Professional Documents
Culture Documents
Awuku 1552016 BJMMR26166
Uploaded by
Kush GuptaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Awuku 1552016 BJMMR26166
Uploaded by
Kush GuptaCopyright:
Available Formats
British Journal of Medicine & Medical Research
15(5): 1-4, 2016, Article no.BJMMR.26166
ISSN: 2231-0614, NLM ID: 101570965
SCIENCEDOMAIN international
www.sciencedomain.org
Primary HIV Infection as an Unusual Cause of
Neutropenia in Crohns Disease: A Case Report
Y. A. Awuku1*, S. R. Thomson1, D. Levin1, S. Hlashtwayo1
and G. Watermeyer1
1
Division of Gastroenterology, Groote Schuur Hospital, Cape Town, South Africa.
Authors contributions
This work was carried out in collaboration between all authors. Author YAA developed the idea and
wrote the manuscript, author GW developed the idea and wrote the manuscript, author SRT wrote
and reviewed the manuscript, authors DL and SH reviewed the manuscript. All authors read and
approved the final manuscript.
Article Information
DOI: 10.9734/BJMMR/2016/26166
Editor(s):
(1) Ricardo Forastiero, Professor of Physiology and Internal Medicine, Haematology, Favaloro University,
Argentina.
Reviewers:
(1) Vicente Estrada, Universidad Complutense, Madrid, Spain.
(2) Einar Arnbjornsson, Skane University Hospital, Lund, Sweden.
Complete Peer review History: http://sciencedomain.org/review-history/14372
th
Case Study
Received 4 April 2016
Accepted 22nd April 2016
th
Published 28 April 2016
ABSTRACT
Although primary human immune deficiency virus (HIV) infection is a well described entity, it is
frequently misdiagnosed or underdiagnosed. This has been attributed to the non-specific clinical
features at presentation, inadequate history taking and a low index of suspicion by practicing
clinicians. Haematological abnormalities are a recognised feature of HIV infection and may present
in the form of pancytopenia or isolated cytopenias. One of the cardinal features of HIV
seroconversion is leucopenia, however primary HIV infection as a cause of neutropenia and
lymphopaenia in Crohns disease, has to our knowledge, not been described in the medical
literature. We present a case of profound neutropenia in Crohns disease secondary to acute HIV
sero-conversion illness.
Keywords: Crohns disease; neutropenia; primary HIV infection; HIV sero-conversion; azathioprine.
_____________________________________________________________________________________________________
*Corresponding author: E-mail: ppawuku@gmail.com;
Awuku et al.; BJMMR, 15(5): 1-4, 2016; Article no.BJMMR.26166
surgical resections of his terminal ileum and
caecum as a result of recurrent episodes of
partial small bowel obstruction. As a
consequence of severe, refractory perianal
disease he underwent an abdominoperineal
resection in 2004 and currently has a sigmoid
end-colostomy. Although his compliance with
medical therapy has been poor in the past he
has been receiving azathioprine without side
effects since January 2010. His TPMT genotype
testing excluded common mutations. He has
subsequently been in clinical remission.
1. INTRODUCTION
Since its initial description in 1985 the diagnosis
of primary human immune deficiency virus (HIV)
infection remains a challenge in clinical practice
[1]. Primary HIV infection, also known as HIV
sero-conversion sickness or acute retroviral
syndrome, encompasses all acute and recent
HIV infections (within 6-12 months of exposure)
[1]. This disease entity is often misdiagnosed or
underdiagnosed, primarily due to the non-specific
presenting features of the illness, inadequate
history taking or a low index of suspicion by
clinicians [2]. Haematological abnormalities are a
recognised feature of primary HIV infection and
typically present as either a pancytopenia or
isolated
cytopenias.
The
incidence
of
neutropenia varies from 5 to 10 percent in the
early phase, to as high as 50 to 70 percent in the
advanced stage of the infection [3]. HIV seroconversion illness should thus be considered in
the work up of any patient with unexplained
neutropenia or lymphopaenia.
He presented to our clinic in 2012 with a 5 day
history of watery non-bloody diarrhoea. He
denied having any concurrent abdominal cramps,
fever, nausea, vomiting, or weight loss. He also
described a week history of odynophagia and
painful oral ulcers. There was no recent travel
history of note. He did however admit having
unprotected sexual intercourse three weeks
before this presentation.
On examination he was afebrile with a
temperature 36.5C, he was not pale and there
were no features of jaundice or pedal oedema.
On further examination he had sunken eyes and
reduced skin turgor in keeping with dehydration.
He also had multiple painful oral aphthous ulcers.
On examination of his abdomen mild generalised
tenderness was noted and his stoma bag
contained large volumes of greenish watery
stool. Perianal examination revealed scarring as
well as an active sinus with minimal drainage.
There was no abscess present. Cardiovascular,
respiratory, and neurological examinations were
unremarkable.
Crohns disease (CD) is a form of inflammatory
Bowel Disease (IBD) which may affect any part
of the gastrointestinal tract in a discontinuous
fashion from mouth to anus, most commonly the
terminal ileum. CD is a life-long disorder which
frequently follows a progressive and destructive
course resulting in irreversible GIT damage. Over
the past decade, there has been an evolution in
treatment
paradigms
with
conventional
immunomodulators such as the thiopurines
azathioprine and 6-mercaptopurine now being
introduced far earlier in the disease course, in an
attempt to change the natural history of CD.
Unfortunately these drugs carry an appreciable
risk of neutropaenia; especially in subjects with
thiopurine methyl transferase (TPMT) mutations
[4]. The use of thiopurines is the commonest
cause of neutropenia in CD. However
neutropenia secondary to HIV sero-conversion
has not previously been described in CD. In this
case report we describe a middle age male with
longstanding CD whose work up for neutropenia
demonstrated primary HIV infection as the
aetiology.
Our initial concern was that he was having an
acute flare of CD, however this was ruled out on
radiological investigations, as well as a
colonoscopy via the stoma which showed
quiescent CD.No pathogens were identified on
stool analysis. Blood cultures were negative and
chest and abdominal x-rays were unremarkable.
At this point we had a very low index of suspicion
for primary HIV infection as the cause.
An
initial
complete
blood
count
was
unremarkable except for mild leucopenia with a
9
white cell count (WBC) of 3.610 /l (4.00-10.00).
His baseline renal function tests were in keeping
with dehydration and pre-renal failure; with a
urea of 22.1 mmol/l (2.6-7.0) and a creatinine of
189 umol/l (64-104).His CRP was elevated 19.9
mg/l (0.0-5.0).He was initially managed with
empiric antibiotics and intravenous rehydration.
2. CASE REPORT
The subject in question is a 53year old
unemployed male, first diagnosed with ileocaecal
and perianal CD in 1985. He is a long standing
smoker. He also has a history of pulmonary
tuberculosis treated in 1997 and chronic
obstructive pulmonary disease. During the
course of his illness he has undergone multiple
2
Awuku et al.; BJMMR, 15(5): 1-4, 2016; Article no.BJMMR.26166
On repeat blood investigations 3 days after
admission his leucopenia was much worse with a
reduction in all white cell lines. His total WBC
9
was 1.9x10 /l (4.00-10.00), his neutrophil count
was 1.29(2.00-7.50), monocytes count was 0.04
(0.18-0.8), and his lymphocyte count was 0.53
(1.00-4.00). His platelet count was normal. His
electrolyte profile had normalised following
rehydration.
usually last 4 days, but may persist for as long as
10 weeks. The formation of HIV-1 specific
antibodies
marks
the
completion
of
seroconversion, and these are generally
detectable within 3-12 weeks [6,7]. The clinical
features are non-specific and may mimic other
clinical conditions. Multiple organs can be
affected, resulting in a broad spectrum of
symptoms and signs [8]. Constitutional
symptoms of fever, malaise or fatigue are
common. Patients may also suffer anorexia,
weight loss or a maculopapular skin rash. As
seen in our case, mucosal membrane ulcerations
are common, as is diffuse lymphadenopathy.
Gastrointestinal symptoms such as nausea,
vomiting and diarrhoea are well described, while
a productive cough is the main pulmonary
manifestation. Neurological and psychiatric
disorders such as meningitis or encephalitis are
not uncommon. In addition liver involvement with
raised transaminases have also been described.
One of the commonest abnormalities seen in
acute HIV infections are however haematological
in nature, in particular leucopenia, neutropaenia,
lymphopenia and thrombocytopenia. These are
usually transient and tend to resolve rapidly
[5,6].
The initial concern was that these abnormalities
were secondary to the use of azathioprine and
the drug was discontinued. However given that
these findings were also suggestive of HIV seroconversion, an HIV test was requested. The HIV
Antigen/Antibody and ELISA were weakly
positive; however the viral load was exceedingly
high (552240 copies/ml) confirming acute seroconversion. His CD4 count was 517 cells/ml. In
consultation with our haematology unit, a bone
marrow biopsy was deemed unnecessary, as the
diagnosis of primary HIV infection was
undisputed and the neutropenia would likely be
transient. Anti-retroviral therapy (ARV) was not
initiated. Over the following 10 days his
haematological parameters rapidly improved and
all white cell lines normalised. Table 1 shows
serial monitoring of his WCC during admission.
He was restarted on azathioprine successfully 3
months after seroconversion and his neutrophil
count remains normal. He is currently attending
both the IBD and HIV clinics on a regular basis
and his CD remains in clinical and endoscopic
remission.
Making the diagnosis of primary HIV infection is
imperative as it represents a period of extremely
high levels of viremia and genital shedding of the
virus. Individual in this phase have a 10-fold
increased risk of transmission, which will be
reduced if a timely diagnosis is made [10,11].
However this remains a challenge in clinical
practice. In one cohort of 46 patients with primary
HIV infection, 85% sought medical attention but
only 25% received the correct diagnosis. In
another study, primary HIV infection was missed
in 48% of patients at first presentation,
suggesting a low index of suspicion [12,13,14].
How best to manage acute HIV infection remains
unclear although some studies suggest benefit of
early ARV treatment, others show no difference
in outcomes [15]. This supports the decision to
withhold therapy in this case at diagnosis.
3. DISCUSSION
Acute retroviral syndrome as a cause of
neutropenia in CD has not previously been
described .Here we report features of acute seroconversion illness in a patient with long standing
CD on azathioprine.
In primary HIV infection up to 40-90% of patients
will develop acute retroviral syndrome which
usually coincides with high levels of viremia and
the hosts initial immunological response [5].
Symptoms occur 2-6 weeks after exposure and
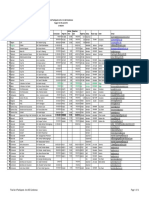
Table 1. Total WBC and differential values on admission
Date
4/12/11
5/12/11
6/12/11
9/12/11
Total WBC
1.87
2.52
3.12
4.77
Neutrophils
0.83
0.6
1.06
2.00
Monocytes
0.14
0.1
0.17
0.24
Lymphocytes
0.6
1.7
1.45
2.16
Eosinophils
0.08
0.1
0.12
0.17
Awuku et al.; BJMMR, 15(5): 1-4, 2016; Article no.BJMMR.26166
4. CONCLUSION
5.
Primary
HIV
infection
may
be
misdiagnosed,hence should be considered an
important differential during work up for
neutropenia in IBD.
6.
CONSENT
7.
Written informed consent was obtained from the
patient for the publication of this case report.
ETHICAL APPROVAL
8.
It is not applicable.
9.
ACKNOWLEDGEMENT
We do acknowledge the contribution of the
infectious disease unit in the management of this
patient.
10.
COMPETING INTERESTS
11.
Authors have
interests exist.
declared
that
no
competing
12.
REFERENCES
1.
mercaptopurine or azathioprine. Am J
Gastroenterol. 2003;98:1058-1063.
Kassutto S, Rosenberg ES. Primary HIV
Type-1 infection. Clin Infect Dis. 2004;
38:1447-53.
Kahn JO, Walker BD. Acute human
immunodeficiency virus type 1 infection
[review]. N Engl J Med. 1998;339:339.
Busch MP, Satten GA. Time course of
viremia and antibody seroconversion
following human immunodeficiency virus
exposure
[review].
Am
J
Med.
1997;102:11724.
MacNeal RJ, Dinulos JGH. Acute retroviral
syndrome. Dermatol Clin. 2006;24:431-8.
Sudarshi D, Pao D, Murphy G, Parry J,
Dean G, Fisher M. Missed opportunities for
diagnosing primary HIV infection. Sex
Transm Infect. 2008;84(1):14-6.
Wawer M, Gray R, Sweankambo N, et al.
Rates of HIV-1 transmission per coital act,
by stage of HIV-1 infection, in Rakai,
Uganda. J Infect Dis. 2005;191:1403
1409.
Hollingsworth T, Anderson R, Fraser C.
HIV-1 transmission, by stage of infection. J
Infect Dis. 2008;198:687693.
Pilcher CD, Eron JJ Jr, Vemazza PL,
Battegay M, Harr T, Yerly S, et al. Sexual
transmission during the incubation period
of primary HIV infection. J Am Med Assoc.
2001;286:17134.
Schacker T, Collier AC, Hughes J, Shea T,
Corey L. Clinical and epidemiologic
features of primary HIV infection. Ann
Intern Med. 1996;125:25764.
(Erratum: Ann Intern Med. 1997;126:174)
Brook MG, Barnes A, Cook GC, Mabey
DCA. Typhus-like illness caused by acute
HIV seroconversion. Postgrad Med J.
1991;67(783):92-3.
Sigall K. Bell, Susan J. Little, Eric S.
Rosenberg 2 clinical management of
acute HIV infection: Best practice
remains
unknown.
J
Infect
Dis.
2010;202(Supplement 2):S278-S288.
DOI: 10.1086/655655
Cooper DA, Gold J, Maclean P, Donovan
B, Finlayson R, Barnes TG, et al. Acute
AIDS retrovirus infection definition of a 13.
clinical
illness
associated
with
seroconversion. Lancet. 1985;1:537-40.
2.
Weintrob AC, Giner J, Menezes P, Patrick
E, Benjamin DK Jr, Lennox J, et al.
Infrequent diagnosis of primary human 14.
immunodeficiency virus infection: Missed
opportunities in acute care setting. Arch
Intern Med. 2003;163:2097-100.
3.
Zon Li, Arkin C, Groopman JE. 15.
Haematologic manifestation of the human
immune deficiency virus(HIV). Br J
Haematol. 1987;66:251.
4.
Dubinsky MC, Feldman EJ, Abreu MT, et
al. Thioguanine: A potential alternate
thiopurine for IBD patients allergic to 6_________________________________________________________________________________
2016 Awuku et al.; This is an Open Access article distributed under the terms of the Creative Commons Attribution License
(http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium,
provided the original work is properly cited.
Peer-review history:
The peer review history for this paper can be accessed here:
http://sciencedomain.org/review-history/14372
4
You might also like
- Nursing Diagnosis Disturbed Sleep PatternDocument8 pagesNursing Diagnosis Disturbed Sleep Patternmaimai324263100% (2)
- Ugib Case StudyDocument33 pagesUgib Case StudyRosemarie Cunanan Grifoni100% (1)
- COPD ExacerbationDocument12 pagesCOPD ExacerbationJeffrey ShermanNo ratings yet
- Cases For Post Prelims Conference 2009-2010Document7 pagesCases For Post Prelims Conference 2009-2010chocoholic potchi100% (1)
- UN Doctors Directory 2015Document18 pagesUN Doctors Directory 2015Kush GuptaNo ratings yet
- Managing IBD: A Case Study on Diagnosis and TreatmentDocument4 pagesManaging IBD: A Case Study on Diagnosis and TreatmentBejan CorinaNo ratings yet
- Hematochezia Case Report on Crohn's Disease in Young MaleDocument3 pagesHematochezia Case Report on Crohn's Disease in Young Maleseptian_tjayaNo ratings yet
- LepsDocument4 pagesLepslynharee100% (1)
- Penyakit Crohn: Laporan Kasus: Paul V. Siwy, Fandy GosalDocument10 pagesPenyakit Crohn: Laporan Kasus: Paul V. Siwy, Fandy GosalyheyenNo ratings yet
- Typhoid Fever: David T Wheeler, MDDocument14 pagesTyphoid Fever: David T Wheeler, MDChandra KushartantoNo ratings yet
- MainDocument3 pagesMainMila KarmilaNo ratings yet
- Life-Threatening Lower Gastrointestinal Hemorrhage in Pediatric Crohn's DiseaseDocument8 pagesLife-Threatening Lower Gastrointestinal Hemorrhage in Pediatric Crohn's DiseasePeregrine Albertus Ricco AzaliNo ratings yet
- Crohn's Disease and TPNDocument13 pagesCrohn's Disease and TPNAira Vida TesoroNo ratings yet
- Intestinal Tuberculosis: A Diagnostic Challenge: Open Access Case DOI: 10.7759/cureus.13058Document4 pagesIntestinal Tuberculosis: A Diagnostic Challenge: Open Access Case DOI: 10.7759/cureus.13058ATIKA INDAH SARINo ratings yet
- Stomach Diseases GuideDocument6 pagesStomach Diseases GuideJames FlanneryNo ratings yet
- Case Report: Streptococcus AnginosusDocument4 pagesCase Report: Streptococcus AnginosusIesanu MaraNo ratings yet
- Case Report: Tuberculosis Liver Abscess in Alcoholism Male PatientDocument4 pagesCase Report: Tuberculosis Liver Abscess in Alcoholism Male PatientWidya Prawirani SiahaanNo ratings yet
- Liver Abscess DissertationDocument4 pagesLiver Abscess DissertationPayForAPaperAtlanta100% (1)
- Pancytopenia Secondary To Bacterial SepsisDocument16 pagesPancytopenia Secondary To Bacterial Sepsisiamralph89No ratings yet
- Pediatric Systemic Lupus Erythematosus Associated With AutoimmuneDocument9 pagesPediatric Systemic Lupus Erythematosus Associated With AutoimmunegistaluvikaNo ratings yet
- Hiding in The Water: Clinical Problem-SolvingDocument6 pagesHiding in The Water: Clinical Problem-SolvingtabareeNo ratings yet
- Hematemesis Melena Due To Helicobacter Pylori Infection in Duodenal Ulcer: A Case Report and Literature ReviewDocument6 pagesHematemesis Melena Due To Helicobacter Pylori Infection in Duodenal Ulcer: A Case Report and Literature ReviewodiNo ratings yet
- Keracunan SianidaDocument8 pagesKeracunan Sianidaclarestatio8No ratings yet
- 54 Shivraj EtalDocument3 pages54 Shivraj EtaleditorijmrhsNo ratings yet
- Case 013: Fever in A Cirrhotic PatientDocument5 pagesCase 013: Fever in A Cirrhotic PatientFitri 1997No ratings yet
- Delay in Diagnosis of Extra-Pulmonary Tuberculosis by Its Rare Manifestations: A Case ReportDocument5 pagesDelay in Diagnosis of Extra-Pulmonary Tuberculosis by Its Rare Manifestations: A Case ReportSneeze LouderNo ratings yet
- Development of type I gastric carcinoid in chronic atrophic gastritis patientsDocument9 pagesDevelopment of type I gastric carcinoid in chronic atrophic gastritis patientsAbristaSeptikasariNo ratings yet
- 2013 URINARY TRACT SUMMER REVIEWDocument12 pages2013 URINARY TRACT SUMMER REVIEWJessica MooreNo ratings yet
- 4th Year Write Up 2 - Int. MedDocument11 pages4th Year Write Up 2 - Int. MedLoges TobyNo ratings yet
- Acute Jejunoileal Obstruction Due To A Pseudopolyp in A Child With Undiagnosed Crohn S DiseaseDocument4 pagesAcute Jejunoileal Obstruction Due To A Pseudopolyp in A Child With Undiagnosed Crohn S Diseasebingl_073No ratings yet
- 2019 Article 1205Document6 pages2019 Article 1205zahra h f aNo ratings yet
- Ajol File Journals - 76 - Articles - 114038 - Submission - Proof - 114038 901 318286 1 10 20150309Document2 pagesAjol File Journals - 76 - Articles - 114038 - Submission - Proof - 114038 901 318286 1 10 20150309alysNo ratings yet
- A 31-Year-Old Man With Chronic Cough and HemoptysisDocument6 pagesA 31-Year-Old Man With Chronic Cough and HemoptysiscocomilkNo ratings yet
- A Girl With Ulcerative Colitis in A Tertiary Care Hospital-A Case ReportDocument4 pagesA Girl With Ulcerative Colitis in A Tertiary Care Hospital-A Case ReportAbdullah KhanNo ratings yet
- A Girl With Ulcerative Colitis in A Tertiary Care Hospital-A Case ReportDocument4 pagesA Girl With Ulcerative Colitis in A Tertiary Care Hospital-A Case ReportWyn AgustinNo ratings yet
- Me219 - Haemato CaDocument21 pagesMe219 - Haemato CaAbby LiewNo ratings yet
- Tuberculosis and Chronic Renal FailureDocument38 pagesTuberculosis and Chronic Renal FailureGopal ChawlaNo ratings yet
- 45-Year-Old Man With Shortness of Breath, Cough, and Fever DiagnosisDocument7 pages45-Year-Old Man With Shortness of Breath, Cough, and Fever DiagnosisFluffyyy BabyyyNo ratings yet
- Acalculous Cholecystitis Prevalence On Abdominal Ultrasonography Examination of HIV/HCV Co-Infection Patients in Cipto Mangunkusumo HospitalDocument3 pagesAcalculous Cholecystitis Prevalence On Abdominal Ultrasonography Examination of HIV/HCV Co-Infection Patients in Cipto Mangunkusumo HospitalDiga AlbrianNo ratings yet
- Clin Infect Dis. 2002 Podnos 62 8Document7 pagesClin Infect Dis. 2002 Podnos 62 8nurhasmaryaniNo ratings yet
- Silvajunior 2016Document3 pagesSilvajunior 2016AmatystNo ratings yet
- Literature Review of Chronic Liver DiseaseDocument6 pagesLiterature Review of Chronic Liver Diseaseafmzodjhpxembt100% (1)
- 1471 230X 12 174 PDFDocument5 pages1471 230X 12 174 PDFAila HinlogNo ratings yet
- Crim Em2013-948071Document2 pagesCrim Em2013-948071m.fahimsharifiNo ratings yet
- Background: Ormdl3 and of GSDMB Were Significantly Increased in Hrv-Stimulated PBMCSDocument6 pagesBackground: Ormdl3 and of GSDMB Were Significantly Increased in Hrv-Stimulated PBMCSSav GaNo ratings yet
- Tuberculosis in Liver Cirrhosis: Rajesh Upadhyay, Aesha SinghDocument3 pagesTuberculosis in Liver Cirrhosis: Rajesh Upadhyay, Aesha SinghAnastasia Lilian SuryajayaNo ratings yet
- Indeterminate ColitisDocument26 pagesIndeterminate ColitisMarlisa YanuartiNo ratings yet
- Case Report: Reynolds SyndromeDocument2 pagesCase Report: Reynolds SyndromePeertechz Publications Inc.No ratings yet
- 0630 - Saturday - SEEK - GrossmanDocument101 pages0630 - Saturday - SEEK - Grossmantechang1No ratings yet
- BMC Dermatology: Schönlein-Henoch Purpura During Pregnancy With Successful Outcome For Mother and NewbornDocument5 pagesBMC Dermatology: Schönlein-Henoch Purpura During Pregnancy With Successful Outcome For Mother and NewbornteguhNo ratings yet
- Case Report Hepato FinalDocument29 pagesCase Report Hepato FinalBangkit PutrawanNo ratings yet
- NewpudpaperDocument15 pagesNewpudpaperapi-2868560640% (1)
- Tuberculous Pleural Effusion Case Study and Literature ReviewDocument3 pagesTuberculous Pleural Effusion Case Study and Literature ReviewtiaanastaNo ratings yet
- The Primary Patient Assessment Form Date Patient Nationality Chief Complaint HPIDocument6 pagesThe Primary Patient Assessment Form Date Patient Nationality Chief Complaint HPIViviaNo ratings yet
- Caso Clinico - AdenocarcinomaDocument1 pageCaso Clinico - AdenocarcinomaXana SoaresNo ratings yet
- Approach For Diagnostic and Treatment of Chronic Diarrhea Caused by Hookworm InfectionDocument7 pagesApproach For Diagnostic and Treatment of Chronic Diarrhea Caused by Hookworm InfectionRianda AkmalNo ratings yet
- Grand Round Presentation on Intestinal TuberculosisDocument40 pagesGrand Round Presentation on Intestinal TuberculosisneptorNo ratings yet
- Case Report and Literature Review On Good's Syndrome, A Form of Acquired Immunodeficiency Associated With ThymomasDocument7 pagesCase Report and Literature Review On Good's Syndrome, A Form of Acquired Immunodeficiency Associated With ThymomasMudassar SattarNo ratings yet
- Non-Traumatic Rupture of Spleen Can Splenectomy BeDocument3 pagesNon-Traumatic Rupture of Spleen Can Splenectomy Beysh_girlNo ratings yet
- Fast Facts: Inflammatory Bowel Disease: Translating the science into compassionate IBD careFrom EverandFast Facts: Inflammatory Bowel Disease: Translating the science into compassionate IBD careNo ratings yet
- Price List Artemis Hospital (In Inr) : CardiologyDocument5 pagesPrice List Artemis Hospital (In Inr) : CardiologyKush GuptaNo ratings yet
- CGHS RatesDocument41 pagesCGHS RatesNagesh RaoNo ratings yet
- Laying Marble AreaDocument2 pagesLaying Marble AreaKush GuptaNo ratings yet
- Laying Marble AreaDocument2 pagesLaying Marble AreaKush GuptaNo ratings yet
- Good Health Plays A Major Role in Achieving The Goals.: Test Regularly. Stay Healthy. Keep SucceedingDocument1 pageGood Health Plays A Major Role in Achieving The Goals.: Test Regularly. Stay Healthy. Keep SucceedingKush GuptaNo ratings yet
- Russian EmbassyDocument14 pagesRussian EmbassyKush GuptaNo ratings yet
- Delhi Uni PDFDocument1 pageDelhi Uni PDFKush GuptaNo ratings yet
- Acrylic BookDocument122 pagesAcrylic BookSonia CireaşăNo ratings yet
- Delhi Uni1Document1 pageDelhi Uni1Kush GuptaNo ratings yet
- Wipro BpoDocument10 pagesWipro BpoKush GuptaNo ratings yet
- AIO-publication-40-eng-Final List PDFDocument14 pagesAIO-publication-40-eng-Final List PDFKush GuptaNo ratings yet
- Tor-Sow For Lab For Cnns Draft Dated 9 OctDocument13 pagesTor-Sow For Lab For Cnns Draft Dated 9 OctKush GuptaNo ratings yet
- Ilae IbrocourseprogramfinalDocument5 pagesIlae IbrocourseprogramfinalKush GuptaNo ratings yet
- Dr Lal Pathlabs Invoice #C000662672Document3 pagesDr Lal Pathlabs Invoice #C000662672Kush GuptaNo ratings yet
- Delhi Pathology PanelsDocument1 pageDelhi Pathology PanelsKush GuptaNo ratings yet
- Detail of CFOsDocument4 pagesDetail of CFOsKush Gupta0% (2)
- Delhi UniDocument1 pageDelhi UniKush GuptaNo ratings yet
- Call ReportDocument15 pagesCall ReportKush GuptaNo ratings yet
- Detail of CFOsDocument4 pagesDetail of CFOsKush Gupta0% (2)
- D7C-C2 (Draft CAR Cabin Crew Medical)Document6 pagesD7C-C2 (Draft CAR Cabin Crew Medical)Kush GuptaNo ratings yet
- CGHS Treatment Procedure/Investigation List (New ListDocument3 pagesCGHS Treatment Procedure/Investigation List (New ListKush GuptaNo ratings yet
- Action Plan Corporate - JuneDocument1 pageAction Plan Corporate - JuneKush GuptaNo ratings yet
- Companies Contact Details Amp HR Name 1Document53 pagesCompanies Contact Details Amp HR Name 1srinathssmNo ratings yet
- Action Plan Corporate - JuneDocument1 pageAction Plan Corporate - JuneKush GuptaNo ratings yet
- LocationsDocument1 pageLocationsKush GuptaNo ratings yet
- IPM - Fresh ListDocument15 pagesIPM - Fresh ListKush GuptaNo ratings yet
- DetailDocument2 pagesDetailKush GuptaNo ratings yet
- The Marfan SyndromeDocument6 pagesThe Marfan SyndromeKush GuptaNo ratings yet
- Schonert-Reichl-Educating The Heart As Well As The MindDocument7 pagesSchonert-Reichl-Educating The Heart As Well As The MindnewoldnoneNo ratings yet
- Makna MsiaDocument19 pagesMakna Msiadivaglrboy9023No ratings yet
- Skills - Care of The Pregnant Patient ComputationsDocument5 pagesSkills - Care of The Pregnant Patient ComputationsMichelle HutamaresNo ratings yet
- Agriculture, biotech, bioethics challenges of globalized food systemsDocument28 pagesAgriculture, biotech, bioethics challenges of globalized food systemsperoooNo ratings yet
- Back From The Bluez - 09 - Self ManagementDocument5 pagesBack From The Bluez - 09 - Self ManagementMelanie DovaleNo ratings yet
- 1a - Hernandez - Research PaperDocument28 pages1a - Hernandez - Research PaperEdgar TorresNo ratings yet
- Tanzania STG 052013-Copy 1544379670122Document220 pagesTanzania STG 052013-Copy 1544379670122Waqar WikiNo ratings yet
- Being Single Vs Being MarriedDocument34 pagesBeing Single Vs Being MarriedPeter MissoleNo ratings yet
- Factors Affecting Adherence to Intranasal CorticosteroidsDocument20 pagesFactors Affecting Adherence to Intranasal CorticosteroidsKathrinna Feliz AlertaNo ratings yet
- RCH DEM Head Injury GuidelinesDocument4 pagesRCH DEM Head Injury GuidelinesJerry LeeNo ratings yet
- Principles of Case Planning in Social Work PracticeDocument4 pagesPrinciples of Case Planning in Social Work PracticeJane GilgunNo ratings yet
- Senior High School: Rizal St. Guimbal, IloiloDocument73 pagesSenior High School: Rizal St. Guimbal, IloiloLizbeth Mari MoqueraNo ratings yet
- MIT Medical Department Pediatrics History Form: AppointmentDocument4 pagesMIT Medical Department Pediatrics History Form: Appointmentmaddythedoc100% (1)
- CBT Flashcard Therapy for Schizophrenia PatientsDocument9 pagesCBT Flashcard Therapy for Schizophrenia PatientsMuhammadAjiWicaksonoNo ratings yet
- Lesson 3: Health Information System How Do Health Information Systems Look Like and What Architectures Are Appropriate?Document13 pagesLesson 3: Health Information System How Do Health Information Systems Look Like and What Architectures Are Appropriate?ajengwedaNo ratings yet
- Common Cause or Etiology of Pott's DiseaseDocument5 pagesCommon Cause or Etiology of Pott's DiseaseStan Aves GarciaNo ratings yet
- Assessment of Functional Pain Score by Comparing To Traditional Pain ScoresDocument7 pagesAssessment of Functional Pain Score by Comparing To Traditional Pain ScoresKepompong KupukupuNo ratings yet
- Framework Nurafni SuidDocument2 pagesFramework Nurafni SuidapninoyNo ratings yet
- Cancer Help & Research Trust: Donation AppealDocument1 pageCancer Help & Research Trust: Donation AppealshahrukhsrsNo ratings yet
- Nursing Care Plan: Chronic Pain and COPDDocument11 pagesNursing Care Plan: Chronic Pain and COPDneuronurse100% (1)
- Life Esidimeni Fact SheetDocument4 pagesLife Esidimeni Fact SheetPrimedia Broadcasting100% (2)
- Full Download Ebook Ebook PDF Nelson Essentials of Pediatrics 8th Edition PDFDocument41 pagesFull Download Ebook Ebook PDF Nelson Essentials of Pediatrics 8th Edition PDFdavid.anderson198100% (37)
- Neo JaundiceDocument67 pagesNeo Jaundicemanisha thakur100% (1)
- Efolio 404Document7 pagesEfolio 404api-377789171No ratings yet
- Psychological Disorders Chapter OutlineDocument13 pagesPsychological Disorders Chapter OutlineCameron PhillipsNo ratings yet
- AHA Activity Hazard AnalysisDocument24 pagesAHA Activity Hazard AnalysisElvyn Fabellore HerreraNo ratings yet
- The So Called Oedematous Skin DiseaseDocument22 pagesThe So Called Oedematous Skin Diseaseمحمد على أحمد أحمدNo ratings yet
- Health Benefits of Vitamin CDocument5 pagesHealth Benefits of Vitamin CZackNo ratings yet
- A Meningioma Is ADocument20 pagesA Meningioma Is ASherry KingNo ratings yet