Professional Documents
Culture Documents
H1d - Microcytic Anemias Chart
Uploaded by
qselmm0 ratings0% found this document useful (0 votes)
97 views3 pagesSummary of Microcytic Anemias including iron deficiency anemia, sideroblastic anemia, and anemia of chronic disease
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentSummary of Microcytic Anemias including iron deficiency anemia, sideroblastic anemia, and anemia of chronic disease
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
97 views3 pagesH1d - Microcytic Anemias Chart
Uploaded by
qselmmSummary of Microcytic Anemias including iron deficiency anemia, sideroblastic anemia, and anemia of chronic disease
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 3
Clinical Medicine Lecture: _____ Topic: ____________________________________________________________ Date: ______________
Iron Deficiency Anemia Sideroblastic Anemia Anemia of Chronic Disease
1. Dietary Lack Not pathognomonic of any one disease Reduction in proliferation of erythroid
2. Impaired absorption Results from a lack of heme due to poor iron progenitors AND impaired iron utilization
3. Increased requirement incorporation Persistent systemic inflammation associated
Etiology 4. Chronic blood loss with chronic disease leads to impaired RBC
(Pathophysiology): o Most common cause of iron deficiency in production by triggering release of hepcidin
the Western world from the liver making iron less available and
o Internal bleeding may occur as a result of inflammation also inhibits marrow.
cancer
Most common nutritional disorder on Earth Excessive alcohol consumption
o Most common in toddlers, adolescent girls, Myelodysplastic Syndrome (MDS)
Risk Factors and women of childbearing age Mitochondrial disorders
(Demographics): Other copper deficiency, vitamin B-6
(pyridoxine deficiency), lead poisoning, drugs,
hypothermia
S/S of Anemia: S/S of Anemia: S/S of Anemia:
Pallor Pallor Pallor
Fatigue/reduced exercise capacity Fatigue/reduced exercise capacity Fatigue/reduced exercise capacity
Dyspnea on exertion Dyspnea on exertion Dyspnea on exertion
Clinical
the underlying chronic disease
Manifestations
(Signs and
Advanced Iron Deficiency: Sideroblastic Anemia S/S: Most are so mild they have no symptoms
Cheilosis/cheilitis Polyuria, blindness, deafness, optic atrophy
Symptoms):
Koilonychia (associated with DIDMOAD syndrome
Pica diabetes insipidus, diabetes mellitus, optic
Plummer-Vinson Syndrome atrophy, and deafness)
o Esophageal webs (dys/odynophagia)
1. CBC 1. CBC 1. CBC
o Hgb low o Hgb moderately low (9-10) o RBC count decreased
o Hct low o Hct low o Hgb mild to moderate decrease
o MCH, MCHC low o MCH, MCHC low o Hct mild to moderate decrease
o MCV low o MCV low o MCH, MCHC normochromic
2. Peripheral Smear and Reticulocytes 2. Peripheral Smear and Reticulocytes o MCV normocytic
o RBC Appearance microcytic, o RBC Appearance microcytic, o Neutrophilia, monocytosis, and
hypochromic hypochromic thrombocytosis due to underlying disease
Diagnostic Studies:
In severe anemia (7-8 g/dL) o Siderocytes with Pappenheimer bodies 2. Peripheral Smear and Reticulocytes
codocytosis and poikilocytosis o Basophilic stippling of the RBCs is lead o RBC Appearance normocytic,
o Absolute Reticulocytes (0.5-1.5%) poisoning normochromic (75%)
o Reticulocyte Index (1-3%) o Reticulocytes o Reticulocytes
Too few poor RBC production (not Too few poor RBC production (not Too few poor RBC production (not
enough iron) enough heme) enough heme)
3. Iron Studies 3. Iron Studies 3. Iron Studies and Other
o Ferritin low o Ferritin normal o Ferritin increased (as a non-specific
Most convenient test for estimating o SI normal inflammatory reactant)
iron stores o TIBC normal o SI decrease
o Serum Iron (SI) low o TSAT normal o TIBC increase
o Total Iron Binding Capacity (TIBC) high 4. Hemoglobin electrophoresis (probably) o TSAT decrease
o Transferrin saturation (TSAT) low o Normal o Other If these are found, then you can
4. Other 5. Bone Marrow Analysis suspect that the lever and marrow are
o Serum erythropoietin level increased o Definitive/Gold Standard necessary to affected
o RBC protoporphyrin levels increased ( find the RINGED SIDEROBLASTS C-reactive protein (CRP)
100 g/dL, normal is <30 g/dL) 6. Other Erythrocyte sedimentation rate
5. Bone Marrow Analysis o Serum lead, ethanol, copper, zinc, - (ESR, Sed Rate)
o Definitive/Gold Standard (but not glutamyltransferase, vitamin B-6 Hepcidin level
necessary) differentiation between iron Growth differentiation factor 15
deficiency and sideroblastic anemia 4. Plasma erythropoietin level
Too few sideroblasts NOT o May or may not be decreased (EPO levels
RINGED <500 mU/mL may respond to an EPO-
stimulating agent)
1. Oral iron Considerations: Preferred initial therapy is correction of the
o Indications Asymptomatic (no advanced Removal of toxic agents underlying disorder
anemia sx) patient with known iron Pyridoxine, thiamine, and/or folic acid If EPO level decreased and no malignancy
deficiency Transfusions (along with antidotes/chelation if and Hgb is <10 g/dL, then EPO (30,000 to
o Ferrous sulfate 325 mg PO TID for 6-12 iron overload develops from transfusion) 40,000 SQ once weekly) or darbepoetin (300
months (to achieve marrow iron stores of Bone marrow transplantation mcg Q 3 weeks)
0.5-1 g) o LAST RESORT o If using either, should also give
Results in absorption of 50 mg of Liver transplantation supplemental iron
elemental iron per day, which supports o Response Hgb increases 0.5 g/dL by 2-
a RBC production level of 2-3 x normal 4 weeks
o Reticulocyte count should begin to o Stop when hemoglobin levels reach 12
increase within 4-7 days after initiation of g/dL
therapy and peak at 1-1 weeks PRBC transfusion if there is insufficient time
Treatment (First & 2. Parenteral Iron for the patient to respond to above treatments
Second Line): o Indications AND symptomatic anemia
Inability to tolerate oral iron
Needs are relatively acute
Ongoing iron needs, usually due to
PERSISTENT GI blood loss
o 100 mg of elemental iron weekly x 10
weeks
3. RBC transfusion
o Indications
Symptoms of anemia
Cardiovascular instability
Continued and excessive blood loss
from whatever source and who
require immediate intervention
Referral: PRN Hematology recommended for all Not usually necessary
You might also like
- Clinical Medicine - Lecture: - Topic: - DateDocument2 pagesClinical Medicine - Lecture: - Topic: - DateqselmmNo ratings yet
- Clinical Medicine - Lecture: - Topic: - DateDocument3 pagesClinical Medicine - Lecture: - Topic: - DateqselmmNo ratings yet
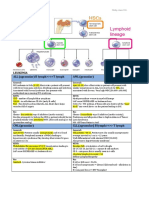
- WBC Lymph Node SpleenDocument12 pagesWBC Lymph Node Spleendr brijesh TiwariNo ratings yet
- Soft Tissue TumoursDocument8 pagesSoft Tissue TumoursGerardLum100% (2)
- Liver Function Tests Diagnostic GuideDocument2 pagesLiver Function Tests Diagnostic GuideostarburstoNo ratings yet
- RBC&WBC AbnormalitiesDocument11 pagesRBC&WBC AbnormalitiesChaineZenCorpuz0% (1)
- Diseases - BiochemDocument4 pagesDiseases - BiochemJay FeldmanNo ratings yet
- Chart - WBC DisordersDocument1 pageChart - WBC DisordersSamuel RothschildNo ratings yet
- HaematinicsDocument2 pagesHaematinicsGerardLum100% (2)
- AnemiaDocument10 pagesAnemiaBia Payawal100% (2)
- Full Blood PictureDocument1 pageFull Blood PicturejslumNo ratings yet
- Clinpath - : Red Blood CellsDocument14 pagesClinpath - : Red Blood CellsYolanda Primrosa NurhanNo ratings yet
- Acute Myeloproliferative Acute Lymphoproliferative Chronic Myeloproliferative Chronic Lymphoproliferative Plasma Cell NeoplasmDocument1 pageAcute Myeloproliferative Acute Lymphoproliferative Chronic Myeloproliferative Chronic Lymphoproliferative Plasma Cell NeoplasmAudreySlitNo ratings yet
- Abnormal LFTsDocument2 pagesAbnormal LFTsRenu RosyNo ratings yet
- Renal Chart 2Document21 pagesRenal Chart 2fortheloveofmedicineNo ratings yet
- Table of Genetic Disorders: Download A Copy of This Study GuideDocument11 pagesTable of Genetic Disorders: Download A Copy of This Study Guideerica perezNo ratings yet
- Anemia Table283Document2 pagesAnemia Table283Bridget ParkerNo ratings yet
- Table of Genetic DisordersDocument9 pagesTable of Genetic DisordersjeslymailNo ratings yet
- Week 7. Renal Pathology Continued.Document9 pagesWeek 7. Renal Pathology Continued.Amber LeJeuneNo ratings yet
- Renal Disease Guide to Glomerular and Tubulointerstitial ConditionsDocument23 pagesRenal Disease Guide to Glomerular and Tubulointerstitial ConditionsKimberly KanemitsuNo ratings yet
- Liver Function Lecture NotesDocument9 pagesLiver Function Lecture NotesMarie Bernadette DigoNo ratings yet
- ENDOCRINE PATHOLOGY WebpathDocument35 pagesENDOCRINE PATHOLOGY Webpathapi-3766657No ratings yet
- Megaloblastic Anemia Testing AlgorithmDocument1 pageMegaloblastic Anemia Testing AlgorithmkatNo ratings yet
- Pathology - Chapter 14Document14 pagesPathology - Chapter 14Cory GrayNo ratings yet
- Nephrotic Nephritic SyndromsDocument4 pagesNephrotic Nephritic SyndromsKimiwari100% (2)
- 4.1d - Pathology of The Pituitary - Nov.10 - Dr. GalangDocument4 pages4.1d - Pathology of The Pituitary - Nov.10 - Dr. GalangMiel Raphael AranillaNo ratings yet
- 19 Intro To AnemiaDocument3 pages19 Intro To AnemiaPeter JosephNo ratings yet
- Genetic and Pediatric Diseases Chapter SummaryDocument16 pagesGenetic and Pediatric Diseases Chapter SummaryJustine HungNo ratings yet
- Red Blood Cell Disorders Anemia: Anemia Is A Laboratory DiagnosisDocument3 pagesRed Blood Cell Disorders Anemia: Anemia Is A Laboratory DiagnosisAnonymous 8hJAATBNo ratings yet
- Hemolytic AnemiaDocument1 pageHemolytic AnemiaTeus FatamorganaNo ratings yet
- OPTOMED-HW2-Diabetic Retinopathy PDFDocument3 pagesOPTOMED-HW2-Diabetic Retinopathy PDFDanalie SalvadorNo ratings yet
- Small Intestine Lesions Comparison ChartDocument9 pagesSmall Intestine Lesions Comparison ChartfadoNo ratings yet
- Chronic Kidney DiseaseDocument2 pagesChronic Kidney DiseasejslumNo ratings yet
- Biochemistry Chart-Dr.G.bhanu PrakashDocument7 pagesBiochemistry Chart-Dr.G.bhanu PrakashAsadullah YousafzaiNo ratings yet
- 2021 Systemic Pathology S4T1 - RBC and Bleeding Disorders PDFDocument27 pages2021 Systemic Pathology S4T1 - RBC and Bleeding Disorders PDFAlexis Bondad100% (1)
- Leukemia and Lymphoma OverviewDocument2 pagesLeukemia and Lymphoma OverviewAyeshaArifNo ratings yet
- Pathology GlomerulonephritisDocument4 pagesPathology GlomerulonephritisGerardLum100% (2)
- Cocci Rod 4 Main Classifications: Gram Staph, Strep Bacillus Clostridium Neisseria Pleiomorphic Enterobact-EriceaeDocument2 pagesCocci Rod 4 Main Classifications: Gram Staph, Strep Bacillus Clostridium Neisseria Pleiomorphic Enterobact-EriceaeKimberly KanemitsuNo ratings yet
- Decreased Levels of Iron by Diet or Hemorrhage Impaired Heme SynthesisDocument8 pagesDecreased Levels of Iron by Diet or Hemorrhage Impaired Heme SynthesisSamuel RothschildNo ratings yet
- IKD9 - Radiological Evaluation of Renal CystsDocument26 pagesIKD9 - Radiological Evaluation of Renal CystsRenal Association MauritiusNo ratings yet
- Exam 1 DiseasesDocument1 pageExam 1 DiseasesSolomon Seth SallforsNo ratings yet
- Anemia Flow ChartDocument1 pageAnemia Flow ChartCynthiaNo ratings yet
- 7sgdfgf PDFDocument438 pages7sgdfgf PDFPratik JadhavNo ratings yet
- MHD Exam 5 MaterialDocument122 pagesMHD Exam 5 Materialnaexuis5467100% (1)
- Genetic Disorders-Www - Qworld.co - inDocument13 pagesGenetic Disorders-Www - Qworld.co - inQworld100% (1)
- Hem-Onc: AnswerDocument3 pagesHem-Onc: AnswerAman Raj KNo ratings yet
- WBC Pathology: Lecturer: Associate Professor T. A. GrekovaDocument49 pagesWBC Pathology: Lecturer: Associate Professor T. A. GrekovaFaheem MusthafaNo ratings yet
- Antivirals, Rubella, Peecorna VIRUSDocument3 pagesAntivirals, Rubella, Peecorna VIRUSErnie G. Bautista II, RN, MDNo ratings yet
- Neuro General Neuro: Proptosis/ Exophthalmos ChemosisDocument4 pagesNeuro General Neuro: Proptosis/ Exophthalmos ChemosisShakina FareedNo ratings yet
- Pathology B - Gastrointestinal Tract (Esguerra, 2015)Document18 pagesPathology B - Gastrointestinal Tract (Esguerra, 2015)Ars MoriendiNo ratings yet
- AnaemiaDocument83 pagesAnaemiadoc19019696No ratings yet
- Flash Notes SyndromesDocument8 pagesFlash Notes SyndromesschxzerrydawnNo ratings yet
- Microcytic Hypochromic Macrocytic Normochromic Normocytic: Anemia HematocritDocument7 pagesMicrocytic Hypochromic Macrocytic Normochromic Normocytic: Anemia Hematocritjjjj31No ratings yet
- Pathology Finals Reviewer on WBCs, Lymph Nodes, Spleen & ThymusDocument5 pagesPathology Finals Reviewer on WBCs, Lymph Nodes, Spleen & Thymusangel_sagun_1No ratings yet
- 15 - Toronto Notes 2011 - HematologyDocument58 pages15 - Toronto Notes 2011 - HematologyWaiwit Chotchawjaru100% (1)
- Pharmacology of EthanolDocument5 pagesPharmacology of EthanolJoshua RemonNo ratings yet
- Iron Deficiency Anemia & ManagementDocument60 pagesIron Deficiency Anemia & Managementswap58war100% (1)
- ANEMIADocument3 pagesANEMIAjessa tabanginNo ratings yet
- Anemia DM-1 - REV.Document44 pagesAnemia DM-1 - REV.abdulrahmanbelewa96No ratings yet
- Hematology - Oncology Div.: Child Health Depart.-School of Medicine University of Sumatera UtaraDocument37 pagesHematology - Oncology Div.: Child Health Depart.-School of Medicine University of Sumatera UtaracccccNo ratings yet
- PAEDIATRIC HANDBOOK GUIDE FOR COMMON ILLNESSESDocument10 pagesPAEDIATRIC HANDBOOK GUIDE FOR COMMON ILLNESSESAbdullah Al - JubairNo ratings yet
- Auoimmune Hepatitis EASL 1Document12 pagesAuoimmune Hepatitis EASL 1Ivan VeriswanNo ratings yet
- Hyperthyroidism of The Child in Abidjan Cote Divoire Retrospective Study of 27 CaseDocument5 pagesHyperthyroidism of The Child in Abidjan Cote Divoire Retrospective Study of 27 CaseArif Rahman FarisNo ratings yet
- Treat Inflammation and Allergies with Hydrocortisone Sodium SuccinateDocument3 pagesTreat Inflammation and Allergies with Hydrocortisone Sodium SuccinateJesrel DelotaNo ratings yet
- Attach 5 Falls Risk Assessment FormDocument4 pagesAttach 5 Falls Risk Assessment FormEko Wahyu AgustinNo ratings yet
- PhenylketonuriaDocument7 pagesPhenylketonuriaReham QueNo ratings yet
- Delivery and Newborn Care AssessmentDocument4 pagesDelivery and Newborn Care AssessmentNaomi RebongNo ratings yet
- Dissociative Identity DisorderDocument2 pagesDissociative Identity DisorderAnca Crețu0% (1)
- Cas 14835Document12 pagesCas 14835Sediki ZakariaNo ratings yet
- Prof. Juli Soemirat - ExtraordinaryDocument47 pagesProf. Juli Soemirat - ExtraordinaryDj ClarrioNo ratings yet
- Betel Nut Chewing and Its Deleterious Effects On Oral CavityDocument7 pagesBetel Nut Chewing and Its Deleterious Effects On Oral Cavitydwi fitrahNo ratings yet
- Depakine Chrono PDFDocument8 pagesDepakine Chrono PDFadil yousafNo ratings yet
- Heparin + PTT 10 Letters Coumadin+Pt 10 LettersDocument5 pagesHeparin + PTT 10 Letters Coumadin+Pt 10 Letterssarah8855No ratings yet
- CEFUROXIMEDocument3 pagesCEFUROXIMEGwyn RosalesNo ratings yet
- Basic Principles of Radiation OncologyDocument34 pagesBasic Principles of Radiation OncologyEstiani Ningsih100% (1)
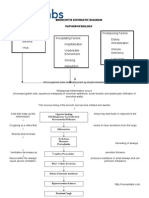
- Introduction To PathophysiologyDocument3 pagesIntroduction To PathophysiologyНадежда КравченкоNo ratings yet
- Bronchitis PathophysiologyDocument23 pagesBronchitis PathophysiologyRama Setya Bagaskara100% (2)
- Poster Daniela JercaianuDocument1 pagePoster Daniela JercaianuMadalin JercaianuNo ratings yet
- Auditing Hospital Associated InfectionsDocument59 pagesAuditing Hospital Associated Infectionstummalapalli venkateswara raoNo ratings yet
- Signs and SymptomsDocument5 pagesSigns and Symptomsasmaa hNo ratings yet
- Understanding Community Knowledge, Attitudes, and Actions Regarding Self-Medication of DiarrheaDocument80 pagesUnderstanding Community Knowledge, Attitudes, and Actions Regarding Self-Medication of DiarrheaPERO PERDANANo ratings yet
- Vaginal Hysterectomy GuideDocument5 pagesVaginal Hysterectomy Guidesensitivity23No ratings yet
- The Journal of Dermatology - 2022 - Sakamoto - T Cell Rich Perivascular Inflammation in A Case of Cutaneous VariantDocument2 pagesThe Journal of Dermatology - 2022 - Sakamoto - T Cell Rich Perivascular Inflammation in A Case of Cutaneous VariantKi IsoNo ratings yet
- Nephrotic Syndrome - Armando HasudunganDocument18 pagesNephrotic Syndrome - Armando HasudunganzahraaNo ratings yet
- Clinical Manifestations and Treatment of Osteoporotic Thoracolumbar Vertebral Compression FracturesDocument19 pagesClinical Manifestations and Treatment of Osteoporotic Thoracolumbar Vertebral Compression Fracturesmnunezh2304No ratings yet
- Osce Bank PDFDocument15 pagesOsce Bank PDFnassir197083% (6)
- DehydrationDocument19 pagesDehydrationIlyes FerenczNo ratings yet
- The Kidney: Glomerular Diseases, Nephrotic Syndrome, and Acute Renal FailureDocument11 pagesThe Kidney: Glomerular Diseases, Nephrotic Syndrome, and Acute Renal FailureElina Drits100% (1)
- Infectious Disease Epidemiology: Alick MwambunguDocument68 pagesInfectious Disease Epidemiology: Alick Mwambungumwambungup100% (2)