Professional Documents
Culture Documents
Zd-Vetm0207f 095-100
Uploaded by
Dalibor CetojevicOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Zd-Vetm0207f 095-100
Uploaded by
Dalibor CetojevicCopyright:
Available Formats
Toxicology Brief managing common poisonings in companion animals
PEER-REVIEWED
Mushroom poisoning in dogs
Rhian B. Cope, BVSc, BSc (Hon 1), PhD, DABT
M
ushroom poisoning of identification (e.g. the Oregon Poi-
companion animals, par- son Center [(800) 222-1222]) or a
ticularly dogs, is a poten- mycologist as needed.9,10
tially underestimated problem in
North America. Because of their Cyclopeptides
wandering and scavenging na- Amanita, Galerina, and Lepiota
ture, dogs seem particularly species mushrooms contain toxic
prone to mushroom poisoning.1-8 cyclopeptides. Amanita species are
While there have been sporadic the most commonly documented
reports of mushroom poisoning cause of fatal mushroom poison-
in dogs in the veterinary litera- ing in dogs,1,2,4-8 and they account
ture,1-8 anecdotal experience in for 95% of mushroom-related fa-
the Pacific Northwest suggests it talities in people.9 Amanita phal-
is more prevalent than the litera- loides, the death cap mushroom
ture indicates. (Figure 1), accounts for more than
This article summarizes the 50% of all mushroom-associated
clinical effects of the toxicologi- deaths in people and most of the
cally important mushrooms in reported fatal cases in dogs.1,2,6,9
North America. Spring, summer, The toxic cyclopeptides in these
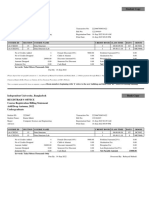
1. Amanita phalloides, the death cap
and fall are the principal seasons mushrooms are amatoxins, phallo-
mushroom, is the most common cause of
for mushroom poisoning in most potentially fatal mushroom poisoning in toxins, and virotoxins.8,9 These pep-
of North America.9 people and dogs. tides are rapidly absorbed from the
gut, and their duration of action is
IDENTIFICATION AND TREATMENT increased by enterohepatic circulation and active resorp-
Toxic mushrooms are divisible into eight groups based on tion of amatoxins from the renal glomerular filtrate. Ama-
their toxin type (Table 1).9 Six of these groups are of poten- toxins and phallotoxins are responsible for most of the
tial veterinary significance, and representative members of pathologic effects.9 Amatoxins interfere with DNA and
these groups are common throughout North America.9 In RNA transcription and, thus, selectively affect the rapidly
line with the adage, There are old mushroom hunters, replicating cells of the gastrointestinal (GI) and renal tubu-
there are bold mushroom hunters, but there are no old, lar epithelium and liver. Phallotoxins irreversibly polymer-
bold mushroom hunters, all wild-growing mushrooms ize hepatic actin filaments, triggering hepatic cholestasis.9
should be regarded as toxic until proven otherwise. Typically, 10 to 12 hours pass between consumption
Ideally, samples of the ingested mushrooms should and the onset of clinical signs.9 This delay is an impor-
be brought in to the clinic along with the affected ani- tant differential diagnostic feature of cyclopeptide inges-
mal. Do not place mushrooms for identification in a tion and is probably due to the time required for amatox-
plastic bag; instead, wrap them in a moist paper towel ins to bind to intranuclear RNA polymerase II.9
or wax paper or place them in a paper bag. Identifying There are three distinct sequential phases of cyclopep-
Photo iStockphoto.com/Tomasz Resiak
mushroom species is often complex, so consult a human tide poisoning. The initial gastroenteritis phase is charac-
poison information center with experience in mushroom terized by profuse bloody diarrhea, vomiting, nausea,
abdominal pain, dehydration, electrolyte imbalance,
Toxicology Brief was contributed by Rhian B. Cope, BVSc, BSc (Hon 1), fever, tachycardia, and hyperglycemia.9 This phase typi-
PhD, DABT, Department of Environmental and Molecular Toxicology, cally lasts about 24 hours. The resolution of clinical signs
College of Agricultural Sciences, Oregon State University, Corvallis, OR
97331.The department editor is Petra Volmer, DVM, MS, DABVT, DABT, and subclinical elevations of serum alanine transaminase
College of Veterinary Medicine, University of Illinois, Urbana, IL 61802. and aspartate transaminase activities characterize the
Veterinary Medicine February 2007 95
Toxicology Brief PEER-REVIEWED
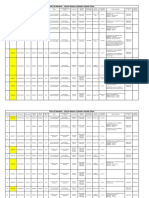
TABLE 1
Toxicologic Classification of Toxic Mushrooms
Toxin Type Relevant Species Methods of Toxicity
Cyclopeptides Amanita species (death Amatoxins inhibit RNA and DNA transcription,
caps, death angels, destroying affecting cells with the highest replication rates.
angels, deadly agaric), Galerina Phallotoxins irreversibly polymerize hepatic
species actin filaments, resulting in cholestasis.
Monomethylhydrazine Gyromitra species (false morels) Gyromitrin is converted to monomethyl-
hydrazine. Other toxic hydrazines are also
present. They antagonize pyridoxine (vitamin B6),
an essential cofactor for the synthesis of GABA.
They also directly inhibit the synthesis of GABA.
Coprine Coprinus atramentarius (ink cap) Hyperacetaldehydemia is triggered if ethanol
(alcohol) is consumed within two to 72 hours
after consuming the mushrooms. Probably
not of veterinary significance.
Muscarine Inocybe, Clitocybe, Panaeolus, Produces the classical muscarinic cholinergic
Gymnopilus, Boletus, Hebeloma, clinical signs: SLUD (salivation, lacrimation,
Mycena, and Omphalotus species urination, and diarrhea).
Isoxazole derivatives Amanita species Ibotenic acid and muscimol are psychoactive and
generally produce distortions in visual perception.
Psilocybin and psilocin Psilocybe, Panaeolus, Copelandia, The LSD-like compounds cause dysphoria,
Gymnopilus, Pluteus, and hallucinations, and sympathomimetic effects.
Conocybe species (hallucinogenic
or magic mushrooms)
GI irritants Agaricus, Boletus, Chlorophyllum, Most of the agents that trigger acute GI distress
Entoloma, Gomphus, Hebeloma, have not been identified. Idiosyncratic and
Lactarius, Naematoloma, allergic mechanisms have been proposed.
Omphalotus, Paxillus, Ramaria, Many, but not all, of these toxins are inactivated
Rhodophyllus, Russula, Scleroderma, by cooking.
and Tricholoma species
Orelline and orellanine Cortinarius species from Europe These species cause irreversible acute renal
and Japan failure; often the only effective treatment is
renal transplant.
onset of the 12- to 24-hour latent phase.9 The finaland gency upper GI decontamination (inducing emesis or gas-
often terminalhepatorenal phase of poisoning begins tric lavage) is probably not beneficial more than four
three to four days after ingestion.9 Severe hepatic dys- hours after ingestion since phallotoxins and amatoxins
function, severe renal failure, cerebral edema, icterus, ele- are rapidly absorbed from the GI tract and do not form
vated serum hepatic enzyme activities, hypoglycemia, gastric concretions or delay gastric emptying.9 Induce
coagulopathies and hemorrhage, azotemia, metabolic emesis only in asymptomatic animals because of the risks
acidosis, and sepsis characterize the hepatorenal phase. associated with this procedure.
In addition, neurologic dysfunction including hepatic en- The effectiveness of activated charcoal is unknown,
cephalopathy and coma can occur.9 Typically, the animal but its use has been recommended.9 Administer an acti-
dies three to seven days after ingestion.9 vated charcoal slurry (1 g/5 ml water) orally at a dose of
2 to 5 ml/kg in combination with a mild cathartic (sor-
Treatment. Early aggressive decontamination and bitol 3 mg/kg orally).11 Repeated doses of activated char-
enhanced elimination are critical.6,8,9 Performing emer- coal may be administered every four to six hours in an
96 February 2007 Veterinary Medicine
attempt to reduce the enterohepatic circulation of ama- verse effects, treatment can be attempted by administer-
toxins and may be of value up to 48 hours after inges- ing a loading dose of 140 mg/kg orally followed by 70
tion.9 Adequately hydrate patients treated with multiple mg/kg orally every six hours for as long as the patient
doses of activated charcoal to prevent constipation.11 Re- needs it based on clinical judgment.
peated doses of sorbitol may cause marked hypotension
or hypovolemic shock, particularly in patients with un- Monomethylhydrazine
derlying cardiovascular problems or in small patients, so Gyromitra species of mushrooms, often called false morels,
monitoring is required if repeated doses of activated vary considerably in their toxicity from year to year and
charcoal and sorbitol are administered.11 location to location. Of the several different toxic hy-
Enhanced elimination using peritoneal dialysis and drazine compounds found in these mushrooms, gy-
other methods of extracorporeal elimination has yielded romitrin is the best known.9
occasional therapeutic successes in people.6,9 Administer- The hydrolysis of gyromitrin in the gut results in the
ing parenteral penicillin G benzathine at doses greater formation of monomethylhydrazine, a GI irritant, and
than 4,300 U/kg, which subsequent gastroenteritis
displaces amatoxins from within six to eight hours
plasma protein-binding
sites making them more
The final hepatorenal of ingestion. Most cases
are relatively mild and
available for renal excre-
tion, has been claimed to
phase of cyclopeptide self-limiting; however, ex-
treme poisonings charac-
improve survival in peo-
ple.9 However, a recent 20-
poisoning begins terized by hepatic damage
have been reported in
year retrospective analysis
has demonstrated that this
three to four days people.9 Monomethyl-
hydrazine also directly in-
treatment, alone or in com-
bination with other agents, after ingestion. hibits the synthesis of
gamma-aminobutyric acid
has little efficacy.12 (GABA) within the central
Supportive care involves administering intravenous nervous system (CNS) and antagonizes pyridoxine (vita-
crystalloids, glucose, fresh frozen plasma, GI protectants min B6), an essential cofactor for the synthesis of GABA.
(e.g. kaolin/pectin 1 to 2 ml/kg orally every six to 12 The net result is uncontrolled CNS electrical activity, anxi-
hours), and broad-spectrum parenteral antibiotics to re- ety, restlessness, excitation, and seizures.9
duce the risk of sepsis. Oral supplementation or par-
enteral treatment with vitamin K1 (2.5 to 5 mg/kg daily) Treatment. Pyridoxine (25 mg/kg administered as a
and packed red blood cell or whole blood transfusions slow intravenous infusion over 15 to 30 minutes) has
may be required if bleeding is severe. been recommended as an antidote for the neurologic ef-
Silibinin dihydrogen disuccinate disodium and fects of this type of mushroom poisoning.9 Additional
acetylcysteine have been suggested as antidotes for cy- treatment consists of upper GI decontamination and
clopeptide poisoning.9 Silibinin is a semisynthetic, com- supportive care. Because of the risk of precipitating
mercialized, active derivative of silymarin, the hepato- seizures, inducing emesis in severe monomethylhy-
protectant and antioxidant mixture of medicinal drazine poisoning cases is potentially risky. Inducing
flavonolignans derived from milk thistle (Silybum mari- emesis with due clinical prudence and judgment may be
anum). Administering silibinin intravenously (20 to 50 appropriate for milder cases. Activated charcoal admin-
mg/kg/day in four doses) substantially increases the istration has been recommended, although its effective-
survival rate in people.9 Unfortunately, the injectable ness is unknown.9 Rehydration by using intravenous
form of this antidote is not available in the United States, crystalloids is the most commonly required supportive
and the poor water solubility and bioavailability of sily- treatment.9 Oral GI protectants may be beneficial. If nec-
marin may limit the effectiveness of this potential anti- essary, anxiety, restlessness, and seizures can be con-
dote when orally administered. Silipide, a complex of trolled with a benzodiazepine (0.25 to 0.5 mg/kg di-
silymarin and phosphatidylcholine (lecithin), is about 10 azepam intravenously or intramuscularly).9
times more bioavailable than silymarin, but its effective-
ness as an oral antidote for A. phalloides mushroom poi- Coprine
soning has not been investigated. The effectiveness of Coprine, the major fungal toxin associated with Coprinus
acetylcysteine for treating mushroom cyclopeptide poi- atramentarius mushroom poisoning, inhibits aldehyde de-
soning is questionable. However, given its low risk of ad- hydrogenase, thus inhibiting the conversion of ethanol (al-
Veterinary Medicine February 2007 97
Toxicology Brief PEER-REVIEWED
cohol) to acetate and resulting in an accumulation of ac- poisoning from isoxazole derivatives.9 Given the popu-
etaldehyde. This effect only occurs if there is an association lar recreational use of these mushrooms by people, it is
between the consumption of C. atramentarius mushrooms surprising that poisoning in companion animals is
and ethanol.9 If ethanol is not consumed concurrently with poorly documented.9
these mushrooms, the poisoning does not occur. Thus, this Ibotenic acid and muscimol, the principal psychoac-
poisoning is unlikely in veterinary medicine. tive isoxazole derivatives present in these mushrooms,
alter visual perception rather than cause true hallucina-
Muscarine tions in people.9 Ibotenic acid, a CNS glutamate acid re-
Muscarine is a muscarinic receptor agonist that pro- ceptor agonist, acts as a CNS stimulant; muscimol, a
duces postganglionic parasympathomimetic effects, CNS GABAB agonist, acts as a CNS depressant and seda-
such as increased genitouri- tive.9 In people, the primary ef-
nary muscle tone, bradycardia,
miosis, and salivation.9 The
Do not use the fects are periods of CNS stimu-
lation and depression that may
most common mushrooms in-
volved in muscarine poisoning correction of alternate and may manifest as
periods of manic excitement
include members of the Inocybe
and Clitocybe genera.9 Al- miosis to judge followed by periods of somno-
lence and deep sleep. Clinical
though Amanita muscaria has signs typically associated with
been classically associated
with muscarine toxicity, it con-
the atropine dose. poisoning in people include
dizziness, ataxia, euphoria,
tains insignificant amounts of this toxin.9 muscle twitches, and initial psychic stimulation fol-
Clinical signs usually occur within two hours after in- lowed by dream-filled sleep.9
gestion and are characterized by the acronym SLUD (sali-
vation, lacrimation, urination, diarrhea).9 Other common Treatment. Treatment consists of upper GI deconta-
clinical signs include bradycardia, hypotension, shock, mination and supportive measures, such as observation,
dyspnea and wheezing due to bronchoconstriction and confinement in a dark and quiet cage, and possibly seda-
increased respiratory secretions, abdominal pain, miosis, tion. Use all hypnotic drugs with caution because the
visual disturbance, and rhinorrhea.9 An alternative isoxazole derivatives potentiate their effects.9
acronym sometimes used to describe the effects of exces-
sive muscarine stimulation is DUMBBELS (diarrhea, uri- Psilocybin and psilocin
nation, miosis, bronchorrhea, bronchoconstriction, eme- Because of its popularity as a recreational drug, this
sis, lacrimation, salivation). group of mushrooms, know as hallucinogenic or magic
mushrooms, occasionally causes poisoning in dogs.3 Im-
Treatment. Performing early upper GI decontamina- portant genera involved in poisoning include Psilocybe,
tion is useful, although spontaneous vomiting may elim- Panaeolus, Copelandia, Gymnopilus, Pluteus, and
inate the need for this treatment.9 Activated charcoal ad- Conocybe.9 The principal toxins in these mushrooms are
ministration is potentially useful. The specific reversal psilocybin and psilocin, which have LSD-like proper-
agent for muscarine poisoning is atropine.9 If clinical ties.9 These compounds typically produce a transient
signs of excessive muscarine stimulation are present, ad- (less than 12-hour duration), dysphoric, and sympath-
minister atropine (0.2 to 2 mg/kg; 50% of the dose ad- omimetic syndrome. Coingestion of other drugs of
ministered intravenously and 50% intramuscularly or abuse such as LSD, PCP, and marijuana is common in
subcutaneously) slowly and progressively to effect using people and is a potentially important consideration in
the drying of the oral and respiratory secretions as the veterinary patients.9
clinical endpoints.9 Do not use the correction of miosis to Common clinical signs, which develop a half an
judge the atropine dose since by the time the pupils re- hour to four hours after ingestion, include anxiety, ag-
turn to normal, most patients have received too much at- gression, disorientation, visual hallucinations (e.g. fol-
ropine, resulting in potentially adverse cardiovascular ef- lowing and biting at imaginary flies, pointless bark-
fects.9 Intravenous crystalloids are usually sufficient to ing), weakness, mydriasis, tachycardia, and
control any hypotension that develops.9 hyperreflexia.3,9 Hypertension, hyperthermia, or con-
vulsions may occur, and patients may become coma-
Isoxazole derivatives tose in cases of extreme overdose. However, trauma
Amanita muscaria and Amanita pantherina are the princi- caused by altered behavior is usually the greatest and
pal North American mushroom species associated with most immediate threat to life.3,9
98 February 2007 Veterinary Medicine
Toxicology Brief PEER-REVIEWED
Treatment. Emergency GI de- within 24 hours. If required, sup-
contamination in a conscious pa- portive care would consist of sub-
tient poisoned by these mushrooms cutaneous or intravenous crystal-
may be difficult because of the pa- loids. The administration of oral GI
tients altered behavior and aggres- protectants could be considered
sion. An easier option may be gas- once vomiting has ceased.
tric lavage after anesthesia and
placement of a cuffed endotracheal Orelline and orellanine
tube.9 The main potential difficulty While Cortinarius species exist in
associated with anesthesia is the in- North America, no poisoning has
duction because of the dysphoric, been recorded to date.9 European
and potentially aggressive, mental and Japanese species from this
state of the patient. Prior sedation genus cause acute, irreversible
with a benzodiazepine (0.5 to 1 tubulointerstitial nephritis and
mg/kg diazepam intravenously or acute renal failure.9
1 to 4 mg/kg rectally) or an alterna-
tive induction technique, such as PREVENTION
using an induction chamber, may As with most poisonings, the best
be required. The use of induction method of controlling mushroom
chambers carries with it the in- poisonings is preventing exposure.
creased risks associated with de- This means that only those who are
creased access to the patient, so knowledgeable about mushroom
their use with dysphoric patients identification should collect wild-
requires careful clinical judgment. growing mushrooms for consump-
Treatment usually consists of tion. Dogs should be prevented
supportive care. Since the most im- from consuming mushrooms or
mediate concern is preventing acci- roaming when they are being exer-
dental trauma, often the most suc- cised. As with most poisonings,
cessful supportive care is placing the prompt upper GI decontamination
animal in a quiet, dark, padded cage and supportive care are critical ele-
in the presence of its owner.9 Warn ments of treatment.
the animals owners and handlers of
the potential for aggressive behavior. REFERENCES
1. Bernard MA. Mushroom poisoning in a dog. Can Vet J
If sedation is required, a benzodi- 1979;20:82-83.
azepine (0.5 to 1 mg/kg diazepam 2. Cole FM. A puppy death and Amanita phalloides. Aust Vet
J 1993;70:271-272.
intravenously or 1 to 4 mg/kg rec- 3. Kirwan AP. Magic mushroom poisoning in a dog. Vet
tally) can be administered. Rec 1990;126:149.
4. Naude TW, Berry WL. Suspected poisoning of puppies
by the mushroom Amanita pantherina. J S Afr Vet Assoc
GI irritants 1997;68:154-158.
5. Ridgway RL. Mushroom (Amanita pantherina) poisoning. J
Numerous mushroom genera are GI Am Vet Med Assoc 1978;172:681-682.
irritants (Table 1).9 For the most part, 6. Tegzes JH, Puschner B. Amanita mushroom poisoning: effi-
cacy of aggressive treatment of two dogs. Vet Hum Toxicol
the toxic principles involved are un- 2002;44:96-99.
known,9 although idiosyncratic and 7. Yam P, Helfer S, Watling R. Mushroom poisoning in a
dog. Vet Rec 1993;133:24.
allergic mechanisms have been pro- 8. Spoerkem D. Mushroom exposure. In: Peterson ME, Tal-
posed. Typically, clinical signs of cott PA, eds. Small animal toxicology. Philadelphia, Pa: WB
Saunders Co, 2001;571-592.
acute GI upset occur within two 9. Schonwald S, Mushrooms. In: Dart RC, ed. Medical toxi-
hours of ingestion and consist of cology. 3rd ed. Philadelphia, Pa: Lippincott Williams and
Wilkins, 2004;1719-1735.
malaise, weakness, nausea, vomit- 10. Menser GP. Hallucinogenic and poisonous mushroom: field
ing, and diarrhea.9 The greatest risk guide. 2nd ed. Berkeley, Calif: Ronin Publishing Inc, 1997;1-115.
11. Peterson M. Toxicologic decontamination. In: Peterson
associated with poisoning by these ME, Talcott PA, eds. Small animal toxicology. Philadelphia,
mushrooms is fluid and electrolyte Pa: WB Saunders Co, 2001;85-98.
12. Enjalbert F, Rapior S, Nouguier-Soule J, et al. Treatment
imbalance. Most cases are mild and of amatoxin poisoning: 20-year retrospective analysis. J Toxi-
usually resolve without treatment col Clin Toxicol 2002;40:715-757.
100 February 2007 Veterinary Medicine
You might also like
- Hamster Diet FinalDocument2 pagesHamster Diet FinalDalibor CetojevicNo ratings yet
- 009 06 Hamster Revolution No Comp VersionDocument21 pages009 06 Hamster Revolution No Comp VersionDalibor CetojevicNo ratings yet
- Mongoose Expert Studies Elusive SpeciesDocument2 pagesMongoose Expert Studies Elusive SpeciesDalibor CetojevicNo ratings yet
- Inverted Roof Insulation: June 2012Document2 pagesInverted Roof Insulation: June 2012Dalibor CetojevicNo ratings yet
- Hamster Anesthesia Guidance ARC 112519Document5 pagesHamster Anesthesia Guidance ARC 112519Dalibor CetojevicNo ratings yet
- Green Roof 2Document20 pagesGreen Roof 2Dalibor CetojevicNo ratings yet
- Bricks, Blocks & Pavers: US Industry Study With Forecasts ForDocument8 pagesBricks, Blocks & Pavers: US Industry Study With Forecasts ForDalibor CetojevicNo ratings yet
- Hamster Care SheetDocument3 pagesHamster Care SheetDalibor CetojevicNo ratings yet
- Hamilton The Hamster: StoryDocument4 pagesHamilton The Hamster: StoryDalibor CetojevicNo ratings yet
- Clay BricksDocument21 pagesClay BricksArul Gnanapragasam100% (1)
- EN24T Alloy Steel: High Strength, Shock & Wear ResistantDocument4 pagesEN24T Alloy Steel: High Strength, Shock & Wear ResistantDalibor CetojevicNo ratings yet
- PSA Testing For Prostate Cancer in Asymptomatic Men: Information For Health PractitionersDocument4 pagesPSA Testing For Prostate Cancer in Asymptomatic Men: Information For Health PractitionersDalibor CetojevicNo ratings yet
- SunCoast Project Platypus Investigation ReportDocument26 pagesSunCoast Project Platypus Investigation ReportDalibor CetojevicNo ratings yet
- RoofDocument20 pagesRoofDalibor CetojevicNo ratings yet
- M78a 1gb 3v Nand SpiDocument60 pagesM78a 1gb 3v Nand SpiDalibor CetojevicNo ratings yet
- Door ClosersDocument4 pagesDoor ClosersDalibor CetojevicNo ratings yet
- CD4011BCDocument8 pagesCD4011BCHenry Manzano TonatoNo ratings yet
- Add Squid to Your Menu in 40 CharactersDocument6 pagesAdd Squid to Your Menu in 40 CharactersDalibor CetojevicNo ratings yet
- SAB HandbookDocument81 pagesSAB HandbookDalibor CetojevicNo ratings yet
- Targetscan Hs Eg DB PDFDocument8 pagesTargetscan Hs Eg DB PDFDalibor CetojevicNo ratings yet
- Control of SlagDocument12 pagesControl of SlagVinay RajputNo ratings yet
- Targetscan Hs Eg DB PDFDocument8 pagesTargetscan Hs Eg DB PDFDalibor CetojevicNo ratings yet
- Kupukupu KukupiuuuDocument3 pagesKupukupu Kukupiuuutoken84No ratings yet
- Common Wombat: JR Fact FileDocument2 pagesCommon Wombat: JR Fact FileDalibor CetojevicNo ratings yet
- Software Licence Application: For Office Computers OnlyDocument1 pageSoftware Licence Application: For Office Computers OnlyDalibor CetojevicNo ratings yet
- Wombat DiariesDocument8 pagesWombat DiariesDalibor CetojevicNo ratings yet
- NSCDocument55 pagesNSCDalibor CetojevicNo ratings yet
- Journal Pone 0024851Document6 pagesJournal Pone 0024851Dalibor CetojevicNo ratings yet
- Etl 0440Document20 pagesEtl 0440Dalibor CetojevicNo ratings yet
- Tunnel and Shaft Solutions HumesDocument46 pagesTunnel and Shaft Solutions HumesrasanavaneethanNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Unit 3 Computer ScienceDocument3 pagesUnit 3 Computer ScienceradNo ratings yet
- Planning A Real Estate ProjectDocument81 pagesPlanning A Real Estate ProjectHaile SilasieNo ratings yet
- Rishte ki baat SMS messages collectionDocument108 pagesRishte ki baat SMS messages collectionTushar AggarwalNo ratings yet
- IGCSE Chemistry Section 5 Lesson 3Document43 pagesIGCSE Chemistry Section 5 Lesson 3Bhawana SinghNo ratings yet
- CMC Ready ReckonerxlsxDocument3 pagesCMC Ready ReckonerxlsxShalaniNo ratings yet
- Maj. Terry McBurney IndictedDocument8 pagesMaj. Terry McBurney IndictedUSA TODAY NetworkNo ratings yet
- Sanhs Ipcrf TemplateDocument20 pagesSanhs Ipcrf TemplateStephen GimoteaNo ratings yet
- AsiaSat 7 at 105Document14 pagesAsiaSat 7 at 105rahman200387No ratings yet
- Reg FeeDocument1 pageReg FeeSikder MizanNo ratings yet
- Portfolio by Harshit Dhameliya-1Document85 pagesPortfolio by Harshit Dhameliya-1Aniket DhameliyaNo ratings yet
- Krok2 - Medicine - 2010Document27 pagesKrok2 - Medicine - 2010Badriya YussufNo ratings yet
- Biology Mapping GuideDocument28 pagesBiology Mapping GuideGazar100% (1)
- MBO, Management by Objectives, Pooja Godiyal, Assistant ProfessorDocument20 pagesMBO, Management by Objectives, Pooja Godiyal, Assistant ProfessorPooja GodiyalNo ratings yet
- Difference Between Text and Discourse: The Agent FactorDocument4 pagesDifference Between Text and Discourse: The Agent FactorBenjamin Paner100% (1)
- Lecture02 NoteDocument23 pagesLecture02 NoteJibril JundiNo ratings yet
- GlastonburyDocument4 pagesGlastonburyfatimazahrarahmani02No ratings yet
- Exercises 6 Workshops 9001 - WBP1Document1 pageExercises 6 Workshops 9001 - WBP1rameshqcNo ratings yet
- How Psychology Has Changed Over TimeDocument2 pagesHow Psychology Has Changed Over TimeMaedot HaddisNo ratings yet
- SEO-Optimized Title for Python Code Output QuestionsDocument2 pagesSEO-Optimized Title for Python Code Output QuestionsTaru GoelNo ratings yet
- Bank NIFTY Components and WeightageDocument2 pagesBank NIFTY Components and WeightageUptrend0% (2)
- Conv VersationDocument4 pagesConv VersationCharmane Barte-MatalaNo ratings yet
- Trading As A BusinessDocument169 pagesTrading As A Businesspetefader100% (1)
- Numerical Methods Chapter 10 SummaryDocument8 pagesNumerical Methods Chapter 10 SummarynedumpillilNo ratings yet
- ASMOPS 2016 - International Invitation PHILIPPINEDocument4 pagesASMOPS 2016 - International Invitation PHILIPPINEMl Phil0% (3)
- Obstetrical Hemorrhage: Reynold John D. ValenciaDocument82 pagesObstetrical Hemorrhage: Reynold John D. ValenciaReynold John ValenciaNo ratings yet
- Resume Template & Cover Letter Bu YoDocument4 pagesResume Template & Cover Letter Bu YoRifqi MuttaqinNo ratings yet
- CAS-GEC04 Module11 Food-SecurityDocument6 pagesCAS-GEC04 Module11 Food-SecurityPermalino Borja Rose AnneNo ratings yet
- Unit-1: Introduction: Question BankDocument12 pagesUnit-1: Introduction: Question BankAmit BharadwajNo ratings yet
- Circular Flow of Process 4 Stages Powerpoint Slides TemplatesDocument9 pagesCircular Flow of Process 4 Stages Powerpoint Slides TemplatesAryan JainNo ratings yet