Professional Documents
Culture Documents
Approach To The Adult With Epistaxis
Uploaded by
TP RMadOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Approach To The Adult With Epistaxis
Uploaded by
TP RMadCopyright:
Available Formats
Approach to the adult with epistaxis
21/09/2016, 6:41 PM
Official reprint from UpToDate
www.uptodate.com 2016 UpToDate
Approach to the adult with epistaxis
Author
Harrison Alter, MD, MS, FACEP
Section Editors
Allan B Wolfson, MD
Daniel G Deschler, MD, FACS
Deputy Editor
Jonathan Grayzel, MD, FAAEM
All topics are updated as new evidence becomes available and our peer review process is complete.
Literature review current through: Aug 2016. | This topic last updated: Feb 02, 2016.
INTRODUCTION Epistaxis is a common problem, occurring in up to 60 percent of the general population [1]. While
most episodes are uncomplicated, epistaxis can occasionally be difficult to control. Knowledge of the basic anatomy of
the nasopharynx and a few hemostatic strategies are reassuring in the face of acute hemorrhage.
This topic addresses epistaxis in adults. Epistaxis in children is discussed separately. (See "Evaluation of epistaxis in
children" and "Management of epistaxis in children".)
EPIDEMIOLOGY Survey data suggest that although 60 percent of adults experience an epistaxis episode, only 10
percent or fewer seek medical attention [2,3]. Epistaxis is a common otolaryngologic cause for hospital admission,
although surgical intervention is rarely needed [4].
Epistaxis appears to have a bimodal age distribution, with most cases occurring before age 10 or between 45 and 65
years of age [1,5]. Hospital admission for epistaxis increases progressively with age, but these data often do not control
for aspirin or anticoagulant use [6]. Among hospitalized patients, there is male predominance prior to age 49, after which
the sex distribution equalizes. This phenomenon has been attributed to a protective effect of estrogen in women,
whether in fostering a healthy nasal mucosa or in preventing vascular disease more generally [6-8].
Seasonal variation, with predominance in winter months, has been found in most [9-13] but not all [14], studies.
Seasonal factors affecting epistaxis include the incidence of upper respiratory infections, allergic rhinitis, and mucosal
changes associated with fluctuations in temperature and humidity.
ANATOMY Epistaxis may be classified as anterior or posterior, depending upon the source of bleeding.
Anterior bleeds Anterior nosebleeds are by far the most common [15]. A large proportion is self-limited and can be
managed definitively in the primary care setting.
Up to 90 percent occur within the vascular watershed area of the nasal septum known as Kiesselbach's plexus (figure 1)
[16]. Anastomosis of three primary vessels occurs in this area: the septal branch of the anterior ethmoidal artery; the
lateral nasal branch of the sphenopalatine artery; and the septal branch of the superior labial branch of the facial artery.
The sphenopalatine artery also gives off branches supplying the posterolateral wall and posterior choana; these vessels
are the most likely source of posterior nosebleeds.
Posterior bleeds Posterior epistaxis arises most commonly from the posterolateral branches of the sphenopalatine
artery but may also arise from the carotid artery (figure 1).
Posterior nosebleeds can result in significant hemorrhage. The skilled clinician may temporize with nasal packing, but
most patients require prompt referral to an emergency department, possible consultation with an otolaryngologist, and
sometimes hospital admission.
ETIOLOGY Anterior nosebleeds often result from mucosal trauma or irritation.
Nose picking is a common cause. The source is usually just proximal to the mucocutaneous junction where there
is little subcutaneous tissue into which an excoriated vessel can retract.
Low moisture content in the ambient air can result in mucosal dryness and irritation. This factor is common in
centrally-heated rooms that are not humidified.
The mucosal hyperemia that accompanies allergic or viral rhinitis makes bleeding from local trauma especially
profuse, which may prompt patients to seek medical care.
The presence of a foreign body should be considered when bleeding is accompanied by purulent discharge;
sinusitis is also in the differential diagnosis in these circumstances.
Chronic excoriation can lead to small septal perforations that may bleed from surrounding friable granulation
https://www.uptodate.com/contents/approach-to-the-adult-with-epistaTerm=epistaxis&selectedTitle=1%7E150&view=print&displayedView=full
Page 1 of 18
Approach to the adult with epistaxis
21/09/2016, 6:41 PM
tissue; chronic intranasal drug use (eg, cocaine) may present similarly.
Patients who suffer facial trauma from a motor vehicle crash or other blunt facial impact often bleed from the nose,
usually from an anterior source.
Anterior and posterior bleeds may be caused by a number of associated conditions:
Anticoagulated patients are at high risk for nosebleeds. The role of warfarin cessation and reversal of
anticoagulation are controversial in the setting of epistaxis. Patients who are in the therapeutic international
normalized ratio (INR) range for their specific indication and in whom hemostasis is achieved may be safely
maintained on their warfarin regimen. (See "Management of warfarin-associated bleeding or supratherapeutic
INR".)
One large retrospective study in an anticoagulation clinic noted that reversal was required for epistaxis at a rate of
only 1.5 per 1000 patient-years [17], despite patient recall data in the same hospital suggesting an annual
incidence of epistaxis of 25 percent among anticoagulated patients [18].
Epistaxis is the most common presenting symptom among patients with hereditary hemorrhagic telangiectasia
(Osler-Weber-Rendu disease) [19]. The bleeding can be quite difficult to control in these individuals. The friable
lesions may appear to bleed more with treatment than without. Nevertheless, the treating clinician should initiate
hemostatic measures and obtain appropriate consultation [19-21]. (See "Hereditary hemorrhagic telangiectasia
(Osler-Weber-Rendu syndrome)".)
Patients with familial blood dyscrasias, particularly platelet disorders, von Willebrand disease, and hemophilia, are
prone to epistaxis. A bleeding diathesis should be considered in the patient with recurrent spontaneous epistaxis.
(See "Approach to the adult patient with a bleeding diathesis".)
Recurrent posterior bleeds or massive hemorrhage may be due to aneurysm of the carotid artery [22]. This is of
particular concern in a patient with a prior history of head and neck surgery, or following trauma (pseudoaneurysm)
[23], but most often posterior bleeds arise spontaneously.
Epistaxis may be a symptom of a nasal neoplasm. The most common tumors associated with epistaxis are
squamous cell carcinoma, adenoid cystic carcinoma, melanoma, and inverted papilloma [16]. Nasopharyngeal
cancers are more common in patients of Chinese or southeast Asian heritage. Patients who have had significant
epistaxis (posterior bleed) should receive a thorough ear, nose, and throat (ENT) evaluation after the bleeding has
been controlled.
The data on the importance of aspirin as a risk factor for epistaxis are not definitive [24]. In one study of habitual
nose bleeders, the recalled rate of aspirin use did not differ from that of controls [25]. In contrast, another case
control study found a positive correlation between aspirin use and epistaxis (relative risk [RR] 2.17 or 2.75,
depending upon whether a community or hospital control group was used) [26]. There is no reported increase in
risk associated with other nonsteroidal antiinflammatory drugs (eg, ibuprofen).
The association between hypertension and epistaxis is uncertain. Multiple studies have related hypertension to
nosebleeds [4,10,27-30], although studies specifically exploring this relationship have been unable to confirm the
association [7,18,31-33]. Some data suggest that longstanding hypertension may contribute to an elevated risk of
epistaxis, most likely due to its vasculopathic effects [32]. Some specialists suggest that hypertension does not
cause epistaxis but does prolong episodes of bleeding [34].
Alcohol may increase the risk for epistaxis [35], as may intranasal preparations for seasonal allergies [36]. Nasal
steroids are used with increasing frequency, and their contribution to the incidence of anterior nosebleeds is likely
to increase. A placebo study of fluticasone nose drops found a significant increase in epistaxis in the treatment
group (19 percent compared with 4 percent for placebo) [37].
One large case-control study explored factors associated with recurrent epistaxis [30]. In addition to known risks
for first-time bleeding, patients with congestive heart failure were noted to be at somewhat higher risk for repeated
episodes of epistaxis.
EVALUATION
Initial assessment The initial evaluation of epistaxis should focus on airway assessment and cardiovascular stability.
Airway intervention, fluid resuscitation, and emergent otolaryngologic consultation can be necessary in severe epistaxis.
Normal appearance, vital signs, and respiratory function are evidence that the examiner can safely attend to the
https://www.uptodate.com/contents/approach-to-the-adult-with-epistaTerm=epistaxis&selectedTitle=1%7E150&view=print&displayedView=full
Page 2 of 18
Approach to the adult with epistaxis
21/09/2016, 6:41 PM
presenting complaint. (See "Basic airway management in adults" and "The decision to intubate".)
History The history should address the following issues [38]:
Conditions that predispose to bleeding, possibly including tumors, coagulation disorders (personal and family
history), recent trauma or surgery, medications (eg, aspirin, warfarin, clopidogrel, intranasal glucocorticoids), and
other conditions (eg, cirrhosis, human immunodeficiency virus [HIV], intranasal cocaine use).
The timing, frequency, and severity of epistaxis should be assessed (eg, is this an isolated episode or one of
many?).
The possible presence of chronic medical problems that can be exacerbated by blood loss, such as coronary
artery disease and chronic obstructive pulmonary disease, and symptoms that may be related (eg, chest
discomfort, dyspnea, lightheadedness).
Coagulation studies and other tests A prothrombin time (PT) with international normalized ratio (INR) is NOT
indicated as a routine test but should be ordered for the anticoagulated patient [39,40]. A hematocrit and type and
crossmatch should be obtained in the setting of massive or prolonged hemorrhage, and two large bore IV lines placed in
such cases.
Initial tamponade Properly instructed patients may achieve hemostasis unassisted while the evaluation gets
underway. The following approach may be helpful:
Patient blows their nose to remove blood and clots.
Clinician sprays the nares with oxymetazoline.
Patient pinches the alae tightly against the septum and holds continuously for 10 minutes (picture 1 and picture 2).
Many otolaryngologists recommend initial treatment with two sprays of oxymetazoline (Afrin) to hasten hemostasis,
although little published data exist to support the practice. One small retrospective study found that oxymetazoline spray
stopped bleeding in 65 percent of patients presenting to an emergency department with epistaxis [41]. The application of
oxymetazoline for the purpose of reducing bleeding through vasoconstriction is unlikely to cause an elevation in blood
pressure.
To achieve tamponade, the patient must exert pressure properly by grasping the alae distally and pinching them tightly
against the septum such that the mucosal surfaces are tightly apposed (picture 1 and picture 2). The patient should
maintain this position continuously for 10 to 15 minutes without releasing pressure to see if the bleeding has stopped.
Other maneuvers include having the patient bend forward at the waist while sitting up (to avoid swallowing blood),
placing a plug of cotton wool or a pledget into the bleeding nostril (sometimes coated with antibiotic ointment),
expectorating blood that accumulates in the pharynx, and applying a cold compress to the bridge of the nose. These
maneuvers should be taught to patients for use at home [18]. The anxious patient may be given a small parenteral dose
of an anxiolytic medication, such as lorazepam.
Another initial measure commonly practiced by otolaryngologists is the acute reduction of elevated blood pressures in
the setting of epistaxis, with the idea that bleeding will not be controlled while systemic pressures remain high [42]. This
practice has not been studied in prospective trials and its validity remains unclear. Furthermore, some patients do not
tolerate acute reductions in blood pressure. For these reasons, we believe that, in the absence of a hypertensive
emergency, antihypertensive medications should NOT be part of initial therapy for epistaxis [43]. (See "Management of
severe asymptomatic hypertension (hypertensive urgencies) in adults".)
Physical examination
General examination It is important to assess the vital signs, mental status, and airway of any patient with
significant bleeding, looking for signs of airway compromise or hypovolemic shock. This assessment is particularly
important in the elderly and those with severe systemic disease. In patients with recurrent nosebleeds, the patient
should be evaluated for signs of coagulopathy (eg, ecchymoses, petechiae, telangiectatic lesions).
Pretreatment The nasal cavity should be anesthetized prior to performing a detailed examination, which
otherwise is uncomfortable. Adequate anesthesia can often be achieved with cotton swabs soaked in an anesthetic and
vasoconstrictive agent. Drugs commonly used for this purpose include 2 percent lidocaine, lidocaine with epinephrine,
and 4 percent cocaine. These agents have not been studied in primary epistaxis, but a small literature on the prevention
of epistaxis in nasotracheal intubation suggests that they are roughly equivalent [44].
The selected medication may be applied using two saturated cotton swabs, one placed directly posteriorly and another
https://www.uptodate.com/contents/approach-to-the-adult-with-epistaTerm=epistaxis&selectedTitle=1%7E150&view=print&displayedView=full
Page 3 of 18
Approach to the adult with epistaxis
21/09/2016, 6:41 PM
posterosuperiorly, or with saturated cotton pledgets hand rolled from cotton wool and placed in the nose with bayonet
forceps.
Oxymetazoline nasal preparation, although it has no anesthetic properties, can provide vasoconstriction. It is
administered as two sprays. Oxymetazoline is readily available, convenient, and inexpensive. Topical phenylephrine is
NOT recommended following reports of several deaths associated with its use intraoperatively [45].
Examination of the nose It is important to obtain as clear and complete a view of the nares as possible. Ideally,
the patient should be examined in a dental chair or its equivalent. If this is unavailable, bring the head of an examination
table to upright so the patient can sit comfortably while head movement is restricted. Good lighting is essential,
preferably with a headlamp or mirror. Use an emesis basin to catch blood and expectorated clots. Encourage the patient
to spit posterior pharyngeal blood into the basin as this will reduce the risk of emesis and aspiration.
An adequate examination for the source of bleeding requires use of a nasal speculum; an otoscope speculum is
significantly less effective [38,46]. When inserted, the nasal speculum is oriented so one blade moves superiorly and the
other moves inferiorly.
Further techniques to optimize use of the nasal speculum are based upon anecdote. The clinician can stabilize the
speculum's position by placing his or her index finger on the bridge of the patient's nose. Alternatively, the clinician can
use the index finger to press the nasal alae against the superior blade of the speculum, once it is inserted. This allows
only the lower blade to move and may reduce patient discomfort.
Ask the patient to look directly ahead and attempt the sniffing position. Patients often try to tilt the head back to facilitate
a nasal examination, but the nasopharynx lies in the anteroposterior plane and extension of the neck will obscure most
of the cavity from view [38].
Clots may be cleared either with suction or by asking the patient to gently blow his or her nose. The most common
suction setup, the Yankauer tip, is poorly suited to the nares, and the surgeon's Zoellner sucker is often too small. Some
clinicians have found a disposable tube connector or a Frazier suction catheter to be helpful [47].
Inspect the area of Kiesselbach's plexus first since the majority of bleeds originate here (figure 1). Look closely for
bleeding, ulceration, or erosion. It is sometimes helpful to displace coagulum gently with a cotton swab to identify a
bleeding source. Also inspect the nasal vestibule, septum, and turbinates for sources of bleeding.
Not uncommonly, a primary bleeding site cannot be identified. In such cases, bleeding may stem from a posterior
source, including a mass that is difficult to identify, or a trivial insult to the nasal mucosa that has resolved spontaneously
or following noninvasive treatment.
Distinguishing anterior and posterior bleeds It can sometimes be difficult to determine the source of epistaxis.
Neither the volume nor the rate of bleeding is helpful; anterior bleeding can be brisk. However, minor bleeding is unlikely
to originate posteriorly. While pinching the alae stops many but not all anterior bleeds, many posterior bleeds stop
spontaneously making interpretation difficult. Perhaps the best way to determine the bleeding source in difficult cases is
to place bilateral anterior nasal packing and examine the patient. Brisk bleeding despite proper packing strongly
suggests a posterior source.
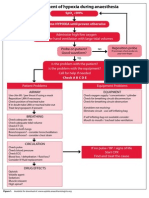
TREATMENT OF ANTERIOR BLEEDING The treatment of anterior epistaxis proceeds in a stepwise fashion until
hemostasis is achieved. The attached flowchart presents a general approach to adult patients with epistaxis (algorithm
1). A list of the equipment that may be needed for epistaxis management is provided (table 1).
Bleeding stops with conservative measures Sometimes minor anterior nosebleeds resolve without intervention
prior to clinical evaluation or with the initial attempt at tamponade described above. If no anterior source is evident and
bleeding has stopped, the nose should be packed only if bleeding recurs rapidly [38]. (See 'Initial tamponade' above.)
It is reasonable to observe the patient for approximately 30 minutes for recurrent bleeding. Such patients should be
discharged with antibiotic ointment to coat the mucosa, applied with a fingertip or cotton swab three times daily for three
days.
The natural history of nosebleeds that resolve spontaneously is not well-described. Among younger patients, it appears
that rebleeding rates are relatively low (approximately one in three or four cases) [48]. Given the discomfort of packing
and the effectiveness of conservative measures in most cases, it is reasonable for patients without recurrence to forego
packing.
Cautery If an anterior bleeding source is visualized, first-line treatment consists of chemical or electrical cautery.
https://www.uptodate.com/contents/approach-to-the-adult-with-epistaTerm=epistaxis&selectedTitle=1%7E150&view=print&displayedView=full
Page 4 of 18
Approach to the adult with epistaxis
21/09/2016, 6:41 PM
Chemical cautery is usually performed with silver nitrate sticks, which are used in the following manner. After
determining that topical anesthesia is adequate, apply the applicator tip to a small area surrounding the bleeding site.
Begin at the periphery of this small area and move towards the center, starting proximally. Avoid cauterizing large areas
and remove excess silver nitrate with a cotton swab [38,46].
Cautery is applied for a few seconds (no longer than 10 seconds), until a white precipitate forms. Both types of cautery
may cause rhinorrhea and crusting. Avoid overzealous cautery of the septum, which can lead to ulceration and
perforation. Rarely, if ever, should both sides of the septum be cauterized in the same session in order to avoid tissue
necrosis [1].
Though silver nitrate requires moisture to act, it will work only on a relatively bloodless surface; the bleeding point itself
cannot be cauterized until hemostasis is achieved either through proximal cautery, vasoconstrictive agents such as
oxymetazoline drops, or tamponade from manual pressure. (See 'Initial tamponade' above.)
Suction may be used to dry areas with minor bleeding. Electrical cautery works equally well [49] but is also not effective
on bloody surfaces. Cautery can be extremely painful if the patient is inadequately anesthetized. Assuming hemostasis
is achieved with cautery, these patients should apply antibiotic ointment with a fingertip or cotton swab three times daily
for three days.
Nasal packing If cautery is unsuccessful, the next step in the management of suspected anterior epistaxis is nasal
packing to tamponade local bleeding. Several packing options are available (picture 3). Before nasal packing is placed,
the anxious patient may be given a small parenteral dose of an anxiolytic medication, such as lorazepam.
Nasal tampons Nasal packing is most easily accomplished with a nasal tampon. These are usually made of
Merocel, a synthetic open-cell foam polymer that appears to provide a less hospitable medium for Staphylococcus
aureus (S. aureus) than traditional gauze packing [50]. (See 'Antibiotics and toxic shock syndrome' below.)
The Merocel tampon is easy to use and effective. It is inserted as follows:
Position the patient properly and pretreat with a topical anesthetic (eg, 2 percent lidocaine) and topical
vasoconstrictor (eg, oxymetazoline). Proper patient positioning and pretreatment are discussed above. (See
'Physical examination' above.)
Coat the tampon with bacitracin ointment to facilitate placement, and possibly decrease the risk of toxic-shock
syndrome.
Insert the tampon by sliding it directly along the floor of the nasal cavity until nearly the entire tampon lies within the
nasal cavity.
Large nares can be packed with two tampons (be sure to leave the tips of both exposed for removal); small nares
can be packed with a pediatric tampon or an adult tampon trimmed with an iris scissor.
Expand the tampon by infusing approximately 10 mL of saline, or bacitracin solution if available. A 22-gauge
angiocatheter on a saline-filled syringe can be used to expand the deep portion of the tampon first and to speed
diffusion.
Gauze packing Nasal packing can be achieved using ribbon gauze, which is dispensed in 180 cm (72 inches)
lengths, though this approach requires greater skill. The gauze is impregnated with petrolatum (eg, Xeroform) or bismuth
subnitrate and iodoform paste (BIPP). The procedure involves stacking layers of gauze in an accordion fashion, starting
on the floor of the nasal cavity.
To insert the packing, grasp the gauze with a bayonet forceps, leaving an approximately 10 cm (4 inches) tail [16]. Next,
gingerly advance the gauze as far as possible into the nasal cavity without touching the walls of the nasopharynx. Then,
grasp another 8 to 10 cm of gauze and advance it atop the prior layer. Repeat this process until the nose is tightly
packed.
One small randomized trial found no difference between the Merocel tampon and BIPP-impregnated gauze packing
(similar to Xeroform) in controlling epistaxis [51].
Nasal balloon catheters Overall, balloon catheters are easier to use than gauze packing, particularly for
clinicians with little experience performing packing. However, the techniques are probably equally effective. Both
procedures are uncomfortable and may require the use of parenteral opioids or anxiolytics.
Several balloon-style products are available to tamponade anterior, and posterior, nosebleeds. The Epistat and Storz T-
https://www.uptodate.com/contents/approach-to-the-adult-with-epistaTerm=epistaxis&selectedTitle=1%7E150&view=print&displayedView=full
Page 5 of 18
Approach to the adult with epistaxis
21/09/2016, 6:41 PM
3100 balloons have a lumen that allows for oxygen delivery and both anterior and posterior balloons. (See 'Treatment of
posterior bleeding' below.)
The Rapid Rhino is a balloon catheter with a large, low-pressure air balloon encased in a carboxymethylated cellulose
(CMC) mesh, available in a 5 cm length for anterior bleeds and 7.5 cm for posterior epistaxis. The Rapid Rhino becomes
slick when it is placed in water for 30 seconds, making placement easier. Upon contact with blood, the CMC fibers act to
promote thrombosis.
The Rapid Rhino is inserted as follows [52]:
Position the patient properly and pretreat with a topical anesthetic (eg, 2 percent lidocaine) and topical
vasoconstrictor (eg, oxymetazoline). Proper patient positioning and pretreatment are discussed above. (See
'Physical examination' above.)
Soak the catheter in sterile water for 30 seconds. Do NOT use saline and do NOT apply lubricants or topical
antibiotics, which impair the CMC fibers.
Insert the catheter by sliding it along the floor of the nasal cavity until the plastic proximal fabric ring lies within the
nares.
Inflate the catheter with air only using a 20 mL syringe; stop inflating when the pilot cuff is round and firm. The
appropriate amount of air varies with the size of the nasal cavity.
After 10 to 15 minutes, reassess the pilot cuff. Add air if it is no longer round and firm. Tape the pilot cuff to the
patient's cheek.
The results of two small, randomized trials and observational data suggest there is no difference between a nasal
tampon and the Rapid Rhino balloon catheter in controlling epistaxis, but note that the Rapid Rhino appears to cause
less discomfort and is easier to insert [53-55]. No significant differences in rebleeding after removal of the devices were
reported.
Thrombogenic foams and gels Gel and foam products that promote thrombogenesis are being developed and
tested for treatment of epistaxis. Quixil, a fibrin glue, is safe, and probably as effective as cautery and packing [56].
Floseal, a bovine-derived thrombin gel, was associated with an absolute 26 percent lower rebleeding rate compared with
nasal packing and was easier to insert and judged more satisfactory by both providers and patients in a randomized trial
of 70 patients with acute anterior nosebleeds [57]. In another prospective study, FloSeal effectively controlled posterior
bleeds in 8 of 10 patients whose initial hemostatic packing failed [58].
Surgicel, Gelfoam, and Avitene, all common conformable hemostatic materials, have each been described in reviews or
small case series as useful in nasal bleeding refractory to cautery [14,34]. These materials can be trimmed to an
appropriate size using an iris scissor and then applied directly to the bleeding source with a bayonet forceps. Once
applied, the material should be held in place with firm pressure for approximately one minute to ensure adherence.
Two reports have evaluated the use of tranexamic acid (TXA) for epistaxis. One small randomized trial involving TXA gel
found no effect [59]. A subsequent randomized trial of 216 patients reported that topical TXA caused cessation of
bleeding in 71 percent of patient within 10 minutes [60]. However, the trial is limited by a substandard comparator (cotton
pledgets soaked in tetracycline). Anecdotally, we have used a Merocel tampon saturated with the 500 mg of the IV
formulation of TXA in refractory cases to good effect. Such interventions should be undertaken with caution in patients in
whom the potential dangers of systemic thrombosis are high (eg, known coronary or cerebrovascular disease), as the
systemic absorption of TXA through the nose is not well characterized.
Persistent bleeding If bleeding persists despite the initial packing, the contralateral naris may be packed, thereby
providing a counterforce to promote tamponade. Some clinicians obtain otolaryngologic consultation once bilateral
packing is needed, although the risk of aspiration, hypoxic complications, and treatment failure is small in this setting
[51,61]. In most cases, 24 to 48 hour follow-up with the consultant is adequate.
Nasal packing in anterior bleeding has about a 90 to 95 percent success rate [51,61]. If bilateral anterior packing fails to
produce hemostasis, the odds of a posterior source increase greatly. Patients with posterior bleeds need posterior
packing and probably hospitalization. (See 'Treatment of posterior bleeding' below.)
As mentioned above, patients with hereditary hemorrhagic telangiectasia can have severe recurrent epistaxis that is
resistant to usual management measures. A report of one such case found that application of five drops (about 0.25 mL)
of 100 mg/mL tranexamic acid (an antifibrinolytic agent) at the onset of bleeding reduced the need for blood transfusions
https://www.uptodate.com/contents/approach-to-the-adult-with-epistaTerm=epistaxis&selectedTitle=1%7E150&view=print&displayedView=full
Page 6 of 18
Approach to the adult with epistaxis
21/09/2016, 6:41 PM
and iron supplements [62]. (See "Hereditary hemorrhagic telangiectasia (Osler-Weber-Rendu syndrome)", section on
'Epistaxis'.)
Antibiotics and toxic shock syndrome The incidence of toxic shock syndrome (TSS) following postoperative nasal
packing is estimated at about 16 per 100,000 packings. Although the incidence in primary nasal packing has not been
established, it is prudent for clinicians and patients to be alert for signs of toxic shock syndrome (fever, hypotension,
desquamation, and mucosal hyperemia). (See "Staphylococcal toxic shock syndrome".)
Systemic antibiotics appear to be of little use in reducing nasal carriage of Staphylococcus aureus (S. aureus)
[50,63,64]. There are no studies that have directly examined the effect of systemic antibiotics on rates of TSS since it is
such a rare event. In addition to the lack of proven efficacy of antibiotics, significant adverse outcomes might occur more
commonly than TSS if antibiotics were given routinely. Such outcomes include allergic reactions and the development of
bacterial strains with resistance to antibiotics.
Use of antibiotics has also been suggested for prevention of secondary bacterial sinus infections, but again, there are no
studies to support this approach. One small prospective study of patients treated with anterior nasal packing for epistaxis
found no evidence of infection [65].
Nevertheless, despite the lack of proven efficacy, many ear, nose, and throat (ENT) specialists prefer to provide
prophylaxis against TSS and antibiotics are commonly prescribed in patients with nasal packing for the duration of the
packing [51,54,57,61,66-68]. We prefer to avoid giving antibiotics and believe they should not be given routinely for
prophylaxis against infection in patients with anterior nasal packing. The decision to prescribe antibiotics is appropriately
individualized to the patient. It may be reasonable to treat patients at greater risk of infection, such as those with
diabetes, advanced age, or immunosuppression.
If prescribed, an antibiotic with staphylococcal coverage should be selected, such as amoxicillin-clavulanate or a
second-generation cephalosporin; topical mupirocin may also be used [66].
Follow-up If vital signs and respiratory function remain normal after packing, the patient may be safely referred for
specialist follow-up in 24 to 48 hours, with advice to present to an emergency department sooner if bleeding recurs.
Some clinicians opt for urgent otolaryngologic consultation once acute anterior epistaxis has progressed to the point of
needing bilateral packing, although the risk of aspiration, hypoxic complications, and treatment failure is small in this
setting [51,61]. In most cases, 24 to 48 hour follow-up is adequate.
After 24 to 48 hours, a more thorough examination may be possible, although tumors or other abnormalities that may
have been missed in the acute setting are seldom found. Nasal packing, particularly Merocel, should be rehydrated with
saline drops prior to removal for patient comfort.
Specialty referral may not be necessary for healthy patients with stable vital signs and uncomplicated bleeding from a
clearly identified source that resolves with simple cautery or one-time packing. Such patients should be reassessed
when the packing is removed at 48 hours. Referral to an otolaryngologist is warranted in patients who do not meet ALL
of these criteria, or about whom the clinician has questions or concerns.
Prevention Patients with uncomplicated anterior bleeds should be advised to sleep in a humidified environment.
Although proof of efficacy is not available [69], a topical antibacterial (eg, mupirocin) or bacteriostatic (eg, bacitracin)
ointment may be gently applied to the nasal mucosa with a cotton-tipped swab in an attempt to prevent recurrence.
Directing nasal medication sprays away from the septum may decrease the risk of epistaxis.
TREATMENT OF POSTERIOR BLEEDING The acute management of a posterior nosebleed differs from that of an
anterior bleed, although it is also based upon the principle of tamponade. Of the several methods of posterior packing
described, we prefer balloon catheters. If balloon catheters are not available, alternatives include a Foley catheter and
cotton packing.
A list of the equipment that may be needed for epistaxis management is provided (table 1). Immediate otolaryngologic
consultation is necessary if bleeding is heavy and cannot be controlled with posterior packing.
Balloon catheters Balloon catheters were developed to simplify posterior nasal packing. Examples include the
Epistat and Storz T-3100. One model of the balloon catheter combines a small posterior balloon and a large anterior
balloon. Such double balloon catheters are inserted as follows:
Position the patient properly and pretreat with a topical anesthetic (eg, 2 percent lidocaine) and topical
vasoconstrictor (eg, oxymetazoline). Proper patient positioning and pretreatment are discussed above. (See
https://www.uptodate.com/contents/approach-to-the-adult-with-epistaTerm=epistaxis&selectedTitle=1%7E150&view=print&displayedView=full
Page 7 of 18
Approach to the adult with epistaxis
21/09/2016, 6:41 PM
'Physical examination' above.)
Advance the catheter along the floor of the nasal cavity until the retention ring reaches the entrance of the naris.
Inflate the posterior balloon with 10 mL of sterile water.
Retract the catheter gently until it lodges against the posterior choana in the nasopharynx.
Once the posterior balloon is seated, inflate the anterior balloon with 30 mL of sterile water. If the patient
experiences severe pain or deviation of the nasal septum or soft palate, gradually deflate the anterior balloon until
the pain or deviation resolve.
Pad and protect the alae and naris entrance as necessary to prevent excessive pressure.
Some balloon catheters are designed to be used with air. The Epistat II has a posterior balloon and an anterior Merocel
nasal tampon. Some devices are built around a central air passage to facilitate nose breathing. All balloon catheters are
designed for temporary control of bleeding and should NOT be left in place for more than three days.
Foley catheter If a balloon catheter is not available, posterior tamponade can be achieved by insertion of a 10 to 14
French Foley catheter using the following approach:
Position the patient properly and pretreat with a topical anesthetic (eg, 2 percent lidocaine) and topical
vasoconstrictor (eg, oxymetazoline). Proper patient positioning and pretreatment are discussed above. (See
'Physical examination' above.)
Before insertion, coat the catheter with a suitable, petroleum-free lubricant and trim the tip of the catheter to
minimize irritation of the posterior structures.
Advance the catheter along the floor of the nose until it is visible in the posterior oropharynx.
Partially fill the balloon with 5 to 7 mL of sterile water.
Retract the catheter gently until it lodges against the posterior choana in the nasopharynx.
Complete the filling of the balloon by adding another 5 mL of sterile water. Pain or distention of the soft palate
suggests overfilling.
Clamp the catheter in place with an umbilical clamp or small c-clamp, as from a nasogastric tube. Place padding
between the clamp and the alae to prevent excessive pressure, which otherwise can lead to necrosis.
Some clinicians prefer filling the balloon with air to minimize the risk of aspiration in case of balloon failure (which has
not been reported in this setting). However, the use of air in a balloon designed for fluid is associated with premature
deflation [67,70].
Many practitioners still pack the anterior nose at this point because, without perfect apposition, some blood will pool
anteriorly and exit the naris. Furthermore, some epistaxis episodes involve both anterior and posterior sources,
especially in the setting of a coagulopathy or hereditary hemorrhagic telangiectasia. Be sure to maintain gentle traction
on the Foley catheter while placing the anterior packing to avoid dislodgement of the former [38].
Be aware that petroleum-based products used for packing (such as BIPP or bacitracin ointment) can degrade the rubber
of the balloon, possibly leading to rupture [67].
Cotton packing Prior to the availability of balloon and Foley catheters, tamponade was achieved by means of cotton
packing. This process involves feeding a small caliber red rubber hose through the nose and retrieving it from the
oropharynx with a ring forceps (figure 2). A cotton pack is then tied to the oral end of the tube, with ties left long. The
hose is then retracted through the nose, while digitally guiding the pack posteriorly, until it lodges against the posterior
choana in the nasopharynx. The ties should now protrude through the nose. A second cotton pack or gauze roll is
secured to the nasal end of the ties against the nares to anchor the pack. When such posterior cotton packing is placed,
anterior packing is also generally needed.
Although direct posterior packing has been superseded in many United States settings, a small European trial,
comparing this technique with a bicameral balloon device demonstrated that it remains an effective and safe alternative
[71].
This type of posterior packing usually necessitates hospitalization out of concern for hypoxic complications, as well as
the risk of asphyxiation should the packing become dislodged.
https://www.uptodate.com/contents/approach-to-the-adult-with-epistaTerm=epistaxis&selectedTitle=1%7E150&view=print&displayedView=full
Page 8 of 18
Approach to the adult with epistaxis
21/09/2016, 6:41 PM
HOSPITALIZATION Most patients with a suspected posterior source of bleeding require hospitalization in a bed with
cardiac monitoring. Hospital admission may also be needed for patients with anterior packing who cannot be reasonably
expected to return for prompt follow-up or who have serious comorbidities or concerning symptoms.
Prolonged retention of nasal packing (greater than 72 hours) increases the risk of complications, including necrosis,
toxic shock syndrome, sinus or nasolacrimal infections, and dislodgment. At 24 to 48 hours, the consultant is likely to
remove any packing to inspect the site; further care may involve observation, repacking and observation, surgical
intervention, or arterial embolization in an interventional radiology suite.
COMPLICATIONS A retrospective review of 250 patients hospitalized for epistaxis (including both anterior and
posterior bleeds) found a 3 percent complication rate [14]. Complications included synechiae (intranasal adhesions),
aspiration, angina, myocardial infarction, and hypovolemia.
The risks of posterior packing do NOT include the hypothetical "nasopulmonary reflex," which was once believed to
account for hypoventilation and decreased arterial oxygen tension in patients with posterior nasal packs, leading to
recommendations for early surgery [72]. Studies have failed to identify physiologic changes attributable to posterior
packing. As examples, one report of 10 healthy volunteers who underwent posterior nasal packing found no changes in
pulmonary or cardiac function [73], and a prospective study of 19 hospitalized patients with posterior packing who were
observed with continuous pulse oximetry for a total of 1200 patient-hours found only two episodes of transient
desaturation, both of which were attributable to other causes [42].
TREATMENT FAILURES The management of conservative treatment failures varies according to available resources
and the clinical scenario. Surgical treatment is often performed endoscopically and can include ligation of the
sphenopalatine or anterior ethmoid artery (figure 1) [28,66,74]. Angiographic embolization is increasingly common, with
results that approximate those of surgical treatment (90 percent range) [75-77]. The rate of severe complications (eg,
stroke, blindness) with embolization is approximately four percent [15].
A number of studies have attempted to determine the likelihood of success and the relative costs of packing and
observation, surgery, and embolization [27,28,36,66,78]. Interpretation of the results is made difficult by the small
number of patients (ranging from 9 to 106), inability to perform blinded trials, and continual changes in surgical and
nonsurgical management. As an example, past comparisons of medical and surgical management generally involve
data obtained prior to the widespread use of endoscopic techniques [68].
Despite the limited data, an otolaryngology consultant would likely make a recommendation for definitive treatment
based upon individual patient factors, individual expertise, and available resources. Nasal packing and hospital
admission for observation remains a viable alternative to the more technology-intensive approaches to intractable
epistaxis.
INFORMATION FOR PATIENTS UpToDate offers two types of patient education materials, The Basics and Beyond
the Basics. The Basics patient education pieces are written in plain language, at the 5th to 6th grade reading level, and
they answer the four or five key questions a patient might have about a given condition. These articles are best for
patients who want a general overview and who prefer short, easy-to-read materials. Beyond the Basics patient
education pieces are longer, more sophisticated, and more detailed. These articles are written at the 10th to 12th grade
reading level and are best for patients who want in-depth information and are comfortable with some medical jargon.
Here are the patient education articles that are relevant to this topic. We encourage you to print or e-mail these topics to
your patients. (You can also locate patient education articles on a variety of subjects by searching on patient info and
the keyword(s) of interest.)
Basics topic (see "Patient education: Nosebleeds (The Basics)")
Beyond the Basics topic (see "Patient education: Nosebleeds (epistaxis) (Beyond the Basics)")
SUMMARY AND RECOMMENDATIONS
Most epistaxis is anterior, occurring in Kiesselbach's plexus; posterior bleeds can cause significant hemorrhage.
Anterior bleeds arise most commonly from trauma; other etiologies for anterior and posterior bleeds include
coagulation or platelet disorders, vascular lesions, nasal tumors, and hereditary telangiectasias. Hypertension
does not cause, but may prolong, epistaxis. (See 'Anatomy' above and 'Etiology' above.)
We suggest not ordering coagulation studies routinely; they are indicated for anticoagulated patients. Obtain a
complete blood count and a type and crossmatch for all patients with profuse bleeding. (See 'Coagulation studies
and other tests' above.)
https://www.uptodate.com/contents/approach-to-the-adult-with-epistaTerm=epistaxis&selectedTitle=1%7E150&view=print&displayedView=full
Page 9 of 18
Approach to the adult with epistaxis
21/09/2016, 6:41 PM
Initial measures for a patient with a nosebleed should include evaluating the airway and hemodynamic stability
(algorithm 1), and then having the patient perform basic tamponade maneuvers (picture 1 and picture 2). (See
'Initial assessment' above and 'Initial tamponade' above.)
The nose should be examined with a nasal speculum. If an anterior bleeding source is seen, we suggest cautery
with silver nitrate or electrocautery (Grade 2B). Both sides of the septum should not be cauterized at the same
time, to avoid septal necrosis. If no bleeding source is identified, the patient should be taught basic tamponade
technique and instructed to return for recurrent bleeding. (See 'Physical examination' above and 'Cautery' above.)
If bleeding continues despite cautery, nasal packing should be inserted into the anterior naris. Endoscopic cautery
is an alternative, if available. We suggest the use of nasal tampons or nasal balloon catheters rather than gauze
nasal packing (Grade 2B). The inserts are easier to apply and better tolerated than gauze packing, although the
treatments appear equally effective in controlling bleeding. (See 'Nasal packing' above.)
The appropriate use of antibiotic prophylaxis in patients with nasal packing remains controversial. We suggest that
antibiotics not be given routinely for prophylaxis against infection in patients with anterior nasal packing (Grade
2C). The decision to prescribe antibiotics is appropriately individualized to the patient. It may be reasonable to treat
patients at greater risk of infection. Patients should be evaluated by an ear, nose, and throat (ENT) specialist within
24 to 48 hours after packing is placed and should be warned about symptoms suggestive of toxic shock syndrome.
(See 'Antibiotics and toxic shock syndrome' above and 'Follow-up' above.)
Patients who continue to bleed after anterior packing most likely have a posterior bleed, and require posterior
packing with a specially developed nasal balloon catheter or a Foley catheter. Petroleum-based products (eg,
bacitracin ointment) may damage the balloon and should be avoided with posterior packing. (See 'Treatment of
posterior bleeding' above.)
Most patients who require posterior packing should be hospitalized for observation and assessment of the need for
further intervention with surgery or angiographic embolization. (See 'Hospitalization' above.)
Use of UpToDate is subject to the Subscription and License Agreement.
Topic 265 Version 16.0
https://www.uptodate.com/contents/approach-to-the-adult-with-epistTerm=epistaxis&selectedTitle=1%7E150&view=print&displayedView=full
Page 10 of 18
Approach to the adult with epistaxis
21/09/2016, 6:41 PM
GRAPHICS
Anatomy of the medial nasal wall
Blood supply to the nasal septum, demonstrating Kiesselbach's plexus.
Graphic 54180 Version 3.0
https://www.uptodate.com/contents/approach-to-the-adult-with-epistaTerm=epistaxis&selectedTitle=1%7E150&view=print&displayedView=full
Page 11 of 18
Approach to the adult with epistaxis
21/09/2016, 6:41 PM
Pinching the alae to stop a nosebleed
The initial attempt to tamponade a nosebleed involves the patient exerting pressure by grasping the alae
distally (below the bony nasal bridge) and pinching them tightly against the septum such that the mucosal
surfaces are tightly apposed, as is shown in the photographs above. This position should be held continuou
for 10 to 15 minutes.
Graphic 104672 Version 1.0
https://www.uptodate.com/contents/approach-to-the-adult-with-epistTerm=epistaxis&selectedTitle=1%7E150&view=print&displayedView=full
Page 12 of 18
Approach to the adult with epistaxis
21/09/2016, 6:41 PM
Patient tamponade of nosebleed
While the provider assembles necessary materials, the patient can
perform tamponade. The patient wears a protective gown. He bends at
the waist to minimize swallowing of blood and the risk of aspiration,
and grasps his nasal alae in firm approximation. The patient should be
encouraged not to check for active bleeding, but rather to hold
constant pressure for at least five minutes.
Courtesy of Harrison Alter, MD.
Graphic 66257 Version 4.0
https://www.uptodate.com/contents/approach-to-the-adult-with-epistTerm=epistaxis&selectedTitle=1%7E150&view=print&displayedView=full
Page 13 of 18
Approach to the adult with epistaxis
21/09/2016, 6:41 PM
Flow diagram for management of epistaxis in adults
ENT: ears, nose, and throat.
Graphic 82548 Version 3.0
https://www.uptodate.com/contents/approach-to-the-adult-with-epistTerm=epistaxis&selectedTitle=1%7E150&view=print&displayedView=full
Page 14 of 18
Approach to the adult with epistaxis
21/09/2016, 6:41 PM
Epistaxis management equipment list
Equipment:
Gloves, gown, mask, drapes
Emesis basin
Tongue depressors
Cotton pledgets, cotton swabs, and sterile gauze
Nasal speculum
Bayonet forceps
Frazier (or comparable) suction catheter
Syringes (10 and 20 mL)
Angiocatheter (22 gauge)
Isotonic saline; sterile water
Silver nitrate sticks
Electrical cautery device
Nasal tampons (eg, Merocel)
Nasal balloon catheters (eg, RapidRhino)
Foley catheter (12 French) and small c-clamp (eg, from nasogastric tube kit)
Ribbon gauze
Medications:
Oxymetazoline
Topical lidocaine (2 percent) or topical cocaine (4 percent)
Topical antibiotic ointment
Injectable lidocaine (1 or 2 percent) with epinephrine
Graphic 58901 Version 3.0
https://www.uptodate.com/contents/approach-to-the-adult-with-epistTerm=epistaxis&selectedTitle=1%7E150&view=print&displayedView=full
Page 15 of 18
Approach to the adult with epistaxis
21/09/2016, 6:41 PM
Tampon and balloon packs
L-R: Merocel tampon, 6 cm; Storz T-3100 balloon packing, 12 cm;
Rapid Rhino balloon pack with carboxymethylated cellulose mesh
casing, 7.5 cm.
Graphic 71487 Version 1.0
https://www.uptodate.com/contents/approach-to-the-adult-with-epistTerm=epistaxis&selectedTitle=1%7E150&view=print&displayedView=full
Page 16 of 18
Approach to the adult with epistaxis
21/09/2016, 6:41 PM
Packing to control posterior epistaxis
Prior to the availability of balloon catheters, tamponade was achieved
by means of cotton packing. This process involves: (A) feeding a small
caliber rubber hose through the nose, retrieving it from the oropharynx,
and attaching a cotton pack; (B) the hose is then retracted through the
nose, while digitally guiding the pack posteriorly, until it lodges against
the posterior choana; (C) a second cotton pack or gauze roll is secured
against the nares to secure the hose. Balloon catheters are preferable.
A foley catheter may be used (D).
Reproduced with permission from: Smelzter, SC, Bare, BG. Textbook of
Medical-Surgical Nursing, 9th Ed. Philadelphia: Lippincott Williams & Wilkins,
2000. Copyright 2000 Lippincott Williams & Wilkins.
Graphic 61765 Version 2.0
https://www.uptodate.com/contents/approach-to-the-adult-with-epistTerm=epistaxis&selectedTitle=1%7E150&view=print&displayedView=full
Page 17 of 18
Approach to the adult with epistaxis
21/09/2016, 6:41 PM
Contributor Disclosures
Harrison Alter, MD, MS, FACEP Nothing to disclose. Allan B Wolfson, MD Nothing to disclose. Daniel G Deschler,
MD, FACS Nothing to disclose. Jonathan Grayzel, MD, FAAEM Nothing to disclose.
Contributor disclosures are reviewed for conflicts of interest by the editorial group. When found, these are addressed by
vetting through a multi-level review process, and through requirements for references to be provided to support the
content. Appropriately referenced content is required of all authors and must conform to UpToDate standards of
evidence.
Conflict of interest policy
https://www.uptodate.com/contents/approach-to-the-adult-with-epistTerm=epistaxis&selectedTitle=1%7E150&view=print&displayedView=full
Page 18 of 18
You might also like
- Brain AbscessDocument25 pagesBrain AbscessprembarnabasNo ratings yet
- Acute Rheumatic Heart DiseaseDocument25 pagesAcute Rheumatic Heart DiseaseArun GeorgeNo ratings yet
- Update On The Management of Upper Gastrointestinal BleedingDocument12 pagesUpdate On The Management of Upper Gastrointestinal Bleedingakbar011512No ratings yet
- Intermediate UveitisDocument33 pagesIntermediate UveitismitaamayNo ratings yet
- Mallory Weiss SyndromeDocument10 pagesMallory Weiss SyndromeGuilherme CaneverNo ratings yet
- Management of Hypoxia During AnaesthesiaDocument5 pagesManagement of Hypoxia During AnaesthesiaNurhafizahImfista100% (1)
- Hydranencephaly ManagementDocument20 pagesHydranencephaly ManagementJohn Christopher LucesNo ratings yet
- TURP Procedure ExplainedDocument36 pagesTURP Procedure ExplainedRight VentricleNo ratings yet
- 33 - Nasal Fractures PDFDocument15 pages33 - Nasal Fractures PDFcarlosNo ratings yet
- Hydrocephalus: I Dewa Ketut Gede Herry Oka Pembimbing: Dr. Dr. I Wayan Niryana, Sp. BS (K)Document40 pagesHydrocephalus: I Dewa Ketut Gede Herry Oka Pembimbing: Dr. Dr. I Wayan Niryana, Sp. BS (K)Dewa Oka100% (1)
- Surgery Papillary Thyroid CADocument15 pagesSurgery Papillary Thyroid CAMelissa LabadorNo ratings yet
- 2013 Sepsis GuidelinesDocument58 pages2013 Sepsis GuidelinesMuhd Azam100% (1)
- 06prof. Riwanto-Abdominal Compartment SyndromeDocument41 pages06prof. Riwanto-Abdominal Compartment SyndromeTanujaa Venugopal100% (1)
- Bacterial Infections of The Skin, Soft TissuesDocument27 pagesBacterial Infections of The Skin, Soft TissuesSHIHAB UDDIN KAZI100% (1)
- Stress Ulcer ProphylaxisDocument24 pagesStress Ulcer ProphylaxisredyhataNo ratings yet
- Acute Dyspnea First RevisionDocument56 pagesAcute Dyspnea First RevisionAradhanaRamchandaniNo ratings yet
- Stevens Johnson DiseaseDocument5 pagesStevens Johnson DiseaseShammy RNNo ratings yet
- Causes and Treatment of EpistaxisDocument40 pagesCauses and Treatment of EpistaxisSilar KhanNo ratings yet
- Bronchial AsthmaDocument25 pagesBronchial AsthmaKamil HannaNo ratings yet
- Airway ManagementDocument63 pagesAirway ManagementGilang GumilangNo ratings yet
- Sepsis Power Point Slide Presentation - The Guidelines - Implementation For The FutureDocument25 pagesSepsis Power Point Slide Presentation - The Guidelines - Implementation For The Futuremontie13No ratings yet
- Referat: Pneumonia in ElderlyDocument41 pagesReferat: Pneumonia in Elderlyathieqah say-syahidahNo ratings yet
- Anatomy and Physiology of the ConjunctivaDocument43 pagesAnatomy and Physiology of the ConjunctivaVincentius Okta VidiandickaNo ratings yet
- ICU Rounds: Pulmonary Leukostasis as a Complication of LeukemiaDocument6 pagesICU Rounds: Pulmonary Leukostasis as a Complication of LeukemiaPratita Jati PermatasariNo ratings yet
- Nasal Fractures: Trauma To NoseDocument38 pagesNasal Fractures: Trauma To NoseSindhura ManjunathNo ratings yet
- Invasive Pulmonary Aspergi Llosis: Seminars in Respiratory and Critical Care MedicineDocument24 pagesInvasive Pulmonary Aspergi Llosis: Seminars in Respiratory and Critical Care MedicineChengShiun ShiueNo ratings yet
- ConjunctivitisDocument52 pagesConjunctivitisFiona H.D.100% (2)
- TLS FinalDocument69 pagesTLS FinalGrace Arthur100% (1)
- Abdominal Compartment SyndromeDocument7 pagesAbdominal Compartment Syndromemezgebu alemnehNo ratings yet
- Bronchiectasis: Dr.K.M.LakshmanarajanDocument238 pagesBronchiectasis: Dr.K.M.LakshmanarajanKM Lakshmana Rajan0% (1)
- Chronic Otitis Media, Cholesteatoma, and Mastoiditis in AdultsDocument14 pagesChronic Otitis Media, Cholesteatoma, and Mastoiditis in AdultschristineNo ratings yet
- Anatomy of The Nose and Paranasal SinusesDocument58 pagesAnatomy of The Nose and Paranasal SinuseschambhaNo ratings yet
- Bronchiolitis Guideline RecommendationsDocument10 pagesBronchiolitis Guideline RecommendationsAmi WilliamsNo ratings yet
- Airway AdjunctsDocument17 pagesAirway AdjunctsChannelGNo ratings yet
- Viral Exanthem (Main)Document94 pagesViral Exanthem (Main)Starlet Rhonadez Bito-onon OrielNo ratings yet
- Surviving Sepsis Campaign 2016 Guidelines PresentationDocument30 pagesSurviving Sepsis Campaign 2016 Guidelines PresentationwisnusigitpratamaNo ratings yet
- Tracheostomy 2Document41 pagesTracheostomy 2Khor Kee GuanNo ratings yet
- Adult Chemotherapy Anaphylaxis PolicyDocument12 pagesAdult Chemotherapy Anaphylaxis PolicyMohammed Gazo100% (1)
- Rheumatic Fever: DR: Kaem Shir AliDocument24 pagesRheumatic Fever: DR: Kaem Shir AliMwanja Moses100% (1)
- Glaucoma Diagnosis & Treatment GuideDocument42 pagesGlaucoma Diagnosis & Treatment GuideSaha DirllahNo ratings yet
- Systemic Inflammatory Response Syndrome (SIRS) PrognosisDocument16 pagesSystemic Inflammatory Response Syndrome (SIRS) PrognosisIPGDx100% (1)
- Anestesi Abdominal ApproachDocument14 pagesAnestesi Abdominal ApproachabdulkadirmunsyNo ratings yet
- Pfeiffer SyndromeDocument3 pagesPfeiffer SyndromeIfanRomliNo ratings yet
- Imaging Pulmonary Infection, Classic Sign and Pattern PRESENTASIDocument84 pagesImaging Pulmonary Infection, Classic Sign and Pattern PRESENTASIMark Brown100% (1)
- FOM Study Guide: Pleural Cavity, Lung Volumes & EffusionsDocument3 pagesFOM Study Guide: Pleural Cavity, Lung Volumes & EffusionsBernadine Cruz Par100% (1)
- Brain Abcess: Ahmad Usama Wali House Servant Medical 1Document28 pagesBrain Abcess: Ahmad Usama Wali House Servant Medical 1Ahmad Talha WaliNo ratings yet
- Ventilation Servo-I With Nava Neurally Controlled VentilationDocument14 pagesVentilation Servo-I With Nava Neurally Controlled Ventilationraju_pnNo ratings yet
- Clinical Assessment and Diagnosis of Hypovolemia (Dehydration) in Children - UpToDateDocument12 pagesClinical Assessment and Diagnosis of Hypovolemia (Dehydration) in Children - UpToDateNedelcu MirunaNo ratings yet
- Anesthesia Adjuvant DrugsDocument9 pagesAnesthesia Adjuvant DrugsArdra SabuNo ratings yet
- Infective Endocarditis: A Multidisciplinary ApproachFrom EverandInfective Endocarditis: A Multidisciplinary ApproachArman KilicNo ratings yet
- Hirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Problem-based Approach to Gastroenterology and HepatologyFrom EverandProblem-based Approach to Gastroenterology and HepatologyJohn N. PlevrisNo ratings yet
- Vascular Responses to PathogensFrom EverandVascular Responses to PathogensFelicity N.E. GavinsNo ratings yet
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsNo ratings yet
- Inflamed Trachea, (Tracheitis) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandInflamed Trachea, (Tracheitis) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Acute Asthma Exacerbations in Children: Emergency Department Management - UpToDateDocument13 pagesAcute Asthma Exacerbations in Children: Emergency Department Management - UpToDateTP RMadNo ratings yet
- Pathogen Es IsDocument2 pagesPathogen Es IsTP RMadNo ratings yet
- Initial Drugs For HFrEFDocument1 pageInitial Drugs For HFrEFTP RMadNo ratings yet
- Initial Drugs For HFrEFDocument1 pageInitial Drugs For HFrEFTP RMadNo ratings yet
- Behmed Quiz 4 Feb 2010Document2 pagesBehmed Quiz 4 Feb 2010TP RMadNo ratings yet
- Imaging of Pneumothorax - UpToDateDocument40 pagesImaging of Pneumothorax - UpToDateTP RMadNo ratings yet
- Treatment of Minor Thermal BurnsDocument22 pagesTreatment of Minor Thermal BurnsTP RMad100% (1)
- Blank 2Document5 pagesBlank 2TP RMadNo ratings yet
- Medical MnemotechnicsDocument149 pagesMedical MnemotechnicsMaja Maja BułkaNo ratings yet
- Secondary Spontaneous Pneumothorax in Adults - UpToDateDocument15 pagesSecondary Spontaneous Pneumothorax in Adults - UpToDateTP RMadNo ratings yet
- Acute Urinary RetentionDocument14 pagesAcute Urinary RetentionTP RMadNo ratings yet
- Med 1 Lecture No. 17 - Involuntary Weight Loss, Eating Disorders, ObesityDocument9 pagesMed 1 Lecture No. 17 - Involuntary Weight Loss, Eating Disorders, ObesityTP RMadNo ratings yet
- Glycopeptide and LincosamideDocument8 pagesGlycopeptide and LincosamideTP RMadNo ratings yet
- 2015 ESC IE Guidelines EHJ 2015Document54 pages2015 ESC IE Guidelines EHJ 2015TP RMadNo ratings yet
- Primary Spontaneous Pneumothorax in Adults - UpToDateDocument13 pagesPrimary Spontaneous Pneumothorax in Adults - UpToDateTP RMadNo ratings yet
- Pracs Reviewer - HematopathologyDocument5 pagesPracs Reviewer - HematopathologyTP RMadNo ratings yet
- PathoPracs SGD HeadNeck ElaineDocument15 pagesPathoPracs SGD HeadNeck ElaineTP RMadNo ratings yet
- Surg Samplex Unknown YearDocument4 pagesSurg Samplex Unknown YearTP RMadNo ratings yet
- Medicine 1 Final Practical Exam ReviewerDocument10 pagesMedicine 1 Final Practical Exam ReviewerTP RMadNo ratings yet
- AuscultogramDocument9 pagesAuscultogramTP RMadNo ratings yet
- COT Pathogenesis & Clin Manifestations PDFDocument1 pageCOT Pathogenesis & Clin Manifestations PDFTP RMadNo ratings yet
- Med 1 Lecture No. 24 - Geriatric MedicineDocument1 pageMed 1 Lecture No. 24 - Geriatric MedicineTP RMadNo ratings yet
- Surg Samplex Unknown YearDocument4 pagesSurg Samplex Unknown YearTP RMadNo ratings yet
- CE2 Schedule AY 09-10Document5 pagesCE2 Schedule AY 09-10TP RMadNo ratings yet
- Clinical Decision Using An Article About Treatment: George G. Lim, MD, FPSGS, FPCS, FpscrsDocument44 pagesClinical Decision Using An Article About Treatment: George G. Lim, MD, FPSGS, FPCS, FpscrsTP RMadNo ratings yet
- Literature SearchDocument3 pagesLiterature SearchTP RMadNo ratings yet
- Clinical Decision Using An Article About Treatment: George G. Lim, MD, FPSGS, FPCS, FpscrsDocument44 pagesClinical Decision Using An Article About Treatment: George G. Lim, MD, FPSGS, FPCS, FpscrsTP RMadNo ratings yet
- Principles of Decision Making: Clinical Decision Using An Article About TreatmentDocument8 pagesPrinciples of Decision Making: Clinical Decision Using An Article About TreatmentTP RMadNo ratings yet
- Revision and Second Term TestDocument15 pagesRevision and Second Term TestThu HươngNo ratings yet
- Engaged Listening Worksheet 3 - 24Document3 pagesEngaged Listening Worksheet 3 - 24John BennettNo ratings yet
- Arraignment PleaDocument4 pagesArraignment PleaJoh SuhNo ratings yet
- History of Early ChristianityDocument40 pagesHistory of Early ChristianityjeszoneNo ratings yet
- BIS Standards in Food SectorDocument65 pagesBIS Standards in Food SectorRino John Ebenazer100% (1)
- The Alkazi Collection of Photography Vis PDFDocument68 pagesThe Alkazi Collection of Photography Vis PDFMochamadRizkyNoorNo ratings yet
- Tele Phone Directory 2023-24Document10 pagesTele Phone Directory 2023-24vinoth5028No ratings yet
- Karnataka Email Id DataDocument5,173 pagesKarnataka Email Id DataSumalatha Venkataswamy100% (6)
- Issues and Concerns Related To Assessment in MalaysianDocument22 pagesIssues and Concerns Related To Assessment in MalaysianHarrish ZainurinNo ratings yet
- VT JCXDocument35 pagesVT JCXAkshay WingriderNo ratings yet
- Bracketing MethodsDocument13 pagesBracketing Methodsasd dsa100% (1)
- AIA Layer Standards PDFDocument47 pagesAIA Layer Standards PDFdanielNo ratings yet
- APFC Accountancy Basic Study Material For APFCEPFO ExamDocument3 pagesAPFC Accountancy Basic Study Material For APFCEPFO ExamIliasNo ratings yet
- Size, Scale and Overall Proportion of Form, Basic Understanding of Various Shapes, Inter-Relationship of Visual FormsDocument17 pagesSize, Scale and Overall Proportion of Form, Basic Understanding of Various Shapes, Inter-Relationship of Visual FormsJabbar AljanabyNo ratings yet
- 3 CRIM LAW 2 CASES TO BE DIGESTED Gambling Malfeasance Misfeasance Bribery Graft Corruption and MalversationDocument130 pages3 CRIM LAW 2 CASES TO BE DIGESTED Gambling Malfeasance Misfeasance Bribery Graft Corruption and MalversationElma MalagionaNo ratings yet
- PCC ConfigDocument345 pagesPCC ConfigVamsi SuriNo ratings yet
- Das Aufkommen Eines Neuen Pseudoephedrinprodukts Zur Bekämpfung Des MethamphetaminmissbrauchsDocument17 pagesDas Aufkommen Eines Neuen Pseudoephedrinprodukts Zur Bekämpfung Des Methamphetaminmissbrauchszossel ringoNo ratings yet
- Reaction PaperDocument1 pageReaction Papermarvin125No ratings yet
- Mixed-Use Proposal Dormitory and Hotel High-RiseDocument14 pagesMixed-Use Proposal Dormitory and Hotel High-RiseShanaia BualNo ratings yet
- Emilia Perroni-Play - Psychoanalytic Perspectives, Survival and Human Development-Routledge (2013) PDFDocument262 pagesEmilia Perroni-Play - Psychoanalytic Perspectives, Survival and Human Development-Routledge (2013) PDFMihaela Ioana MoldovanNo ratings yet
- I CEV20052 Structureofthe Food Service IndustryDocument98 pagesI CEV20052 Structureofthe Food Service IndustryJowee TigasNo ratings yet
- 2020 Non Student Candidates For PCL BoardDocument13 pages2020 Non Student Candidates For PCL BoardPeoples College of LawNo ratings yet
- Model Test Paper Maths CBSE Class IX - IIIDocument8 pagesModel Test Paper Maths CBSE Class IX - IIIAnanthakrishnan Tinneveli VNo ratings yet
- Maheshwar Handlooms Cluster Diagnostic StudyDocument15 pagesMaheshwar Handlooms Cluster Diagnostic Studyumang31390100% (3)
- Compiled May 5, 2017 Case DigestDocument16 pagesCompiled May 5, 2017 Case DigestGrace CastilloNo ratings yet
- Strategies in Various Speech SituationsDocument6 pagesStrategies in Various Speech SituationsSky NayytNo ratings yet
- Presentation 1Document13 pagesPresentation 1lordonezNo ratings yet
- Portland Cement: Material Safety Data Sheet (MSDS)Document6 pagesPortland Cement: Material Safety Data Sheet (MSDS)eslam sokaNo ratings yet
- Evirtualguru Computerscience 43 PDFDocument8 pagesEvirtualguru Computerscience 43 PDFJAGANNATH THAWAITNo ratings yet
- New Member OrientationDocument41 pagesNew Member OrientationM.NASIRNo ratings yet