Professional Documents
Culture Documents
Paraplegic Acupuncture
Uploaded by
Med AliCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Paraplegic Acupuncture
Uploaded by
Med AliCopyright:
Available Formats
Authors:
Alice M. K. Wong, MD
Chau-Peng Leong, MD
Ting-Ya Su, MS Acupuncture
Shang-Won Yu, MD
Wen-Chung Tsai, MD
Carl P. C. Chen, MD
Affiliations:
Research Article
From the Departments of Physical
Medicine and Rehabilitation (AMKW,
TYS, WCT, CPCC) and Traumatic and
Emergent Surgery (SWY), Chang
Gung Memorial Hospital, Taipei,
Taiwan, Republic of China; the
Department of Physical Medicine and Clinical Trial of Acupuncture for
Rehabilitation, Chang Gung Memorial
Hospital, Kaohsing, Taiwan, Republic
Patients with Spinal Cord Injuries
of China (CPL); and the Department
of Physical Medicine and ABSTRACT
Rehabilitation, Chang Gung Wong AMK, Leong CP, Su TY, Yu SW, Tsai WC, Chen CPC: Clinical trial
University, Taipei, Taiwan, Republic
of China (CPL).
of acupuncture for patients with spinal cord injuries. Am J Phys Med
Rehabil 2003;82:21–27.
Disclosures: Objective: To examine whether electrical acupuncture therapy through
FIM™ is a trademark of the Uniform
adhesive surface electrodes and concomitant auricular acupuncture ther-
Data System for Medical apy could improve the neurologic or functional recovery in acute traumatic
Rehabilitation, a division of UB spinal cord injury patients.
Foundation Activities, Inc.
Design: A total of 100 acute traumatic spinal cord injury patients with
Correspondence: American Spinal Injury Association (ASIA) impairment grading of A and B
were recruited into this study. They were randomly divided into the acu-
All correspondence and requests for puncture and control groups. In the acupuncture group, electrical acu-
reprints should be addressed to Alice puncture therapy via the adhesive surface electrodes were applied to the
M. K. Wong, MD, Department of
Physical Medicine and Rehabilitation,
bilateral Hou Hsi (SI3) and Shen Mo (B62) acupoints. In auricular acu-
Chang Gung Memorial Hospital, 199, puncture, four acupoints related to the spinal cord were selected for
Tun-Hwa North Road, Taipei, 105, stimulation at the antihelix, helix, and lower portion of the ear-back areas.
Taiwan, ROC. Acupuncture therapy was initiated early in the emergency room setting or
soon after spinal surgical intervention. Rehabilitation therapy was also
0894-9115/03/8201-0021/0
provided to the patients during acupuncture therapy. In the control group,
American Journal of Physical
Medicine & Rehabilitation only rehabilitation therapy was provided to the patients. Neurologic and
Copyright © 2002 by Lippincott functional scores were assessed during the time of admission, hospital
Williams & Wilkins discharge, and 1-yr postinjury follow-up.
DOI: 10.1097/01.PHM.0000043517.06642.D0 Results: There were significant improvements in neurologic (sensory
and motor), functional, and FIM™ scores in the acupuncture group com-
pared with the initial admission period when assessed during the time of
hospital discharge and the 1-yr postinjury follow-up. A greater percentage
of patients in the acupuncture group recovered to a higher ASIA impair-
ment grading.
Conclusion: The use of concomitant auricular and electrical acupunc-
ture therapies, when implemented early in acute spinal cord injury, can
contribute to significant neurologic and functional recoveries.
Key Words: Spinal Cord Injury, American Spinal Injury Association, Re-
habilitation, Electrical Acupuncture, Auricular Acupuncture
January 2003 Acupuncture on Patients with SCI 21
S pinal cord injury (SCI), a trau-
matic insult to the spinal cord, can
examine whether concomitant treat-
ment of electrical acupuncture
through adhesive surface electrodes
The exclusion criteria were: pa-
tients who required mechanical ven-
tilation and those with concomitant
result in alternations of normal motor, and auricular acupuncture therapies traumatic brain injury, peripheral
sensory, and autonomic function.1 could improve the neurologic or func- nerve injury, loss of consciousness,
When the traumatic episode is severe tional recoveries in acute traumatic and multiple bony fractures. All pa-
enough, many SCI patients do not re- SCI patients. The effectiveness of ther- tients gave informed consent to par-
cover from the lost neurologic func- apy was assessed based on the neuro- ticipate in the study, which was per-
tions.2 As a result, some of them will logic and functional score changes be- formed according to the guidelines of
pursue alternative treatments, such as fore and after acupuncture therapies. the local ethics committee.
acupuncture, in hoping for possible
improvement in neurologic recovery. MATERIALS AND METHODS Evaluation of Patients
Acupuncture is an ancient Chi-
Subjects The neurologic status or score
nese therapy practiced for more than
2500 yr to cure disease and relieve A total of 100 traumatic spinal was assessed by the International
pain.3 In 1979, the World Health Orga- cord–injured patients with complete Standards for Neurologic and Func-
nization drew up a provisional list of 47 motor paralysis below the injury level tional Classification of SCI as devel-
diseases that could be treated with acu- were recruited into this study. Table oped by the American Spinal Injury
puncture. Neurogenic bladder, which 1 summarizes the subjects’ charac- Association (ASIA). The neurologic
can be an impairment encountered in teristics. All the recruited patients re-
score included sensory and motor ex-
SCI patients, was referenced as poten- ceived the necessary initial emergent
aminations. For the sensory exami-
tially treatable with acupuncture.4 treatments for SCI, which included
nation, each dermatome was tested
Politis and Korchinski5 reported surgical bone fusions and fixations
for both sharp (pin-prick) and light-
the use of “first-aid” acupuncture for some patients. Fifty of the pa-
touch sensation. Sharp sensation was
treatment in rats with experimental tients received additional acupunc-
tested by using a disposable safety
standardized spinal cord contusion at ture therapy, and these patients were
pin, and light touch was tested with
the eighth thoracic spinal level (T8 regarded as the acupuncture group.
For patients not requiring surgical cotton. The scale for sensory testing
level). Results showed that when acu- was from 0 to 2, with 0 as absent
puncture therapy was initiated within interventions, acupuncture and reha-
bilitation therapies were initiated sensation and 2 as normal sensation.
15 min after surgery, minimization of When all the dermatomal levels were
posttraumatic cord shrinkage and re- early at the emergency center and
continued until the day of discharge. tested bilaterally, a maximum score
markable sparing of ventral horn
For patients requiring surgery, the would be 112.
neurons became evident. A clinical
aforementioned therapies were initi- A total of ten myotomes were
study on humans also reported im-
ated after the patients were trans- assessed bilaterally, with a manual
provement in 120 paraplegic patients
ferred back to ordinary wards. The muscle testing score of 0 –5 per mus-
after acupuncture therapy.6
other 50 patients without acupunc- cle group. The overall score range
Acupuncture is an invasive proce-
ture therapy were regarded as the was from 0 to 100. The ASIA impair-
dure in which thin metal needles are
inserted into specific body sites and control group, and they only received ment scale was used for the determi-
slowly twisted manually or stimulated necessary rehabilitation therapies. nation of degree of completeness in
electrically. As a result, it carries the
risks of local pain, hematoma forma-
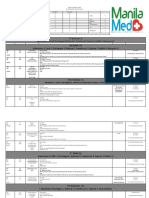
tion, infection, and even syncope. TABLE 1
Therefore, acupuncture should only be Demographic data of acupuncture and control groups
performed by certified acupuncturists. Acupuncture Group Control
The uncomfortable pain sensation in- (n ⫽ 50) (n ⫽ 50) Group P Value
duced by needle manipulation could be Age, yr 35.1 ⫾ 13.0 34.7 ⫾ 13.1 0.53
replaced by the application of electrical Sex, M/F 41/9 39/11 0.62
acupuncture in which adhesive surface Level of lesion, quadriplegia/ 19/31 18/32 0.84
electrodes are used. It was postulated paraplegia
ASIA grade A/B 28/22 32/18 0.419
to be an effective treatment method in
Duration of hospitalization, days 58.6 ⫾ 17.1 57.1 ⫾ 18.7 0.68
terms of functional recovery in hemi-
plegic stroke patients.7 ASIA, American Spinal Injury Association.
The purpose of this study was to
22 Wong et al. Am. J. Phys. Med. Rehabil. ● Vol. 82, No. 1
injury. This scale closely parallels adhesive tape for 1 wk at the ear acu- group, only the motor score revealed
that of Frankel. point. Four acupoints related to the significant improvement when at
The functional status was as- spinal cord were selected for stimula- 1-yr postinjury follow-up (P ⫽
sessed by using the Chinese version tion at the antihelix, helix, and lower 0.023). In terms of the individualized
of the FIM™ instrument due to its portion of the ear-back areas (Fig. 1). area of sphincter function in the FIM
high interrater reliability. All patients The small needles were changed every score, the bladder control score was
were evaluated by a well-trained week. 3.02 ⫾ 1.39 and the bowel control
nurse practitioner. FIM scores were score was 3.42 ⫾ 0.98 when exam-
constructed based on seven levels of Data Analysis ined at the 1-yr postinjury follow-up
function. The assessment defines 18 The FIM, sensory, and motor as- for the acupuncture group. In the
items within the following six areas sessment data were gathered during control group, the bladder control
of functioning: self-care, sphincter initial admission to the rehabilitation score was 1.49 ⫾ 1.35 and the bowel
control, mobility, locomotion, com- ward, discharge from the hospital, control score was 1.70 ⫾ 1.47 when
munication, and social cognition. and 1 yr after SCI. Statistical compar- examined at the 1-yr follow-up. When
The scores may range from a low of isons were performed based on these both groups were compared, signifi-
18 to a maximum of 126. three time points. The SPSS software cant improvement in sphincter func-
(SPSS, Chicago, IL) was used for sta- tion was noted in the acupuncture
Acupuncture Protocol tistical data analysis. Means were group (P ⫽ 0.001).
compared by the two-tailed t test or The comparison of ASIA and FIM
Selected Acupoints. The acupoints of repeated measurements of the analy- scores of both groups during the
bilateral Hou Hsi (SI3) and Shen Mo sis of variance test. The repeated three different time points are sum-
(B62) (Fig. 1) were selected for acu- measurements of the analysis of vari- marized in Table 3. During initial ad-
puncture therapy. The Hou Hsi acu- ance test was confirmed by the post mission to the rehabilitation ward, no
point is located at the end of transverse hoc Hermert test. The nonparametric significant difference in ASIA and
crease of the fifth metacarpophalangeal FIM data were compared by using FIM scores were noted. At the time of
joint when the hand is placed in a fisted Wilcoxon’s signed-rank test. Propor- discharge and at the 1-yr postinjury
position. Shen Mo is located at the feet, tions were further compared by ap- follow-up, the acupuncture group re-
near the inferior lateral malleoli areas. plying 2 tests. Statistical signifi- vealed significant improvement in all
Both acupoints are connected to the cance was set at P ⬍ 0.05. the ASIA and FIM scores when com-
Governic meridian, which is related to pared with the control group (P ⬍
the spinal cord as documented by tra- 0.05).
RESULTS
ditional Chinese medicine. The ASIA impairment scale of
Patients in the acupuncture During initial admission to the all the patients are listed in Table 4.
group received electrical acupunc- hospital, all the 100 acute SCI pa- The most remarkable finding is that
ture therapy via the 4 ⫻ 5 cm2 adhe- tients belonged to ASIA impairment more patients in the acupuncture
sive surface electrodes at the afore- scale A or B. They were matched for group improved to an ASIA grade of
mentioned bilateral acupoints. The age, sex, level of injury, and ASIA C or better when examined at the
HANS electro-acupuncture apparatus impairment scale. Patients were ran- time of discharge and at 1-yr
(Wearnes Technology, Singapore) domly distributed to the acupuncture postinjury follow-up as compared
was applied for stimulation. The fre- and control group, with 50 patients with the control group (P ⬍ 0.05).
quency was set at 75 Hz, with a pulse in each group (Table 1). The changes in the ASIA impair-
duration of 200 sec, and the magni- The neurologic status (ASIA sen- ment scale of both groups during
tude of stimulation was set at 10 mV. sory and motor scores) and func- the three different time points are
Each treatment session was 30 min, tional status (FIM total score) of each further illustrated in Figure 2.
with a total of five sessions per week. group at the time of admission to
rehabilitation ward, discharge from
Auricular Acupuncture. In addition to
DISCUSSION
the hospital, and 1-yr postinjury fol-
the Hou Hsi (SI3) and Shen Mo (B62) low-up examination are summarized Acupuncture has been used in tra-
acupoints, acupuncture therapy to bi- in Table 2. In the acupuncture group, ditional Chinese medicine to relieve
lateral ears was also performed for pa- all the sensory, motor, and FIM pain and cure a variety of diseases for
tients in the acupuncture group. The scores improved significantly when more than 2500 yr. There are 361 iden-
auricular acupuncture was performed examined on the day of discharge tified acupoints, and together they
by using a small needle (1 mm in from the hospital and 1 yr after injury form a network of 14 channels, called
length) with a ring-tail, held in place by (P ⬍ 0.05). Whereas in the control the meridians. Through these meridi-
January 2003 Acupuncture on Patients with SCI 23
Figure 1: Selected acupoints for acupuncture therapy.
ans, the internal organs are believed to peutic trials of acupuncture therapy for followed by slow manual twisting ac-
be interconnected with the superficial neurogenic bladder of SCI patients also tion of the acupuncturist. The needles,
parts of the body. Acupuncture therapy showed significantly shortened dura- once correctly inserted into the acu-
has been shown to be effective in im- tion for bladder training.8 points, can also be stimulated electri-
proving functional outcomes in hemi- Acupuncture therapy is usually cally. The de qi response is a prerequi-
plegic stroke patients and paraplegic done by the insertion of thin metal site for effective acupuncture therapy.
spinal cord–injured patients. Thera- needles to the acupoints, and this is It is often described as an uncomfort-
24 Wong et al. Am. J. Phys. Med. Rehabil. ● Vol. 82, No. 1
TABLE 2
Comparison of neurologic and functional status of the twogroups during different time
points
ASIA Scores FIMTM
Motor PP Sensory LT Sensory Total Score
Acupuncture group
Admission 41.0 ⫾ 21.5 60.8 ⫾ 27.7 63.0 ⫾ 23.2 49.9 ⫾ 13.1
Discharge 58.8 ⫾ 21.4 80.0 ⫾ 20.8 81.7 ⫾ 20.3 75.8 ⫾ 19.2
1-yr follow up 74.2 ⫾ 23.7 90.0 ⫾ 29.1 92.5 ⫾ 27.8 106.9 ⫾ 21.5
P value 0.000a 0.000a 0.000a 0.000a
Control group
Admission 41.0 ⫾ 17.7 59.1 ⫾ 24.9 60.8 ⫾ 24.4 47.7 ⫾ 12.3
Discharge 45.1 ⫾ 20.4 63.2 ⫾ 27.4 64.1 ⫾ 27.7 64.5 ⫾ 19.7
1-yr follow up 52.3 ⫾ 23.2 69.8 ⫾ 26.8 70.5 ⫾ 26.7 88.7 ⫾ 24.0
P value 0.023a 0.128 0.179 0.000a
ASIA, American Spinal Injury Association; PP, pinprick; LT, light touch.
a
P ⬍ 0.05.
able sensation, causing a numb, sore, through adhesive surface electrodes through the twitching and contraction
or heavy feeling during needle twirling and auricular acupuncture therapy motions of the stimulated muscles.
at the acupoint.9,10 In our ASIA grade A were applied to the patients.7,11 Reha- However, in electrical acupuncture
and B SCI patients, sensory perception bilitation treatments were also per- therapy, stimulation is provided di-
is absent caudal to the injury level. The formed on these patients in addition to rectly to the acupoint areas, not to the
usual de qi response could not be per- the acupuncture therapies. muscles nor the neuromuscular junc-
ceived by these patients. The applica- The mechanism of action provided tion areas. As a result, the typical mus-
tion of needles might even be a noxious by electrical acupuncture therapy is be- cle contraction motions will not be ob-
stimulus causing autonomic hyperre- lieved to be different than that of tra- served during electrical acupuncture
flexia, especially in patients with higher ditional therapeutic electrical stimula- therapy.
cord level injury. As a result, the alter- tion. In electrical stimulation, muscles In this study, the Hou Hsi (SI3)
native electrical acupuncture therapy are stimulated. This can be observed and Shen Mo (B62) were selected as
TABLE 3
Comparison of neurologic and functional status in the two groups during different time
points
ASIA Scores FIMTM
Motor PP Sensory LT Sensory Total Score
Admission
Acupuncture group 41.0 ⫾ 21.5 60.8 ⫾ 22.7 63.0 ⫾ 23.2 48.7 ⫾ 13.1
Control group 41.0 ⫾ 17.7 59.1 ⫾ 24.9 60.8 ⫾ 24.4 47.7 ⫾ 12.3
P value 0.992 0.425 0.616 0.407
Discharge
Acupuncture group 58.8 ⫾ 21.4 80.0 ⫾ 20.8 81.7 ⫾ 20.3 75.8 ⫾ 19.2
Control group 45.3 ⫾ 20.4 63.2 ⫾ 27.4 64.1 ⫾ 27.7 64.5 ⫾ 19.7
P value 0.002a 0.001a 0.000a 0.004a
1-yr follow up
Acupuncture group 74.4 ⫾ 23.7 90.0 ⫾ 29.1 92.5 ⫾ 27.8 106.9 ⫾ 21.5
Control group 52.3 ⫾ 23.2 69.9 ⫾ 26.8 70.5 ⫾ 26.7 88.7 ⫾ 24.0
P value 0.000a 0.000a 0.000a 0.000a
ASIA, American Spinal Injury Association; PP, pinprick; LT, light touch.
a
P ⬍ 0.05.
January 2003 Acupuncture on Patients with SCI 25
TABLE 4
Changes in American Spinal Injury Association (ASIA) impairment scale of both groups
during three different time points
Acupuncture Group Control Group
ASIA Grade A B C D E A B C D E P
A
Admission 28 32 1.0
Discharge 10 4 12 2 0 28 3 1 0 0 0.000
1-yr follow-up 8 3 10 2 5 27 2 3 0 0 0.000
B
Admission 22 18 1.0
Discharge 0 0 9 12 1 0 6 7 5 0 0.003
1-yr follow-up 0 0 0 6 16 0 3 5 6 4 0.000
Total
Admission 28 22 0 0 0 32 18 0 0 0 0.419
Discharge 10 4 21 14 1 28 9 8 5 0 0.000
1-yr follow-up 8 3 10 8 21 27 5 8 6 4 0.000
the acupoints for acupuncture therapy. els of the spinal cord, which also in- compared with the control group. The
The Hou Hsi (SI3) and Shen Mo (B62) cluded the lumbar cord level.9 acupuncture group also had many pa-
acupoints belong to the Yang Ming me- As evident in our results, patients tients improved to an ASIA grade of C
ridian of the hands and feet, which are in the acupuncture group had signifi- or better. There can be numerous neu-
connected to the cervical spinal cord. cant motor, sensory, and FIM score im- rophysiologic factors contributing to
The four auricular acupoints selected provements during the time of dis- the aforementioned improvements
in this study were related to more lev- charge and 1-yr postinjury follow-up as that are difficult to be proved clinically
Figure 2: Changes in American Spinal Injury Association (ASIA) impairment scale of both groups during the three
different time points. SCI, spinal cord injury.
26 Wong et al. Am. J. Phys. Med. Rehabil. ● Vol. 82, No. 1
and scientifically. Nevertheless, it is be- SCI patients with ASIA grade A and B. patients: A preliminary report. Spinal
lieved that acupuncture therapy Therefore, acupuncture therapy may Cord 1998;36:476 – 80
through the correct acupoints and me- be considered as an effective alternative 9. Tsay RC: Textbook of Chinese Acupunc-
ture Medicine: General Introduction to
ridians in the acute SCI episode will treatment strategy for SCI patients.
Acupuncture. Wappinger Falls, Association
assist in the minimization of posttrau- With combined rehabilitation therapy, of Chinese Medicine and East-West Medical
matic cord shrinkage and sparing of a higher quality treatment plan can Center, 1974, vol 1, pp, 40 –52
the ventral horn neurons.5,6 Even in thus be offered to SCI patients. 10. Wu D: Acupuncture and neurophysiol-
the cases of complete SCI, Dimitrijevic ogy. Clin Neurol Neurosurg 1990;92:13–25
et al.12,13 and Sherwood et al.14 pro- 11. Johansson K, Kindgren I, Windener
posed that some tracts are actually REFERENCES H, et al: Can sensory stimulation improve
“spared” with intact continuity of white the functional outcome in stroke pa-
1. Staas WE, Formal CS, Freedman MK, et
tients? Neurology 1993;43:2189 –92
matter across the lesion site. However, al: Spinal Cord Injury and Spinal Cord In-
jury Medicine: Rehabilitation Medicine 12. Dimitrijevic MR, Faganel J, Leh-
these tracts may become electrophysi-
Principles and Practice, ed 3. Philadelphia, mkuhl D, et al: Motor control in man
ologically silent and even progress to after partial or complete spinal cord in-
Lippincott-Raven, 1998, pp 1259 –91
cell death when cord injury is too se- jury. Adv Neurol 1983;39:915–26
vere.15–19 Acupuncture therapy, when 2. Wong MK, Chen CF, Lien IN: Evaluation
13. Dimitrijevic MR: Residual motor
of the result of rehabilitation for spinal cord
applied early in SCI, might hasten the function in spinal cord injury. Adv Neurol
injuries over a recent 10-year period. J For-
healing process in these tracts. 1988;47:138 –55
mos Med Assoc 1981;80:433– 41
The prognoses of neurologic and 14. Sherwood AM, Dimitrijevic MR,
3. Lee MHM, Liao SJ;: Acupuncture in
functional recoveries are known to be Mckay WB: Evidence of subclinical brain
physiatry, in Kottke FJ, Lehmann JF
influence in clinically complete spinal
poor in ASIA grade A SCI patients. (eds): Krusens Handbook of Physical
cord injury: Discomplete SCI. J Neurol
The study by Waters et al.20 reported Medicine and Rehabilitation, ed 4. Phila-
Sci 1992;110:90 – 8
that functional and neurologic recov- delphia, Saunders, 1990, pp 402–32
15. Kakulas BA: A review of the neuropa-
ery after acute SCI seems to be better 4. Bonnerman R: Acupuncture: The thology of human spinal cord injury with
in patients with higher muscle power World Health Organization view. World emphasis on special features. J Spinal
Health 1979;31:24 –29 Cord Med 1999;22:119 –24
and a lower level of cord injury. How-
ever, our results revealed that with 5. Politis MJ, Korchinski MA: Beneficial 16. Kakulas BA: The applied neuropa-
effects of acupuncture treatment follow- thology of human spinal cord injury. Spi-
early acupuncture therapy, signifi-
ing experimental spinal cord injury: A nal Cord 1999;37:79 – 88
cant neurologic and functional recov- behavioral, morphological, and biochem- 17. Little JW, Ditunno JF, Stiens SA, et
eries can be achieved even in patients ical study. Acupunct Electrother Res al: Incomplete spinal cord injury: Neuro-
with ASIA grade A, absent muscle 1990;15:37– 49 nal mechanisms of motor recovery and
power, and higher cord injuries. 6. Ran C, Ba S, Liu X, et al: Acupuncture hyperreflexia. Arch Phys Med Rehabil
treatment of spinal paraplegia with acu- 1999;80:587–97
points selected, basing on neuroanatomy. 18. Murray M: Strategies and mecha-
CONCLUSION World J Acupunct Mox 1992;2:3–9 nisms of recovery after spinal cord injury.
7. Wong AMK, Su TY, Tang FT, et al: Adv Neurol 1997;72:219 –25
The use of concomitant auricular
Clinical trial of electrical acupuncture on 19. Lu J, Waite P: Advances in spinal cord
acupuncture and electrical acupunc- hemiplegic stroke patients. Am J Phys regeneration. Spine 1999;24:926 –30
ture therapy through adhesive surface Med Rehabil 1999;78:117–22 20. Waters RL, Akins R, Yakura J, et al:
electrodes, when implemented early in 8. Cheng PT, Wong MK, Chang PL: A Functional and neurological recovery fol-
acute SCI, can contribute to significant therapeutic trial of acupuncture in neu- lowing acute spinal cord injury. J Spinal
neurologic and functional recoveries in rogenic bladder of spinal cord injured Cord Med 1998;21:195–9
January 2003 Acupuncture on Patients with SCI 27
You might also like
- YNSADocument8 pagesYNSAGracielle VasconcelosNo ratings yet
- The Acupuncture Prescription:: A Holistic Approach to HealthFrom EverandThe Acupuncture Prescription:: A Holistic Approach to HealthNo ratings yet
- Accupuncture Needle DepthDocument21 pagesAccupuncture Needle DepthStephen T LeNo ratings yet
- SULPYCO Method: A New Quantum and Integrative Approach to DepressionFrom EverandSULPYCO Method: A New Quantum and Integrative Approach to DepressionNo ratings yet
- Immortalizing Emotions: A Chinese Medicine perspective of TattoosFrom EverandImmortalizing Emotions: A Chinese Medicine perspective of TattoosNo ratings yet
- Earth Persona: Mnemonic Method an Informal Chinese Herbal GuidebookFrom EverandEarth Persona: Mnemonic Method an Informal Chinese Herbal GuidebookNo ratings yet
- Tran MentalactivityDocument33 pagesTran MentalactivityKiran JoshiNo ratings yet
- Ynsa Class PicDocument2 pagesYnsa Class PicGobinath SekarNo ratings yet
- Acupuncture As A FasciaDocument5 pagesAcupuncture As A Fasciacelliastt100% (1)
- 2008 Acupuncture Core Therapy - ToCDocument15 pages2008 Acupuncture Core Therapy - ToCdoktormin106100% (1)
- Setting Fire On The MountainDocument5 pagesSetting Fire On The MountainElizabeth Durkee NeilNo ratings yet
- Alchemical Facial Acupuncture Protocols, Part 3: by Mary Elizabeth Wakefield, Lac, Dipl. Ac., MS, MMDocument3 pagesAlchemical Facial Acupuncture Protocols, Part 3: by Mary Elizabeth Wakefield, Lac, Dipl. Ac., MS, MMHaryono zhuNo ratings yet
- Metabolic Disorders and Shen in Integrative Cardiovascular Chinese Medicine: Volume 7From EverandMetabolic Disorders and Shen in Integrative Cardiovascular Chinese Medicine: Volume 7No ratings yet
- Zhen Jiujia Yi JingDocument6 pagesZhen Jiujia Yi Jingsuperser123465No ratings yet
- Managing Pain: And Other Medically Proven Uses of AcupunctureFrom EverandManaging Pain: And Other Medically Proven Uses of AcupunctureNo ratings yet
- Poetry of the Body: Stories About Acupuncture PointsFrom EverandPoetry of the Body: Stories About Acupuncture PointsNo ratings yet
- Acupuncture Treatment PrinciplesDocument4 pagesAcupuncture Treatment PrinciplessoriboNo ratings yet
- Stop Suffering from Arthritis: Tcm Can Help YouFrom EverandStop Suffering from Arthritis: Tcm Can Help YouNo ratings yet
- 2017 Acupuncture For Chronic PainDocument49 pages2017 Acupuncture For Chronic Painvera100% (1)
- ScoliosisDocument9 pagesScoliosisexcalidorNo ratings yet
- Advanced Clinical Therapies in Cardiovascular Chinese MedicineFrom EverandAdvanced Clinical Therapies in Cardiovascular Chinese MedicineNo ratings yet
- Acupuncture For AsthmaDocument16 pagesAcupuncture For AsthmaRichard SiahaanNo ratings yet
- Anatomy and Physiology For The Acupuncturist "Made Easy"From EverandAnatomy and Physiology For The Acupuncturist "Made Easy"Rating: 5 out of 5 stars5/5 (1)
- Hematology in Traditional Chinese Medicine CardiologyFrom EverandHematology in Traditional Chinese Medicine CardiologyNo ratings yet
- Acupuncture For Acute Management and Rehabilitation of Traumatic Brain InjuryDocument10 pagesAcupuncture For Acute Management and Rehabilitation of Traumatic Brain InjuryTomas MascaroNo ratings yet
- Cham Cuu Dong Thi Dieu Tri CA Benh KhoDocument111 pagesCham Cuu Dong Thi Dieu Tri CA Benh KhoTrieu VuongNo ratings yet
- Secrets of the Hidden Vessels: Explains how Chinese acupuncture works in terms Western readers can understandFrom EverandSecrets of the Hidden Vessels: Explains how Chinese acupuncture works in terms Western readers can understandRating: 5 out of 5 stars5/5 (1)
- Acupuncture Pulse Diagnosis and the Constitutional Conditional ParadigmFrom EverandAcupuncture Pulse Diagnosis and the Constitutional Conditional ParadigmNo ratings yet
- Pain Management by AcupunctureDocument72 pagesPain Management by AcupunctureAna RacovitaNo ratings yet
- Acupuncture For Memory LossDocument3 pagesAcupuncture For Memory Losspeter911xNo ratings yet
- Prescriptions for Virtuosity: The Postcolonial Struggle of Chinese MedicineFrom EverandPrescriptions for Virtuosity: The Postcolonial Struggle of Chinese MedicineNo ratings yet
- Neuropuncture™ Case Studies and Clinical Applications: Volume 1From EverandNeuropuncture™ Case Studies and Clinical Applications: Volume 1No ratings yet
- Acupuncture Bell's Palsy RecoveryDocument7 pagesAcupuncture Bell's Palsy RecoveryJk SalvadorNo ratings yet
- Diaphragmatic Reactivity and Stress ReactionsDocument10 pagesDiaphragmatic Reactivity and Stress Reactionsmamun31No ratings yet
- 促脈 Cu Mai Abrupt Skipping HastyDocument3 pages促脈 Cu Mai Abrupt Skipping HastyEthan KimNo ratings yet
- Acupuncture Today and in Ancient China: Explains How Chinese Acupuncture Works in Terms Western Readers Can UnderstandFrom EverandAcupuncture Today and in Ancient China: Explains How Chinese Acupuncture Works in Terms Western Readers Can UnderstandNo ratings yet
- Abdominal Acupuncture IntroductionDocument4 pagesAbdominal Acupuncture Introductionhellsin666100% (1)
- Formulae of TMCDocument480 pagesFormulae of TMCcarlo radaoniNo ratings yet
- EJOM-9.5.final - A.BruchDocument10 pagesEJOM-9.5.final - A.Bruchmarcia yadavNo ratings yet
- GlaucomaDocument6 pagesGlaucomaratamanoNo ratings yet
- Physiological Basis of Acupuncture TherapyDocument6 pagesPhysiological Basis of Acupuncture Therapydrak44No ratings yet
- Micro Current CobraDocument3 pagesMicro Current CobraDarren Starwynn100% (1)
- Yang Motility Vessel Acupuncture PointsDocument5 pagesYang Motility Vessel Acupuncture Pointsلوليتا وردةNo ratings yet
- Compilation Conditions + FormulasDocument2 pagesCompilation Conditions + Formulaspeter911x0% (1)
- Acupuncture: Ancient Treatment For Modern IllnessesDocument31 pagesAcupuncture: Ancient Treatment For Modern IllnessesJessica PaulNo ratings yet
- In Demand: The Health Professionals Guide to a Winning PracticeFrom EverandIn Demand: The Health Professionals Guide to a Winning PracticeNo ratings yet
- AJACM 2011 6 1 Wang Juyi Interview Part 2 of 2 - LiuDocument4 pagesAJACM 2011 6 1 Wang Juyi Interview Part 2 of 2 - LiuYagtaliNo ratings yet
- Japanese DiagnosisDocument1 pageJapanese DiagnosisMed AliNo ratings yet
- Pta 236 Kines I o TapingDocument17 pagesPta 236 Kines I o TapingPedro GouveiaNo ratings yet
- Paraplegic AcupunctureDocument7 pagesParaplegic AcupunctureMed AliNo ratings yet
- KneeDocument1 pageKneeMed AliNo ratings yet
- Acupuncture ChartsDocument7 pagesAcupuncture ChartsAifaa A GhaniNo ratings yet
- Outsmart Pain E-BookDocument69 pagesOutsmart Pain E-BookMed AliNo ratings yet
- AcupointDocument1 pageAcupointMed AliNo ratings yet
- DR Tan NeedlingDocument1 pageDR Tan NeedlingMed AliNo ratings yet
- Facial Acupuncture Seminar NotesDocument23 pagesFacial Acupuncture Seminar NotesNilton100% (11)
- Dr. Tan's Balance MethodDocument0 pagesDr. Tan's Balance MethodHarijan Fernandez88% (16)
- Five ElementsDocument2 pagesFive Elementskadokanaikidoka100% (3)
- BeinDocument16 pagesBeinMed AliNo ratings yet
- Dr. Tan's Balance MethodDocument0 pagesDr. Tan's Balance MethodHarijan Fernandez88% (16)
- Case 3 - Sinus HeadacheDocument6 pagesCase 3 - Sinus HeadacheJohn FightakisNo ratings yet
- DR - Cantor's Longevity DietDocument248 pagesDR - Cantor's Longevity DietKenyaReyes67% (3)
- Neuromuscular Facilitation Techniques: Miss Rojaramani Vasamshetty MPT Ii YrDocument24 pagesNeuromuscular Facilitation Techniques: Miss Rojaramani Vasamshetty MPT Ii YrdeepuphysioNo ratings yet
- ADR UzbekistanDocument80 pagesADR UzbekistanJose Juan Velazquez GarciaNo ratings yet
- Case Study On Observation and Newborn CareDocument38 pagesCase Study On Observation and Newborn CarePiyush Dutta100% (2)
- ShaylaDocument3 pagesShaylaapi-530728661No ratings yet
- Unit - 10 - General Characters and Classification of Fungi by Dr. Kirtika PadaliaDocument38 pagesUnit - 10 - General Characters and Classification of Fungi by Dr. Kirtika PadalianucleophilicmishraNo ratings yet
- Terminologia LatinaDocument7 pagesTerminologia LatinaКонстантин ЗахарияNo ratings yet
- Stallard's eye surgery pdf free download guideDocument3 pagesStallard's eye surgery pdf free download guideCod Mobile100% (1)
- Biology 10Th Edition Raven Test Bank Full Chapter PDFDocument36 pagesBiology 10Th Edition Raven Test Bank Full Chapter PDFlewis.barnes1000100% (12)
- Balanced Diet: Includes Foods From All Food Groups During The DayDocument19 pagesBalanced Diet: Includes Foods From All Food Groups During The DayMayuri VohraNo ratings yet
- Ebr MacalolotDocument4 pagesEbr Macalolotquen.chuaNo ratings yet
- CretDocument63 pagesCretMtpa MashoorNo ratings yet
- Canine Disobedient, Unruly and ExcitableDocument5 pagesCanine Disobedient, Unruly and ExcitableBrook Farm Veterinary CenterNo ratings yet
- Annual Health Checkup (Executive) : Package Amt. Package Actual AmtDocument1 pageAnnual Health Checkup (Executive) : Package Amt. Package Actual AmtPAWAN KUMARNo ratings yet
- Material Safety Data Sheet: 1. Chemical Product and Company IdentificationDocument7 pagesMaterial Safety Data Sheet: 1. Chemical Product and Company IdentificationKun Adi ReksatamaNo ratings yet
- Vet Tech ExamDocument39 pagesVet Tech Examransingh100% (1)
- Answers To Questions:: Analysis of SalivaDocument2 pagesAnswers To Questions:: Analysis of Salivaerisseval14No ratings yet
- Karthik Covid Report 1295Document1 pageKarthik Covid Report 1295Karthikeya PuttaguntaNo ratings yet
- Census August 8 - August 9, 2020Document6 pagesCensus August 8 - August 9, 2020Patrick JohnNo ratings yet
- TIME Magazine December 1Document99 pagesTIME Magazine December 1rathneshkumar100% (2)
- VSL TB Workplace Policy ProgramDocument3 pagesVSL TB Workplace Policy ProgramAlexander John AlixNo ratings yet
- Vicorder PWA-PWV Pres 15-04 EnglDocument79 pagesVicorder PWA-PWV Pres 15-04 EnglHatem FaroukNo ratings yet
- Archer (Staphylococcus Aureus)Document3 pagesArcher (Staphylococcus Aureus)_meiantiNo ratings yet
- Hipospadia, PPT Blok 3.1 (English)Document11 pagesHipospadia, PPT Blok 3.1 (English)weniNo ratings yet
- Abdominal ExaminationDocument14 pagesAbdominal ExaminationValeria Guerra CastilloNo ratings yet
- Basics of Microvascular SurgeryDocument33 pagesBasics of Microvascular SurgeryPratikshya KothiaNo ratings yet
- Allele-specific expression of variant-specific surface proteins in Giardia lambliaDocument7 pagesAllele-specific expression of variant-specific surface proteins in Giardia lambliawiwienNo ratings yet
- AmavataDocument14 pagesAmavataSamhitha Ayurvedic ChennaiNo ratings yet
- Neuro NihstrokescaleDocument1 pageNeuro NihstrokescaleVictorine Levana PudjiadiNo ratings yet
- Bulimia NervosaDocument17 pagesBulimia NervosaJheanAlphonsineT.Means100% (1)