Professional Documents
Culture Documents
Viral Encephalitis
Uploaded by
DellCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Viral Encephalitis
Uploaded by
DellCopyright:
Available Formats
Downloaded from http://jnnp.bmj.com/ on April 28, 2016 - Published by group.bmj.
com
VIRAL ENCEPHALITIS: CAUSES,
DIFFERENTIAL DIAGNOSIS, AND
MANAGEMENT
i10
P G E Kennedy
J Neurol Neurosurg Psychiatry 2004; 75(Suppl I):i10i15. doi: 10.1136/jnnp.2003.034280
ncephalitis refers to an acute, usually diffuse, inflammatory process affecting the brain.
While meningitis is primarily an infection of the meninges, a combined meningoencephalitis
may also occur. An infection by a virus is the most common and important cause of
encephalitis, although other organisms may sometimes cause an encephalitis. An encephalitic
illness caused by alteration of normal immune function in the context of a previous viral infection
or following vaccination is also well recognised (acute disseminated encephalomyelitis, ADEM).
An infectious encephalitis may also be difficult to distinguish from an encephalopathy that may
be associated with numerous metabolic causes. Among the factors which have helped to focus
attention on viral encephalitis over the last few years have been:
c the development of effective antiviral agents for this condition, most notably acyclovir for
herpes simplex virus encephalitis (HSE) which is caused by herpes simplex virus (HSV)-1 or
HSV-2
c the advent of human immunodeficiency virus (HIV) infection of the central nervous system
(CNS) with its wide range of associated acute viral infections
c the recent recognition of emerging viral infections of the CNS such as West Nile encephalitis
and Nipah virus encephalitis.
This article will address three broad areas of viral encephalitisits causes, differential
diagnosis, and management. While the approach will be a general one, I shall focus particularly
on HSE which is the most frequent cause of sporadic fatal encephalitis in humans in the western
world.
_________________________
Correspondence to:
Professor P G E Kennedy,
Department of Neurology,
University of Glasgow, Institute
of Neurological Sciences,
Southern General Hospital,
Glasgow G51 4TF, UK;
p.g.kennedy@
clinmed.gla.ac.uk
_________________________
www.jnnp.com
CAUSES OF VIRAL ENCEPHALITIS
The various causes of acute infectious viral encephalitis are shown in table 1. While precise figures
for the incidence of encephalitis following these various viruses are not available, estimates have
been given for some of them. For example, it has been estimated that HSE, the most important
treatable viral encephalitis, has an incidence of about one case per million per year.1 About 2000
cases occur annually in the USA.2 About 90% of cases of cases of HSE are caused by HSV-1, with
10% due to HSV-2, the latter usually being the cause of HSE in immunocompromised individuals
and neonates in which it causes a disseminated infection. Molecular analyses of paired oral/labial
and brain sites have indicated that HSE can be the result of a primary infection, a reactivation of
latent HSV, or a re-infection by a second HSV.1 These estimates of HSE may well be
underestimates as judged by the experience of individual neurological centres and detailed
studies using the polymerase chain reaction (PCR). Thus, a small PCR based study suggested that
up to a fifth of patients with HSE may have mild or atypical disease caused by either HSV-1 or
HSV-2, occurring especially in immunocompromised individuals such as those with HIV
infection.3
A recent study in Finland also used PCR to detect various viruses in the CSF of over 3000
patients who had infections of the CNS including encephalitis, meningitis, and myelitis.4 It was
found that, rather surprisingly, varicella zoster virus (VZV), the cause of chickenpox and herpes
zoster, was the most frequently detected virus at 29%, with HSV and enteroviruses accounting for
11% of cases each, and influenza A virus found in 7% of cases. If one assumes a cause-and-effect
relation between the detected virus and the CNS condition in a significant proportion of these
cases, then it indicates that VZV has been generally underestimated, and HSV perhaps
overestimated in frequency. Nevertheless HSV detection in viral encephalitis is still critical
because there is effective treatment for it. Further prospective PCR based studies will be needed to
answer these questions.
While HIV has not been listed as it usually causes a type of subacute encephalitis, it is
important in so far as its associated immunosuppression predisposes the individual to viral
encephalitis caused by, for example, HSV-1, HSV-2, VZV, and cytomegalovirus (CMV). The
frequency and distribution of these viruses clearly varies according to the geographical region,
with large differences seen between Europe, Asia, and the USA. Thus, St Louis virus encephalitis,
which is caused by a mosquito borne arbovirus, occurs in the midwestern and eastern states of the
NEUROLOGY IN PRACTICE
Downloaded from http://jnnp.bmj.com/ on April 28, 2016 - Published by group.bmj.com
USA, and not in the UK, while Japanese encephalitis is a
major problem in Asia, and is the most important cause of
epidemic encephalitis worldwide, causing up to 15000 deaths
annually.5 Two emerging viral infections of the nervous
system which have received much attention recently are West
Nile virus encephalitis and Nipah virus encephalitis. The
former is caused by the transport of neurovirulent strains of
West Nile virus into the Western hemisphere, while the latter
has resulted from the penetration of a newly recognised
paramyxovirus across a species barrier from bat to pig,6 and
represents the first large scale epizoonotic encephalitis
involving direct animal to human transmission.
DIFFERENTIAL DIAGNOSIS OF VIRAL ENCEPHALITIS
The characteristic presentation of viral encephalitis usually
consists of fever, headache, and clouding of consciousness
together with seizures and focal neurology in some cases.
However, the distinction between an infective viral encephalitis and a metabolic encephalopathy or ADEM may not
always be straightforward. Once a diagnosis of infective viral
encephalitis has been established it is then necessary to have
a clear investigative plan to try to determine the likely cause.
These three issues will now be considered in turn.
How can a viral encephalitis be distinguished from a
non-infective encephalopathy?
There are numerous medical conditions which may produce
an encephalopathic illness which may mimic viral encephalitis, and some of the most important of these are listed in
table 2. Particularly prominent among these are systemic
infections which can look very much like an encephalitis on
presentation. In patients recently returning from abroad,
particular vigilance must be paid to the possibility of such
non-viral infections as cerebral malaria which may be rapidly
fatal if not treated early. A number of metabolic conditions
including liver and renal failure and diabetic complications
may also cause confusion. The possible role of alcohol and
drug ingestion must always be considered. Table 2 also
indicates the need to sometimes consider some of the rarer
causes of encephalopathy where appropriate pointers exist.
While the distinction may not always be straightforward,
there are a number of clues which may indicate that the
patient has an infective viral encephalitis rather than a nonviral encephalopathy. Table 3 summarises the most important of these and indicates the need for a careful examination
and usually cranial imaging to exclude a structural lesion
followed by CSF examination. These various clues should not
be taken in isolation but considered as a whole to guide the
Table 1 Causes of viral encephalitis
c
c
c
c
c
c
c
c
c
c
c
Herpes simplex virus (HSV-1, HSV-2)
Other herpes viruses: varicella zoster virus (VZV), cytomegalovirus
(CMV), Epstein-Barr virus (EBV), human herpes virus 6 (HHV6)
Adenoviruses
Influenza A
Enteroviruses, poliovirus
Measles, mumps and rubella viruses
Rabies
Arbovirusesfor example, Japanese B encephalitis, St Louis
encephalitis virus, West Nile encephalitis virus, Eastern, Western, and
Venezuelan equine encephalitis virus, tick borne encephalitis viruses
Bunyavirusesfor example, La Crosse strain of California virus
Reovirusesfor example, Colorado tick fever virus
Arenavirusesfor example, lymphocytic choriomeningitis virus
Modified from Chaudhuri and Kennedy,9 with permission.
clinician, as not all of them are likely to be present in the
same patient. Thus, the author has seen one patient with a
proven metabolic encephalopathy who had a fluctuating
mental status, but has found that the presence or absence of
focal signs and seizures, the presence or absence of
electroencephalographic (EEG) changes, normal or otherwise
cranial imaging, and CSF profile have been particularly
helpful in making the distinction between these two
conditions.
How can an infective viral encephalitis be
distinguished from ADEM?
ADEM, also known as postinfectious encephalomyelitis,
usually follows either a vaccination within the preceding
four weeks, or an infection which may be a childhood
exanthema such as measles, rubella or chickenpox, or else a
systemic infection characteristically affecting the respiratory
or gastrointestinal systems.7 There is very good evidence from
various sources to suggest an immune pathogenesis of this
disorder, with an abnormal immune reaction directed against
normal brain. Potential immune mechanisms include molecular mimicry between epitopes expressed by myelin antigens
and viral or other pathogens, immune dysregulation, superantigen induction, and a direct result of the infection.8 It is
important to distinguish ADEM from acute infectious
encephalitis, acute non-infectious encephalitis, and an acute
metabolic or toxic encephalopathy.8 While the diagnosis may
not always be immediately obvious, there are a number of
helpful clues in the history, examination, and investigative
profile that may greatly assist in the distinction between
ADEM and an infectious encephalitis. These differences have
been very clearly identified by Davis7 and are summarised in
table 4. The typical clinical picture is of a younger person with
a history of vaccination or infection presenting abruptly,
without fever at the onset of symptoms, and with multifocal
neurological signs affecting both the CNS and possibly the
peripheral nerve roots.9 It should also be appreciated that
ADEM can also present with a very restricted neurological
picture such as transverse myelitis, optic neuritis, and
cerebellar ataxia, and differentiation from acute multiple
sclerosis can sometimes be difficult. As is the case for table 3,
these various diagnostic pointers should be taken together
and not in isolation when trying to make the diagnosis of
ADEM.
How can the likely cause of an acute infective
encephalitis be determined?
The possible viral causes of acute infectious encephalitis have
already been listed in table 1. There are also numerous nonviral causes of infectious encephalitis comprising various
bacteria, rickettsia, fungi, and parasites; these are broadly,
but not exhaustively, summarised in table 5. The general
diagnostic approach to the differential diagnosis which I shall
outline here is straightforward, and consists of the history,
examination and then general and neurological investigations. However, it should be appreciated that in approximately half of cases the cause of viral encephalitis is not
found.
Historical clues
A carefully taken history, usually obtained from the comatose
patients relatives, is of crucial importance in determining the
likely cause of encephalitis. The presence of a prodromal
illness, or a recent vaccination, may indicate ADEM, as would
www.jnnp.com
i11
Downloaded from http://jnnp.bmj.com/ on April 28, 2016 - Published by group.bmj.com
Examination clues
Table 2 Common causes of encephalopathy
c
c
c
c
c
i12
c
c
c
c
c
c
c
c
Anoxic/ischaemic
Metabolic
Nutritional deficiency
Toxic
Systemic infections
Critical illness
Malignant hypertension
Mitochondrial cytopathy (Reyes and MELAS syndromes)
Hashimotos encephalopathy
Paraneoplastic
Neuroleptic malignant syndrome
Traumatic brain injury
Epileptic (non-convulsive status)
Reproduced from Chaudhuri and Kennedy,9 with permission.
a clinical development over a few days. A biphasic onset with
a systemic illness followed by CNS disease is characteristic of
enterovirus encephalitis.9 HSE usually has an abrupt onset
with rapid progression over a few days, but there are no
clearly distinguishing features that can be used to differentiate HSE from the other causes of viral encephalitis.7 A
history of recent travel and the geographical context of the
illness may also be important. For example, both cerebral
malaria and human African trypanosomiasis should be considered in a patient who has recently travelled to Africa,
Japanese encephalitis in the case of travel to Asia, and Lyme
disease in the case of travel to high risk regions of Europe and
the USA. A history of recent animal bites should raise suspicion of tick borne encephalitis or even rabies, and recent
contact with infectious conditions such as a childhood exanthema or polio may also be relevant. The occupation of the
patient may also be relevantfor example, a forest worker
may be exposed to tick bites and medical personnel may have
had recent exposure to individuals with infectious diseases.
The season may also be relevantfor example, Japanese
encephalitis is more common during the rainy season and
arbovirus infections in the USA are more frequent during the
summer and autumn months. Any predisposing factors
should also be noted such as immunosuppression caused
by disease and/or drug treatment. Individuals with organ
transplants are particularly prone to opportunistic infections
such as listeria, aspergillosis and cryptococcus, and HIV
patients are also prone to a variety of CNS infections including HSV-2 encephalitis and CMV infection. A possible history
of drug ingestion and/or abuse may also be highly relevant.
Table 3
NEUROLOGY IN PRACTICE
A thorough general examination may reveal systemic
features indicating, for example, involvement of the respiratory or gastrointestinal systems. Skin rashes may indicate
VZV or other viral infection such as measles, as well as nonviral causes such as rickettsial infection. Evidence of bites
may point towards a possible diagnosis of Lyme disease or
rabies. The incidence of cold sores in patients with HSE has
not been shown to be different from that in the normal
population and so they are not diagnostic.
Neurological examination may reveal focal features such as
fronto-temporal signs, aphasia, personality change, and focal
seizures which are characteristic of HSE, but such focality
may be minimal during acute viral encephalitis and may not
be diagnostic of a particular viral cause. It has recently been
recognised that about 20% of HSE cases may be relatively
mild and atypical without the typical focal features.3 Raised
intracranial pressure may be evident but does not necessarily
occur, certainly at the early stages. If the peripheral nervous
system is involved then this raises the possibility of the
encephalitis being ADEM or an infection with CMV, VZV or
Epstein-Barr virus (EBV), which can all produce a combination of central and peripheral signs. The presence of myelitis
or poliomyelitis points away from HSE and towards the
possibility of polio, enterovirus, or arbovirus infection
(especially West Nile virus and Japanese encephalitis).
Investigations
These are both general and specifically neurological.
General investigations include a routine full haematological and biochemical blood screen. A leucocytosis is common
in ADEM and a relative lymphocytosis may occur in viral
encephalitis. A leucopenia may occur in rickettsial infections,
and a very raised erythrocyte sedimentation rate (ESR) might
suggest tuberculosis or underlying malignancy. A thin and
thick peripheral blood smear may be required in cases of
suspected cerebral malaria. Biochemical screening is required
in cases of suspected metabolic encephalopathy. A drug
screen and urine analysis may also be relevant in some cases.
A chest x ray should always be performed and if abnormal
raises the possibilities of tuberculosis, mycoplasma, malignancy, and legionella. Serological investigations may be
diagnostically useful but usually take over a week to perform
which is of no utility in the acute situation. However, the
presence of cold agglutinins can be quickly determined and,
if positive, indicate a diagnosis of mycoplasma; an enzyme
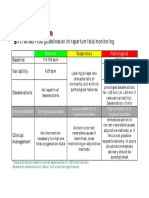
Frequent differences between encephalopathy and encephalitis
Clinical features
Fever
Headache
Depressed mental status
Focal neurologic signs
Types of seizures
Laboratory findings
Blood
CSF
EEG
MRI
Encephalopathy
Encephalitis
Uncommon
Uncommon
Steady deterioration
Uncommon
Generalised
Common
Common
May fluctuate
Common
Generalised or focal
Leucocytosis uncommon
Pleocytosis uncommon
Diffuse slowing
Often normal
Leucocytosis common
Pleocytosis common
Diffuse slowing and focal abnormalities
Focal abnormalities
Reproduced from Davis,7 with permission.
These features are only guidelines for the clinician to help in the distinction between the two conditions. An
individual patient is likely to show various combinations of these features.
CSF, cerebrospinal fluid; EEG, electroencephalogram; MRI, magnetic resonance imaging.
www.jnnp.com
Downloaded from http://jnnp.bmj.com/ on April 28, 2016 - Published by group.bmj.com
NEUROLOGY IN PRACTICE
Table 4 Comparison of acute disseminated encephalomyelitis and infectious encephalitis
Clinical features
Most common age
Recent vaccination
Prodromal illness
Fever
Visual loss (one or both eyes)
Spinal cord signs
Laboratory findings
Blood
MRI (T2 weighted)
CSF
Acute disseminated encephalomyelitis
Infectious encephalitis
Children
Common
Usually
May occur
May occur
May occur
Any age
Uncommon
Occasionally
Common
Uncommon
Rare
Leucocytosis occasionally occurs
Multiple focal areas of hypertensity that are the same
and may involve white matter of both hemispheres,
basal ganglia, brainstem, cerebellum, and spinal cord
Lymphocytic pleocytosis, elevated protein, normal
glucose, and negative cultures. Red blood cells seen
in acute haemorrhagic leucoencephalitis.
Leucocytosis common
One or more diffuse areas of hypertensity involves the grey
matter of both cerebral cortices and its underlying white matter
and, to a lesser extent, basal ganglia, brainstem, and cerebellum
Lymphocytic pleocytosis, elevated protein, normal glucose, and
negative cultures. Red blood cells may be seen in herpes simplex
encephalitis.
i13
Reproduced, in part, from Davis, with permission.
linked immunosorbent assay (ELISA) can detect IgM
antibodies to arboviruses as a rapid method of diagnosis.
Viral culture from different sites may assist in eventual
diagnosis, but in the authors opinion is seldom of use in the
acute situation.
Neurological investigation usually starts with cranial
imaging with a computed tomographic (CT) or magnetic
resonance imaging (MRI) scan, primarily to exclude quickly
an intracranial tumour or abscess, but also to yield specific
diagnostic information. MRI is the imaging of choice in
suspected cases of viral encephalitis, although CT scanning
may be used where MRI facilities are not available. CT may be
normal in HSE, especially early in the illness, but characteristically shows reduced attenuation in one or both temporal
lobes or areas of hyperintensity.7 MRI is sensitive in the early
stages of HSE although rarely it may be normal in this
Table 5 Non-viral causes of infectious encephalitis
Bacterial
Mycobacterium tuberculosis
Mycoplasma pneumoniae
Listeria monocytogenes
Borrelia burgdorferi
Leptospirosis
Brucellosis
Leptospirosis
Legionella
Tropheryma whippeli (Whipples disease)
Nocardia actinomyces
Treponema pallidum
Salmonella typhi
All causes of pyogenic meningitis
Rickettsial
Rickettsia rickettsia (Rocky Mountain spotted fever)
Rickettsia typhi (endemic typhus)
Rickettsia prowazeki (epidemic typhus)
Coxiella burnetti (Q fever)
Ehrlichiosis (Ehrlichia chaffeensishuman monocytic ehrlichiosis)
Fungal
Cryptococcus
Aspergillosis
Candidiasis
Coccidiomycosis
Histoplasmosis
North American blastomycosis
Parasitic
Human African trypanosomiasis (sleeping sickness)
Cerebral malaria
Toxoplasma gondii
Echinococcus granulosus
Schistosomiasis
Modified from Chaudhuri and Kennedy,9 with permission.
condition. The typical MRI features in HSE are areas of focal
oedema in the temporal lobes and orbital surface of the
frontal lobes as well as the insular cortex and angular gyrus10
(fig 1); abnormal areas may show enhancement with
gadolinium. Midline shift may be present in cases with
significant cerebral oedema. Some other types of viral
encephalitis such as Japanese encephalitis and eastern
equine encephalitis are also associated with particular MRI
abnormalities. Where available, functional imaging such as
SPECT (single photon emission computed tomography) may
yield additional useful information in cases of viral encephalitisfor example, temporal lobe hyperperfusion may be a
marker of HSE. An EEG should also be performed in all cases
of possible encephalitis, and is particularly useful in the
distinction between encephalitis and metabolic encephalopathy. The EEG is invariably abnormal in HSE showing either
early non-specific slowing or later PLEDS (periodic
lateralising epileptiform discharges), although these are not
themselves diagnostic of HSE.
Figure 1 HSE. T2 weighted MRI showing extensive area of increased
signal in right temporal lobe and lesser involvement of the left.
Reproduced from Baringer10, with permission.
www.jnnp.com
Downloaded from http://jnnp.bmj.com/ on April 28, 2016 - Published by group.bmj.com
NEUROLOGY IN PRACTICE
i14
Figure 2
Suggested flow chart for basic management of suspected herpes simplex encephalitis (HSE).
Provided cranial imaging has excluded any contraindications such as a space occupying lesion or severe cerebral
oedema and brain shift, a CSF analysis by lumbar puncture
should be carried out in cases of suspected encephalitis.
When significant cerebral oedema is present, I favour
treatment with steroids and/or mannitol to reduce the
intracranial pressure before lumbar puncture being reconsidered. Although about 5% of patients with HSE have a
normal CSF profile, the typical features of HSE are a
lymphocyte cell of 10200/mm3 and an increased protein of
0.66 g/l.11 A low CSF glucose is rare in viral encephalitis but
when it occurs it raises the possibility that the encephalitis is
actually caused by tuberculous meningoencephalitis. While
xanthochromia may be present in HSE it is of no specific
diagnostic value.10 The diagnosis of viral encephalitis has
been greatly facilitated by CSF PCR. In an experienced
diagnostic laboratory the CSF will should be positive for HSV
DNA in about 95% of cases during the first week of the
illness, with false negative results most likely occurring
within the first 2448 hours or after 1014 days of the illness.
The specificity of this test for HSE is over 95%. PCR can also
be used to help diagnose viral encephalitis from other causes
such as CMV, VZV, influenza, and enterovirus infection.
While serum and CSF are frequently taken for estimation of
viral antibody titres in the acute and convalescent phases,
these are of little value in the acute management of the
patient because of the delay in obtaining the results. Brain
biopsy is now seldom performed largely because of the
advent of acyclovir treatment (see below) and CSF PCR
www.jnnp.com
diagnosis, but still may have to be considered where there is
serious diagnostic doubt.
MANAGEMENT OF VIRAL ENCEPHALITIS
This can be considered from both the general and specific
aspects.
The general management is essentially supportive and in
severe cases is likely to be in a high dependency medical
environment. Focal and generalised seizures need to be
treated effectively with anticonvulsants, typically intravenous
fosphenytoin in the first instance. While a degree of raised
intracranial pressure, not requiring treatment, may well be
present in viral encephalitis, it may become severe as
evidenced by the development of papilloedema and rapid
clinical deterioration, and severe sulcal effacement and
midline shift on brain imaging. Such significantly raised
intracranial pressure should be treated with intravenous
mannitol and/or steroids. Despite the lack of an evidence
base, the author does not usually withhold steroids in this
situation, especially if the encephalitis is already being
treated with antiviral agents. In the case of rapidly increasing
intracranial pressure with clinical deterioration unresponsive
to medical treatment, very serious consideration should be
given to surgical decompression which can be lifesaving if
carried out in time. In addition, other complications such as
fluid and electrolyte imbalance, secondary bacterial infections, aspiration pneumonia, respiratory failure, and cardiac
abnormalities should be detected early and treated appropriately. In the case of ADEM, steroids are frequently given
NEUROLOGY IN PRACTICE
Downloaded from http://jnnp.bmj.com/ on April 28, 2016 - Published by group.bmj.com
but in fact there have been no placebo controlled studies to
prove their efficacy or otherwise in this condition.
If antiviral therapy is not given to patients with HSE the
mortality is over 70%.12 Specific antiviral therapy for HSE is
intravenous acyclovir, a nucleoside analogue which acts
specifically against virus infected cells which explains its
remarkable safety and lack of toxicity. This drug has
revolutionised the treatment and prognosis of HSE, although
even with acyclovir therapy the morbidity and mortality is
unacceptably high at 28% at 18 months after treatment.12 If
HSE is a definite possibility then acyclovir, 10 mg/kg three
times daily, should be started as soon as possible. When the
diagnosis is confirmed by CSF PCR, and/or where there are
characteristic MRI changes, acyclovir should be continued for
14 days. During this period renal function should be closely
monitored because of the rare development of renal impairment. Acyclovir should only be stopped where there is a
definite alternative diagnosis made, otherwise a deterioration
after cessation of therapy may be very difficult to interpret
and manage.11 The situation of still suspected HSE in the
presence of a negative CSF PCR and MRI is less easy to
manage. My own preference is to give acyclovir for 10 days in
this scenario. This suggested scheme of management is
summarised in fig 2. The prognosis of HSE is better in
younger patients, and those having a disease duration of four
days or less and a Glasgow coma score of 6 or less at the time
of acyclovir initiation.12 In some centres the CSF PCR is
repeated at the end of acyclovir treatment and a further
course of acyclovir recommended if it is positive to prevent a
relapse.13 At present, the evidence base for this approach is
awaited and in the authors centre this is not routine practice.
However, the Collaborative Antiviral Study Group has just
initiated a study in which this issue will be clarified and also
the efficacy or otherwise of a 90 day course of oral
valacyclovir after 14 days of acyclovir treatment will be
determined. Thus this practice could become standard in the
future. For CMV encephalitis, particularly prominent in HIV
infection, combination therapy with intravenous gancyclovir
plus or minus foscarnet has been recommended,9 but there is
not the evidence base in this condition that exists in the case
of HSE therapy with acyclovir.
i15
ACKNOWLEDGEMENTS
I wish to thank Professor Larry Davis for very helpful discussions and
his critical review of the manuscript.
REFERENCES
1 Whitley R, Laeman AD, Nahmias A, et al. DNA restriction enzyme analysis of
herpes simplex virus isolates obtained from patients with encephalitis.
N Engl J Med 1982;307:10602.
2 Johnston RT. Viral infections of the nervous system, 2nd ed. Philadelphia:
Lippincott-Raven, 1998.
3 Fodor PA, Levin MJ, Weinberg A, et al. Atypical herpes simplex virus
encephalitis diagnosed by PCR amplification of viral DNA from CSF.
Neurology 1998;51:5549.
4 Koskiniemi M, Rantalaiho T, Piiparinen H, et al. Infections of the central
nervous system of suspected viral origin: a collaborative study from Finland.
J Neurovirol 2001;7:4008.
5 Solomon T. Recent advances in Japanese encephalitis. J Neurovirol
2003;9:27483.
6 Johnson RT. Emerging viral infections of the nervous system. J Neurovirol
2003;9:1407.
7 Davis LE. Diagnosis and treatment of acute encephalitis. The Neurologist
2000;6:14559.
8 Coyle PK. Postinfectious encephalomyelitis. In: Davis LE, Kennedy PGE, eds.
Infectious diseases of the nervous system, 1st ed. Butterworth-Heinemann,
2000:83108.
9 Chaudhuri A, Kennedy PGE. Diagnosis and treatment of viral encephalitis.
Postgrad Med J 2002;78:57583.
10 Baringer JR. Herpes simplex virus encephalitis. In: Davis LE, Kennedy PGE,
eds. Infectious diseases of the nervous system, 1st ed. Butterworth-Heinemann,
2002:13964.
11 Kennedy PGE, Chaudhuri A. Herpes simplex encephalitis. J Neurol
Neurosurg Psychiatry 2002;73:2378.
12 Whitley RJ, Gnann JW. Viral encephalitis: familiar infections and emerging
pathogens. Lancet 2002;359:50714.
13 Cinque P, Cleator GM, Weber T, et al. The role of laboratory investigation in
the diagnosis and management of patients with suspected herpes simplex
encephalitis: a consensus report. J Neurol Neurosurg Psychiaryt
1996;61:33945.
www.jnnp.com
Downloaded from http://jnnp.bmj.com/ on April 28, 2016 - Published by group.bmj.com
VIRAL ENCEPHALITIS: CAUSES,
DIFFERENTIAL DIAGNOSIS, AND
MANAGEMENT
P G E Kennedy
J Neurol Neurosurg Psychiatry 2004 75: i10-i15
doi: 10.1136/jnnp.2003.034280
Updated information and services can be found at:
http://jnnp.bmj.com/content/75/suppl_1/i10
These include:
References
Email alerting
service
Topic
Collections
This article cites 9 articles, 3 of which you can access for free at:
http://jnnp.bmj.com/content/75/suppl_1/i10#BIBL
Receive free email alerts when new articles cite this article. Sign up in the
box at the top right corner of the online article.
Articles on similar topics can be found in the following collections
HIV/AIDS (104)
Immunology (including allergy) (1834)
Infection (neurology) (466)
Multiple sclerosis (882)
Spinal cord (515)
Notes
To request permissions go to:
http://group.bmj.com/group/rights-licensing/permissions
To order reprints go to:
http://journals.bmj.com/cgi/reprintform
To subscribe to BMJ go to:
http://group.bmj.com/subscribe/
You might also like
- Disertasi Dr. TerawanDocument8 pagesDisertasi Dr. TerawanNurhaidah AchmadNo ratings yet
- B135 Work and EpilepsyDocument33 pagesB135 Work and EpilepsyDrSajid BuzdarNo ratings yet
- Labour and Delivery Care Module - 4 Using The Partograph - View As Single PageDocument21 pagesLabour and Delivery Care Module - 4 Using The Partograph - View As Single PageDellNo ratings yet
- Year 4 OSCEguideDocument159 pagesYear 4 OSCEguideDrSajid BuzdarNo ratings yet
- HTN Late PregnancyDocument2 pagesHTN Late PregnancyDellNo ratings yet
- KADDocument30 pagesKADDellNo ratings yet
- Module 14 Pediatric TB ENGLISHDocument85 pagesModule 14 Pediatric TB ENGLISHDellNo ratings yet
- Sliwa Et Al-2017-European Journal of Heart FailureDocument11 pagesSliwa Et Al-2017-European Journal of Heart FailureDellNo ratings yet
- KADDocument30 pagesKADDellNo ratings yet
- Nature CardiologyDocument7 pagesNature CardiologyDellNo ratings yet
- SalerioDocument28 pagesSalerioRizqaFebrilianyNo ratings yet
- GLM0021 Postpartum HaemorrhageDocument13 pagesGLM0021 Postpartum HaemorrhageDellNo ratings yet
- SPSS Crosstab PDFDocument3 pagesSPSS Crosstab PDFDellNo ratings yet
- Clinical Yeoh PDFDocument5 pagesClinical Yeoh PDFAzizan HannyNo ratings yet
- Year 4 OSCEguideDocument159 pagesYear 4 OSCEguideDrSajid BuzdarNo ratings yet
- Fitzpatrick's Dermatology in General Medicine, Eighth Edition, 2 Volume SetDocument30 pagesFitzpatrick's Dermatology in General Medicine, Eighth Edition, 2 Volume SetDellNo ratings yet
- Clinical Diagnosis and Complications of Paratubal Cysts: Review of The Literature and Report of Uncommon PresentationsDocument10 pagesClinical Diagnosis and Complications of Paratubal Cysts: Review of The Literature and Report of Uncommon PresentationsDellNo ratings yet
- Sliwa Et Al-2017-European Journal of Heart FailureDocument11 pagesSliwa Et Al-2017-European Journal of Heart FailureDellNo ratings yet
- Journal Pone 0158499Document11 pagesJournal Pone 0158499DellNo ratings yet
- Jurnal Farmakologi Anti Konvulsi PDFDocument13 pagesJurnal Farmakologi Anti Konvulsi PDFtherempongss100% (1)
- NICEguidelineonAEDsAugust2014 0Document3 pagesNICEguidelineonAEDsAugust2014 0DellNo ratings yet
- Family Planning HandbookDocument387 pagesFamily Planning HandbookvthiseasNo ratings yet
- 5 Morisky Medication Adherence-Scale PDFDocument1 page5 Morisky Medication Adherence-Scale PDFDellNo ratings yet
- TB CutisDocument16 pagesTB CutisDellNo ratings yet
- CE-Hypertension The Silent KillerDocument8 pagesCE-Hypertension The Silent KillerD.E.P.HNo ratings yet
- A Practical Classification of Septonasal Deviation.42Document3 pagesA Practical Classification of Septonasal Deviation.42DellNo ratings yet
- CTG Classification PDFDocument1 pageCTG Classification PDFDellNo ratings yet
- 144TD (C) 25 (E3) - Issue No 3 - Ear, Nose and Throat (ENT) Infections Antibiotic Guidelines PDFDocument9 pages144TD (C) 25 (E3) - Issue No 3 - Ear, Nose and Throat (ENT) Infections Antibiotic Guidelines PDFDellNo ratings yet
- Jnma00266 0071Document4 pagesJnma00266 0071DellNo ratings yet
- Functional Endoscopic Sinus Surgery - American Family PhysicianDocument8 pagesFunctional Endoscopic Sinus Surgery - American Family PhysicianDellNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5784)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Postpartum Fever Presentation: Causes, Symptoms and TreatmentDocument14 pagesPostpartum Fever Presentation: Causes, Symptoms and TreatmentRamandeep KaurNo ratings yet
- Document from அகத்தியன் அகாடமிDocument4 pagesDocument from அகத்தியன் அகாடமிarunkumarNo ratings yet
- ERYTHROLEUKOPLAKIADocument14 pagesERYTHROLEUKOPLAKIARajsandeep Singh100% (1)
- COVID-19's Impact on Student Lifestyles and Mental HealthDocument9 pagesCOVID-19's Impact on Student Lifestyles and Mental HealthAjay LakshmananNo ratings yet
- 248413-Article Text-594567-1-10-20230527Document8 pages248413-Article Text-594567-1-10-20230527Dewi RizkiNo ratings yet
- MCQ 2019 Part 1 UseDocument94 pagesMCQ 2019 Part 1 UseMimmey YeniwNo ratings yet
- Medical Certificate Form For Non Immigrant O A Long Stay OnlyDocument1 pageMedical Certificate Form For Non Immigrant O A Long Stay OnlyFiroz KhanNo ratings yet
- Presentation 5 The Infection Control Risk Assessment and PlanDocument24 pagesPresentation 5 The Infection Control Risk Assessment and PlanLany PasauNo ratings yet
- Supercare Medical Services, Inc. Health Declaration Form: Remarks of Examining PhysicianDocument1 pageSupercare Medical Services, Inc. Health Declaration Form: Remarks of Examining PhysicianJunexielJalop100% (1)
- Bleeding Disorders FinalDocument35 pagesBleeding Disorders FinalsanthiyasandyNo ratings yet
- Nephrotic SyndromeDocument28 pagesNephrotic Syndromerupali khillareNo ratings yet
- Diabetes MellitusDocument29 pagesDiabetes MellitusFourthMolar.com100% (1)
- Global Impact of The First Year of COVID-19 VaccinationDocument10 pagesGlobal Impact of The First Year of COVID-19 VaccinationRoel PlmrsNo ratings yet
- Necrotizing FasciitisDocument5 pagesNecrotizing Fasciitisnsl1225No ratings yet
- Exercise 4.1Document1 pageExercise 4.1Belle LatNo ratings yet
- 2014 Final Paediatric Exam (تم الحفظ تلقائيًا)Document258 pages2014 Final Paediatric Exam (تم الحفظ تلقائيًا)wea xcz100% (4)
- Morpheus8 Consent FormDocument3 pagesMorpheus8 Consent FormOnurNo ratings yet
- PCV Septia 2003Document16 pagesPCV Septia 2003WondaNo ratings yet
- Lecture 1 - Smear Positive PTBDocument40 pagesLecture 1 - Smear Positive PTBNasibah Tuan YaacobNo ratings yet
- Epstein-Barr Virus and MonoDocument2 pagesEpstein-Barr Virus and MonoMihai PetrescuNo ratings yet
- 紅白斑Document20 pages紅白斑b202104023 TMUNo ratings yet
- Dr. Dhani Redhono Hariosaputro, SP - PD-KPTI - Invasive Fungal Infection in SepsisDocument32 pagesDr. Dhani Redhono Hariosaputro, SP - PD-KPTI - Invasive Fungal Infection in SepsisOlivia DwimaswastiNo ratings yet
- Slow Contact Tracing' Blamed For Spread of New CoronavirusDocument6 pagesSlow Contact Tracing' Blamed For Spread of New CoronavirusProdigal RanNo ratings yet
- Community DentistryDocument5 pagesCommunity DentistryDenis BaftijariNo ratings yet
- Leg and Feet Swelling Natural RemediesDocument4 pagesLeg and Feet Swelling Natural Remediesghica05100% (1)
- Princess Arianne Macaranas Five Hello Rache PracticeDocument2 pagesPrincess Arianne Macaranas Five Hello Rache PracticeDianne MacaranasNo ratings yet
- RSV Bronchiolitis Discharge SummaryDocument2 pagesRSV Bronchiolitis Discharge SummaryIndranil SinhaNo ratings yet
- Toms River Regional School District Athletic Waiver and Release of Liability Form Related To COVID-19Document4 pagesToms River Regional School District Athletic Waiver and Release of Liability Form Related To COVID-19Asbury Park PressNo ratings yet
- Connect with a Vet for Canine Adenovirus 1 AdviceDocument3 pagesConnect with a Vet for Canine Adenovirus 1 Adviceaurrasinger9157No ratings yet
- Arora PLAB 2 60 Day Planner - Min2Document9 pagesArora PLAB 2 60 Day Planner - Min2malmegrimNo ratings yet