Professional Documents
Culture Documents
Cervical Spine Stomatognatic System and Craniofacial
Uploaded by
Denise MathreOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cervical Spine Stomatognatic System and Craniofacial
Uploaded by
Denise MathreCopyright:
Available Formats
16/04/2015
The cervical spine,
Stomatognathic System
and Craniofacial Pain:
What is the Connection?
Susan Armijo-Olivo, BScPT, MScPT, PhD
Faculty of Rehabilitation Medicine
University of Alberta
Canada
susanarmijo@gmail.com
Why is this
Connection
Important?
16/04/2015
Introduction
DENTISTS
PHYSICAL THERAPISTS
PSYCHOLOGISTS
SPEECH PATHOLOGISTS
PHYSICIANS....
Craniomandibular
System
Types of Connections
Anatomical
Biomechanical
Neurological
Pathological
Pathophysiological
Clinical
16/04/2015
Anatomic and Biomechanical
Connection
Body Systems and
Craniomandibular system
16/04/2015
Craniomandibular System
Head,
Neck, and
.
shoulder Girdle,
work anatomically,
physiologically, and
biomechanically
together.
Gillies G et al.,. A biomechanical model of the craniomandibular complex and cervical spine based on the inverted pendulum. Journal of Medical Engineering & Technology. 1998;22(6):263-269.
Gillies GT, et al.,. Equilibrium and non-equilibrium dynamics of the cranio-mandibular complex and cervical spine. Journal Of Medical Engineering & Technology. 2003;27(1):32-40
Rocabado M. Biomechanical relationship of the cranial, cervical, and hyoid regions. The Journal Of Cranio-Mandibular Practice. 1983;1(3):61-66.
Craniocervical Equilibrium
Inverted Pendulum
Craniocervical equilibrium
- Importance of Cervical
Muscles
Gillies G et al.,. A biomechanical model of the craniomandibular
complex and cervical spine based on the inverted pendulum. Journal of
Medical Engineering & Technology. 1998;22(6):263-269.
16/04/2015
Craniocervical Equilibrium
Importance of cervical Muscles
Global muscle system
Upper trapezius
Splenius capitis
Splenius cervicis
Semispinalis capitis, and
Sternocleidomastoid
Local muscle system.
Cervical multifidus,
Longissimus capitis,
Longissimus cervicis,
Intertransversus,
Longus colli,
Rectus capitis,
and the suboccipitalis muscles at upper cervical level
Superficial Multifidus
Craniocervicomandibular Relations
Deep Multifidus
10
Craniocervical posture is
related to the position of
the mandible and facial
structures
Makofsky HW. The influence of forward head posture on dental occlusion. Cranio: The Journal Of Craniomandibular Practice. 2000/1 2000;18(1):30-39.
Makofsky HW, Sexton TR, Diamond DZ, Sexton MT. The Effect of Head Posture on Muscle Contact Position Using the T-Scan System of Occlusal Analysis.
Cranio-the Journal of Craniomandibular Practice. Oct 1991;9(4):316-321.
16/04/2015
Sliding Cranium Theory
11
Changes in head posture
produce a change in the
position of the jaw and
consequently a modification
of teeth contact and
muscular activity
Makofsky H. The effect of head posture on muscle contact position: the sliding cranium theory. Cranio: The Journal Of
Craniomandibular Practice. 1989/10 1989;7(4):286-292.
Cervical Flexion
12
Anterior mandibular
displacement
First contact in the anterior
zone ( Schwarz, 1928; Preskel, 1965)
Increase of the
electromyographic activity of
digastric muscles (Fumakoshi, 1976)
16/04/2015
Cervical Extension
13
Posterior mandibular displacement
The first contact is in the posterior zone (Schwarz, 1928; Posselt
1952; Preiskel, 1965)
Increases in the activity of the temporal and masseter
muscles (Funakoshi and Fujita, 1976)
Increases the tension of the suprahyoid muscles,
masticatory muscles and cervical muscles (Yamabe, Yamashita
and Fuji, 1999)
Mandibular retrusion (stretching ) (sollow and Tallgren , 1976;
Golsdtein 1984; Gonzalez and Manns 1996; Kohno et al. 2001)
14
During Mouth Opening head moves
toward extension and during mouth
closing moves toward flexion
Kohno S, Kohno T, Medina RU. Rotational head motion concurrent to rhythmical mandibular opening
movements. Journal Of Oral Rehabilitation. 2001/8 2001;28(8):740-747.
16/04/2015
Craniocervicomandibular Relations
Forward head posture required more
masseter muscle activity when compared
with a corrected posture (21.7% MVC) (in
sitting position).
Slouched posture increased the activity of
masseter muscle in 21.9% MVC in standing
position compared with the other studied
postures (corrected posture, habitual posture
15
and forward head posture).
The increase in masseter Normalized EMG in
forward head posture and slouched
posture was clinically significant
McLean L. The effect of postural correction on muscle activation amplitudes recorded from the cervicobrachial region. Journal of Electromyography and Kinesiology.
2005;15(6):527-535.
16
16/04/2015
17
Neurological Connection
Cervical spine
18
(C1, C2, C3)
Trigeminocervical
Nucleus
Craniofacial
Pain
16/04/2015
Trigeminal nerve
19
Convergence
Trigeminocervical Nucleus
20
Bogduk N. Cervicogenic headache: anatomic basis and pathophysiologic
mechanisms. Current Pain And Headache Reports. 2001/8 2001;5(4):382-386.
10
16/04/2015
Trigeminocervical Nucleus
21
Pain from any structure innervated by
C1, C2, and C3 can be perceived in
regions innervated by trigeminal nerve
Bogduk N. cervical causes of headache. In: Grieves BJ, Palastanga N, ed. Grievess Modern Manual Therapy: The vertebral
Column. Edingburg, London, Madrid, Melbourne, New York, and Tokyo: Churchill Livingstone; 1994:317-332.
Structures Innervated by C1, C2, and C3
22
11
16/04/2015
Trigeminocervical Nucleus
23
Some recent evidence has proposed that subnucleus caudalis (SC) and C1 and C2 dorsal horns
may act together as one functional unit to process nociceptive information from craniofacial and
cervical tissues
Pain coming from orofacial region or cervical spine could be interpreted as coming from either
region (i.e. orofacial or cervical spine) since sensory information coming from both areas is
integrated at the trigeminocervical nucleus,
Thus responses to this pain could be directed to either place (i.e. orofacial or cervical spine).
Morch CD, Hu JW, Arendt-Nielsen L, Sessle BJ. Convergence of cutaneous, musculoskeletal, dural and visceral afferents onto nociceptive neurons in the first cervical dorsal horn.
European Journal of Neuroscience. 2007;26: 142-54.
Hu JW, Sun KQ, Vernon H, Sessle BJ. Craniofacial inputs to upper cervical dorsal horn: Implications for somatosensory information processing. Brain Research. 2005;1044: 93.
24
Experimental
Evidence :
Neurological
Connection
12
16/04/2015
Animal Experiments
25
First 3 levels of the cervical spine and Trigeminal Nerve merge into a
single column of gray matter (Kerr , 1961; 1972)
Craniofacial inputs ( tooth pulp, mucosa, tongue muscles, larynx, TMJ
and neck) converge in Nucleus caudalis of the trigeminal nerve in cats
(Sessle et al. 1986).
Stimulation of afferents from jaw , tongue muscles and neck muscles
excited WDR and nociceptive neurons in Pars caudalis nucleus (Sessle et al.
1986)
Animal Experiments
26
The irritation of TMJ caused an increase in the activity of masticatory
and cervical Muscles in rats. ( Yu et al. 1995)
Irritation ( bradykinin) of the TMJ caused changes in the sensitivity of
muscles spindles in cervical spine. ( Hellstrom et al, 2002)
13
16/04/2015
Animal Experiments
27
Stimulation of cervical
paraspinal tissues ( mustard
oil) caused increase in the
Masticatory muscles as well
cervical muscles EMG (Hu et al,
1993)
28
14
16/04/2015
29
Cervical Joints , their
Nerves and Craniofacial
Pain
30
Cervical Joints
(C2-C3 and C3-C4)
Atlantoaxial Joints
15
16/04/2015
31
32
Experimental Evidence
16
16/04/2015
Zygapophysial joints Pattern
33
Cervical Joints
(zygapophysial joints)
pain patterns obtained in
healthy volunteers (Dwyer et.
al. 1990)
Pain more spread in
patients than
healthy subjects
34
17
16/04/2015
35
Patterns of pain evoked in a volunteer by stimulating the Zygaphophyseal joints at
segments C2-C3 to C6-C7 ( Dwyer et al., 1990)
36
Pain similar to
reported by patients.
Cervical blocks
(nerves and joints)
caused relief of
symptoms
Aprill C, Dwyer A, Bogduk N. Cervical zygapophyseal
joint pain patterns. II: A clinical evaluation. Spine. 1990/6
1990;15(6):458-461.
18
16/04/2015
37
Patterns from Joints C2-C3, extended
further into the head, toward the ear,
vertex, forehead, or eye.
Bogduk N, Marsland A. The cervical zygapophysial joints as a source of neck pain. Spine. 1988/6 1988;13(6):610-617.
Atlantoaxial joints pain patterns
38
Atlantoaxial joint
blocks caused relief
of pain in patients
with occipital
headache
Aprill C, Axinn MJ, Bogduk N. Occipital headaches stemming from the lateral atlantoaxial (C1-2) joint. Cephalalgia: An International Journal Of Headache. 2002/2
2002;22(1):15-22.
19
16/04/2015
39
Symptoms reproduced by injection of contrast medium into cervical
joints ( C0-C1; C7-T1) or by electrical stimulation of the dorsal rami (C3C7) with a larger number of patients
Fukui S, Ohseto K, Shiotani M, et al. Cervical zygapophyseal joint pain patterns - Pain distribution determined by electrical stimulation of the
cervical dorsal rami*. Pain Clinic. 1996;9(3):285-293.
40
Cervical Medial
branches blocks
and cervical joints
relief referred
symptoms
Bogduk N, Marsland A. On the concept of third occipital headache. Journal
Of Neurology, Neurosurgery, And Psychiatry. 1986/7 1986;49(7):775-780.
20
16/04/2015
41
Cervical Muscles, Myofascial
Pain, Muscular pain models
and Craniofacial Pain
42
21
16/04/2015
Myofascial Syndrome: Trigger Points
43
Myofascial Pain Syndrome ( MFPS):
Pain that is derived from myofascial
trigger points, which are highly
localized and hyperirritable spots in
a palpable taut band of skeletal
muscle fibers
Pain, stiffness, weakness
Restricted Movements
Cervical Myofascial Pain : Evidence
44
Referred pain to the cranial zone ( Fricton 1985, Davidoff 1998,Travell and Simmons 1999,
Wright, 2000)
Muscles innervated by C1, C2 and C3 commonly refer pain to the facial
region (Fricton, 1985, Travell and Simmons; Wright, 2000).
Active TPs in the cervical and shoulder muscles of patients with headache
and orofacial pain are usually found (Wright, 2000)
22
16/04/2015
SCM Myofascial Pain Syndrome
45
The SCM causes pain in the
fronto-temporal region,
occiput, vertex, forehead,
and the orbit
Upper Trapezius and Splenius Myofascial Pain Syndrome
46
Trapezius muscle refers pain to
the head, neck, orbital, and
preorbital regions.
Splenius capitis and splenius
cervicis refer pain to the vertex
of the head, behind the head,
behind the eye and the
occiput
Simons D. Travell & Simons Myofascial Pain and Dysfunction :The Trigger point Manual. 2nd ed. Baltimore: Williams and
Wilkins; 1999.
23
16/04/2015
Cervical Myofascial Pain and Craniofacial Pain
47
Patients with MFPS of the upper trapezius
decreased their pain and EMG activity in masseter muscle after injecting upper Trapezius
TP (Carlson et al, 1993)
Splenius capitis and the splenius cervicis TP treatment caused relief in patients
occipital neuralgia (Grad-Radford et al, 1986)
Stimulation of the TPs during an headache attack exacerbates or intensifies the
headache.
TP Inactivation relief the symptomatology (Davidoff, 1998; Wright 2000).
Cervical occipital Myofascial Pain and Craniofacial
Pain
48
TPs from suboccipital
muscles cause referred
pain in patients with
occipital neuralgia
(Davidoff, 1998)
Davidoff RA. Trigger points and myofascial pain: toward understanding how they affect headaches.
Cephalalgia. 1998;18(7):436-448.
24
16/04/2015
Cervical Myofascial Pain and Craniofacial
Pain
49
Lower cervical intramuscular
anesthetic injections have
demonstrated good results in relief of
symptoms in patients with intractable
head or face pain (Mellick and Mellick, 2003)
Map of referred pain generated by palpation
50
The most common referred pain
source in the craniofacial region
was from palpating the trapezius
muscle ( Wright , 2000)
Wright EF. Referred craniofacial pain patterns in patients with temporomandibular disorder.[see comment][erratum appears in J
Am Dent Assoc 2000 Nov;131(11):1553]. Journal of the American Dental Association. 2000;131(9):1307-1315.
25
16/04/2015
51
Muscle Pain Experimental
Models
Experimental Pain Models: Muscular Pain
52
Glutamate injections on the splenius capitis
muscle referred pain to:
The ipsilateral neck and occipital region,
And in some subjects, toward the ipsilateral upper
head and temporal region (46.15%). (Svensson et al.
2005)
In one subject, the reference pattern reached
the teeth and masseter region (Svensson et al
2004)
Svensson P, Wang K, Arendt-Nielsen L, Cairns BE, Sessle BJ. Pain effects of glutamate injections
into human jaw or neck muscles. Journal Of Orofacial Pain. 2005;19(2):109-118.
26
16/04/2015
Experimental Pain Models: Muscular
Pain
Hypertonic saline in Upper Trapezius caused
pain at the base of the neck in 83% of the
subjects, infra-auricular zone in 50% and 42% to
the retro-auricular zone ( Komiyama et al, 2005).
53
Greater spread of pain to the temporomandibular joint
region
Experimental pain in upper trapezius caused a
significant decrease in the mean maximum
mouth opening (54 to 47.8 mm) ( Komiyama et al,
2005)
Komiyama, O., et al. (2005). "Pain patterns and mandibular dysfunction
following experimental trapezius muscle pain." Journal of Orofacial Pain
19(2): 119-126.
Experimental Pain Models: Muscular Pain
54
Upper trapezius referred pain after experimental pain model ( Madeleine et al.
1998 and Ge et al. 2003)
27
16/04/2015
Experimental Pain Models: Muscular Pain
55
When glutamate was injected into masseter, the EMG activity of the
masseter as well as the activity of the SCM and Splenius was
increased ( Svensson et al. 2004)
Muscle Pain Sensitivity in TMD
56
Significantly increased masticatory and cervical
muscle tenderness and pain sensitivity in the hand
in subjects with TMD when compared with healthy
subjects.
Moderate to high effect sizes showed the clinical
relevance of the findings
Silveira A, Armijo-Olivo S, Gadotti IC, Magee D. Masticatory and cervical muscle tenderness and pain sensitivity in a
remote area in subjects with a temporomandibular disorder and neck disability. J Oral Facial Pain Headache.
2014;28(2):138-146.
28
16/04/2015
57
Cervical Discs and
Craniofacial Pain
Cervical Discs and Craniofacial Pain
58
Disc is innervated
and as a result can
cause Pain
Bogduk N. Innervation and Pain patterns of the Cervical Spine. In: Grant R, ed. Physical
therapy of the Cervical and Thoracic Spine. St Louis: Churchill Livingstone; 1988:61-72.
29
16/04/2015
Cervical Discs and Craniofacial Pain
59
Cervical Disc
Sites
C3-C4
Mastoid, temple, temporal, parietal,
occiput, jaw, temporomandibular joint,
craniovertebral junction, neck, throat,
back ,trapezius muscle, top of the
shoulder, and upper extremity
C4-C5
Mastoid, temporomandibular joint,
parietal, occiput, craniovertebral junction,
neck, throat, back ,trapezius muscle, top
of the shoulder, upper extremity, anterior
chest , and upper back.
C5-C6
occiput, craniovertebral junction, neck,
throat, back ,trapezius muscle, top of the
shoulder, upper extremity, anterior chest ,
and upper back.
C6-C7
Neck, upper back, scapula, shoulders,
trapezius muscles, upper extremity, and
anterior chest
Grubb SA, Kelly CK. Cervical discography: clinical implications from 12 years of experience. Spine. 2000/6/1 2000;25(11):1382-1389.
Schellhas KP, Garvey TA, Johnson BA, Rothbart PJ, Pollei SR. Cervical diskography: analysis of provoked responses at C2-C3, C3-C4, and C4-C5. AJNR.
American Journal Of Neuroradiology. 2000/2 2000;21(2):269-275.
60
30
16/04/2015
61
Cervical Spine
Dysfunction and TMD
Cervical spine Dysfunction:
Collective term
Clinical problem
Musculoskeletal structures (cervical spine)
Pain is usually aggravated by moving the head or adopting certain
62
head positions.
Neck pain main symptom
Dysfunction related to acute (macrotrauma) or chronic ( microtrauma)
affecting the joints or periarticular tissues surrounding the cervical spine
31
16/04/2015
Cervical Spine Dysfunction and TMD
63
Symptoms of the stomatognathic system overlap in patients with TMD
and CSD, and symptoms of the cervical spine overlap in these
patients (De Wijer et al. 1996 a, b)
Patients with TMD more often suffer from cervical spine pain than
subjects without TMD (Visscher et al, 2001,Stiesch-Scholz et al 2003 Fink et al,
2003)
Cervical Spine Dysfunction and TMD
Patients with internal derangement showed more cervical symptoms
such as tenderness in cervical muscles and shoulder muscles
alteration of the mobility of the upper cervical segments
64
than healthy controls (Fink et al, 2002)
Facial pain has an association with reported pain in the neck and tenderness in the
neck- occiput area (Sipila et al. 2002)
32
16/04/2015
65
Cervical Spine Dysfunction and TMD
Positive relationship between neck pain and temporomandibular
disorders (Ciancaglini et al.1999)
Patients suffering TMD had more than double the odds (odds ratio of
2.33) of suffering neck pain than patients without TMD. (Ciancaglini et al.1999)
Individual symptoms such as facial and jaw pain were significantly
associated with neck pain with odds ratio of 2.09 (Ciancaglini et al.1999).
Cervical Spine Dysfunction and TMD
66
Patients with myogenous TMD had increased resting EMG activity of
the upper trapezius muscles as well as the SCM muscles when
compared with control subjects (Pallegama et al. 2004)
The presence of pain over the SCM and trapezius muscles was
significantly associated with masticatory muscle pain without disc
displacement.
Pallegama RW, Ranasinghe AW, Weerasinghe VS, Sitheeque MA. Influence of masticatory muscle pain on
electromyographic activities of cervical muscles in patients with myogenous temporomandibular disorders. Journal of Oral
Rehabilitation. May 2004;31(5):423-429.
33
16/04/2015
Relationship between Cervical Spine and
TMD
67
Neck pain was the most strongly associated with TMD
Plesh O, et al. Temporomandibular joint and muscle disorder-type pain and comorbid pains in a national US sample. Journal of Orofacial Pain.
2011;25(3):190-198.
Relationship between Spinal pain and TMD
68
The prevalence of frequent spinal pain increasing
with increasing frequency/severity of TMD symptoms.
The operational definition of 'spinal
pain' was pain in the neck, shoulders
and/or low back.
Wiesinger B, Malker H, Englund E, Wnman A. Does a dose-response relation
exist between spinal pain and temporomandibular disorders? BMC
Musculoskeletal Disorders. 2009;10.
34
16/04/2015
Relationship between Spinal pain and TMD
69
Wiesinger B, Malker H, Englund E, Wnman A. Does a dose-response relation exist between spinal pain and temporomandibular disorders? BMC
Musculoskeletal Disorders. 2009;10.
70
Discussion
35
16/04/2015
71
There is evidence in the literature
that supports the connection
among cervical spine,
stomatognathic system and
craniofacial pain
Moya et al., 1994; Rocabado, 1983; B Solow & Tallgren, 1976; B. Solow & Sandham,
2002a; Zuniga et al., 1995; Kohno, Kohno, & Medina, 2001; Kohno, Matsuyama,
Medina, & Arai, 2001; Torisu, Yamabe, Hashimoto, Yoshimatsu, & Fujii, 2001; C. M.
Visscher, Slater, Lobbezoo, & Naeije, 2000; Yamabe, Yamashita, & Fujii, 1999;
Yamada, Ogawa, & Koyano, 1999; makosfsky, 1989.)
72
Anatomic, neurological
biomechanical,
physiological and pathological
connections between
craniocervical region
and craniofacial pain exist
(Escolar, 1948; Hellstrom et al., 2002; F. W. L. Kerr, 1972; Sessle et al., 1986; X.M. Yu et al., 1995). (Anonymous, 2004; Aprill et al., 1990; Bartsch T, 2003;
Benoliel & Sharav, 1998; N. Bogduk, 1982; Bogduk & Marsland, 1986; BorgStein, 2002; R. A. Davidoff, 1998; Dreyfuss et al., 1994; Dwyer et al., 1990;
Edmeads, 1990; Steven B Graff-Radford & Newman, 2002; Grubb & Kelly, 2000;
Hack et al., 1995; J. W. Hu, Sessle, Amano, & Zhong, 1984; Kuhn et al., 1997;
Mackley, 1990; Mellick & Mellick, 1109; Piovesan et al., 2001; Schellhas et al.,
2000)
36
16/04/2015
73
However.....
Levels of Evidence
74
Sackett D et al. Evidence-Based Medicine. How to Practice and Teach. Edinburg, London, New York, Philadelphia, St Louis, Sydney,
Toronto: Churchill Livingstone, 2000.
37
16/04/2015
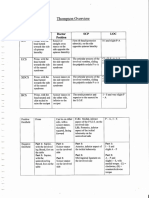
Levels of Evidence
75
Level
Characteristics
Expert opinion
40
Case series and poor quality of cohort and case
control studies
45
3b
Case control-studies ( cross sectional studies)
13
3a
Systematic Reviews of case control studies
2b
Individual cohort studies and low quality of RCTs
2a
Systematic Reviews of cohort studies
1b
Individual RCTs with narrow confidence interval
1a
Systematic Reviews of RCTs
total
Number of
references
101
76
This is the information that
we have, So
38
16/04/2015
77
The Advice:
Do not consider this information useless.
The evidence pointed out a tendency to link cervical spine, neck
structures and craniofacial pain. This tendency should not be
undervalued.
Analyze carefully the studies results.
It is necessary more well designed studies to strongly conclude
We have to evaluate and treat patients based on this knowledge
78
Questions
?
39
16/04/2015
79
40
You might also like
- Physio Shacklock 95Document8 pagesPhysio Shacklock 95Raihan HabibNo ratings yet
- Ijspt-Biomechanics and Pathomechanics of The Patellofemoral JointDocument11 pagesIjspt-Biomechanics and Pathomechanics of The Patellofemoral JointDevi MigiekaNo ratings yet
- Tendon Problems in Athletic IndividualsDocument15 pagesTendon Problems in Athletic IndividualsMuhammadskNo ratings yet
- Bogduk 2009Document3 pagesBogduk 2009Borys100% (1)
- Neck PainDocument1 pageNeck PainHasan RahmanNo ratings yet
- Nupur Agarwal (BPT Iii Year)Document29 pagesNupur Agarwal (BPT Iii Year)nupur agarwalNo ratings yet
- Ann Cools 4Document51 pagesAnn Cools 4Walter Pelaez100% (1)
- Adolescent Idiopathic Scoliosis - From Normal Spinal Anatomy To Three-Dimensional Deformity (PDFDrive)Document252 pagesAdolescent Idiopathic Scoliosis - From Normal Spinal Anatomy To Three-Dimensional Deformity (PDFDrive)AuraNo ratings yet
- Clinical Neurodynamics and Sports Medicine: Origins and DevelopmentDocument8 pagesClinical Neurodynamics and Sports Medicine: Origins and DevelopmentWahid NasrudinNo ratings yet
- Patterns of Triangular Fibrocartilage Complex (TFCC) Injury Associated WithDocument7 pagesPatterns of Triangular Fibrocartilage Complex (TFCC) Injury Associated WithCésarLópezNo ratings yet
- Week 2 Ortho Tests Figure NoDocument14 pagesWeek 2 Ortho Tests Figure Noapi-468597987No ratings yet
- Shoulder Anatomy & Biomechanics (Halder) PDFDocument18 pagesShoulder Anatomy & Biomechanics (Halder) PDFNedelcuGeorgeNo ratings yet
- 2 Biomechanics of The ShoulderDocument47 pages2 Biomechanics of The ShoulderDaniel PereiraNo ratings yet
- Manipulation of The Spine, Thorax and Pelvis: With Access To WWW - Spinethoraxpelvis.com - Peter GibbonsDocument5 pagesManipulation of The Spine, Thorax and Pelvis: With Access To WWW - Spinethoraxpelvis.com - Peter GibbonspyhedizyNo ratings yet
- Pediatrics FracturesDocument14 pagesPediatrics Fracturesخالد الغامديNo ratings yet
- A Kinetic Chain Approach For Shoulder RehabDocument9 pagesA Kinetic Chain Approach For Shoulder RehabRicardo QuezadaNo ratings yet
- Cat 2Document5 pagesCat 2Edgardo BivimasNo ratings yet
- De Quervain SyndromeDocument5 pagesDe Quervain Syndromebangla018No ratings yet
- ICF-Ankle Trimalleolar (Cotton's) Fracture RehabDocument18 pagesICF-Ankle Trimalleolar (Cotton's) Fracture RehabdvenumohanNo ratings yet
- Overhead Throwing: Biomechanics and PathologyDocument7 pagesOverhead Throwing: Biomechanics and Pathologyrapannika100% (1)
- TFCCDocument22 pagesTFCChmtno3100% (1)
- Lumbar Spine AssessmentDocument26 pagesLumbar Spine Assessmentyoyo_pt2007100% (1)
- Transverse Rotation of The Segments of The Lower Extremity in LocomotionDocument15 pagesTransverse Rotation of The Segments of The Lower Extremity in Locomotionpetcudaniel100% (1)
- DFDSFSDDocument213 pagesDFDSFSDTamara IlicNo ratings yet
- Distal Biceps Repair Rehabilitation Protocol by Tendayi MutsopotsiDocument5 pagesDistal Biceps Repair Rehabilitation Protocol by Tendayi MutsopotsiPhysiotherapy Care SpecialistsNo ratings yet
- History of Spine BiomechanicsDocument13 pagesHistory of Spine BiomechanicsLeopoldo AguayoNo ratings yet
- Red Flag: MSK Services Pathway - Shoulder PathologyDocument11 pagesRed Flag: MSK Services Pathway - Shoulder PathologyMuhammed ElgasimNo ratings yet
- Application of Fascial Manipulation Technique in Chronic Shoulder Pain Ok PDFDocument8 pagesApplication of Fascial Manipulation Technique in Chronic Shoulder Pain Ok PDFBruno DiasNo ratings yet
- PHT 1261C Tests and Measurements Dr. KaneDocument17 pagesPHT 1261C Tests and Measurements Dr. Kanenico7christian100% (1)
- Interactions between the Craniomandibular System and Cervical Spine: The influence of an unilateral change of occlusion on the upper cervical range of motionFrom EverandInteractions between the Craniomandibular System and Cervical Spine: The influence of an unilateral change of occlusion on the upper cervical range of motionNo ratings yet
- Cools. Scapular Mechanics and RehabilitationDocument9 pagesCools. Scapular Mechanics and RehabilitationWalter PelaezNo ratings yet
- Muscle GuardingDocument3 pagesMuscle GuardingRomeo OpaonNo ratings yet
- PathomechanicsDocument8 pagesPathomechanicsMike B AndersonNo ratings yet
- 香港脊醫 Hong Kong Chiropractors Sep 2016Document6 pages香港脊醫 Hong Kong Chiropractors Sep 2016CDAHKNo ratings yet
- Hanger PDRDocument63 pagesHanger PDRTetay JavierNo ratings yet
- Aaop2003 PDFDocument102 pagesAaop2003 PDFSalemNo ratings yet
- Joint Mobilizations PDFDocument1 pageJoint Mobilizations PDFErik TellezNo ratings yet
- Balance and Vestibular Rehabilitation KitDocument9 pagesBalance and Vestibular Rehabilitation Kitmsnobody8No ratings yet
- 2014 Helsinki Workshop Material ShacklockDocument43 pages2014 Helsinki Workshop Material ShacklockAl100% (1)
- Pediatric SplintingDocument51 pagesPediatric SplintingNathalie Michelle HenriquezNo ratings yet
- IvdpDocument89 pagesIvdpFelix SabuNo ratings yet
- Chiro HIODocument18 pagesChiro HIOPierre SERPAGGINo ratings yet
- ManualDocument95 pagesManualcristina_c_43No ratings yet
- LowBackPain PDFDocument217 pagesLowBackPain PDFBugis MuslimNo ratings yet
- Basic Mulligan, Indikasi Dan Kontrakindikasi: Fitri Yani, M.FisDocument10 pagesBasic Mulligan, Indikasi Dan Kontrakindikasi: Fitri Yani, M.Fisrisa tifaNo ratings yet
- (OS 203) Basic Biomechanics of Musculoskeletal System PDFDocument3 pages(OS 203) Basic Biomechanics of Musculoskeletal System PDFSham David PTNo ratings yet
- Gmi PDFDocument71 pagesGmi PDFAlma GlinacNo ratings yet
- Baseline Bubble Inclinometer User ManualDocument2 pagesBaseline Bubble Inclinometer User Manualphcproducts100% (2)
- Passive Scapular Adduction TestDocument15 pagesPassive Scapular Adduction Testapi-468597987No ratings yet
- 2012 C Liebenson - Hip Mobility TrainingDocument2 pages2012 C Liebenson - Hip Mobility TrainingLuis VargasNo ratings yet
- PDFDocument328 pagesPDFBreak DerulsNo ratings yet
- Effectiveness of Mulligan's Mobilization Technique Versus Eccentric Exercises On Pain, Hand Grip Strength and Function in Subjects With Lateral EpicondylitisDocument8 pagesEffectiveness of Mulligan's Mobilization Technique Versus Eccentric Exercises On Pain, Hand Grip Strength and Function in Subjects With Lateral EpicondylitisInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Sport Injuries: ShoulderDocument67 pagesSport Injuries: ShoulderNabiha AjmalNo ratings yet
- Department of Orthopaedic and Traumatology Faculty of Medicine - Hasanuddin University Makassar 2017Document24 pagesDepartment of Orthopaedic and Traumatology Faculty of Medicine - Hasanuddin University Makassar 2017aritrisnawatiNo ratings yet
- JOSPT Shoulder Pain and Mobility Deficitis Adhesive Capsulitis PDFDocument33 pagesJOSPT Shoulder Pain and Mobility Deficitis Adhesive Capsulitis PDFAbdul Wahid ShaikhNo ratings yet
- Biomechanics of MovementDocument17 pagesBiomechanics of Movements_chandrubioNo ratings yet
- Piriformis Syndrome (Silvanna)Document9 pagesPiriformis Syndrome (Silvanna)Jonathan QuirogaNo ratings yet
- Orthopaedic Management in Cerebral Palsy, 2nd EditionFrom EverandOrthopaedic Management in Cerebral Palsy, 2nd EditionHelen Meeks HorstmannRating: 3 out of 5 stars3/5 (2)
- Physiology and BiochemistryFrom EverandPhysiology and BiochemistryGeoffrey BourneNo ratings yet
- Great Diagrams Osteopathic Medicine in General Practice Pain ManagementDocument12 pagesGreat Diagrams Osteopathic Medicine in General Practice Pain ManagementDenise MathreNo ratings yet
- Entrainement and The Cranial Rythmic ImpulseDocument7 pagesEntrainement and The Cranial Rythmic ImpulseDenise Mathre100% (1)
- Worse Than The Disease? Reviewing Some Possible Unintended Consequences of The mRNA Vaccines Against COVID-19Document42 pagesWorse Than The Disease? Reviewing Some Possible Unintended Consequences of The mRNA Vaccines Against COVID-19Jamie White100% (33)
- Downline Accelerator Playbook Reveals Upside Down EnrollmentDocument22 pagesDownline Accelerator Playbook Reveals Upside Down EnrollmentDenise Mathre100% (1)
- Next Generation Bioweapons: Genetic Engineering and BW: Michael J. AinscoughDocument38 pagesNext Generation Bioweapons: Genetic Engineering and BW: Michael J. AinscoughDenise Mathre100% (1)
- Healing Within Beginner Guide To Reiki Healing Crystals Healing Mindful Meditation 3rd Eye 201229005245Document49 pagesHealing Within Beginner Guide To Reiki Healing Crystals Healing Mindful Meditation 3rd Eye 201229005245Denise MathreNo ratings yet
- 001 Microcurrent - Therapy - A - Novel - Treatment - M SEE PAGE 5Document11 pages001 Microcurrent - Therapy - A - Novel - Treatment - M SEE PAGE 5Denise MathreNo ratings yet
- Eco LuxBizPlan PDFDocument24 pagesEco LuxBizPlan PDFDenise MathreNo ratings yet
- Visceral Responses To Spinal ManipulationDocument8 pagesVisceral Responses To Spinal ManipulationDenise MathreNo ratings yet
- The Parable of The Good Samaritan Luke CH 10 Verses 25-37Document11 pagesThe Parable of The Good Samaritan Luke CH 10 Verses 25-37Denise Mathre100% (3)
- 11 04 Low Back Pain 40pageDocument40 pages11 04 Low Back Pain 40pageDenise MathreNo ratings yet
- Brain-Immune Interactions in Health and DiseaseDocument2 pagesBrain-Immune Interactions in Health and DiseaseDenise MathreNo ratings yet
- 10 Houses Made From Shipping ContainersDocument10 pages10 Houses Made From Shipping ContainersDenise MathreNo ratings yet
- 12 Container HousesDocument10 pages12 Container HousesDenise Mathre100% (1)
- F1BD 34 Reflexology 130 PageDocument130 pagesF1BD 34 Reflexology 130 PageDenise Mathre100% (2)
- Collaborative Healthcare LeadershipDocument20 pagesCollaborative Healthcare LeadershipDenise MathreNo ratings yet
- Towards A Neurophysiology of The Alexander TechniqueDocument68 pagesTowards A Neurophysiology of The Alexander TechniqueDenise MathreNo ratings yet
- MSA Testing Reveals Body's Energetic HealthDocument4 pagesMSA Testing Reveals Body's Energetic HealthDenise MathreNo ratings yet
- Iron, Brain Ageing and Neurodegenerative DisordersDocument13 pagesIron, Brain Ageing and Neurodegenerative DisordersDenise MathreNo ratings yet
- 36 Foods That Help Detox Your BodyDocument38 pages36 Foods That Help Detox Your BodyDenise MathreNo ratings yet
- Make Market Launch ItDocument169 pagesMake Market Launch ItDenise MathreNo ratings yet
- Benign Paroxysmal Positional VertigoDocument12 pagesBenign Paroxysmal Positional VertigoErnesto Trinidad Jr RNNo ratings yet
- Periarthritis Shoulder By: DR - Sindhu.MPT (Ortho)Document39 pagesPeriarthritis Shoulder By: DR - Sindhu.MPT (Ortho)Michael Selvaraj100% (1)
- Intertwined Movements, Interwoven Histories: HIV & AIDS in TurkeyDocument40 pagesIntertwined Movements, Interwoven Histories: HIV & AIDS in TurkeyGülşah TekinNo ratings yet
- LRD DIV SPE FM 001a RITM Lab Test Request Form - Clinical Lab 1Document1 pageLRD DIV SPE FM 001a RITM Lab Test Request Form - Clinical Lab 1Megen PLCNo ratings yet
- Omega 3 Fatty Acids 1Document16 pagesOmega 3 Fatty Acids 1sarav dhanuNo ratings yet
- Antihuman Globulin TestsDocument6 pagesAntihuman Globulin TestsElla OrtegaNo ratings yet
- Fallen Angels - Walter Dean MyersDocument815 pagesFallen Angels - Walter Dean MyersTache_Georgescu60% (5)
- CV RemyDocument6 pagesCV RemyremythomasNo ratings yet
- Essential Principles of Primary Health CareDocument25 pagesEssential Principles of Primary Health CareEmily BernatNo ratings yet
- Traumatic Brain Injury Final 2013.5.29Document59 pagesTraumatic Brain Injury Final 2013.5.29asylum1968No ratings yet
- Petry, Nancy M - Behavioral Addictions - DSM-5 and Beyond-Oxford University Press (2016) PDFDocument257 pagesPetry, Nancy M - Behavioral Addictions - DSM-5 and Beyond-Oxford University Press (2016) PDFanang7No ratings yet
- Virtual Learning - Insights and Perspectives-Routledge (2022)Document203 pagesVirtual Learning - Insights and Perspectives-Routledge (2022)Dritan LaciNo ratings yet
- CH 7 MseDocument20 pagesCH 7 MseIyanna BaylonNo ratings yet
- BIBC102 Dr. Gen-Sheng FengDocument10 pagesBIBC102 Dr. Gen-Sheng FengpuuuuyaNo ratings yet
- Buprenorphine/naloxone Treatment GuideDocument5 pagesBuprenorphine/naloxone Treatment GuidePhilipNo ratings yet
- Discrimination Resource Dec. 2020Document33 pagesDiscrimination Resource Dec. 2020Fiorella CastilloNo ratings yet
- 001 210197064 Ci2 117 1Document1 page001 210197064 Ci2 117 1tooba arshadNo ratings yet
- Medicine Cupboard Keys Part BDocument6 pagesMedicine Cupboard Keys Part BSojiNo ratings yet
- PDF Dis StandardsDocument35 pagesPDF Dis StandardsEdén PastoraNo ratings yet
- Asphyxia Types and SignsDocument31 pagesAsphyxia Types and SignsSita SilastutiNo ratings yet
- Pill CameraDocument21 pagesPill CameraAnil DsouzaNo ratings yet
- Thyroid Disorders in Children and AdolescentsDocument12 pagesThyroid Disorders in Children and AdolescentsCharity TololiuNo ratings yet
- M5 - Talons of NightDocument54 pagesM5 - Talons of NightThiago PedrozaNo ratings yet
- Hodgkins LymphomaDocument3 pagesHodgkins LymphomaLefe Arvie Dela PeñaNo ratings yet
- Biology: Chapter 1 Invitation To BiologyDocument9 pagesBiology: Chapter 1 Invitation To Biologyamstrghtr94No ratings yet
- The Thalidomide HistoryDocument11 pagesThe Thalidomide HistoryJesus VuelvasNo ratings yet
- Sweet Cherry 1973Document98 pagesSweet Cherry 1973Francisca Beltrán GuzmánNo ratings yet
- Routine Medical Checkup PublicationDocument11 pagesRoutine Medical Checkup Publication백만호No ratings yet
- Roche Cardiac Reader ManualDocument59 pagesRoche Cardiac Reader ManualKate Camat FaminialagaoNo ratings yet
- Short Cases in MedicineDocument30 pagesShort Cases in MedicineselamuNo ratings yet