Professional Documents
Culture Documents
Junior Intern Notes
Uploaded by
Tin SumangaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Junior Intern Notes
Uploaded by
Tin SumangaCopyright:
Available Formats
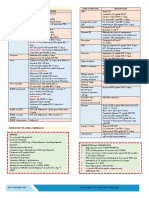
Cardio Notes First Degree Heart Block
2:1 Heart Block
Lead II long PR interval
Lead II 2 P waves per QRS complex
JNC Classification and Initial Drug Therapy NYHA FUNCTIONAL CLASSIFICATION FRAMINGHAMS CRITERIA FOR CHF DIAGNOSIS
ECG CLASS I No limitation of PA
Heart Rate = # of small boxes 1500 Digitalis Effect Lead II scooping ST segment No sx w/ ordinary exertion
<120/80 normal Major Minor
Hypercalcemia Lead II short/absent ST segment 120-139 PreHPN no antiHPN drugs indicated CLASS II Slight limitation of PA PND Extremity edema
Normal Cardiac Rhythm: Hyperkalemia Lead II tent-shaped T wave 80-89 Ordinary activity causes sx NVD Dyspnea on exertion
QRS width 0.08-0.12 sec Idioventricular Rhythm Lead II no P wave, bizarre QRS, 140-159 Stage I thiazide diuretic for most: ACE- CLASS III Marked limitation of PA Rales Hepatomegaly
P-R interval 0.12-0.20 sec (IVR) R 20-40 90-99 I,ARB,B-blocker, CCB or combination Less than ordinary activity causes sx Cardiomegaly Pleural Effusion
Q-T interval 0.30-0.40 sec Premature Atrial Lead II premature P wave, >160 Stage II 2-drug combination for most, Thiazide Asx at rest Acute Pulmonary Edema Vital capacity reduced by
Contraction (PAC) irregular P-P interval 100 diuretic +ACE-I or ARB or B-blocker, CLASS IV Inability to carry out PA w/o S3 Gallop 1/3 of normal
PR interval >0.20 sec Premature Ventricular Lead II wide QRS unrelated to P wave CCB discomfort Increased venous pressure Tachycardia >120 bpm
1st Degree AV Block - >0.20 sec Contraction (PVC) Sx at rest angina + hepatojugular reflus
2nd Degree AV Block Ventrricular Fibrillation Chaotic waves Hypertensive Urgency: Major or Minor: wt loss >4.5 kg over 5days of treatment
Type 1 (Mobitz I or Wenckeback) (VFib) no end organ damage; BP >180/>120mmHg, lower BP w/n 2-3 days; PO ANGINA PECTORIS: CCS CLASSIFICATION
-PR interval til QRS drop after 3 or 4 P waves(benign) Ventricular Tachycardia Bizarre, wide QRS,no P waves, R >100 meds I Ordinary PA does not cause angina
Type 2 (Mobitz II) (VTAC) II Slight limitation of ordinary activity DUKE CRITERIA: INFECTIOUS ENDOCARDITIS
-prog PR interval w/ unexpected QRS drop Hypertensive Emergency: (2 major; 1 major & 3 minor; 5 minor)
III Marked limitation of ordinary PA
3rd Degree (complete heart block) Presence of changes in sensorium, papilledema or heart failure; lower MAJOR:
P Wave IV Inability to carry out any PA w/o discomfort
no relationship bet P waves & QRS BP w/n 24 hrs; IV meds 1. (+) Blood culture
Upright in Leads I, II a. Typical microorgs for IE for 2 separate blood cultures: viridians
PR interval <0.12 sec..eval (WPW)
Negative in aVR
<3 small squares in duration CA drip KILLIP CLASSIFICATION OF MI strep, S. bovis, HACEK grp, S. aureus, or community acquired
2amps apresoline+2amps clonidine in 500cc D5W @ CLASS I No signs of pulmonary or venous congestion enterococci in the absence of primary focus
<2.5 small squares in amplitude b. Persistently positive blood culture, defined as a recovery of a
QRS Q wave in V1 V2 V3 (Infarct) 10ugtts/min,then titrate by increments/decrements of 0-5% mortality
Best seen in Leads II microorganism consistent w/ IE frm: blood culture drawn >12H
Q wave in III, aVR (Normal) 5ugtts/30mins to maintain BP 140/90mmHg CLASS II Moderate heart failure w/ bibasal rales, S3 gallop,
tachypnea, or signs of R heart failure incl venous & - all of 3 or a majority of 4 or more separate blood cultures
R Atrial Enlargement w/ 1st and last drawn at least 1H apart
ST segment hepatic congestion
Depression ischemia
Tall (>2.5mm) pointed P waves Grading of Murmur: 10-20% mortality - single (+) bld culture for C. burnetti or phase I IgG Ab titer> 1:800
Elevation infarction 1 faintest murmur CLASS III Severe heart failure, rales >50% of the lung fields 2. Evidence of endocardial involvement (+) 2D echo
L Atrial Enlargement 2 soft but readily audible or pulmonary edema
Myocardial Infarction Prominent terminal P negativity (biphasic) in Lead V1(P terminal 3 prominent murmur, loudest without thrill 30-35% mortality MINOR:
Anterior wall infarct V1V2 force) 4 loud murmur with a palpable thrill CLASS IV Shock w/ systolic pressure <90mmHg evidence of 1. Predisposing heart condition or injection drug use
ST Lateral wall infarct V3V4 Duration > 0.04sec, depth >1mm 5 murmur audible with a portion of diaphragm off the chest peripheral vasoconstriction, peripheral cyanosis, 2. Fever >38C
Inferior wall infarct V5V6, I, aVL Notched/bifid P wave (P mitrale) in Limb Leads w/ the inter-peak 6 murmur audible with stethoscope held off the chest mental confusion & oliguria 3. Vascular phenomena: Major arterial emboli, septic pulmonary infarcts,
Posterior wall infarct V1V2, large R wave Duration >0.04sec(1mm)
85-95% mortality mycotic aneurysm, intracranial hge, conjunctival hge, Janeway lesions
Lateral wall l,V5,V6,aVL TROPONIN Levels INTERPRETATION
Inferior wall ll,lll,aVF Short PR Interval 4. Immunologic phenomena: GN, Oslers nodes, Roths spots, RF
<0.10 Negative 5. Microbiologic evidence: + blood culture or serologic evidence of active
Anteroseptal wall V1-V3 WPW(Wolf Parkinson White) Syndrome
0.10-0.63 Borderline infection w/ organism consistent w/ IE
Ant. & anteroseptal wall V3 0.61-1.53 Significant
Anterior wall V2-V4 QRS Complexes
>1.50 Positive
Posterior wall V1,V2 Nonpathological Q waves are often present in leads I,III,aVL,V5,V6 HACEK: Haemophilus species, Actinobacillus actinomycetemcomitans
Anterolateral wall l, aVL,V4-V6 The R wave in Lead V6 is smaller than the R wave in V5 Cardiobacterium hominis, Eikenella corrodens, Kingella kingae
The depth of the S wave, generally, should not exceed 30mm
Ischemia T wave inversion Pathological Q wave >2mm deep and >1mm wide or >25%
Hyperkalemia tall,peak T wave,flat P wave, wide QRS amplitude of the subsequent R wave
Hypokalemia flat T wave, v waves, u waves taller than T
Obstetrics IVF for prepartum (augment): D5LR 1L + 10u oxytocin to run at 5-
10ugtts to titrate to good uterine contractions
N ursery
Normal CBG: 60-140 Fast drip: 10cc/kg
IV rate/kg/H= IV rate in cc/H weight
TOD Pls admit to NICU under the service of Dr
Pregnancy 9 months/280days/40weeks IVF for postpartum: D5LR 1L + 10u oxytocin to run at 30ugtts/mi
BW TPR q15mins until stable
Bilirubin level: all values 17.1 IV set
& dc if with minimal bleeding Start phototherapy if w/ value 15 Enteric fever- soluset
BL Breastfeeding AGE/Dengue- macroset
Tetanus toxoid HC Labs: WBC 20,000, start meds
TT1-20wks AOG TT3-6mos TT5-1yr Diabetic Screening CC CBC APC NBS @ 24H old DEHYDRATION
TT2-1moAOG TT4-1yr AG BT w/ Rh typing IT ratio: stabs/juvenile total neutrophil = 0.2 infection
TB Classification Deficit <10kg(10-10.9) >10kg(11 & )
P IV Fluids
renatal ff-up
D
(OGTT 100Fever
engue grams) I
AS MMUNIZATION Meds: CLASSIFICATION
Mild (30-50) OF ASTHMA BY LEVEL OF CONTROL
50 30
FBS
2-7 days 105
fever,leucopenia, (+/-)thrombocytopenia,no95mg/dL
change in hct Temp BCG Terramycin ophthal ointment OU (GINA
<28wks q4wks Retic
Classcount= actualExposure
hct 0.40(desired
PPD hct)xSSxretic ct CXR Moderate (60-90) 100 GUIDELINES) 60
Na+ K+ Cl- Lactulose,etc Dengue
1H Grading: 190 180mg/dL <1yoVit K 1mg IM if no scar, rpt BCG
>28wks q2wks 1-fever, >1yoHep B vaccine if0.5ml IM yet, test for PPD,
no BCG I TB exposure N= 1-1.5
+ - - - Severe (100) 150 90
D5LRqwk 130 4 109 28 2H 165 155mg/dL Partly Uncontrolled
37wks (+)TT,platelet(100,000),hematocrit(20%) SO: If (-),give BCG II TB infection 1 hemolysis
+ + - - Characteristics Controlled Controlled
D5 0.3NaCl 51 51 3H 145
easy bruising
140mg/dL
OBAOG Routine newborn careIf (+), dont give BCG III TB disease <1 bone
+ marrow+failure + + Mild DHN: D5 0.3NaCl
# of days D5 0.45NaCl
0.14=1/7 75 75 Antibiotic
IV TB inactive + + - + Moderate DHN: D5LR(all,of D5
the ff) (any measure
0.3NaCl present
2-grade 1 symptoms + spont bleeding hemorrhages PAOGHepa B vaccine Gastric lavage FT PT
in any
D5 0.9NaCl
0.28= 2/7 154 154 Severe DHN: D5LR 1/3, D5 0.3 NaCl 2/3 week)
3-grade 2 + thread pulse,pulse pressure (20mmHg) Suction secretion
1st dose: at birthprn <7days old q12H <14do q12H
D5NR0.42= 3/7 140 5 98 50 R BS (50grams) hypotension MBT Thermoregulate
2nd dose: 6wks@(1month
36.5-37.5C& 2 wks) Daytime Sx None > 2x/wk
PPD>7days old q8H(volar area of >14do
D5IMB 0.57= 4/7 25 20 22 23 1H <130mg/dL
4-grade 3 + profound shock,(-)BP, (-)pulse BBT Daily
3rd cord
dose:care
14wksw/ 70%
(3mosIPA& 2wks) subcutaneous forearm)q8H
encircle Computation Sample (2x(DHN):
or </wk)
D5NM 0.71= 5/7 40 13 40 16 5 Tu or 0.1ml 7kg, moderately
Limitation of dehydrated,
none fast drip=70cc
any
Mat hx Hepa Watch out for tachypnea, tachycardia,alar flaring,
B (+) mother:
0.86= 6/7 * RBS/OGTT at 24-28 weeks,DHF
the soonest time if w/ hx of DM in the
Blood Products Retractions
If baby (-), vaccinate at least 12H of birth w/ HepBIg Intravenous
Day 1 = Fluid:
time & date 48 & 72 hrs activities Wt x 100 = 700 4 = 175
175-70cc(FD) = 105 D5LR
3 or more
AOG by LMP family FWB 20ml/kbw blood loss >25% Refer prn B vaccine
& Hep >20kg <20kg Nocturnal none any x 2H features of
175 x 3 = 525 8H = 65-66cc/H D5 0.3NaCl
partly x 8H
D eficits # of days in mos LMP, result + succeeding days hct 20% MMR PPD (+) if: D5LR D5 0.3NaCl sxs/awakening
ORS
Divide by 7 *2+ more values 1st dose: 15mos old 6-10mm
Maint: wheal D5NM D5IMB Need for None > 2x/wk controlled
PRBC 10ml/kbw blood loss <25% <2y0 50-100ml
AOG byNa+:
UTZ135-150mEq/L or 3-4mEq/kg/day
FFP 15ml/kbw prolonged PT (2x) N ewborn (Final Dx) 2nd dose: 4-6years 5mm= close to TB px w/ clinical or xray TB;Immunocompromised reliever/
2-10yo
(2x or </wk)
100-200ml
asthma present
in any week
Na+Result of AOG
def (mEq)= in UTZ(in
(desired days) +no.
140-actual)x of days from date
TBW Cryoppt 1unit/5kg prolonged APTT >50sec Full term
Rotavirus
(_wks)vaccine:
PA, _kg xAGA,
2 doses,
cephalic
givenvia
<6mos
NSVD, old live Bb Girl, AS 10mm= <4yo
*Maintenance IV rateor w/
(wtmedical
x cc/kg conditions,
24H) exposure rescue tx
>10yo as many as they want
of Where TBW (L)= 0.6x body wt(kg) 9,10. N. sepsis, uninvestigated
- Lessen
physiologic
severity
jaundice
of AGE 15mm= 4yo0-3 or older w/o risk75cc/kg
factors Lung function Normal <80%
UTZ up to date of consult 10sec N 4-10 100cc/kg
Urine Output (N: 1-3cc/kg/H) predicted or
EDC K+: 3.5-6mEq/L 1st day or
of 2-3mEq/kg/day
LMP + 7 days 20sec control 1st 2 mos: 3 (IRP)11-20
Aminosteril
IPV: given
(dose=
on 0.5g/kg
months Feb-June
by 0.5/day,max 3g/kg) 75cc/kg personal
Mos(mmol)=
of LMP desired-actual
3mos Platelet conc 1unit/7kg plt <50,000 + bleeding Last 4 mos: 2 (IR)21-30 UO= total urine output weight
K+ def x 0.3 x wt(kg) or = wt x dose x 100 24H = __cc/H 60cc/kg best
yr of LMP += 1wtyear plt <20,000 # of Hrs admitted or IV inserted
(kg) x 50 x estimated % def PPV: pneumococcal
6(standard)
polysaccharide vaccine 31-40 50cc/kg Exacerbation none 1 or >/yr
Vit K 1mg/kg max of 10mg/amp OD x 3 Lung function 41-50 :<80% predicted Based on BSA
40cc/kg
TimingEstimated
from ovulation=last ovulation + 267days IV 2kg=give 1mg Exacerbation :1 or more /yr ABG
BSA= Height(cm) x weight(kg)
COMPUTATIONS
K def
<2kg=give 0.5mg
IVF:
>Vaccination
TFR x wt of 24H preterms
+ 20% is(ifineffective
w/ phototherapy)
due to underdeveloped organs. N ewborn: I. 3600 PaCO2= 713 (FiO2)-pCO2/0.8
K+ serum level Estimated def >2TFRlive xvaccines
wt 24H ofsame
feeding
route aminosteril
(parenteral) should be given with OFI=
Timing3-3.5mEq/L
from quickening 5% approx 200-400mmol(0.05) minimum interval
(use thisofformula
4 weeksifw/dueAminosteril
to presence&offeeding)
circulating antibodies
Age IV rate II. BSA x 500 + UO pO2/I
a/AO2=
16-18wks AOG multipara
2-2.5mEq/L 10% (0.1) that
e.g.may
wt=3kg
affect TFR=80
the live vaccines given less than 4wks interval. G ood X-ray film
0-1 day old 80cc/kg/24H III. = tot UO BSA
MIO 24H
FiO2= O2 reqt/II + pCO2/0.8
18-20wks AOG primipara
1-2.0mEq/L 20% (0.2) Typhoid Fever >Inactivated vaccines
80x324+20%=12
can be givenoranytime.
2
5-6 anterior3 ribs
90
good inspiration
100
TFR = BSA x 500 + UO (prev day)713
Ingestion of contaminated food & water 80x3=240 x 0.2 =48, next Room air: 0.21
Height *1
of the 9-10 posterior
4 ribs 110 Oliguria= <1cc/kg/H
KClFundus
vial = 2mEqs/ml High grade fever >5 days 240+48= 288 24H = 12cc/H + diaphragm 5 120
1L=0.24 O2 reqt:
12 wks *1 NaCl vial
above sp
= 2.5mEqs/ml Headache, variable abdominal pain 1st 24H D10W,then 2L=0.28 COPD/BA=60
6 130
16wks halfway bet sp & umbilicus D10IMB CT Ratio 7 140
B
3L=0.32
lood Transfusion <60=80
20wks umbilicus IgM IgG D5IMB 4L=0.36
FFP 10cc/kg usually >60=140-age
28wks 6cm above umbilicus 8 diameter widest
Widest cardiac thoracic diameter
150(max) 5L=0.40
(Typhoid fever) + - Acute infection N: up to 0.5 PRP in 2H depending on the calculated weight
36wks 2cm below xiphoid + + Recent infection HBsAg reactive mother: give HB Ig 0.5ml deep IM w/in 12H of life F eeding 6L=0.44
PC PF ratio: 300-400
40wks 4cm below xiphoid - + Equivocal; past/ *CRP at 24hrs old, BCS anytime after birth 1cc Q3H, increase by increments of 1cc thereafter 7L=0.48 PF: pO2/FiO2
(Enteric fever) Recent infection *Allowable amount of blood for extraction in preterms: = wt x 80 x 0.10 8L=0.52
(10%) 9L=0.56 TV=wt x age
10L=0.60 BUR=18-20
FiO2=100%
PFR=40-60
Face mask=O2-1x10
Normal Values:
pH=7.35-7.45
pCO2=35-45
pO2=80-100
HCO3=22-26mEq/L
BE=2mEq/
O2 sat= 97%
INTUBATION Neuro Notes STAGES OF DIABETIC NEPHROPATHY DETSKY et al GOLDMAN et al
Indication: I hyperfiltration (GFR)
pCO2 >50
SOL CRANIAL Nerves II incipient stage (microalbuminuria) MI in previous 6mos 10 Age >70 3
pO2 <60 Mannitol - cellular III overt stage (macroalbuminuria) MI>6mos previously 5 MI in prev 6mos 11
I intact sense of smell
acute pulmonary edema Steroids- vasogenic II ROR, papilledema, IV azotemia (crea) CCS A (Angina) Important AS 3
shock PERLA V ESRD Class III 10 Rhythm other than sinus or PACs
Problem: apnea, dyspnea, (-)BP, CP arrest, LOC III,IV,VI intact EOMs Class IV 20 On last preop ECG 7
- Hyperventilate patient now M eds Indications V (+) corneal reflex
CHILD PUGH CLASSIFICATION Unstable angina in previous 6mo 10 >5 PVC/min at any time b4 OR 7
- Diazepam 5mg ivtt now Ciprofloxacin VII (-)facial SCORE I Bilirubin=<2mg/dL Alveolar pulmonary edema w/in pO2 <60 or pCO2 >50; K<3 or
- Intubate patient now For cystic fibrosis Albumin=>35g/L 1wk 10 HCO3 <20;BUN >50 or or crea>30;
asymmetry
- Suction secretions now Prone to recurrent pseudomonas infection VIII (-) hearing loss PT=4sec,INR=<1.7 Newer 5 Abn AST, signs of chronic dse, or
- Attach to cardiac monitor & pulse oximeter Imepenem Ascites=none Suspected critical AS 20 Bedridden from noncardiac causes 3
IX, X (+) gag reflex
B URCH - & WARTOFSKYS
Insert NGT & foley DIAGNOSTIC
catheter CRITERIA FOR B acteremia :
Not recommendedpresence of bacteria
for CNS in the blood as evidenced by
infection XI can shrug shoulder
C omputations Hepatic enceph=none A CTRAPID
Rhythm SLIDING
other than sinusSCALE
or PACs on INSULIN DRIPintrathoracic, or Aortic
Intraperitoneal, 3
THYROID- STORM
Attach to VR w/ following set-up Inhibits GABA(+)bld culture SCORE II Bilirubin=2-3mg/dL HGT
Last preop ECG ACTRAPID 5 PNSS 250 mLoperation
Emergency + 50u Humulin R (cmc 0.2u/mL) 4
VR Set-up Meropenem Albumin=30-35g/L
Na def: desired- actual x 0.6 x wt >5 PVC/min at any <160
time b4 OR No coverage 5
Thermoregulatory FiO2dysfunction
100% S epticemia: presence
Less seizure of microbes & their toxins in blood
reported 2 PT=4-6sec,INR=1.7-2.3 Poor gen. med. 161-200
Status 3 units 5 Class
FBSI 0-5 pts Low risk
TemperatureTV 400-500 CNS Effect NaHCO3 = 1-2mEqs/kg Ascites=easily controlled Age >70 201-300 5 5 Class II Full
6-12diabetic diet 1800kcal/day
Intermediaterisk
in 3 meals + 2 snacks
Hepatic enceph=minimal
37.2-37.7C
VUR 5 20
37.8-38.2PFR 1040
Absent -
Mild -
0
10
S IRS 2 or more of the ff. conditions: Corrected Na: Na + 1.6
SCORE III
(glucose mg/dL-100)
Bilirubin5mg/dL
100
Emergency operation
301-400 7 10 Class III Diabetic
13-25 diet: 1800kcal
snacks;
Highinrisk
3 equal feedings including 2
Paracetamol
1. not given
Fever (oral<1mo
temp >38C 401-500 9 Class IV >26 no source ofHigh simple
risksugar
38.3-38.8ACmode 15 Moderate - 20 Albumin=>30g/L CBG TID premeals
Ambroxol2. not given <1yo
Tachypnea (>24) *<15 points >500
low risk 10
38.9-39.3 20 Delusion Ibuprofen PT=>6sec,INR=>2.3
HCO3 def: desired (24)-actual x 0.4 x wt >15 points high risk Triglycerides
E XTUBATION
39.4-39.9 (dislodged)
25 Psychosis Iterax
3. Leukocytosis (12,000/uL), leucopenia (<4000) or 10%
not given <2yo Ascites=partly
2 controlled H UMULIN R SLIDING SCALE Low fat diet
->40C PAI- w/ 30 1 neb salbutamol now Extreme lethargy Antamin bands; may have a non-infectious etiology Hepatic enceph=advanced Lipanthyl 160mg/tab OD
- Extubate patient now Severe(sz,coma) - 30 Salbutamol CLASS
Plasma A 5-6(mOsm/L):
osmolality CLASS C 10 ABOVE L HGT
EE et al ACTRAPID
<160 No coverage
-
GI-Hepatic Suction secretions thoroughly
Dysfunction S EVERE SEPSIS: Sepsisrecommended
Cetirizine w/ 1 or more signs of organ dysfunction
for <1yo CLASS B 7-92(Na+K)+ SEVERE OF 7 OR+MORE
BUN(mg/dL) RBS_ decompensated Intrathoracic, intraperitoneal,or
161-199 3 units
Uric acid
- Attach to 6Lpm O2 via face mask
Absent 0 1.
Muconase/salinaseCV: arterial SBP <90mmHg, or MAP <70mmHg that 2.8 18 Infrainguinal vascular sx 1 Low purine diet
-
-
PAIModerate
w/ 1 neb salbutamol
Rpt ABGDiarrhea,
30 mins after
N/V,extubation
abdl pain
15
2.
responds to administration of IV fluids
Renal:
NST UO <0.5ml/kg/hr for 1 hr despite adequate fluid
- <6mos
E N: 280-300mOsm/L
STIMATED CREA CLEARANCE (mL/min)
Hx of IHD
Hx of CHF
200-249
250-299
4
5
1
1
Allopurinol 300mg/tab OD
- Chest xray post intubation
Severe(jaundice) 20 Crea
H2O def:clearance
Na-140 = 140-age x wt(kg) Insulin tx for DM 300-349 6 1 SGPT w/ symptoms
resuscitation
ANST - >6mos
- Standby intubation set 72 male x s. crea(mg/dL)
140xTBW *0.4 female*or 85 female s. crea >2 350-399 7 1
3. Respiratory: PaO2/FiO2 <250 or if the lung is the only Livolin forte
CV Dysfunction dysfunctional organ *0.5 male Hx of CVD 400-449 8 1 Godex
CVP (N: 8-12mmHg H20)
Tachycardia Normal: 100-125mL/min(male)
4. Platelet: Glasgow
Plt ct <80,000/uL or 50% dec in plt ct from
Coma Scale 450-499 10 Essentiale
: auscultate 99-109 5 85-105mL/min
Anion gap: Na (Cl+HCO3) (female) *0-1 low risk
Eye highest value recorded
Verbalover previous 3 days Motor >500 12
(+) crackles: give furo now w/ BP precautions 10 Opening 50-80=renal impairment 2 intermediate risk
110-119 5. Unexplained metabolic acidosis: pH <7.30 or Activitybase N: 10-12 mmol/L Albumin
120-129 15 Non-intubated
deficit >5mEq/L and plasma Intubated
lactate level >1.5x upper 10-50=CRI INSULIN3 or SLIDING
more pointsSCALE
high risk Req 50cc 25% HA;transfuse once
S PUTUM 130-139 20 4
Spontaneous
5 Oriented &
limit of mmol
talking
5 seems able
talk
6 verbal
command
5-10=CRF HGT ACTRAPID HUMULIN R Available
Sputum graded GS,>140 proceed to CS if epithelial cells
25 <10/Hpf & <5=uremia <160 No coverage
PMNs >25/Hpf CHF (good specimen)
6.
3 verbal
stimuli
Adequate
pressure
fluid resuscitation:
4 disoriented &
talking>12mmHg or cvp >8mmHg
pulmonary artery
to
wedge
5 localizes D OPAMINE DOSE
161-199 3 units 2
Or
Moriamin cap OD
*include KOH Absent
& AFB x 3 determinations 0 pain Dopa (single dose) Renal
Aminoleban sachet
Mild(pedal edema) 5 SEPTIC SHOCK 3 inappropriate
2 painful 3 4 withdraws 1-3mg/kratio:
BUN/crea x wt 200-249 4 4
Aminovita cap OD
250-299 5 6
P neumothorax Moderate(bibasal rales) 10 Sepsis w/ hypotension
stimuli words(arterial BP 90 0rquestionable
40mmHg less thantopxs
abilityresuscitation
to
13.3 BUN: mmol/0.356
300-349 6 8 Na
Severe(pulmonary
(1 diameter of hemithorax) x 100 edema) 15 normal BP) for at least 1 hr despite adequate fluid or pain
need Dopa (double dose) Crea:
Inotropic
mmol/88.4
talk 350-399 7 10 PNSS 1L + 1 vial (30meqs) NaCl
AF Absent 0 for vasopressors to maintan SBP 90 or MAP 70mmHg 3-5mg/k x wt >20 pre-renal
Diameter of pneumothorax
>15% - significant Present 10
1 no
response
2
incomprehensibl
3
decorticate 26.6 <5-10 intrinsic renal 400-499 9 12& refer Rapid K Replacement
Dopa (single dose)- adrenergic >500 10 -In a soluset, incorporate 10mEq KCl + 90cc PNSS x 1H x 3cycles
Precipitant history R EFRACTORY SEPTIC
e
SHOCK
words
(flexion)
5-8mg/k x wt -rpt s. K after last cycle
Negative 0 Septic shock that lasts for >1H & does not respond to fluid or pressor 13.3 GLUCOSE INSULIN DRIP ( Na) *Incorporate 20mEqs KCl to present IVF x __bottles
Positive 10 administrator 1 vial D50 in 10u actrapid or humulin R x 1H x 2/3
SCORE: cycles
45 0r > - thyroid storm
25-44 impending storm MODS Rpt K often last cycle HYPERKALEMIA
Dysfunction of more than 1 organ requiring intervention maintain Nondiabetic:
<25 unlikely to represent thyroid storm Calcium gluconate 1 amp slow IVTT c/o
homeostasis D5W 50cc + 10u regular insulin to run for 1H
Rpt K 2H after last cycle
BLOOD CS: No K containing IVF BLADDER TRAINING
No fruits in diet Clamp foley catheter for 2H then release for 30mins or anytime if
Hgt now, then G1 drip is done w/ sensation to void.
NaHCO3 25 x 1 tab tid
Albumin:
Request 50cc 25% human albumin, transfuse once available or
Drips Metabolic Syndrome Gram Stain Results
1.Abdominal obesity
Moriamin cap OD or aminolevan sachet or aminovita cap OD M >102cm(>40inch) NORMAL: Numerous epithelial cells seen no PMNs with or without
Dopa drip: F >88cm(>35inch) large Gram (+) bacilli.
ALBUMIN TRANSFUSION 200mg dopamine + 250cc D5W x 10ugtts/min to titrate by 2.Triglycerides >1.7mmol/L (>150mg/dL)
3.HDL
Transfuse albumin w/ incorporation of furosemide 20mg per 50cc of increments/decrements of 5 ugtts/min to maintain BP >90/60mmHg NORMAL: Few epithelial cells seen less than 20 PMNs/hpf, no
albumin to run for 6H M <1mmol/L(<40mg/dL) organism seen
F <1.3mmol/L(<50mg/dL)
Dobutamine drip: 4.BP 130/85mmHg
Dobutamine 250/amp + 250cc D5W at 10-60 ugtts/min CANDIDIASIS: Numerous epithelial cells seen, PMNs with or without
5. fasting glucose >6.1mmol/L(>110mg/dL)
HGT CONVERSION large gram (+) budding yeast cells with or without pseudohyphae
Mg% mmol (result x 0.055) Levophed/Noradrenaline drip:
Mmol mg% ( 0.055) 2 amps levophed + 250cc D5W at 15-60 ugtts/min to titrate by Appendicitis (Alvardo Scoring) BACTERIAL VAGINOSIS: Numerous epithelial cells seen few PMNs
Migrating R iliac fossa pain 1 and clue cells.
increments/decrements of 5ugtts/min to maintain BP >90/60mmHg
Nausea & vomiting 1 ( Clue cells epith cells covered with small gram (-) rods.)
DOSE reqt of Platelet Anorexia 1
Conc/kg BW Nicardipine drip: MIXED GONOCOCCAL & CHLAMYDIAL INFXN: Numerous
R iliac fossa tenderness 2
iU/10 kg BW 20 mg conc Nicardipine in 250cc D5W PMNs and gram (-) intracellular diplococci
Fever >37.8C 1
Rebound tenderness R iliac fossa 1
PREmedication (30min 1H prior BT) Cordarone drip: Leukocytosis >10,000 2
Paracetamol 300mg/IVTT 4 amps Cordarone in 250cc D5W x 24H *Patient has gonococcal cervicitis, this patient should also have non-
Neutrophilic shift to L >75% 1
Solucortef 50mg/IVTT gonococcal cervicitis, that is mixed gonococcal and chlamydial
10
Benadryl 25mg/IVTT Piracetam (Nootropil) drip: infection
Or 12 gm/vial x 24H
Paracetamol 500mg/tab
Prednisone 20mg/tab NON-GONOCOCCAL CERVICITIS but could still have
AC drip: gonococcal infection: More than 20 PMNs but no gram (-) intracellular
Benadryl 25mg/tab
Apresoline 20mg/amp, 2 amps + Clonidine 150mg/amp, 2 amps in diplococci
250cc D5W to run initially at 5 ugtts/min to titrate by increments/
HYPERSENSITIVITY RXN/ ANAPHYLACTIC SHOCK: decrements by 5 ugtts/min to maintain BP <150/90 mmHg
0.2cc of 1:1000 SQ now; 0.3 of 1:1000 SQ now
Heparin drip:
10,000 u Heparin + 250cc D5W via soluset to run at 10-20
H. pylori (+) Ulcer Treatment ugtts/min via infusion pump
PPI bid x 1 week
+ Streptokinase drip:
Amoxicillin 500mg/tab, 2 tabs bid x 1 week or 1,500 u Streptokinase + 90cc PNSS in a soluset to run x 1H
Metronidazole 500mg/tab, 1 tab bid x 1 week
+ Amiodarone (Cordarone) drip:
Clarithromycin 500mg/tab, 1 tab bid x 1 week 150mg/3ml of Cordarone, 5 amps in 500cc D5W x 24H
Aminophylline drip:
Aminophylline 250mg/amp + 250cc D5W at 15-40 ugtts/min
LD: 5mkbw in 30 ml D5W in a soluset
M: 0.4-0.8 mk/H
You might also like
- Substance Abuse Counseling Complete 5th EditionDocument379 pagesSubstance Abuse Counseling Complete 5th Editionnintendoagekid86% (59)
- Derma MegatableDocument21 pagesDerma MegatableCoy NuñezNo ratings yet
- Basic Reconnaissance Course Preparation GuideDocument6 pagesBasic Reconnaissance Course Preparation GuideJohn Leclair100% (1)
- Acute Medicine: Shock: Inadequate Tissue and Organ PerfusionDocument3 pagesAcute Medicine: Shock: Inadequate Tissue and Organ Perfusionmyat252No ratings yet
- JI RevalidaDocument61 pagesJI RevalidaAren LingadNo ratings yet
- New Intern Guide Quick NotesDocument8 pagesNew Intern Guide Quick NotesTrisNo ratings yet
- Ancient Indian Medicine Systems OverviewDocument11 pagesAncient Indian Medicine Systems OverviewAmrutha AyinavoluNo ratings yet
- JI Chart OrdersDocument4 pagesJI Chart OrdersMel BillonesNo ratings yet
- Notes ImDocument5 pagesNotes Imsharmee sarmientaNo ratings yet
- Review Slides OphthaDocument14 pagesReview Slides OphthaSUSHMITA MAE ROSE CONTRERASNo ratings yet
- Cheat Sheet (Draft)Document3 pagesCheat Sheet (Draft)bonziebuddyNo ratings yet
- MediterraneanDocument39 pagesMediterraneanJeff Lester PiodosNo ratings yet
- (Warding) Guideline 1 - QCGH-HISTORY - PE - GUIDELINEDocument4 pages(Warding) Guideline 1 - QCGH-HISTORY - PE - GUIDELINEHynne Jhea Echavez100% (1)
- FIRST PRENATAL VISIT CHECKLISTDocument8 pagesFIRST PRENATAL VISIT CHECKLISTNadine BacalangcoNo ratings yet
- Pedia CardDocument4 pagesPedia CardPatricia Kate RegalaNo ratings yet
- Internal MedicineDocument83 pagesInternal MedicineSumbul PNo ratings yet
- Revalida Reviewer AsmphDocument237 pagesRevalida Reviewer AsmphShey ShocNo ratings yet
- 2 0CommDiseaseIMPTVisionDocument3 pages2 0CommDiseaseIMPTVisionAndrea Patricia DaquialNo ratings yet
- 107 Rle Virtual Duty - Opd: Internal MedicineDocument6 pages107 Rle Virtual Duty - Opd: Internal MedicineGiel Margareth LindoNo ratings yet
- NYHA Functional Classification of Heart Failure and Molecular Markers in AMI DiagnosisDocument2 pagesNYHA Functional Classification of Heart Failure and Molecular Markers in AMI DiagnosisJohn Christopher LucesNo ratings yet
- Basic ECG For Refresher Course 2014Document116 pagesBasic ECG For Refresher Course 2014Winz DolleteNo ratings yet
- Medicine OSCE - Common Diseases Ver2Document4 pagesMedicine OSCE - Common Diseases Ver2TrisNo ratings yet
- Emergency Drugs: Drug Action Indications Adverse Effects Contraindications Nursing Management Atropine SulfateDocument15 pagesEmergency Drugs: Drug Action Indications Adverse Effects Contraindications Nursing Management Atropine Sulfate092109No ratings yet
- Fabella NotesDocument96 pagesFabella NotesAndrassy Twinkle AlineaNo ratings yet
- CPG PneumoniaDocument31 pagesCPG PneumoniaJo Anne100% (3)
- Spinal Cord CompressionDocument4 pagesSpinal Cord Compressionian3yeung-2No ratings yet
- SYS-3010 Syringe Pump Operation Manual - V1.1Document62 pagesSYS-3010 Syringe Pump Operation Manual - V1.1bprz50% (2)
- Waves and Intervals Heart Activity Normal/Abnormal (1 Small Box 0.04sec) (1 Big (5 Small) 0.2sec)Document6 pagesWaves and Intervals Heart Activity Normal/Abnormal (1 Small Box 0.04sec) (1 Big (5 Small) 0.2sec)Eben Ezar Dela CruzNo ratings yet
- Audits, Gap Assessments, CAPA - 0Document230 pagesAudits, Gap Assessments, CAPA - 0mgvtertv100% (3)
- Esophageal Achalasia DysphagiaDocument14 pagesEsophageal Achalasia DysphagiaTirtha Taposh100% (1)
- USMLE Flashcards: Anatomy - Side by SideDocument190 pagesUSMLE Flashcards: Anatomy - Side by SideMedSchoolStuff100% (3)
- Dementia Rating ScaleDocument2 pagesDementia Rating ScaleIqbal BaryarNo ratings yet
- Review Lectures Forlu6: Basic Eye Exam Common Opd Complaints Common Er Cases PharmacologyDocument110 pagesReview Lectures Forlu6: Basic Eye Exam Common Opd Complaints Common Er Cases Pharmacologyupmed2012block9No ratings yet
- Pediatric NotesDocument20 pagesPediatric Notestweet196% (23)
- SPJ LAS Q2 Week 1 To 5Document67 pagesSPJ LAS Q2 Week 1 To 5Lovilyn EncarnacionNo ratings yet
- IM Cardiology Samplex All-In - LDocument35 pagesIM Cardiology Samplex All-In - LDeepbluexNo ratings yet
- Anaesthesia For Medical StudentDocument266 pagesAnaesthesia For Medical Studentprevet100% (4)
- OB NotesDocument4 pagesOB NotesMaris Sarline OpenianoNo ratings yet
- Biochem Lab NotesDocument7 pagesBiochem Lab NotesTin SumangaNo ratings yet
- Trinx Product Catalog 2019 ENDocument64 pagesTrinx Product Catalog 2019 ENFernando BlancoNo ratings yet
- Patient with Eustachian Tube Dysfunction and Otitis MediaDocument5 pagesPatient with Eustachian Tube Dysfunction and Otitis MediaRenz Marion AlemaniaNo ratings yet
- Medical grading scales and assessment criteriaDocument17 pagesMedical grading scales and assessment criteriaSerious LeoNo ratings yet
- ECG - ACLS 2020 ModuleDocument68 pagesECG - ACLS 2020 ModuleRasheedAladdinNGuiomala100% (1)
- Physician Order Sheet Format GuideDocument9 pagesPhysician Order Sheet Format GuideRoland Philip GoNo ratings yet
- Approach to Dyslipidemia Based on 2015 CPGDocument26 pagesApproach to Dyslipidemia Based on 2015 CPGRenzy SalumbreNo ratings yet
- 2020 Apr Common Treatment OrdersDocument32 pages2020 Apr Common Treatment OrdersAlistair LauNo ratings yet
- Core Values of Family MedicineDocument68 pagesCore Values of Family MedicineJodene Rose RojasNo ratings yet
- TicklerDocument11 pagesTicklerJustine Issa YuNo ratings yet
- Reviewer For Pedia Osce: 10.5 KG 45.16 CM / 17.8 in 75 CM SixDocument10 pagesReviewer For Pedia Osce: 10.5 KG 45.16 CM / 17.8 in 75 CM SixJamora ManilynNo ratings yet
- Drug Dose PediatricDocument5 pagesDrug Dose PediatricPierre LaPaditeNo ratings yet
- Dem Tickler NotesDocument1 pageDem Tickler NotesSeff CausapinNo ratings yet
- Case PCAPDocument2 pagesCase PCAPNina Anne ParacadNo ratings yet
- Case Presentation: NeurologyDocument19 pagesCase Presentation: NeurologySydrex SarmientoNo ratings yet
- Eportfolio SampleDocument46 pagesEportfolio SampleJolaine ValloNo ratings yet
- Ward Census OB Ward Aug 26 DUTYDocument26 pagesWard Census OB Ward Aug 26 DUTYRobz Apacionado100% (1)
- Created by Cindy Montana at Washington University in St. LouisDocument201 pagesCreated by Cindy Montana at Washington University in St. LouisBob DaBuilderNo ratings yet
- Small Group DiscussionDocument3 pagesSmall Group DiscussionBea SamonteNo ratings yet
- Pediatric Tickler by RemDocument7 pagesPediatric Tickler by RemRem AlfelorNo ratings yet
- 2016 CPG Ent PDFDocument21 pages2016 CPG Ent PDFCamelle CelisNo ratings yet
- 01-05-21 - 01-12-21 - Fluid & ElectrolytesDocument8 pages01-05-21 - 01-12-21 - Fluid & ElectrolytesJolaine ValloNo ratings yet
- PEDIA ER FormularyDocument1 pagePEDIA ER FormularyAnonymous ic2CDkFNo ratings yet
- GYNECOLOGY Chief ComplaintsDocument3 pagesGYNECOLOGY Chief ComplaintsJennifer HerediaNo ratings yet
- Murmur EvaluationDocument4 pagesMurmur EvaluationManjunath GeminiNo ratings yet
- Pre-Op Case Protocol #4Document2 pagesPre-Op Case Protocol #4IC BNo ratings yet
- First Line Drugs by Infection and ConditionDocument3 pagesFirst Line Drugs by Infection and ConditionKeisha Dela CernaNo ratings yet
- OBGYN TransDocument6 pagesOBGYN TransanonymousNo ratings yet
- Medical Management of Postpartum HemorrhageDocument17 pagesMedical Management of Postpartum HemorrhageCatherine PingNo ratings yet
- Pedia DosesDocument7 pagesPedia DosesSai Krishna MaddiralaNo ratings yet
- Dystocia: A Case PresentationDocument63 pagesDystocia: A Case PresentationRoxanneGailBigcasGoleroNo ratings yet
- Problem-based Approach to Gastroenterology and HepatologyFrom EverandProblem-based Approach to Gastroenterology and HepatologyJohn N. PlevrisNo ratings yet
- ECG InterpretationDocument3 pagesECG InterpretationBIANCA ROMELLE STEPHANIE PAYOTNo ratings yet
- Cardiac Dysrhythmias For Heart PatientsDocument3 pagesCardiac Dysrhythmias For Heart PatientsAlaa OmarNo ratings yet
- Spinal Anesthesia Output To PrintDocument5 pagesSpinal Anesthesia Output To PrintTin SumangaNo ratings yet
- Prioritization of The Problems - Work Place VisitDocument4 pagesPrioritization of The Problems - Work Place VisitTin SumangaNo ratings yet
- ANESTHESIA: A BRIEF HISTORY AND GUIDE TO AIRWAY MANAGEMENTDocument4 pagesANESTHESIA: A BRIEF HISTORY AND GUIDE TO AIRWAY MANAGEMENTTin SumangaNo ratings yet
- Community Oriented Primary Care: Meaning and Scope: General ConsiderationsDocument33 pagesCommunity Oriented Primary Care: Meaning and Scope: General ConsiderationsShams JailaniNo ratings yet
- Anesthesia HistoryDocument1 pageAnesthesia HistoryTin SumangaNo ratings yet
- Pelvic Inflammatory DiseaseDocument4 pagesPelvic Inflammatory DiseaseTin SumangaNo ratings yet
- Placenta Previa: Case DiscussionDocument4 pagesPlacenta Previa: Case DiscussionTin SumangaNo ratings yet
- Airway Managment: Sensory - CN VDocument3 pagesAirway Managment: Sensory - CN VTin SumangaNo ratings yet
- History Taking GuideDocument6 pagesHistory Taking GuideTin SumangaNo ratings yet
- IM HXpocketguideDocument4 pagesIM HXpocketguideTin SumangaNo ratings yet
- History Taking GuideDocument6 pagesHistory Taking GuideTin SumangaNo ratings yet
- (Gastric Lymphoma) Journal ClippingsDocument3 pages(Gastric Lymphoma) Journal ClippingsTin SumangaNo ratings yet
- Anesthesia HistoryDocument1 pageAnesthesia HistoryTin SumangaNo ratings yet
- People Living With Hiv: The Gap Report 2014Document12 pagesPeople Living With Hiv: The Gap Report 2014Tin SumangaNo ratings yet
- College Entrance Exam Review Chemistry HandoutDocument6 pagesCollege Entrance Exam Review Chemistry HandoutTin SumangaNo ratings yet
- Airway Managment: Sensory - CN VDocument3 pagesAirway Managment: Sensory - CN VTin SumangaNo ratings yet
- Substance Use Disorder Fact SheetDocument2 pagesSubstance Use Disorder Fact SheetAnonymous nz9rhHNo ratings yet
- (PCFM 3-Dr. Bullo) Hiv 101Document4 pages(PCFM 3-Dr. Bullo) Hiv 101Tin SumangaNo ratings yet
- Manipulation TherapyDocument6 pagesManipulation TherapyTin SumangaNo ratings yet
- Youthful Lusts: Eyes and The Pride of Life Is NOT of The Father But Is If The World." (I John 2: 15-16, KJV)Document3 pagesYouthful Lusts: Eyes and The Pride of Life Is NOT of The Father But Is If The World." (I John 2: 15-16, KJV)Tin SumangaNo ratings yet
- (PCFM 3) Health EconomicsDocument3 pages(PCFM 3) Health EconomicsTin SumangaNo ratings yet
- Obstetrics2 High Yield Finals ReviewerDocument9 pagesObstetrics2 High Yield Finals ReviewerTin SumangaNo ratings yet
- How To Drink Orange Juice To The Glory ofDocument3 pagesHow To Drink Orange Juice To The Glory ofTin SumangaNo ratings yet
- How To Drink Orange Juice To The Glory ofDocument3 pagesHow To Drink Orange Juice To The Glory ofTin SumangaNo ratings yet
- Advances and Limitations of in Vitro Embryo Production in Sheep and Goats, Menchaca Et Al., 2016Document7 pagesAdvances and Limitations of in Vitro Embryo Production in Sheep and Goats, Menchaca Et Al., 2016González Mendoza DamielNo ratings yet
- List of 220KV Grid Stations-NTDCDocument7 pagesList of 220KV Grid Stations-NTDCImad Ullah0% (1)
- LC (Lethal Concentration) : Uji Toksisitas KuantitatifDocument31 pagesLC (Lethal Concentration) : Uji Toksisitas Kuantitatifbagi_fileNo ratings yet
- ManeuversDocument16 pagesManeuversCezar-George BadaleNo ratings yet
- Latest Requirements on Safe Lifting OperationsDocument22 pagesLatest Requirements on Safe Lifting OperationsThanThanscc100% (1)
- Progress Test 04Document6 pagesProgress Test 04Lemmy the GamerNo ratings yet
- Referralsystem 161202080450Document21 pagesReferralsystem 161202080450DRx Sonali Tarei100% (1)
- DRRM Plan2020 2021Document5 pagesDRRM Plan2020 2021SheChanNo ratings yet
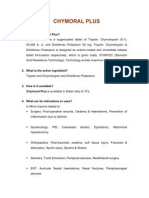
- Chymoral Plus'Document3 pagesChymoral Plus'Neha SureshNo ratings yet
- C & W Meat Packers Carly Courtney Cynthiana KY Notice of Suspension Humane Treatment LivestockDocument4 pagesC & W Meat Packers Carly Courtney Cynthiana KY Notice of Suspension Humane Treatment LivestockghostgripNo ratings yet
- RecormonDocument36 pagesRecormonShamal FernandoNo ratings yet
- Chronic Cough in Dogs: Published With The Permission of LAVC Close Window To Return To IVISDocument4 pagesChronic Cough in Dogs: Published With The Permission of LAVC Close Window To Return To IVISJuanEstebanOspinaNo ratings yet
- Anti-epileptic drugs: Types, Mechanisms & TreatmentDocument7 pagesAnti-epileptic drugs: Types, Mechanisms & TreatmentSampada ghodkiNo ratings yet
- Theoretical Models of Nursing Practice AssignmentDocument6 pagesTheoretical Models of Nursing Practice Assignmentmunabibenard2No ratings yet
- Roles and Responsibilities of UnderwritingDocument6 pagesRoles and Responsibilities of UnderwritingShubham DubeyNo ratings yet
- Essay On Current Poverty State of India After COVID-19: KeywordsDocument10 pagesEssay On Current Poverty State of India After COVID-19: KeywordsMALLI ROYALNo ratings yet
- Beddtiot ORTHO / Orthodontic Courses by Indian Dental AcademyDocument60 pagesBeddtiot ORTHO / Orthodontic Courses by Indian Dental Academyindian dental academyNo ratings yet
- Schedule - Topnotch Moonlighting and Pre-Residency Seminar Nov 2022Document2 pagesSchedule - Topnotch Moonlighting and Pre-Residency Seminar Nov 2022Ala'a Emerald AguamNo ratings yet
- Mechanical Syllabus PDFDocument225 pagesMechanical Syllabus PDFshashiNo ratings yet
- Iimplant AbutmentsDocument8 pagesIimplant AbutmentsDr. AtheerNo ratings yet
- Emergent Care Clinic StudyDocument5 pagesEmergent Care Clinic StudyAna Bienne0% (1)
- Ethical Counselling and Defense MechanismsDocument9 pagesEthical Counselling and Defense MechanismscklynnNo ratings yet