(13.7%)
(0.9%) (3.1%) (6.6%) (7.1%)
(0.2%) (0.4%) (0.7%) (2%)
Male
100
165
138 (7.6%)
(6.4%)
158
(29%)
140
(25.7%)
200
Female
No. of subjects (percentage)
600
46-55
56-65
>100
70-100
LDL-C levels (mg/dl)
Fig. 3: Age and gender-wise distribution of LDL-C levels
2338
(75.7%)
No. of subjects (percentage)
2500
2000
1500
1000
500
0
25
(0.8%)
6
(0.2%)
Clo
Feno
336
(10.9%)
18
(0.6%)
18
(0.6%)
2
(0.1%)
Fluv
Lova
Pit
Ator
Fib
Rosu
3
(0.1%)
Sim
1
(0%)
Ator, Eze, Ator,
Feno
Feno
Eze w/
Fib w/
Stat
Stat
324
(10.5%)
10
(0.3%)
5
(0.2%)
2
(0.1%)
1
(0%)
Feno,
Rosu
Ator, Nic
Acet,
Ator
Acet,
Ator,
Ator C
Fib w/ Stat
Nic w/
Stat
Stat w/ other
Medication for dyslipidemia
Fig. 4: Medication for dyslipidemia
acid, ezetimibe, and combination
therapy), vital parameters (systolic
and diastolic blood pressure),
laboratory investigations (fasting
plasma glucose [FPG], postprandial
glucose [PPG] levels, and glycated
hemoglobin [HbA1c]), and
concomitant medications.
Study Endpoint
The primary study endpoint
was to evaluate the percentage of
high-risk dyslipidemia patients
achieving adequate LDL-C level
(< 70 mg/dL) on lipid-lowering
therapy. The secondary study
e n d p o i n t wa s t o e va l u a t e t h e
association of lipid parameters with
patient characteristics, comorbid
conditions, and lipid lowering
drugs.
Statistical Analysis
As this was a non-interventional
study, no formal sample size
c a l c u l a t i o n wa s d o n e . A l l t h e
enrolled patients were analysed in
the study. The statistical analysis
was done using Statistical Analysis
System version 9.3 software. The
data was summarized descriptively.
Results
Patient Characteristics
3089 (70.4%) patients were
enrolled in the study and
constituted the analysis population.
1973 (64%) of the patients were
males while 1116 (36%) were
females. Higher proportion of
patients (46%) in males and females
Journal of The Association of Physicians of India Vol. 64 April 2016
561
(24%)
600
No. of subjects (percentage)
500
433
(18.5%)
367
(15.7%)
400
300
228
(9.8%)
184
(7.9%)
200
100
0
43
39
(1.7%)
49
(2.1%)
Female
Male
Female
Male
43-65 years
18-42 years
10
37
(1.6%)
44
(1.9%)
Female
Male
Female
18-42 years
Male
11
(0.5%)
18
(0.8%)
Female
Male
43-65 years
79
(3.4%)
2
(0.1%)
Female
18-42 years
43-65 years
40
20
Male
Male
43-65
years
80
Atorvastatin dose (mg)
Fig. 5: Age and gender-wise distribution of patients in different dose levels of atorvastatin
category were aged 56-65 years
followed by patients of age 46-55
ye a r s . S e d e n t a r y l i f e s t yl e a n d
vegetarian diet was reported in
higher proportion of females
a g e d 5 6 - 6 5 ye a r s c o m p a r e d t o
other age categories. The patients
characteristics are summarized
in Table 1. Waist circumference
above normal (pre-obese/obese)
was reported in higher proportion
of females of age category 36 to 65
years than males of the same age
category (Figure 1).
Lipid Profile
The mean value of LDL-C (130.8
41.8 mg/dL), HDL-C (44.5 22.2
mg/dL), TG (187.4 72.9 mg/dL),
TC/LDL-C ratio (1.7 0.6 mg/
d L) , a n d T C ( 2 1 2 . 2 5 4 . 8 m g /
dL) were recorded, respectively.
T h e m e a n L D L - C va l u e s we r e
comparable between males and
females. Similarly, mean HDL-C,
TG, TC/LDL-C ratio, and TC was
also comparable between males and
females (Figure 2). Overall, LDL-C
data was available for 2941 of
3089 (95.2 %) patients. Out of 2941
patients, 226 (7.7%) patients (males:
139 [61.5 %]; females: 87 [38.5 %])
achieved LDL-C levels < 70 mg/dL
on lipid-lowering therapy (Table 2).
Higher number of males aged 26-35,
46-55, and 56-65 years achieved
LDL-C < 70 mg/dL than females.
The level of LDL-C < 70 mg/dL was
comparable in males and females of
age 36-45 years. 545 of 2941 (18.5
%) patients (381 males and 164
females) achieved LDL-C levels
between 70-100 mg/dL. Higher
number of males aged 36-45, 46-55,
and 56-65 years achieved the LDL-C
level 70-100 mg/dL as compared
to females of the same age groups.
The level of LDL-C 70-100 mg/
dL was comparable in males and
females of age 18-25 and 26-35
years (Figure 3).
Percentage of Patients on Lipid
Lowering Therapy
All 3089 patients received either
statin, fibrates, statins with fibrates,
statins with nicotinic acid, or statins
with other combination as the lipid
lowering therapy. 87.9% patients
received statins; with Atorvastatin
being the most common statin used
by the patient population (86.1%)
(Figure 4).
Association of Lipid-Lowering Therapy
with Lipid Parameters
88% (2715/3089) of patients
received statins. Atorvastatin was
the most common statin used (86%)
followed by Rosuvastatin (13%),
Fluvastatin (0.7%) and Lovastatin
(0.7%). The other drugs received
by the patients includes either
fibrates (1%), fibrates with statins
(10.8%), nicotinic acid with statins
(0.2%), ezetimide with fibrates
and statins (0.03%), or statins with
other combination as the lipid
lowering therapy (0.1%) (Table
2). Overall, Atorvastatin was the
most common statin used by 86%
patients (2338/2715 patients) with
10 mg dose (43.5%, 1016/2338
patients) as the most commonly
used dose followed by 20 mg dose
(31.7%, 742/2338 patients); genderwise, higher proportion of males
than females of age category 43-65
years were on atorvastatin doses
10 to 80 mg (Figure 5). Atorvastatin
was found to be effective statin in
achieving LDL-C < 70 mg/dL (141
[4.6%] patients), LDL-C 70-100
mg/dL (453 [14.7%] patients),
HDL-C 40-59 mg/dL (1014 [32.8%]
patients), HDL 60 mg/dL (180
[5.8%] patients), TG < 150 mg/dL
(630 [20.4%] patients), TG 150-199
mg/dL (833 [27%] patients), TC <
200 mg/dL (948 [30.7%] patients),
44
Journal of The Association of Physicians of India Vol. 64 April 2016
Table 3: Association of lipid modifying therapy with patient characteristics
Classification
n (%)
Age
mean (SD)
BMI (kg/m2)
mean (SD)
Ezetimibe w/
Fibrates w/ Statins
Fibrates
1
(0.03)
31
(1.00)
334
(10.81)
5
(0.16)
2715
(87.89)
3
(0.10)
55.0
(.)
54.6
(6.77)
54.4
(7.76)
49.8
(15.06)
53.3
(7.67)
55.7
(4.04)
24.80
(.)
25.17
(3.179)
28.15
(5.421)
26.44
(3.710)
27.09
(3.827)
25.63
(1.097)
Fibrates w/ Statins
Nicotinic acid w/
Statins
Statins
Statins w/ other
combinations
and TC 200-239 mg/dL (587 [19%]
patients).
Association of Lipid Modifying Therapy
with Patient Characteristics
Gender-wise, the proportion
of males using Fibrates with or
without statins, and only statins
was higher than females (fibrates:
males, 83.9%, females, 16.1; fibrates
with statins: males, 67.7%, females,
32.3%; statins: males, 63.3%,
females, 36.7%) and the proportion
of females using nicotinic acid
with statins and statins with
other combinations was higher
than males (Nicotinic acid with
statins: males, 40%, females, 60%;
statins with other combinations:
males, 33.3%, females, 66.7%). The
higher proportion of patients using
Ezetimibe with fibrates and statins,
Fibrates with or without statins,
nicotinic acid with statins, and
statins with other combination had
a sedentary lifestyle and vegetarian
diet.
Co-morbid Conditions
The most common risk categories
were CVD (70.5%; 2177/3089) and
DM (69.7%; 2152/3089). Genderwise, males are in between age
43-65 years had a high incidence of
CVD (59.3% versus 31.8%) and DM
(56.5% versus 33.1%) than females
of same age category (Figure 6).
The most common concomitant
medication was anti-diabetic drugs
(1731 [65.4%] patients) and renin
angiotensin system inhibitors (1132
[42.8%] patients). Metformin (1066
[61.6%] patients) and Glimepiride
Gender, n (%)
Male
Female
1
(100.0)
5
(16.1)
108
(32.3)
3
(60.0)
997
(36.7)
2
(66.7)
26
(83.9)
226
(67.7)
2
(40.0)
1718
(63.3)
1
(33.3)
Lifestyle, n (%)
NonSedentary
sedentary
1
(100.0)
21
10
(67.7)
(32.3)
266
68
(79.6)
(20.4)
3
2
(60.0)
(40.0)
1383
1331
(50.9)
(49.0)
3
(100.0)
(667 [38.5%] patients) were the
most common anti-diabetic drugs.
Telmisartan (742 [65.5%] patients)
and Olmesartan (254 [22.4%]
patients) were the most common
renin-angiotensin system inhibitors
used.
Association of Comorbid Conditions
with Defined Lipid Parameters
CVD and DM were reported
as the most common comorbid
conditions in patients who achieved
the LDL-C < 70 mg/dL and LDL-C
70-100 mg/dL (Table 4).
Discussion
Dyslipidemia as a common
health problem in India. As per
ESC/EAS guideline, a patient with
high-risk dyslipidemia is defined
as the person with known CVD,
type 2 or type 1 diabetes with
microalbuminuria, CKD, or with
very high levels of individual risk
factors. Prevalence of dyslipidemia
is reported to be higher in males
compared to females in India. 11
Higher (64%) number of the
p a t i e n t s we r e m a l e s a n d a g e d
more than 46 years in our study. In
2006, Goff et al. reported that men
had 30% more likelihood to have
dyslipidemia than women with
higher proportion of dyslipidemic
patients (both genders) in the older
age groups.12 The reason for having
dyslipidemia in higher proportion
of aged population may be due
to their high sedentary activities
and lack of physical exercise,
altered dietary habits, abnormal
Diet, n (%)
Veg
Non-veg
1
(100.0)
20
(64.5)
264
(79.0)
3
(60.0)
1343
(49.5)
3
(100.0)
11
(35.5)
70
(21.0)
2
(40.0)
1372
(50.5)
-
lipid profile, etc. Hence, lifestyle
modifications or lipid-lowering
drugs help in management of
dyslipidemia patients. Both
s e d e n t a r y l i f e s t yl e a n d t r a n s unsaturated fatty acid diet lead
to an increase in body weight and
hence increases the risk for CVD
either directly or by influencing
the lipid profile. We found females
of age 46-65 years to have a more
sedentary lifestyle and a higher
waist circumference than males
along with lower proportion to
a c h i e ve a d e q u a t e l i p i d l e ve l s
(LDL-C < 70 mg/dL, LDL-C 70-100
mg/dL, HDL-C 60 mg/dL, TC <
200 mg/dL, TG < 150 mg/dL, and
TG 150-199 mg/dL); which may be
due to insufficient dosing, failure
to adequately up titrate the dose,
not switching to a more potent
drug when essential, and lack
of follow-up after initiation of
treatment.
As per ESC/EAS guideline,
treatment target for LDL-C for a
high-risk dyslipidemic patient was
< 70 mg/dL or a 50 % reduction
from baseline LDL-C. Of all the
lipid-lowering drugs, statins have
been considered as the mainstay
at lowering the LDL-C levels in
dyslipidemic patients acts by
reducing the cholesterol synthesis
i n t h e l i ve r a n d s u b s t a n t i a l l y
reducing cardiovascular-associated
morbidity and mortality. In a
Cholesterol Treatment Trialists
Collaboration (CTT) meta-analyses
of > 170000 participants in 26
randomized trials of statins, per
Journal of The Association of Physicians of India Vol. 64 April 2016
1290
(59.3%)
1400
1215
(56.5%)
1200
No. of subjects (percentage)
45
1000
713
(33.1%)
693
(31.8%)
800
600
400
200
0
25
13
(34.2%) (65.8%)
Female
Male
43-65
65
(3%)
Female
129
(5.9%)
Male
18-42
Female
Male
98
(4.6%)
126
(5.9%)
Female
Male
18-42
43-65
Male
43-65
DM (n=2152)
CVD (n=2177)
CBD (n=38)
Female
1
(4.8%)
12
8
(38.1%) (57.1%)
Male
Female
18-42
Male
43-65
CKD (n=21)
Risk categories
Fig. 6: Age and gender-wise distribution of co-morbid conditions
Table 4: Association of comorbid
conditions with defined lipid
parameters
Lipid
Comorbid
parameter
conditions
LDL-C (mg/dL)
< 70
CVD
DM
70-100
CVD
DM
HDL-C (mg/dL)
40-59
CVD
DM
60
CVD
DM
Triglycerides (mg/dL)
<150
CVD
DM
150-199
CVD
DM
TC (mg/dL)
200-239
CVD
DM
Number of
patients (%)
126 (55.8)
174 (77.0)
394 (72.3)
347 (63.7)
951 (70.7)
931 (69.2)
152 (61.8)
187 (76.0)
559 (71.4)
546 (69.7)
718 (69.4)
687 (66.4)
549 (72.7)
492 (65.2)
Cardiovascular disease included ischemic
heart disease, peripheral arterial disease,
hypertension and cardiovascular disease
1 mmol/L LDL-C reduction was
associated with 10 % proportional
reduction in all-cause mortality
and 20 % proportional reduction
in coronary artery disease death. 13
A meta-analysis of randomized
clinical trials have reported that
the use of Statins in patients
without CVD but with risk factors
was associated with improved
s u r v i va l a n d r e d u c t i o n i n t h e
r i s k o f C V e v e n t s . 14 H i g h e r
proportion of patients on statins
had attained LDL-C goal with
lower cardiovascular outcomes
previously. 15 In our study as well,
statin was the most commonly
used drug in the management of
dyslipidemia. Approximately 7.7%
of the patients achieved LDL-C < 70
mg/dL compared to 19% patients
with LDL-C 70-100 mg/dL. On the
contrary statin monotherapy (for >
90 days) had also achieved LDL-C
< 100 mg/dL (67% to 77%) than
LDL-C < 70 mg/dL (20% to 26%
patients) in higher proportion of
high-risk dyslipidemic patients. 16
The present study results show
that lipid management remains
unsatisfactory in high-risk
dyslipidemia patients. The reason
for low proportion of patients to
have adequate LDL-C level may
be due to their drug intolerance,
inability to follow therapeutic
plans or poor compliance. In
addition, physicians play a major
role in achieving the target LDL-C
goal in their patients by extensive
counselling to improve their
treatment adherence. However they
often, fail to titrate medications,
choose inappropriate drug with
limited effectiveness, or are unable
to address patient noncompliance.
Clinical benefit is only dependent
on the extent of LDL-C lowering
rather than on the type of statin.
The statin chosen should provide
appropriate percent reduction of
LDL-C required to reach the target
goal in a given patient. 13,17
Our study had few limitations.
It was an observational study and
did not give any information on
treatment compliance, duration of
treatment, types of sedentary and
non-sedentary activities, and type
of fats in the diet. It was a single
v i s i t n o n - i n t e r ve n t i o n a l s t u d y
which did not provide the lipid
values over time. Only high-risk
dyslipidemic patients who were
o n l i p i d l o we r i n g d r u g s we r e
selected in the study; hence the
lipid profile of patients without
lipid lowering drugs cannot be
evaluated. The data of lipid profile
was taken from patient medical
records without routine blood
sample collection or central, corelaboratory evaluation; moreover,
the study reflected a more real world practice in which patients
with high-risk dyslipidemia who
presented themselves for routine
46
Journal of The Association of Physicians of India Vol. 64 April 2016
health check-up to their treating
physician were enrolled. The
strength of our study was that it
presented a real-world Indian
data in a big cross-sectional setting.
Conclusion
As per the ESC guidelines the
ideal LDL-C levels in high risk
dyslipidemic patients should be
less than 70 mg/dL. In the present
study, only 7.7% of the patients
achieved LDL-C levels < 70 mg/
dL with lipid lowering therapy.
Despite the availability of statins,
lipid management in high-risk
patients remains unsatisfactory.
The reasons for poor achievement
of LDL-C goals may be due to
inability to follow therapeutic plans,
poor compliance, or inadequate
counselling by physician. The
p h y s i c i a n s l a c k o f a wa r e n e s s
about recent treatment guidelines
also might contribute to patients
poor adherence, not explaining
adequately the benefit and risks
of a medication, not giving
consideration to the patients life
style and the cost of medication.
Hence, a more aggressive patients
counselling and treatment is
r e q u i r e d t o a c h i e ve t h e t a r g e t
lipid goals.
Acknowledgements
The authors would like to thank
all doctors who participated in this
study. The authors would also like
to acknowledge site management
organization and medical
writing agency (Max-Neeman
International) for their efforts.
We are also like to thank Dr. Amit
Bahulayan PhD (Pharmacology)
and Dr. Jyotirmoy Paul MD
(Pharmacology) for reviewing the
manuscript.
Disclosure
This study was funded by Abbott
Healthcare Pvt Ltd. Dr. Abhijit
Trailokya, Chief Manager- Medical
Services, Dr. Kalpesh Dalvi,
Medical Advisor- Medical Services,
Mr. Suhas Talele, Manager-Clinical
Research; Medical Services all are
employees of Abbott Healthcare
Private Limited, Mulund, Mumbai.
References
1.
Kingsbury KJ, Bondy G. Understanding the
essentials of blood lipid metabolism. Prog
Cardiovasc Nurs2003; 18:13-8.
2.
Wei YQ. Treating dyslipidemia in high-risk
group patients- current management and
future approach. Singapore Fam Physician
2011; 37:18-24.
3.
Ford I, Murray H, Packard CJ, Shepherd
J, Macfarlane PW, Cobbe SM. Long-term
follow-up of the West of Scotland Coronary
Prevention Study. N Engl J Med 2007;
357:1477-86.
4.
Gaziano TA, Bitton A, Anand S, AbrahamsGessel S, Murphy A. Growing epidemic of
coronary heart disease in low- and middleincome countries. Curr Probl Cardiol 2010;
35:72-115.
5.
6.
7.
8.
Gersh BJ, Sliwa K, Mayosi BM, Yusuf S. Novel
therapeutic concepts: the epidemic of
cardiovascular disease in the developing
world: global implications. Eur Heart J 2010;
31:642-8.
ATP III At-A-Glance: Quick Desk Reference,
2001. Available from: http://www.nhlbi.
nih.gov/health-pro/guidelines/current/
cholesterol- guidelines/quick- deskreference-html
Exper t D yslipidemia Panel of the
International Atherosclerosis Society Panel
members. An International Atherosclerosis
Society Position Paper: global
recommendations for the management of
dyslipidemia--full report. J Clin Lipidol2014;
8:29-60.
Reiner Z, Catapano AL, De Backer G,
Graham I, Taskinen MR, Wiklund O, et al.
ESC/EAS guidelines for the management of
dyslipidaemias. Eur Heart J 2011; 32:17691818.
9.
Goodman SG, Langer A, Bastien NR,
McPherson R, Francis GA, Genest JJ,
et al. Prevalence of dyslipidemia in
statintreated patients in Canada: Results
of the DYSlipidemia International Study
(DYSIS). Can J Cardiol 2010; 26:e330-e335.
10. Vashitz G,Meyer J,Parmet Y,Henkin Y,Peleg
R, Gilutz H. Physician adherence to the
dyslipidemia guidelines is as challenging
an issue as patient adherence. Fam
Pract2011; 28:524-31.
11. Karnik R, Trailokya A, Dalvi K, Patel K.
Efficacy evaluation and safety assessment
of Rosuvastatin 40mg treatment in high
risk dyslipidemic patients (Earth Study).
Indian Medical Gazette 2015; 149:314-19.
12. Goff DC Jr, Bertoni AG, Kramer H, et al.
Dyslipidemia prevalence, treatment,
and control in the Multi-Ethnic Study
of Atherosclerosis (MESA): gender,
ethnicity, and coronary artery calcium.
Circulation2006; 113:647-56.
13. Cholesterol Treatment Trialists (CTT )
Collaboration. Efficacy and safety of more
intensive lowering of LDL cholesterol:
a meta-analysis of data from 170000
participants in 26 randomised trials.Lancet
2010; 376:1670-81.
14. Brugts JJ, Yetgin T, Hoeks SE, Gotto AM,
Shepherd J, Westendorp RGJ, et al. The
benefits of statins in people without
established cardiovascular disease but with
cardiovascular risk factors: meta-analysis
of randomised controlled trials. BMJ 2009;
338:b2376.
15. Raal F, Schamroth C, Blom D, Marx J, Rajput
M, Haus M ,et al. CEPHEUS SA: a South
African survey on the undertreatment of
hypercholesterolaemia. Cardiovasc J Afr
2011; 22:234-40.
16. Jones PH, Nair R, Thakker KM. Prevalence of
dyslipidemia and lipid goal attainment in
statin-treated subjects from 3 data sources:
a retrospective analysis. J Am Heart Assoc
2012; 1:e001800.
17. Catapano AL. Perspectives on low-densitylipoprotein cholesterol goal achievement.
Curr Med Res Opin 2009; 25:431-47.
You might also like
- Dyslipidemia 2018Document8 pagesDyslipidemia 2018R JannahNo ratings yet
- Diagnosis and Management of Dyslipidemia in Family PracticeDocument41 pagesDiagnosis and Management of Dyslipidemia in Family PracticeKai ChuaNo ratings yet
- 2013 ACC/AHA Guideline On The Treatment of Blood Cholesterol To Reduce Atherosclerotic Cardiovascular Risk in AdultsDocument37 pages2013 ACC/AHA Guideline On The Treatment of Blood Cholesterol To Reduce Atherosclerotic Cardiovascular Risk in AdultsIman SaksoukNo ratings yet
- 27 FullDocument6 pages27 FullKrishna R KhanalNo ratings yet
- Dislipid 2 PDFDocument4 pagesDislipid 2 PDFWahyuningsih HamidNo ratings yet
- Dyslipidemias in Chronic Kidney Disease: Current Guidelines and Future PerspectivesDocument5 pagesDyslipidemias in Chronic Kidney Disease: Current Guidelines and Future PerspectivesAn-Nisa Khoirun UmmiNo ratings yet
- Effect of Adherence To Lipid Profiles of Dyslipidemia Patients A Case Study at A Pharmacy Service in MedanDocument5 pagesEffect of Adherence To Lipid Profiles of Dyslipidemia Patients A Case Study at A Pharmacy Service in MedanInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- CCRR 1 114 PDFDocument3 pagesCCRR 1 114 PDFBruno Mario AngelNo ratings yet
- Diagnosis and Management of Dyslipidemia in Family PracticeDocument19 pagesDiagnosis and Management of Dyslipidemia in Family PracticeMikhaela Katrina AzarconNo ratings yet
- Screening and Management of Lipids: Patient Population: ObjectiveDocument20 pagesScreening and Management of Lipids: Patient Population: ObjectiveKatie Kroll BradyNo ratings yet
- Pharmacological Treatment of HyperlipiedmiaDocument8 pagesPharmacological Treatment of HyperlipiedmiajeffaguilarNo ratings yet
- Correlation of Dyslipidemia and Type 2 Diabetes Mellitus Amongst The People of Vidarbha Region of IndiaDocument6 pagesCorrelation of Dyslipidemia and Type 2 Diabetes Mellitus Amongst The People of Vidarbha Region of IndiaKiki FatmawatyNo ratings yet
- Achievement of Target LDL-C in Type 2 DM Patients in Saudi ArabiaDocument4 pagesAchievement of Target LDL-C in Type 2 DM Patients in Saudi ArabiaIJAR JOURNALNo ratings yet
- Li 2017Document32 pagesLi 2017akshayNo ratings yet
- Dyslipidemia in Diabetes Mellitus and Cardiovascular DiseaseDocument6 pagesDyslipidemia in Diabetes Mellitus and Cardiovascular DiseaseEward Rod SalNo ratings yet
- Lipoprotein Abnormalities in Patients With Diabetes 2013Document6 pagesLipoprotein Abnormalities in Patients With Diabetes 2013Luis Javier CastroNo ratings yet
- Endocrinology and Metabolism Clinics-Lípidos 2009Document234 pagesEndocrinology and Metabolism Clinics-Lípidos 2009Tony Miguel Saba SabaNo ratings yet
- Ezetimibe - A Novel Add On Treatment Strategy To Achieve Targeted LDL in Patients With Uncontrolled LDL Levels On High Dose Statin AloneDocument9 pagesEzetimibe - A Novel Add On Treatment Strategy To Achieve Targeted LDL in Patients With Uncontrolled LDL Levels On High Dose Statin AloneEditor ERWEJNo ratings yet
- LipidsupdateDocument23 pagesLipidsupdatedrshekarforyouNo ratings yet
- Lipids JBDocument48 pagesLipids JBMuvenn KannanNo ratings yet
- Dipiro DislipidemiaDocument49 pagesDipiro DislipidemiaMila ErnilaNo ratings yet
- CPG-Dyslipidemia 2005Document22 pagesCPG-Dyslipidemia 2005lovelots1234No ratings yet
- Kelompok 1Document14 pagesKelompok 1Aurent WidjanarkoNo ratings yet
- DyslipidemiaManagement Continuum 2011Document13 pagesDyslipidemiaManagement Continuum 2011Zuleika DöObsönNo ratings yet
- Guideline StatinDocument7 pagesGuideline StatinNurul Kamilah SadliNo ratings yet
- Management Dislipidemia PDFDocument5 pagesManagement Dislipidemia PDFkemalmiaNo ratings yet
- LDL Apheresis: An Effective and Safe Treatment For Refractory HypercholesterolemiaDocument10 pagesLDL Apheresis: An Effective and Safe Treatment For Refractory HypercholesterolemiagekayuuNo ratings yet
- KDIGO Lipid Management in CKDDocument13 pagesKDIGO Lipid Management in CKDIrma AwaliaNo ratings yet
- No-Hdl Como Indicador de CalidadDocument3 pagesNo-Hdl Como Indicador de CalidadSergio GonzalezNo ratings yet
- (CLINPHAR) 2015 Clinical Practice Guidelines For The Management of Dyslipidemia in The Philippines - ExtractedDocument44 pages(CLINPHAR) 2015 Clinical Practice Guidelines For The Management of Dyslipidemia in The Philippines - ExtractedDenise Yanci DemiarNo ratings yet
- Out 21 PDFDocument10 pagesOut 21 PDFBlank SpaceNo ratings yet
- Asap LipidDocument131 pagesAsap LipidagassiNo ratings yet
- Applicability of Recent Dyslipidemia Guidelines in Clinical PracticeDocument4 pagesApplicability of Recent Dyslipidemia Guidelines in Clinical PracticeDokter FebyanNo ratings yet
- Elevated LDL Cholesterol Levels Among Lean Mass HyDocument4 pagesElevated LDL Cholesterol Levels Among Lean Mass Hy8v6y5jsykbNo ratings yet
- Design and Rationale For The Patient and Provider Assessment of Lipid ManagementDocument25 pagesDesign and Rationale For The Patient and Provider Assessment of Lipid ManagementDr. RajibNo ratings yet
- Secondary Causes of DyslipidemiaDocument3 pagesSecondary Causes of DyslipidemiaAnghelo Aldair Velásquez CarrilloNo ratings yet
- DyslipidemiaDocument12 pagesDyslipidemiawalaaahmed213No ratings yet
- Type 2 Diabetes Mellitus Treatment & ManagementDocument3 pagesType 2 Diabetes Mellitus Treatment & ManagementRahman JrNo ratings yet
- Lipid Profile Pattern in Anginal Syndrome Patients From Marathwada Region of Maharashtra StateDocument5 pagesLipid Profile Pattern in Anginal Syndrome Patients From Marathwada Region of Maharashtra StateDr. Arvind YadavNo ratings yet
- Original Article: Journal of Clinical Lipidology (2017)Document12 pagesOriginal Article: Journal of Clinical Lipidology (2017)IrhamNo ratings yet
- Objective:: BackgroundDocument23 pagesObjective:: BackgroundJanine DimaangayNo ratings yet
- Srikant H 2016Document10 pagesSrikant H 2016aditya sekarNo ratings yet
- Recommendations For The Intensity of Statin Therapy Based On Statin Benefit Group Diagram. (AdaptedDocument8 pagesRecommendations For The Intensity of Statin Therapy Based On Statin Benefit Group Diagram. (Adaptedعزالدين الطيارNo ratings yet
- Approach To DyslipedimiaDocument26 pagesApproach To Dyslipedimiaazharuddin imamuddinNo ratings yet
- Kohli Giugliano 2013 Low Density Lipoprotein Lowering in 2013 by Nonstatin Agents The Discovery and Development ofDocument12 pagesKohli Giugliano 2013 Low Density Lipoprotein Lowering in 2013 by Nonstatin Agents The Discovery and Development ofOana MihaelaNo ratings yet
- Efficacy of Low-Dose Rosuvastatin in Patients With Type 2 Diabetes and Hypo High-Density Lipoprotein CholesterolaemiaDocument11 pagesEfficacy of Low-Dose Rosuvastatin in Patients With Type 2 Diabetes and Hypo High-Density Lipoprotein CholesterolaemiaZahid MahmoodNo ratings yet
- Lipid Management For The Prevention of Atherosclerotic Cardiovascular DiseaseDocument6 pagesLipid Management For The Prevention of Atherosclerotic Cardiovascular DiseaseemirkurtalicNo ratings yet
- Atherogenic Dyslipidemia in Patients With Established Coronary Artery DiseaseDocument6 pagesAtherogenic Dyslipidemia in Patients With Established Coronary Artery DiseasebilahalvirayuNo ratings yet
- Primary and Secondary Prevention of Cardiovascular DiseasesDocument38 pagesPrimary and Secondary Prevention of Cardiovascular DiseasesJuwanto WakiminNo ratings yet
- AnnotationsDocument3 pagesAnnotationsAegina FestinNo ratings yet
- Artículo Dislipemia ESCDocument12 pagesArtículo Dislipemia ESCSMIBA MedicinaNo ratings yet
- Polypharmacy in The Aging Patient A Review of Glycemic Control in Older Adults With Type 2 DiabetesDocument12 pagesPolypharmacy in The Aging Patient A Review of Glycemic Control in Older Adults With Type 2 Diabetesapi-311409998No ratings yet
- Levels of LDL Cholesterol, Triglyceride and Urate in Patients With Type 2 Diabetes MellitusDocument8 pagesLevels of LDL Cholesterol, Triglyceride and Urate in Patients With Type 2 Diabetes Mellitusstalker2222No ratings yet
- Dyslipidemia: Dr. Sohail AhmadDocument36 pagesDyslipidemia: Dr. Sohail AhmadChong Zhi LinNo ratings yet
- LDL Particle Number As Assessed by NMR SpectrosDocument17 pagesLDL Particle Number As Assessed by NMR SpectrosCTAFDocuments100% (1)
- Relationship Between Dyslipidemia and Glycemic StaDocument5 pagesRelationship Between Dyslipidemia and Glycemic Staoliffasalma atthahirohNo ratings yet
- Lectura - Manejo DM2Document25 pagesLectura - Manejo DM2Patricia Jesùs PérezNo ratings yet
- NursingresearchreportDocument12 pagesNursingresearchreportapi-300699057No ratings yet
- DiabetesDocument19 pagesDiabetesYasmin ElsobkyNo ratings yet
- Communication Interaction in ICU-Patient and Staff Experiences and Perceptions.Document5 pagesCommunication Interaction in ICU-Patient and Staff Experiences and Perceptions.osondoarNo ratings yet
- Annotated BibDocument3 pagesAnnotated Bibapi-489789428No ratings yet
- Rees Et Al-2019-Neurourology and UrodynamicsDocument9 pagesRees Et Al-2019-Neurourology and UrodynamicsMIHAELANo ratings yet
- Factors Affecting Drug Abosrtion and DistributionDocument5 pagesFactors Affecting Drug Abosrtion and DistributionBruno Adriel ZamoraNo ratings yet
- Pharmacology Table For Cardiovascular LectureDocument10 pagesPharmacology Table For Cardiovascular LecturemuhammadridhwanNo ratings yet
- Dentine HypersensitivityDocument32 pagesDentine Hypersensitivityitdoc100% (1)
- Dialysis Nurse Responsibilities and DutiesDocument22 pagesDialysis Nurse Responsibilities and DutiesWyn Agustin0% (1)
- Implementation of The Early Start Denver Model in An Italian CommunityDocument8 pagesImplementation of The Early Start Denver Model in An Italian CommunityLuis SeixasNo ratings yet
- Surgical SkillsDocument47 pagesSurgical SkillsSamah SuhailNo ratings yet
- Corporate Massage ContractDocument2 pagesCorporate Massage ContractCiorîcă Denisa TerapeutNo ratings yet
- Abscess Incision and Drainage NEJMDocument4 pagesAbscess Incision and Drainage NEJMMarcela CharryNo ratings yet
- Drug Study For HELLP SyndromeDocument19 pagesDrug Study For HELLP SyndromeRosemarie CarpioNo ratings yet
- EXSA - Gold Award Recipients 2009Document1 pageEXSA - Gold Award Recipients 2009applebarrelNo ratings yet
- Medication Related Osteonecrosis of The JawDocument26 pagesMedication Related Osteonecrosis of The Jawapi-265532519100% (1)
- Odtp Boards Exam OverviewDocument5 pagesOdtp Boards Exam OverviewAndrew McDonald100% (1)
- Benefits of Zinc:: 1 - Zinc and Regulating Immune FunctionDocument3 pagesBenefits of Zinc:: 1 - Zinc and Regulating Immune FunctionHuda BaharoonNo ratings yet
- Hyponatremia Inpatient Management of JCG0342 V3Document12 pagesHyponatremia Inpatient Management of JCG0342 V3zikryauliaNo ratings yet
- Steven K. Huprich - Psychodynamic Therapy - Conceptual and Empirical Foundations (2008) PDFDocument288 pagesSteven K. Huprich - Psychodynamic Therapy - Conceptual and Empirical Foundations (2008) PDFChalwe HowardNo ratings yet
- nsg-300 Care Plan 2Document21 pagesnsg-300 Care Plan 2api-521003884100% (1)
- Homoeopathic Treatment of Parkinson DieseDocument23 pagesHomoeopathic Treatment of Parkinson DieseNidhi SrivastavaNo ratings yet
- Silverstein and Bellack A Scientific Agenda For The Concept of Recovery CPR 2008 Published VersionDocument18 pagesSilverstein and Bellack A Scientific Agenda For The Concept of Recovery CPR 2008 Published VersionAmada NeferNo ratings yet
- Mmvr19 / Nextmed Conference ScheduleDocument21 pagesMmvr19 / Nextmed Conference SchedulepvaldastriNo ratings yet
- The Learning Curve For Laparoscopic Cholecystectomy PDFDocument5 pagesThe Learning Curve For Laparoscopic Cholecystectomy PDFIgor CemortanNo ratings yet
- Yakeley 2018 Psychoanalysis in Modern Mental Health PracticeDocument8 pagesYakeley 2018 Psychoanalysis in Modern Mental Health PracticeJonathan RiveraNo ratings yet
- My Sister's KeeperDocument27 pagesMy Sister's KeepersindhujaNo ratings yet
- Coagulation Profile in Diabetes MellitusDocument5 pagesCoagulation Profile in Diabetes MellitusAsfandyar RoghaniNo ratings yet
- Pembrolizumab MonographDocument8 pagesPembrolizumab MonographpmuftiaNo ratings yet
- Intra Uterine Insemination - IUIDocument15 pagesIntra Uterine Insemination - IUIlayyous100% (1)
- TerminologyDocument11 pagesTerminologyMustafa SaßerNo ratings yet
- Emphasis On Non-Pharmacologic Aspect: Key Principles: o Gate Control & Neuromatrix Theory of PainDocument3 pagesEmphasis On Non-Pharmacologic Aspect: Key Principles: o Gate Control & Neuromatrix Theory of PainJudy Ignacio EclarinoNo ratings yet