Professional Documents
Culture Documents
2016-The - Clinical - Teacher (Clinical Teaching Lesson Plan)
Uploaded by
Justin Vergara0 ratings0% found this document useful (0 votes)
11 views2 pagesclinical teaching
Original Title
2016-The_clinical_teacher (Clinical Teaching Lesson Plan)
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentclinical teaching
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
11 views2 pages2016-The - Clinical - Teacher (Clinical Teaching Lesson Plan)
Uploaded by
Justin Vergaraclinical teaching
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 2
Editorial
Empathy and the clinical
teacher
E
veryone seems to be talking accuracy; and to act on that 15 studies of interventions with
or writing about empathy. understanding in a helpful medical students that seemed to
There is general consensus therapeutic way’.4 be effective in this, although most
that good clinicians demonstrate involved pre- and post-intervention
it, and that we should help As well as defining and comparisons, and the authors
students and trainees to develop differentiating empathy from highlighted a need for larger, more
it.1 There is also an increasing related concepts such as ‘sympa- rigorous longitudinal studies.1 The
understanding of the underlying thy’ and ‘patient-centredness’, interventions included creative arts
social psychological and neuro- much of the clinical education around patient narratives, drama,
biological mechanisms;2,3 how- literature describes or applies reflective writing, training in
ever, although over a hundred instruments to try and measure communication and interpersonal
years have passed since Tichener it.2,6 One systematic review skills, problem-based learning,
introduced ‘empathy’ into the identified 36 different instruments, patient-interviewing tasks and
English language, we still lack a eight of which demonstrated simulation. Many other interven-
common understanding of the sufficient reliability, internal tions seem likely to influence
concept and its implications for consistency, and validity to study clinician empathy but have yet to
clinical teaching.1,4 In this issue, empathy in clinical care and be evaluated for this outcome
Walsh and colleagues report that training.6 Most were only self- specifically. Examples in this issue
most patients, when asked by reported measures, however, and include the work of Crampton and
medical students, ‘What kind of the authors felt none had suffi- colleagues that placed students in
doctor would you like me to be if cient predictive validity to deprived and underserved general
you came to me with an illness?’, recommend their use in selecting practice and community settings,8
emphasised ‘personal qualities’, applicants for training. Using such and work by Bennet and colleagues
including empathy and also instruments, potential associations in which students undertook
communication skills.5 A minority have been identified between everyday activities whilst wearing a
emphasised knowledge and empathy and gender, ethnicity, suit that simulates functional
intelligence, but none empha- speciality choice, risk of being impairments.9
sised manual skills. A recent sued for malpractice, and suscepti-
systematic review in general bility to burnout.1,7 Another A Digest article in this issue
practice (family medicine) found systematic review found that after summarises a systematic review in
that increased empathy in a possible initial increase, empathy our sister journal Medical
doctors seems to lower patient seems to decline during medical Education, which compares how
anxiety and distress, improve school and speciality training, with researchers have defined (concep-
patient satisfaction and enable- potential contributing factors tualised) and measured empathy in
ment (confidence and ability to including unrealistic expectations, medical education.10 The review
cope with life and illness), and mistreatment by superiors, high identified 109 articles, most of
improve clinical outcomes such workload, lack of support and which included a definition of
as diabetic control.4 The authors unsuitable learning environments.7 empathy incorporating two or more
described empathy as the ability of the following three elements:
of a doctor, ‘To understand the Many strategies to help thinking (cognitive); feeling
patient’s situation, perspective clinicians develop empathy have (emotional); and acting (behav-
and feelings; to communicate been described in the literature. A ioural, including communication).11
that understanding and check its recent systematic review identified These elements of the definition
© 2016 John Wiley & Sons Ltd. THE CLINICAL TEACHER 2016; 13: 89–90 89
tct_12527.indd 89 3/11/2016 6:42:25 AM
related closely to those identified health care disciplines. Students Academy of Sciences 2011;1231:
in the instruments used to measure and trainees frequently report that 35–45.
empathy in only 13 per cent of they do not feel sufficiently
4. Derksen F, Bensing J, Lagro-
studies. In other words, for most understood, valued and supported, Janssen A. Effectiveness of
quantitative studies on empathy, and there is a substantial and empathy in general practice: a
researchers do not seem to be disturbing body of literature on systematic review. Br J Gen Pract
measuring what they think they are student and trainee discrimina- 2013;63:e76–e84.
measuring. As we develop our tion, harassment and abuse in 5. Walsh S, Arnold B, Pickwell-Smith
understanding of the important clinical education.14 We know that B, Summers B. What kind of doctor
elements of empathy in clinical some forms of intimidation and would you like me to be? Clin Teach
2016;13(2):98–101.
practice and education, we are harassment may be viewed by
likely to want ever-more sophisti- those involved as useful educa- 6. Hemmerdinger JM, Stoddart SDR,
Lilford RJ. A systematic review of
cated ways to assess and study tional tools, especially if per-
tests of empathy in medicine. BMC
them. David Jeffrey, for example, ceived to have an acceptable Med Educ 2007;7:24.
conceptualises empathy as a purpose, to be necessary in the
7. Neumann M, Edelhäuser F, Tauschel
two-way relationship with many situation and to have positive D, Fishcher MR, Wirtz M, Woopen
more context-dependent elements, clinical or educational outcomes.14 C, Haramati A, Scheffer C. Empathy
including developing a reciprocal Yet they are likely to have a decline and its reasons: a system-
connection with the patient, being negative influence on the atic review of studies with medical
emotionally engaged yet able to development of empathy.7 How students and residents. Acad Med
2011;86:996–1009.
differentiate your own emotions can we expect learners to develop
from theirs, being curious to learn empathy if they are not treated 8. Crampton P, Hetherington
J, McLachlan J, Illing J.
about the patient’s perspective and with empathy themselves? The key
Learning in underserved UK
experience, and acting dynamically attributes of a good clinical areas: a novel approach. Clin Teach
and ethically with care, concern, teacher, as perceived by medical 2016;13(2):102–106.
and humility.12 students in the article by Burgess 9. Bennett P, Moore M, Wenham J.
and colleagues in this issue, The PAUL Suit©: an experi-
At a recent local medical include being able to develop ence of ageing. Clin Teach
education meeting we were struck rapport and relate to students in 2016;13(2):107–111.
by similarities between our addition to role-modelling rapport 10. Sterling M, Amiel J, Konopasek L.
research on student empathy and and empathy with patients.15 The conceptualisation and study of
aspects of our continuing work Empathy seems to be just as empathy by medical educators. Clin
Teach 2016;13(2):162–163.
on faculty development and important in the teacher–learner
student evaluation of teaching. A relationship as it is in the 11. Sulzer SH, Feinstein NW, Wendland
CL. Assessing empathy develop-
national survey of clinical clinician–patient relationship, and
ment in medical education: a
teachers suggested that many do indeed in the relationship systematic review. Med Educ
not feel recognised, valued or between teachers and their 2016;50(3):300–301.
supported in their educational colleagues. After all, who wouldn’t
12. Jeffrey D. Clarifying empathy:
roles, with one respondent want to be valued, understood the first step to more humane clini-
writing, ‘The band of overworked, and treated with respect, irrespec- cal care. Br J Gen Pract 2016;66:
stressed and overstretched tive of whether we are currently e143–e145.
clinicians are your customers learning, teaching or sick? 13. Ross MT, MacRae C, Scott J,
– you need to treat them with Renwick L, Moffat M, Needham G,
respect, cultivate them and really Scott H, Shippey B, Jackson C,
listen to them’.13 The teachers
seem to have perceived a lack of
Michael Ross Edgar S, Aitken D, Evans P, Irvine
S. Core competencies in teach-
ing and training for doctors in
empathy in their relationship Co-Editor in Chief Scotland: a review of the literature
with those responsible for the and stakeholder survey. Med Teach
training programmes. We are now REFERENCES 2014;36:527–538.
studying this in more depth and 1. Batt-Rawden SA, Chisolm MS, 14. Musselman LJ, MacRae HM, Reznick
exploring how medical school Anton B, Flickinger TE. Teaching RK, Lingard LA. ‘You learn better
communication and management empathy to medical students: an under the gun’: intimidation and
updated, systematic review. Acad harassment in surgical education.
practices might affect the
Med 2013;88:1171–1177. Med Educ 2005;39(9):926–934.
experiences and perceptions of
clinical teachers. 2. Irving P, Dickson D. Empathy: 15. Burgess A, Oates K, Goulston
towards a conceptual framework for K. Role modelling in medi-
health professionals. Int J Health cal education: the importance
Although much of the research of teaching skills. Clin Teach
Care Qual Assur 2004;17:212–220.
on clinician empathy has been 2016;13(2):134–137.
undertaken in medicine, the issues 3. Decety J. The neuroevolution of
empathy. Annals of the New York
seem to be common across the doi: 10.1111/tct.12527
90 © 2016 John Wiley & Sons Ltd. THE CLINICAL TEACHER 2016; 13: 89–90
tct_12527.indd 90 3/11/2016 6:42:25 AM
You might also like
- Example DBA PDP APA 6th EdDocument23 pagesExample DBA PDP APA 6th EdMonica SoniNo ratings yet
- CHN QuestionsDocument52 pagesCHN QuestionsJustin VergaraNo ratings yet
- Case Formulation in PsychotherapyDocument5 pagesCase Formulation in PsychotherapySimona MoscuNo ratings yet
- What S in A Case Formulation PDFDocument10 pagesWhat S in A Case Formulation PDFNicole Flores MuñozNo ratings yet
- Projective Psychology - Clinical Approaches To The Total PersonalityFrom EverandProjective Psychology - Clinical Approaches To The Total PersonalityNo ratings yet
- Emotional Intelligence Among Nursing Students - An Integrated ReviewDocument9 pagesEmotional Intelligence Among Nursing Students - An Integrated ReviewShirleyNo ratings yet
- Detailed Lesson Plan No. 1 Learning Area: Computer System Servicing Quarter: Quarter I Week: Week-1 Grade Level: Grade 8 Duration: 2 HoursDocument3 pagesDetailed Lesson Plan No. 1 Learning Area: Computer System Servicing Quarter: Quarter I Week: Week-1 Grade Level: Grade 8 Duration: 2 HoursMark John Bernaldez100% (2)
- 2019 Audit-1 Course OutlineDocument5 pages2019 Audit-1 Course OutlineGeraldo MejillanoNo ratings yet
- Front Page Case Study PLM NursingDocument1 pageFront Page Case Study PLM NursingJustin Vergara100% (1)
- Why Mindfulness Is Better Than ChocolateDocument16 pagesWhy Mindfulness Is Better Than ChocolateDavid Michie0% (1)
- Nursing TherapeuticsDocument5 pagesNursing TherapeuticsDWNo ratings yet
- Results-Based Performance Management System: PortfolioDocument74 pagesResults-Based Performance Management System: PortfolioWella Mallory ArmentaNo ratings yet
- SLM - Ro - Mil-Q2 Module 12Document20 pagesSLM - Ro - Mil-Q2 Module 12Bill Villon90% (10)
- LFD - A Reflective Experience in A Student Nurse's Clinical ExperienceDocument9 pagesLFD - A Reflective Experience in A Student Nurse's Clinical ExperienceCarmel GuazonNo ratings yet
- Surgical IntuitionDocument1 pageSurgical IntuitionRoxana ElenaNo ratings yet
- A Review of Empathy, Its Importance, and Its Teaching in Surgical TrainingDocument7 pagesA Review of Empathy, Its Importance, and Its Teaching in Surgical TrainingMárcia SoaresNo ratings yet
- Teaching Empathy To Medical Students An Updated, Systematic ReviewDocument7 pagesTeaching Empathy To Medical Students An Updated, Systematic ReviewariqNo ratings yet
- Letters To The Editor: Change in Empathy in Medical SchoolDocument3 pagesLetters To The Editor: Change in Empathy in Medical SchoolBaoz PingNo ratings yet
- Physician Empathy: Definition, Components, Measurement, and Relationship To Gender and SpecialtyDocument7 pagesPhysician Empathy: Definition, Components, Measurement, and Relationship To Gender and SpecialtySheilla Gomez TejadaNo ratings yet
- The Clinical Teacher - 2020 - Cairns - Empathy Maps in Communication Skills TrainingDocument5 pagesThe Clinical Teacher - 2020 - Cairns - Empathy Maps in Communication Skills TrainingHina TipuNo ratings yet
- Empathy Levels in Medical Students Do They ReallyDocument26 pagesEmpathy Levels in Medical Students Do They ReallyaldyNo ratings yet
- Reviews: Kathy A. Stepien, BS, MA, Amy Baernstein, MDDocument7 pagesReviews: Kathy A. Stepien, BS, MA, Amy Baernstein, MDNythNo ratings yet
- Reviews: Kathy A. Stepien, BS, MA, Amy Baernstein, MDDocument7 pagesReviews: Kathy A. Stepien, BS, MA, Amy Baernstein, MDNythNo ratings yet
- Empatia - 2017 - 2 (Texto A)Document5 pagesEmpatia - 2017 - 2 (Texto A)juliana bNo ratings yet
- Hooker - Understanding Empathy: Why Phenomenology and Hermeneutics Can Help Medical Education and PracticeDocument12 pagesHooker - Understanding Empathy: Why Phenomenology and Hermeneutics Can Help Medical Education and PracticeCamille TobilloNo ratings yet
- An Exploratory Study of Student Nurses' Empathy: Christina Ouzouni, Konstantinos NakakisDocument19 pagesAn Exploratory Study of Student Nurses' Empathy: Christina Ouzouni, Konstantinos NakakisBojana VulasNo ratings yet
- Nci 55649 Research - Article Malakcioglu PDFDocument9 pagesNci 55649 Research - Article Malakcioglu PDFAmalH.IssaNo ratings yet
- Batt Rawden2013Document7 pagesBatt Rawden2013Baoz PingNo ratings yet
- Underlying Construct of Empathy, Optimism, and Burnout in Medical StudentsDocument5 pagesUnderlying Construct of Empathy, Optimism, and Burnout in Medical StudentsChristiana TomescuNo ratings yet
- Dissertation Mental Health NursingDocument8 pagesDissertation Mental Health NursingHelpWritingPapersUK100% (1)
- Effectiveness of Empathy in General Practice:: ResearchDocument9 pagesEffectiveness of Empathy in General Practice:: ResearchAndrés Ricardo Horta JaraNo ratings yet
- Failure in Clinical EducationDocument11 pagesFailure in Clinical EducationAnnette WillgensNo ratings yet
- Branch Et Al 2001 Teaching The Human Dimensions of Care in Clinical SettingsDocument8 pagesBranch Et Al 2001 Teaching The Human Dimensions of Care in Clinical Settingsapi-264671444No ratings yet
- The Role of The Individual in The Coming Era of Process-Based Therapy (Articulo Examen Final)Document14 pagesThe Role of The Individual in The Coming Era of Process-Based Therapy (Articulo Examen Final)Cristian Steven Cabezas JoyaNo ratings yet
- Patient Practitioner Relationship 1Document24 pagesPatient Practitioner Relationship 1Dr Aniqa SundasNo ratings yet
- Richard Adams, 2012, Clinical Empathy - A Discussion On Its Benefits For PractitionersDocument6 pagesRichard Adams, 2012, Clinical Empathy - A Discussion On Its Benefits For PractitionersLisa-Mari De KlerkNo ratings yet
- A Review of Empathy Education in NursingDocument11 pagesA Review of Empathy Education in Nursinglora ardyaNo ratings yet
- D BNP 20 0016Document16 pagesD BNP 20 0016Nadeesha DissanayakaNo ratings yet
- Adopting The Right Attitude Can Convert A Negative Stress Into A Positive One.Document43 pagesAdopting The Right Attitude Can Convert A Negative Stress Into A Positive One.France Jannica Petallar - OrbetaNo ratings yet
- Educación: MédicaDocument8 pagesEducación: MédicaMARTINA CESARINA EDITH GUILLERMO ROMANNo ratings yet
- BismillahDocument10 pagesBismillahlatifah nur khasanahNo ratings yet
- Teaching EmpathyDocument12 pagesTeaching EmpathyLaura Pineda MartinezNo ratings yet
- Using Self Regulated Learning Theory To Understand.9 PDFDocument4 pagesUsing Self Regulated Learning Theory To Understand.9 PDFMuhamad Nur Syukriani YusufNo ratings yet
- Validación - Escala de EmpatiaDocument7 pagesValidación - Escala de EmpatiaNidia MontoyaNo ratings yet
- Uncovering A Curricular Model of Self Care in Pediatric Physical TherapyDocument17 pagesUncovering A Curricular Model of Self Care in Pediatric Physical TherapyAnnette WillgensNo ratings yet
- Literature Review On Emotional ExhaustionDocument4 pagesLiterature Review On Emotional Exhaustionaflskeqjr100% (1)
- Medu 13014Document2 pagesMedu 13014afsdsaadsNo ratings yet
- Jeffrey 2016 Empathy Sympathy and Compassion in Healthcare Is There A Problem Is There A Difference Does It MatterDocument7 pagesJeffrey 2016 Empathy Sympathy and Compassion in Healthcare Is There A Problem Is There A Difference Does It MatterFrancisco BohorquezNo ratings yet
- Riess Et Al (2012)Document7 pagesRiess Et Al (2012)Alicia BrevaNo ratings yet
- L'Effet D'une Éducation À L'empathie Structurée Sur La Compétence D'empathie Des Stagiaires en Soins Infirmiers de Premier CycleDocument6 pagesL'Effet D'une Éducation À L'empathie Structurée Sur La Compétence D'empathie Des Stagiaires en Soins Infirmiers de Premier CycleMeryeme KoudriNo ratings yet
- Članak 1Document11 pagesČlanak 1InesCNo ratings yet
- Teaching Empathy Through Movies: Reaching Learners' Affective Domain in Medical EducationDocument13 pagesTeaching Empathy Through Movies: Reaching Learners' Affective Domain in Medical EducationSorina NataliaNo ratings yet
- A Pattern Language of Compassion in Intensive CareDocument9 pagesA Pattern Language of Compassion in Intensive CareYael NepoNo ratings yet
- Annotated Bibliography For Ethics Behind Informed ConsentDocument5 pagesAnnotated Bibliography For Ethics Behind Informed Consentapi-709745869No ratings yet
- Behaviour Based Functional and Dysfunctional Strategies of Medical Students To Cope With BurnoutDocument12 pagesBehaviour Based Functional and Dysfunctional Strategies of Medical Students To Cope With BurnoutyodaNo ratings yet
- A Culture of Caring: How Nurses Promote Emotional Wellbeing and Aid Recovery Following A StrokeDocument7 pagesA Culture of Caring: How Nurses Promote Emotional Wellbeing and Aid Recovery Following A Strokeputu juniNo ratings yet
- PDFarticulopublicado PDFDocument18 pagesPDFarticulopublicado PDFDanna Trejo HernandezNo ratings yet
- Peer Caring Behaviour Among Nursing StudentsDocument8 pagesPeer Caring Behaviour Among Nursing StudentsAgung PermanaNo ratings yet
- Dawis, Kaye Frances Abendan, Lyca Joy, Alonso, Alyssa Vita, Caspe, JP Castel, Robert Jr. Ebanos, Pauline MarieDocument24 pagesDawis, Kaye Frances Abendan, Lyca Joy, Alonso, Alyssa Vita, Caspe, JP Castel, Robert Jr. Ebanos, Pauline MariejpNo ratings yet
- Thomas 2016Document6 pagesThomas 2016Septyana M ANo ratings yet
- To Identify Irrational Beliefs, Locus of Control, Quality of Work Life Among Nurses Working in Government and Corporate HospitalsDocument8 pagesTo Identify Irrational Beliefs, Locus of Control, Quality of Work Life Among Nurses Working in Government and Corporate HospitalsAnonymous CwJeBCAXpNo ratings yet
- 2 Tsiantou2013Document10 pages2 Tsiantou2013yioulaNo ratings yet
- E144 Vol. 52 No. 6 December 2016 Selected AbstractsDocument2 pagesE144 Vol. 52 No. 6 December 2016 Selected AbstractsJos CanalesNo ratings yet
- Empathic Communication and Gender in The Physician-Patient EncounterDocument10 pagesEmpathic Communication and Gender in The Physician-Patient EncounterDouglas MarinNo ratings yet
- The Role of PhysiciansDocument5 pagesThe Role of PhysiciansMarvin ThomasNo ratings yet
- Coetzee Et Al-2018-Nursing & Health Sciences Review CompasionDocument12 pagesCoetzee Et Al-2018-Nursing & Health Sciences Review CompasionFlory23ibc23No ratings yet
- Vol 51 No 2 01 Prevalence Med PDFDocument4 pagesVol 51 No 2 01 Prevalence Med PDFJustin VergaraNo ratings yet
- C. Models of Teaching and LearningDocument12 pagesC. Models of Teaching and LearningJustin VergaraNo ratings yet
- General Objectives: Activity Specific Objectives Time Frame Strategies ResourcesDocument2 pagesGeneral Objectives: Activity Specific Objectives Time Frame Strategies ResourcesJustin VergaraNo ratings yet
- OJT JazzDocument5 pagesOJT JazzJustin VergaraNo ratings yet
- EngengDocument1 pageEngengJustin VergaraNo ratings yet
- Rationale SpellingDocument1 pageRationale SpellingHassan Funsho AkandeNo ratings yet
- Video Lectures - Differential Equations - Mathematics - MIT OpenCourseWareDocument4 pagesVideo Lectures - Differential Equations - Mathematics - MIT OpenCourseWareyashwant1299523No ratings yet
- Manual Testing Course Content 2011Document2 pagesManual Testing Course Content 2011Jamie RossNo ratings yet
- American Cultural SyllabusDocument3 pagesAmerican Cultural Syllabusapi-236350851No ratings yet
- Q1W8 FBS DLLDocument4 pagesQ1W8 FBS DLLKei LansangNo ratings yet
- Bread of SaltDocument2 pagesBread of SaltEduardo GarciaNo ratings yet
- MGMT 371 Syllabus-Fall2011-Sect002Document4 pagesMGMT 371 Syllabus-Fall2011-Sect002e9b9t9No ratings yet
- Classroom Rules and ProceduresDocument13 pagesClassroom Rules and ProceduresTetzie SumayloNo ratings yet
- Tle 8 CarpentryDocument2 pagesTle 8 CarpentryEdem Irish Rivera SenerpidaNo ratings yet
- M4GE-IIIa-12.2-w1 - d1Document7 pagesM4GE-IIIa-12.2-w1 - d1MARY JUSTINE SIENNE D. CORPORALNo ratings yet
- Informatics Student BrochureDocument4 pagesInformatics Student BrochureHanan AhmedNo ratings yet
- The Best Teaching Strategies Used by TeachersDocument11 pagesThe Best Teaching Strategies Used by TeachersJam JamNo ratings yet
- Educ 404Document18 pagesEduc 404Mary Cris MalanoNo ratings yet
- Curriculum Audit (C.A.) : School Year 2020-2021Document2 pagesCurriculum Audit (C.A.) : School Year 2020-2021juvelyn abuganNo ratings yet
- Final Portfolio EssayDocument7 pagesFinal Portfolio Essayapi-340129196No ratings yet
- Course Outline Physics EducationDocument3 pagesCourse Outline Physics EducationTrisna HawuNo ratings yet
- Anthropology Is A Science of HumankindDocument2 pagesAnthropology Is A Science of HumankindSuman BaralNo ratings yet
- Job Vacancies - JESS DubaiDocument4 pagesJob Vacancies - JESS DubaiRizwan FaridNo ratings yet
- Nursing AuditDocument28 pagesNursing Auditmarsha100% (1)
- Daily Lesson Log School: Grade Level: Teacher: Learning Area: Quarter: Checked byDocument3 pagesDaily Lesson Log School: Grade Level: Teacher: Learning Area: Quarter: Checked byRonnel Jay RodriguezNo ratings yet
- Law On Negotiable Instruments Law SyllabusDocument2 pagesLaw On Negotiable Instruments Law SyllabusThea FloresNo ratings yet
- Nghe TOEFLDocument18 pagesNghe TOEFLdongochieu81No ratings yet
- Brochure 6 Labour LawDocument10 pagesBrochure 6 Labour Lawlemajor69No ratings yet
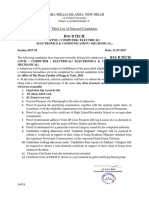
- Jamia Millia Islamia, New Delhi: B14: B.TECHDocument11 pagesJamia Millia Islamia, New Delhi: B14: B.TECHMrinalNo ratings yet