Professional Documents
Culture Documents
Hypertonic Saline Myth
Uploaded by
Richo Wijaya0 ratings0% found this document useful (0 votes)
26 views2 pageshoo
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documenthoo
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
26 views2 pagesHypertonic Saline Myth
Uploaded by
Richo Wijayahoo
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 2
Editorials
Hyperosmolar Therapy for Intracranial Hypertension:
Time to Dispel Antiquated Myths
Pharmacologic induction of supraphysiologic serum osmolality
(hyperosmolar therapy) with either mannitol or hypertonic saline
(HTS) is the mainstay of medical management for patients with
acute intracranial hypertension, and its efficacy for reduction of intracranial pressure (ICP) has been demonstrated consistently (1).
Despite the absence of supporting evidence, several myths regarding the selection, administration, titration, and complications of
hyperosmolar therapy endure. Regrettably, their perpetuation
risks delaying the delivery or compromising the appropriate use
of this potentially life-saving therapy. This commentary examines
four of the most significant myths regarding hyperosmolar therapy and summarizes briefly the refuting evidence with the goal
of removing unsubstantiated treatment barriers and improving
the evidence-based delivery of appropriate medical therapy to
patients with elevated ICP.
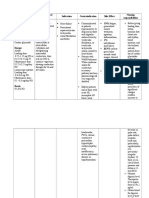
MYTH #1: MANNITOL AND HTS THERAPY
ARE EQUIVALENT
The term hyperosmolar therapy may inadvertently connote
that the ultimate goal is supraphysiologic osmolality without
regard to the agent selected to induce the hyperosmolar state.
Although both mannitol and HTS are effective in reducing brain
water content and ICP (13), animal studies suggest greater
short- and intermediate-term reduction in brain water with
HTS (3). The results of human studies are more ambiguous,
but recent data also suggest that HTS may outperform mannitol
in ICP reduction (3, 4). In addition, HTS is effective at achieving
ICP control when mannitol therapy fails (4, 5). Although overall
superiority may ultimately depend on a variety of clinical factors,
these data refute the notion that all agents for inducing and
maintaining hyperosmolar states are clinically equivalent.
MYTH #2: MANNITOL THERAPY SHOULD BE
TITRATED TO SERUM OSMOLALITY TO AVOID
RENAL INSUFFICIENCY
A common misconception is that the risk of acute renal insufficiency (ARI) among patients receiving maintenance mannitol
therapy is mitigated by maintaining serum osmolality (Sosm) ,
320 mOsm/L, and thus this parameter is frequently used as
a threshold for dose titration. However, recent data demonstrate
no independent association between Sosm and ARI (6). Conversely, the serum osmolal gap (OG, Osmcalculated 2 Osmmeasured)
may be a more predictive metric (7, 8), and ARI is rare when OG
is less than 55 mOsm/L (8). OG is also preferable because its
levels are stable in the ICU population and because, as an unmeasured osmole, mannitol accumulation correlates well with
increasing OG (7). Together, these data suggest that strategies
Author Contributions: N.M.: manuscript design, acquisition of data, and writing
and editing manuscript.
Dr. Nicholas Marko is a neurosurgeon supported by a grant from the William P.
Van Wagenen fellowship program of the American Association of Neurological
Surgeons.
Am J Respir Crit Care Med Vol 185, Iss. 5, pp 467478, Mar 1, 2012
Internet address: www.atsjournals.org
for monitoring and titrating mannitol therapy to OG may be
more clinically relevant than those based on following Sosm.
MYTH #3: ACUTE, INTERMITTENT PERIPHERAL
INFUSION OF HTS CAUSES PHLEBITIS, REGIONAL
NECROSIS, AND INTRAVASCULAR HEMOLYSIS
Peripheral infusion of HTS, even in the acute setting, is often
avoided by clinicians or prohibited by institutions because of concerns for phlebitis, regional necrosis, or intravascular hemolysis.
These practices are likely based on literature regarding infusion
of hypertonic parenteral nutrition, which reveals a duration- and
osmolality-dependent relationship between peripheral infusion
and local vascular complications (9). These data, however, describe the sequelae of long-term peripheral infusion, and there is
no evidence suggesting their generalizability to the practice of
intermittent, peripheral bolus administration of HTS. To the contrary, histologic investigations from animal models demonstrate
no evidence of vascular damage associated with peripheral boluses
(10), and human data from prehospital resuscitation with peripherally administered HTS report no regional vascular complications
(11). In the absence of evidence of clinical complications, and with
both animal and human data suggesting the safety of peripheral
HTS boluses (10, 11), the practice of withholding hyperosmolar
therapy for lack of central venous access appears unjustified.
A related concern is the fear of intravascular hemolysis after
peripheral administration of HTS. This may be grounded in
early in vitro investigations of red blood cell membrane fragility and augmented by more recent evidence of hemolysis when
HTS was administered in a canine model (12). However, the
former results are not reproducible in vitro (13), whereas the latter
are confounded by a uniquely canine deficiency of the red
blood cell membrane Na1/K1-ATPase that increases susceptibility to osmolality-associated hemolysis (14). Accordingly, no modern evidence supports the concern for HTS-induced intravascular
hemolysis with peripheral bolus administration in humans.
MYTH #4: HTS THERAPY MUST BE INITIATED
SLOWLY TO REDUCE THE RISK OF CENTRAL
PONTINE MYELINOLYSIS
Since its characterization in 1959 (15), concerns for iatrogenically
inducing the often-discussed yet rarely witnessed syndrome of
osmotic demyelination (central pontine myelinolysis [CPM])
have engendered a tendency among clinicians toward slow
administration of supraphysiologic sodium solutions. Although
50 years of investigation have yet to identify definitively the etiology of CPM (16), investigators have reported several findings
that appear to mitigate the requisite clinical concern over CPM
when HTS is used to treat elevated ICP. First, CPM typically
occurs in the setting of chronic comorbidities believed to compromise neuronal and glial energy supply and is, therefore, rarely
observed without concomitant chronic alcoholism, malnourishment, liver disease, hypoglycemia, or syndrome of inappropriate
antidiuretic hormone (16). Next, only approximately 22% of modern cases of CPM are associated with intravenous sodium therapy,
and nearly all of these involve correction of profound baseline
468
AMERICAN JOURNAL OF RESPIRATORY AND CRITICAL CARE MEDICINE
hyponatremia (16). Finally, evidence suggests that bolus infusions
of more than 300 mOsm of sodium given over 20 minutes are
clinically well tolerated (17), even though the resulting increase
in serum sodium significantly exceeds the often-quoted safe rate
of 0.5 mEq/L/hour. In the absence of preexisting hyponatremia
and predisposing comorbidities, there is little evidence to suggest
that rapid elevation of serum sodium with HTS during initiation
of acute hyperosmolar therapy presents a significant CPM risk for
most patients.
This discussion is not intended to be a comprehensive review of
hyperosmolar therapy, and interested readers should consult such
a publication (18) for additional information and for further references. Additionally, the goal is not to encourage the injudicious use
of hyperosmolar therapy, as the modality is not without risk and
because the aforementioned side effects, although highly improbable, are not theoretically impossible. Accordingly, consultation
with an experienced intensivist, neurologist, or neurosurgeon remains invaluable in the management of patients with elevated ICP,
particularly since this represents a rapidly evolving field in which
ongoing appraisal of the literature is necessary. Notwithstanding,
the preponderance of clinical evidence dispels several antiquated
myths associated with hyperosmolar therapy that have persisted
for generations within the collective consciousness of the medical
community. Changes in individual practice and institutional policies grounded in concerns for patient safety but predicated upon
these unsubstantiated myths are long overdue, as appropriate delivery of hyperosmolar therapy reduces morbidity and improves
survival among patients with intracranial hypertension.
Author disclosures are available with the text of this article at www.atsjournals.org.
Acknowledgment: The author thanks Drs. Robert Weil and Andrew Torre-Healey
for their generous contributions to and valuable insights regarding this discussion.
Nicholas F. Marko, M.D.
Cancer Research UK Cambridge Research Institute
Cambridge, United Kingdom
and
Department of Applied Mathematics and Theoretical Physics
University of Cambridge
Cambridge, United Kingdom
References
1. Kamel H, Navi BB, Nakagawa K, Hemphill JC III, Ko NU. Hypertonic saline
versus mannitol for the treatment of elevated intracranial pressure: a metaanalysis of randomized clinical trials. Crit Care Med 2011;39:554559.
2. Freshman SP, Battistella FD, Matteucci M, Wisner DH. Hypertonic
saline (7.5%) versus mannitol: a comparison for treatment of acute
head injuries. J Trauma 1993;35:344348.
VOL 185
2012
3. Qureshi AI, Wilson DA, Traystman RJ. Treatment of elevated intracranial
pressure in experimental intracerebral hemorrhage: comparison between
mannitol and hypertonic saline. Neurosurgery 1999;44:10551063. [Discussion, pp. 10631054.]
4. Mortazavi MM, Romeo AK, Deep A, Griessenauer CJ, Shoja MM,
Tubbs RS, Fisher W. Hypertonic saline for treating raised intracranial
pressure: literature review with meta-analysis. J Neurosurg 2011.
5. Horn P, Munch E, Vajkoczy P, Herrmann P, Quintel M, Schilling L,
Schmiedek P, Schurer L. Hypertonic saline solution for control of
elevated intracranial pressure in patients with exhausted response to
mannitol and barbiturates. Neurol Res 1999;21:758764.
6. de Assis Aquino Gondim F, Aiyagari V, Shackleford A, Diringer MN.
Osmolality not predictive of mannitol-induced acute renal insufficiency. J Neurosurg 2005;103:444447.
7. Garcia-Morales EJ, Cariappa R, Parvin CA, Scott MG, Diringer MN.
Osmole gap in neurologic-neurosurgical intensive care unit: its normal
value, calculation, and relationship with mannitol serum concentrations. Crit Care Med 2004;32:986991.
8. Visweswaran P, Massin EK, Dubose TD Jr . Mannitol-induced acute
renal failure. J Am Soc Nephrol 1997;8:10281033.
9. Timmer JG, Schipper HG. Peripheral venous nutrition: the equal relevance of volume load and osmolarity in relation to phlebitis. Clin Nutr
1991;10:7175.
10. Hands R, Holcroft JW, Perron PR, Kramer GC. Comparison of peripheral and central infusions of 7.5% NaCl/6% dextran 70. Surgery
1988;103:684689.
11. Mattox KL, Maningas PA, Moore EE, Mateer JR, Marx JA, Aprahamian C, Burch JM, Pepe PE. Prehospital hypertonic saline/dextran
infusion for post-traumatic hypotension: the U.S.A. multicenter trial.
Ann Surg 1991;213:482491.
12. Rocha e Silva M, Velasco IT, Porfirio MF. Hypertonic saline resuscitation: saturated salt-dextran solutions are equally effective, but induce
hemolysis in dogs. Crit Care Med 1990;18:203207.
13. Moore GL, Summary JJ, Dubick MA, Ledford ME, Ryan BA, Gonzales
A, Wade CE. Effects of hypertonic saline (7.5%)/dextran 70 on human
red cell typing, lysis, and metabolism in vitro. Vox Sang 1990;59:227231.
14. Parker JC. Dog red blood cells: adjustment of salt and water content in
vitro. J Gen Physiol 1973;62:147156.
15. Adams RD, Victor M, Mancall EL. Central pontine myelinolysis:
a hitherto undescribed disease occurring in alcoholic and malnourished patients. AMA Arch Neurol Psychiatry 1959;81:154172.
16. Kleinschmidt-Demasters BK, Rojiani AM, Filley CM. Central and
extrapontine myelinolysis: then.and now. J Neuropathol Exp Neurol
2006;65:111.
17. Huang SJ, Chang L, Han YY, Lee YC, Tu YK. Efficacy and safety of
hypertonic saline solutions in the treatment of severe head injury.
Surg Neurol 2006;65:539546. [Discussion, p. 546.]
18. Torre-Healy A, Marko NF, Weil RJ. Hyperosmolar therapy for intracranial hypertension. Neurocrit Care (In press)
Copyright 2012 by the American Thoracic Society
DOI: 10.1164/rccm.201109-1698ED
Interferon-l1 and Viral Wheeze in Asthma:
A Gothic Duality?
A recurring theme in Gothic literature is that the human condition is an enigmatic mixture of good and evil. These themes
are central in classics such as Robert Louis Stevensons
Dr. Jekyll and Mr. Hyde, in which the protagonist begins as
a respected pillar of the community, but his darker side
becomes evident as the story unfolds. In this issue of the Journal, Miller and colleagues (pp. 508516) suggest that IFN-l1,
Supported by National Institutes of Health Grants U19 AI070503-01, P01
HL070831, and HHSN272200900052C.
a prototypic antiviral cytokine, may also have an injurious
duality (1).
Previous studies have demonstrated that rhinovirus (HRV)
infections are closely associated with exacerbations of childhood
asthma. Since HRV infections often cause mild or asymptomatic
illnesses, this raises questions as to mechanisms that differentiate
mild colds from severe episodes of wheezing and shortness of
breath in children with asthma. Viral factors could relate to the
great diversity among HRVs, which consist of over 150 different
types in three species (A, B, and C). In fact, there is some evidence
that infections with HRV-C species viruses may be more likely to
You might also like
- Review ArticleDocument11 pagesReview ArticleZainuddin Surkan HNo ratings yet
- Hyperosmolar Treatment For Patients at Risk For Increased Intracranial Pressure: A Single-Center Cohort StudyDocument12 pagesHyperosmolar Treatment For Patients at Risk For Increased Intracranial Pressure: A Single-Center Cohort Studyandi kurniawanNo ratings yet
- Risk Factors For Nonadherence To Antihypertensive Treatment: Original ArticleDocument11 pagesRisk Factors For Nonadherence To Antihypertensive Treatment: Original Articlebram AyuNo ratings yet
- SSH en HTE. J Neuros 2012Document12 pagesSSH en HTE. J Neuros 2012Laura López Del Castillo LalydelcaNo ratings yet
- Biruh T Workeneh Hyponatremia Demystified IntegratingDocument17 pagesBiruh T Workeneh Hyponatremia Demystified IntegratingsaqqarazoserNo ratings yet
- Blood Transfusion in Critical Care: Giora Netzer, Richard P Dutton and John R HessDocument3 pagesBlood Transfusion in Critical Care: Giora Netzer, Richard P Dutton and John R Hessnevermore11No ratings yet
- Hta (G4)Document9 pagesHta (G4)Juan LeonNo ratings yet
- E2f7 PDFDocument7 pagesE2f7 PDFSujith KumarNo ratings yet
- Review Article Permissive Hypotensive Resuscitation - An Evolving Concept in TraumaDocument3 pagesReview Article Permissive Hypotensive Resuscitation - An Evolving Concept in TraumareioctabianoNo ratings yet
- Coherencia HemodinamicaDocument9 pagesCoherencia HemodinamicaMaritza Alejandra Baeza EricesNo ratings yet
- NEJMra 040291Document12 pagesNEJMra 040291alamajorNo ratings yet
- Wa0004.Document17 pagesWa0004.nhunhuochachNo ratings yet
- Plasma Exchange For Heparin-Induced Thrombocytopenia: Is There Enough Evidence?Document4 pagesPlasma Exchange For Heparin-Induced Thrombocytopenia: Is There Enough Evidence?sayednourNo ratings yet
- Saline TherapyDocument3 pagesSaline Therapysatyagraha84No ratings yet
- Protection Against Severe Hypokalemia But Impaired Cardiac Repolarization After Intense Rowing Exercise in Healthy Humans Receiving SalbutamolDocument3 pagesProtection Against Severe Hypokalemia But Impaired Cardiac Repolarization After Intense Rowing Exercise in Healthy Humans Receiving SalbutamolLuthfiya NabiilaNo ratings yet
- Evidence and Triggers For The Transfusion of Blood and Blood ProductsDocument9 pagesEvidence and Triggers For The Transfusion of Blood and Blood Productscahaya tinggiNo ratings yet
- HIE and CVSDocument11 pagesHIE and CVSakshayajainaNo ratings yet
- Manejo de La Sepsis 2Document5 pagesManejo de La Sepsis 2Rachmi Pratiwi Febrita PartiNo ratings yet
- Study of Drug Use in Essential Hypertension and Their ComplianceDocument13 pagesStudy of Drug Use in Essential Hypertension and Their ComplianceRachmat MuhammadNo ratings yet
- Review Article: Animal Models of Hypertension: An OverviewDocument14 pagesReview Article: Animal Models of Hypertension: An OverviewrodrigodaliascienceNo ratings yet
- Burden of Sodium Abnormalities in Patients Hospitalized For Heart FailureDocument7 pagesBurden of Sodium Abnormalities in Patients Hospitalized For Heart FailureVincent ReyesNo ratings yet
- Circ Heart Fail 2009 Patten 138 44Document8 pagesCirc Heart Fail 2009 Patten 138 44bogdan202No ratings yet
- End of The Road For Heparin Thromboprophylaxis 2016Document3 pagesEnd of The Road For Heparin Thromboprophylaxis 2016Michael FreudigerNo ratings yet
- Thrombolitic TeraphyDocument8 pagesThrombolitic TeraphyFyan FiradyNo ratings yet
- "Triple H" Therapy For Aneurysmal Subarachnoid Haemorrhage: Real Therapy or Chasing Numbers?Document0 pages"Triple H" Therapy For Aneurysmal Subarachnoid Haemorrhage: Real Therapy or Chasing Numbers?ganpur01No ratings yet
- Resistant HypertensionDocument12 pagesResistant Hypertensionsury listinNo ratings yet
- Intradialitic HypotensionDocument7 pagesIntradialitic HypotensionanitaNo ratings yet
- Abraham 2015Document14 pagesAbraham 2015Luis Rafael Suárez U.No ratings yet
- Art Farmaco 2Document7 pagesArt Farmaco 2Nataly Rico JimenezNo ratings yet
- Hemorrhagic Transformation After Cerebral InfarctionDocument14 pagesHemorrhagic Transformation After Cerebral InfarctionAlyk Tumayan CalionNo ratings yet
- Mechanisms, Clinical Implications, and Treatment of Intradialytic HypotensionDocument7 pagesMechanisms, Clinical Implications, and Treatment of Intradialytic Hypotensionhemer hadyn calderon alvitesNo ratings yet
- Tilburg University: Franse, L.V. Pahor, M. Di Bari, M. Somes, G.W. Cushman, W.C. Applegate, W.BDocument8 pagesTilburg University: Franse, L.V. Pahor, M. Di Bari, M. Somes, G.W. Cushman, W.C. Applegate, W.Bpooria shNo ratings yet
- Frank 2019Document15 pagesFrank 2019Oliver ArteagaNo ratings yet
- Hypothermia May Facilitate Liver Transplant in Patients With Increased Intracranial PressureDocument18 pagesHypothermia May Facilitate Liver Transplant in Patients With Increased Intracranial Pressurexai_teovisioNo ratings yet
- Vox SanguinisDocument179 pagesVox SanguinistristanmunarNo ratings yet
- Massive Transfusion ProtocolDocument11 pagesMassive Transfusion ProtocolAlaa Abdelmoaty OmranNo ratings yet
- Tratamiento de Hta ResistenteDocument19 pagesTratamiento de Hta Resistenteoscar Montoya LopezNo ratings yet
- Santoso2005Document11 pagesSantoso2005ayubahriNo ratings yet
- Practice ParametersDocument48 pagesPractice Parametersmisbah_mdNo ratings yet
- Revista Brasileira de AnestesiologiaDocument9 pagesRevista Brasileira de Anestesiologiapc pNo ratings yet
- VHRM 5 1043Document16 pagesVHRM 5 1043AldiKurosakiNo ratings yet
- Jurnal 6Document10 pagesJurnal 6rifkipspdNo ratings yet
- VisionDocument10 pagesVisionJoao LucasNo ratings yet
- Diabetes Mellitus and Heart Failure 2017 The American Journal of MedicineDocument11 pagesDiabetes Mellitus and Heart Failure 2017 The American Journal of MedicineAlina PopaNo ratings yet
- TransfusiDocument10 pagesTransfusiDevia PebriyentiNo ratings yet
- Hipertrofia VD en HTADocument8 pagesHipertrofia VD en HTAgustavo reyesNo ratings yet
- Treatment of Venous Thromboembolism: ReviewDocument12 pagesTreatment of Venous Thromboembolism: ReviewMayra Alejandra Prada SerranoNo ratings yet
- Senam OtakDocument15 pagesSenam OtakDewi WulandariNo ratings yet
- Therapeutic Strategies For Treatment of Immune MedDocument23 pagesTherapeutic Strategies For Treatment of Immune MedTactvisNo ratings yet
- 12 JMSCRDocument6 pages12 JMSCRArdianNo ratings yet
- Contraindications To Vasoconstrictors in Dentistry: Part IIDocument5 pagesContraindications To Vasoconstrictors in Dentistry: Part IIBunga Erlita RosaliaNo ratings yet
- Hemorrhagic Shock in The Pediatric Patient - New Therapies and PracticeDocument6 pagesHemorrhagic Shock in The Pediatric Patient - New Therapies and Practicefitrah fajrianiNo ratings yet
- Perioperativefluid Therapy: Denise Fantoni,, Andre C. ShihDocument12 pagesPerioperativefluid Therapy: Denise Fantoni,, Andre C. ShihDaniela BenavidesNo ratings yet
- Anesth Analg 2010 Elliott 1419 27Document9 pagesAnesth Analg 2010 Elliott 1419 27Darrel Allan MandiasNo ratings yet
- Determinants of IV Heparin Treatment in Patients With Ischemic StrokeDocument3 pagesDeterminants of IV Heparin Treatment in Patients With Ischemic StrokeDewi LestariNo ratings yet
- Fluid Therapy in Septic ShockDocument12 pagesFluid Therapy in Septic ShockAnn BartonNo ratings yet
- A Study To Evaluate Effectiveness of Cold Application and Magnesium Sulphate Application On Superficial Thrombophlebitis Among Patients Receiving Intravenous Therapy in Selected Hospitals Amritsar.Document25 pagesA Study To Evaluate Effectiveness of Cold Application and Magnesium Sulphate Application On Superficial Thrombophlebitis Among Patients Receiving Intravenous Therapy in Selected Hospitals Amritsar.Navjot Brar71% (14)
- Hypothermia-Ischemia Final Draft E-PortfolioDocument11 pagesHypothermia-Ischemia Final Draft E-Portfolioapi-317145308No ratings yet
- Complementary and Alternative Medical Lab Testing Part 4: VascularFrom EverandComplementary and Alternative Medical Lab Testing Part 4: VascularNo ratings yet
- Praktis-The Role of Echocardiogram in Outpatient Paediatric Chest PainDocument8 pagesPraktis-The Role of Echocardiogram in Outpatient Paediatric Chest PainRicho WijayaNo ratings yet
- Guideline ITPDocument11 pagesGuideline ITPRicho WijayaNo ratings yet
- ILAE Classification of The Epilepsies Scheffer2017Document10 pagesILAE Classification of The Epilepsies Scheffer2017Richo WijayaNo ratings yet
- Biomarker in Early Neonatal Sepsis PDFDocument5 pagesBiomarker in Early Neonatal Sepsis PDFRicho WijayaNo ratings yet
- Enteral Nutrition Practices in Critically Ill.1Document6 pagesEnteral Nutrition Practices in Critically Ill.1Richo WijayaNo ratings yet
- Eating Disorders Identifying and TreatingDocument10 pagesEating Disorders Identifying and TreatingRicho WijayaNo ratings yet
- MrsaDocument38 pagesMrsahahmed78No ratings yet
- Cancer Prevention and Early DetectonDocument64 pagesCancer Prevention and Early DetectonRicho WijayaNo ratings yet
- Vitamin K Coagulopathy 2017Document10 pagesVitamin K Coagulopathy 2017Richo WijayaNo ratings yet
- Haemophilia and DentalDocument8 pagesHaemophilia and DentalRicho WijayaNo ratings yet
- Eating Disorder Medication PDFDocument4 pagesEating Disorder Medication PDFRicho WijayaNo ratings yet
- Circumcision in HemophiliaDocument11 pagesCircumcision in HemophiliaRicho WijayaNo ratings yet
- Piis0022347614007379 PDFDocument6 pagesPiis0022347614007379 PDFDevi SiagianNo ratings yet
- Nutrional ManagementDocument8 pagesNutrional ManagementRicho WijayaNo ratings yet
- Dai KenchuDocument6 pagesDai KenchuRicho WijayaNo ratings yet
- Immunopathogenesis of HIV InfectionDocument13 pagesImmunopathogenesis of HIV InfectionRicho WijayaNo ratings yet
- Hypertonic Saline Reduce TIKDocument9 pagesHypertonic Saline Reduce TIKRicho WijayaNo ratings yet
- Signs of Childhood CancerDocument10 pagesSigns of Childhood CancerCrizina VashtiNo ratings yet
- 3 Statistical Approaches To Analysis of Small Clinical Trials - Small Clinical Trials - Issues and Challenges - The National Academies PressDocument47 pages3 Statistical Approaches To Analysis of Small Clinical Trials - Small Clinical Trials - Issues and Challenges - The National Academies PressSFDNo ratings yet
- Inguinal HernioplastyDocument10 pagesInguinal HernioplastyfiansisNo ratings yet
- Xper Information Management: Quick Reference Guide - Arterial TreesDocument11 pagesXper Information Management: Quick Reference Guide - Arterial TreeswiwingNo ratings yet
- DigoxinDocument4 pagesDigoxinJaessa FelicianoNo ratings yet
- Nclex PDFDocument35 pagesNclex PDFHan NahNo ratings yet
- Inotropes and vasoactive drugs in the PICUDocument2 pagesInotropes and vasoactive drugs in the PICULynda TsaiNo ratings yet
- Gerontology in CroatiaDocument20 pagesGerontology in Croatiasirup_girlNo ratings yet
- Reed Mod3 Assignment 3 Policies For Retention and Destruction of Health RecordsDocument3 pagesReed Mod3 Assignment 3 Policies For Retention and Destruction of Health Recordsapi-340267228100% (1)
- Presentasi Dr. Deddy Saputra, SpBP-RE FIXDocument25 pagesPresentasi Dr. Deddy Saputra, SpBP-RE FIXwiko wicaksonoNo ratings yet
- Assessing Pain in Patients: Art ScienceDocument5 pagesAssessing Pain in Patients: Art ScienceShweta SheoranNo ratings yet
- Advances in Surgical EndodonticsDocument16 pagesAdvances in Surgical EndodonticsBianca NeaguNo ratings yet
- Benefits of massage therapyDocument2 pagesBenefits of massage therapyCleyton MendesNo ratings yet
- Community-Oriented Nursing and Public HealthDocument6 pagesCommunity-Oriented Nursing and Public Healthsbg04No ratings yet
- Daftar Pustaka Fistula Preaurikular TerinfeksiDocument2 pagesDaftar Pustaka Fistula Preaurikular TerinfeksiTheofilus AswadiNo ratings yet
- Deep Neck Infection 051005Document43 pagesDeep Neck Infection 051005Vishal GauravNo ratings yet
- Crab Tales Issue 029Document16 pagesCrab Tales Issue 029Crab TalesNo ratings yet
- Schoolssummit11 Pierce ChecklistDocument39 pagesSchoolssummit11 Pierce ChecklistMiljan MadicNo ratings yet
- Workshop CRRT PDFDocument88 pagesWorkshop CRRT PDFDesy rahmatNo ratings yet
- DGHS IPHS CommunityHealthCentresDocument120 pagesDGHS IPHS CommunityHealthCentresSargam MahendruNo ratings yet
- Clinical Management VHF Pocket BookDocument113 pagesClinical Management VHF Pocket BookZeljnaznanjaNo ratings yet
- Comprehensive Nursing AssessmentDocument3 pagesComprehensive Nursing AssessmentIvana Dobras100% (2)
- Growth in Children With Congenital Heart DiseaseDocument9 pagesGrowth in Children With Congenital Heart DiseaseAlbert SantosoNo ratings yet
- DRUG STUDY MetoprololDocument1 pageDRUG STUDY MetoprololSymone Jay Lapiz100% (2)
- MODS Presentation FinalDocument38 pagesMODS Presentation Finaljoe_egypt_866088307100% (1)
- Inguinal Hernia OperationDocument2 pagesInguinal Hernia Operationjanispachie7No ratings yet
- Crowe S ClassificationDocument3 pagesCrowe S ClassificationErnesto Ewertz MiquelNo ratings yet
- Annotated - Exam Key - First Aid C - 10 28 2014 PDFDocument5 pagesAnnotated - Exam Key - First Aid C - 10 28 2014 PDFSuliemanNo ratings yet
- Ksad PDFDocument215 pagesKsad PDFLNo ratings yet
- AST Recommended Standards of Practice For Surgical DrapesDocument7 pagesAST Recommended Standards of Practice For Surgical DrapesJeff HowardNo ratings yet
- A New Drug-Shelf Arrangement For Reducing MedicatiDocument9 pagesA New Drug-Shelf Arrangement For Reducing MedicatiEmmanuel LawerNo ratings yet