Professional Documents
Culture Documents
29 Hand Hygiene Jun04
Uploaded by
skittypieOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
29 Hand Hygiene Jun04
Uploaded by
skittypieCopyright:
Available Formats
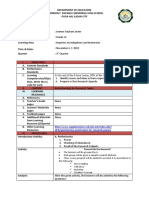
ISSN 1449-440X
Issue No. 29
June 2004
Promoting Evidence-Based Nursing Practice:
Redifining Community Based Infection Control: Hand Hygiene
Introduction facilities available in client’s homes (Gould, 2000).
Historically, washing one’s hands before and after A clinical audit conducted by Kenny (2002), a District
patient/client contact has proved to be beneficial in Nurse from Royal District Nursing Service (RDNS) of
reducing the transmission of infections. In the 19th SA Inc. found that hand hygiene was below best
century, hand hygiene evolved thanks to some practice. Most nurses used medi prep wipes or pre-
physicians; Philip Semmelweis, Louis Pasteur and used bar soaps (Kenny, 2002) and this was not
Joseph Lister all linked the transmission of considered as best practice. As suggested by previous
microorganisms to unwashed hands. Semmelweiss studies, lack of adequate hand washing facilities (clean
introduced washing hands in chlorine water, Lister hand towel or paper towel, and liquid soap) were
instituted hand washing with carbolic acid (Manza et al, reasons for poor hand hygiene. Kenny (2002)
1987). Recent statistics show us that hand hygiene is recommended that hand hygiene practice required
the single most important measure in preventing the review and that the use of a portable kit or waterless
spread of infection. hand hygiene product be implemented and evaluated.
However, most people still do not wash hands In October 2002 the Center for Disease Control
appropriately. A survey of more than 2000 people found released its “Guidelines for Hand Hygiene in Health-
that 31% of men and 17% of women confessed to not Care Setting” which comprises recommendations by the
washing hands after going to the toilet. One in five said Hand Hygiene Task Force. This comprehensive
they did not bother washing their hands because they document explores all aspects of hand hygiene,
looked clean: including history, transmission, compliance and
The next time you meet someone and shake their recommendations. One paper examined transmission
hand – there’s a one in five chance that they are one of of gram-negative bacilli and found that even after hand
those who do not always wash their hands after going to washing with soap and water the organisms were still
the toilet (Pennington H A. June 11th 2001) transferred to another site and that washing with soap
Germs are cited as being the enemy and hiding on and water failed to remove pathogens from hands and
every surface, just waiting to make you sick. The increased the chances of skin irritation and dryness.
highest risks of transmitting germs are on hands. This study also found that an alcohol based hand rub
Something so simple as shaking hands with people can can prevent the transmission of pathogens more
transmit bacteria (Germworld web site). effectively than handwashing with soap and water.
Gram-negative bacilli were transferred to another site
Searching for evidence via hands of nurses in only 17% of cases where an
Hand hygiene is considered the leading measure to alcohol based hand rinse was used and 92%
reduce infection in healthcare settings (Pittet et al transference where soap and water was used (Boyce et
2001). Best practice hand washing should include al 2002). In addition, authors claimed that frequent use
removing jewellery, wetting hands thoroughly and then of alcohol-based formulations can cause drying of the
lather vigorously using a pH neutral liquid soap for a skin unless emollients or other skin conditioning agents
duration of fifteen seconds. The hands should then be are added to the product. In recent trials alcohol based
rinsed under running water, taps turned off with paper gels containing emollients caused less skin irritation
or clean towel (National Guidelines Communicable and dryness than soap and water and is less damaging
Diseases Network. Draft 2002). This practice refers to to the skin than soap and water (Winnefeld 2000; Boyce
hand washing in the acute care sector. In the same et al 2000). Pittet (2001) concluded that alcohol-based
guidelines it is suggested that community health care hand rubs compared with traditional handwashing (soap
workers may use single-use towelettes (with detergent) and water) is better practice because it required less
before an alcoholic handrub. Hands should then be time, acted faster and irritated hands less often and
washed as soon as possible with liquid soap and finally that alcohol-based rubs resulted in sustained
running water at the first opportunity. Pittet (2000) improvement in hand hygiene compliance associated
suggests that hand washing is not sufficiently with decreased infection rates.
recognized by healthcare workers as best practice and
that compliance with recommended hand washing Implementing evidence based practice
guidelines is unacceptably (Pittet, 2000). McGuckin In 2003 RDNS (SA), under the umbrella of ‘Year of
(1999) found that hand washing still occurs in only half Clinical Focus’, selected infection control as the first
the instances and for a shorter time than clinical risk strategy to undergo review and revision. A
recommended. In a community study, Gould found that project officer (the author) was funded for three months
community nurses washed hands with soap and water to develop a framework for an infection control program
only 53% of 125 visits and with water 21% of the visits. and an implementation strategy. As part of this
Reasons cited were environmental conditions such as program, it was decided to explore the introduction of a
lack of clean towels, hand gel or clean unused soap waterless hand hygiene product with community nursing
which significantly impacted on the nurses’ ability to staff. District Nurses are aware that hand washing
comply with best practice guidelines for hand hygiene. deters transmission of bacteria but they do not always
In short, these authors found that community nurses have access to clean bathroom facilities in peoples’
were likely to encounter problems following hand homes. Therefore, what can district nurses do to ensure
hygiene guidelines because of the dependence on the their hands are clean? Fortunately several waterless
alcohol based hand hygiene products are now available preference, should RDNS provide the product, any
but it was important to consider the cost, portability and concerns/issues to be considered and whether the
product acceptance by staff when choosing the right product should be recommended. The results were
product. In 2003 a trial of two waterless alcohol based analyzed manually.
hand rubs was undertaken in RDNS (SA).
Summary of findings
Trial of two waterless alcohol based hand rubs Most nurses (69%) preferred product A, whilst 19%
Twenty four (24) RDNS nurses participated in a two preferred product B and 12% had no preference. Eighty
week trial of two alcohol based, waterless hand gels. percent of respondents felt that their hands were
There was concern with transporting liquid alcohol cleaner after using the gels. Following the results of this
products in a car in summer due to its flammable nature trial, it was highly recommended that Product A (Aquim)
and that a liquid would pose a safety concern if spilt on be provided as a product for hand hygiene in practice.
the floor. Clearance was given by the safety manager. Issues considered were cost, effect of heat or cold if left
The product also had to be available in pocket size so it in the car, education, compliance, losing bottles in the
could be readily carried in nurse’s pockets. Two house or car, potential for reactions, allergies or dry
companies (who prefer to remain nameless) had alcohol skin. The use of the hand gel ensures that nurses have
based gel available in pocket size and agreed to supply the opportunity to use a product that has been
the product for the trials. The products were available in developed specifically for hand hygiene.
100ml and 70ml size. Three other companies were
contacted for products that fitted the criteria (pocket size Conclusions
and gel); however none had products that were suitable. Anecdotal evidence demonstrates that many nurses
Two products, A and B, were selected. are reluctant to use soap and towels provided by
Participating nurses were given a short education clients. This is especially an issue when nurses have
program about hand hygiene and the use of gels prior to sensitive skin and are reluctant to expose their hands to
commencement of the trial. Content of these education a variety of soaps and detergents. The use of hand gel
programs was - overview of hand hygiene, transmission ensures that nurses have the opportunity to use a
and prevention of pathogens, how and when to use the product that has been designed specifically for hand
gel and provision of laminated instructions. Nurses were hygiene.
asked to use the product before and after any client This small project has raised hand washing
contact or procedure and that hands needed to be awareness amongst nurses, particularly those who
washed with soap and water if visibly soiled. were involved in the trial. It is hoped that information in
Two tools were developed for the trial hand hygiene this newsletter will provide the stimulus for nurses to
survey (tool 1) and a final and hygiene survey (tool 2). consider the evidence provided by the literature and the
The tools were designed by the trial coordinators and project. The literature available on hand hygiene and
adapted from a similar tool used by a large public compliance demonstrates that hand hygiene needs to
hospital. be addressed in all health care institutions - this
Nurses were asked to use product A continuously includes community based organizations.
for five days (Monday to Friday). Evening, night and References
weekend staff were excluded from the trial for ease of Boyce, JM, Pittet, D. (2002). Guideline for Hand Hygiene in Health Care
Settings – Centre for Disease Control & Prevention . October 25th Vol. 51. No.
administration, observation and availability of advice RR-16
and provisions. A questionnaire was then completed. Communicable Diseases Network. (Draft 2002) Infection Control
and returned to the trial coordinators. The following Guidelines for the prevention of transmission of infectious diseases in the health
care setting, version 3. Commonwealth of Australia
week, Product B was then used continuously for five Gould D, Gammon, J, Donnelly M (2000). Improving Hand Hygiene in
days and the same questionnaire completed. A final Community Healthcare Settings: the impact of research & clinical collaboration.
Journal of Clinical Nursing. Vol. 9 (1), pp.95-102.
questionnaire was then completed providing information Kenny B. (2001). Hand Washing & Community Nursing. ACCNS Journal
about preference and any issues. for Community Nurses. Vol.7, No.2. August.
Manza RJ, Oesting H. (1987) Handwashing: Re-examining the Ritual.
Tool 1 was used during the first week with product Journal of Practical Nursing. September.
A. It contained a brief explanation of the trial and the McGuckin M, Waterman R et al.(1999. Patient Education Model for
products and when to complete the tool. Twenty increasing Handwashing Compliance. American Journal of Infection Control.
27:30, pp. 9-14.
questions were asked and included the condition of Pittet, D. (2001). Improving Adherence to Hand Hygiene Practice: A
nurse’s hands prior to and after using the product, use Multidisciplinary Approach. Emerging Infectious Diseases. Vol. 7. No. 2, March-
April, pp. 234-240.
of moisturiser, glove use, convenience of the product, Pittet, D. (2000). Improving Compliance with Hand Hygiene in Hospital.
and whether the nurse would recommend using the Infection Control & Hospital Epidemiology.. Vol.21. No. 6. pp. 381-385.
Pittet, D, Boyce JM. (2001). Hand Hygiene & Patient Care: pursuing the
product. The tool was designed for ease and quick Semmelweis theory. The Lancet – Infectious Disease. April. pp. 9-20.
completion using true/false answers. Comments were Rosenheimer L. (1995) Establishing a surveillance system for infections
invited if the nurses wished to do so. Tool 1 was again acquired in home healthcare. Home Healthcare Nurse. Vol. 13. No.3. pp. 20-
26
used the second week following the use of the second (http://news.bbc.co.uk/1/hi/health/1378634 )
product, product B. http://www.securityworld.com/library/health/germwar.html) In another web
site called Security World – The Education Site, an article titled “The Germ
After the second week, nurses were asked to War”,
complete a final survey (tool 2) consisting of five items. (http://news.bbc.co.uk/1/hi/health/1378634 ) Pennington H A BBC Health
web site (Monday, 11th June 2001), titled “Dirty hands poison thousands”
These questions required a written answer and included
questions on problems with both products, product
This issue written by Linda Hayford (RN, Grad Cert Infection Control).
Edited by Dr Debbie Kralik, Professor Tina Koch and Natalie Howard, RDNS Research Unit.
The Research Unit is proudly supported by the RDNS Foundation
Contact Details: Research Coordinator, RDNS Research Unit, PO Box 247, GLENSIDE SA 5065, Ph: (08) 8206 0111,
Fax (08) 8206 0010, Email: howard.natalie@rdns.sa.gov.au, Web: http://www.rdns.net.au (newsletter available on website)
© Copyright (2004) RDNS Research Unit, Adelaide, South Australia This work is copyright. Apart from any use as permitted under the copyright act 1968, no part of this
work may be reproduced by means electronic or otherwise without the permission of the copyright holders.
You might also like
- Chapter 2 HandwashingDocument18 pagesChapter 2 HandwashingMylene Valdez50% (2)
- Replace Hand Washing With Use of A Waterless Alcohol Hand Rub?Document2 pagesReplace Hand Washing With Use of A Waterless Alcohol Hand Rub?Angela NeriNo ratings yet
- Hand Hygiene Handout PDFDocument32 pagesHand Hygiene Handout PDFms RN100% (1)
- Hand drying reviewDocument12 pagesHand drying reviewHima Muchlashin AlBathyNo ratings yet
- Hand HygieneDocument39 pagesHand HygienearingkinkingNo ratings yet
- The Effectiveness of Using A Sanitizer As A Preventive Measure in CovidDocument11 pagesThe Effectiveness of Using A Sanitizer As A Preventive Measure in CovidNicole MargaretteNo ratings yet
- CHAPTER 1pusaDocument4 pagesCHAPTER 1pusaJimwel EstebanNo ratings yet
- G H H H - C S: R H I C P A C Hicpac/Shea/Apic/Idsa H H T FDocument39 pagesG H H H - C S: R H I C P A C Hicpac/Shea/Apic/Idsa H H T FAbidi HichemNo ratings yet
- Discuss SassyDocument4 pagesDiscuss SassySisanda DalasileNo ratings yet
- Hand Wash GuideDocument10 pagesHand Wash GuideUchi Nurul FauziahNo ratings yet
- Hand Hygiene: Protocol For UWS ClinicsDocument8 pagesHand Hygiene: Protocol For UWS ClinicsOliaNo ratings yet
- Hand Hygiene Review Highlights Alcohol Rub BenefitsDocument8 pagesHand Hygiene Review Highlights Alcohol Rub Benefitsdebby claudiNo ratings yet
- Literature Review HandwashingDocument6 pagesLiterature Review Handwashingaflsbegdo100% (1)
- Hand HygieneDocument6 pagesHand HygieneCarolWestinghouseNo ratings yet
- Paghuhugas NG TamaDocument31 pagesPaghuhugas NG TamaJustin BacaniNo ratings yet
- Wizzy ProjectDocument21 pagesWizzy ProjectOlawale GabrielNo ratings yet
- Con VizerDocument39 pagesCon VizerUrbana RaquibNo ratings yet
- GenericDocument25 pagesGenericmikeysiopaoNo ratings yet
- Hand SanitizerDocument21 pagesHand SanitizerVitalis MbuyaNo ratings yet
- Artikel 4Document7 pagesArtikel 4Iale JasmineNo ratings yet
- AbstractDocument3 pagesAbstractCircuits BazaarNo ratings yet
- NURS1002-Berman Audrey-Skills in Clinical Nursing-Section 12 Hand Hygiene-Pp6-11Document87 pagesNURS1002-Berman Audrey-Skills in Clinical Nursing-Section 12 Hand Hygiene-Pp6-11dannyrorke9530No ratings yet
- Improving Hand Hygiene Compliance in HospitalsDocument5 pagesImproving Hand Hygiene Compliance in Hospitalskencheen100% (1)
- QLD Health HandwashingDocument10 pagesQLD Health HandwashinggregraynerNo ratings yet
- Performing Hand HygieneDocument4 pagesPerforming Hand HygieneVANTAE 9495No ratings yet
- Review of Related LiteratureDocument4 pagesReview of Related LiteraturePopoyNo ratings yet
- Review of Related LiteratureDocument4 pagesReview of Related LiteraturePopoyNo ratings yet
- Review of Related LiteratureDocument4 pagesReview of Related LiteraturePopoyNo ratings yet
- Hand Hygiene IdaDocument7 pagesHand Hygiene IdaOem Boed ColectionNo ratings yet
- Hand Hygine Guideline WHODocument365 pagesHand Hygine Guideline WHOvinnyNo ratings yet
- American Journal of Infection ControlDocument5 pagesAmerican Journal of Infection ControlAchmad LatiefNo ratings yet
- Guide To Infection Control in The Hospital: Hand HygieneDocument11 pagesGuide To Infection Control in The Hospital: Hand HygieneSlepy chngNo ratings yet
- APIC Hand WashingDocument18 pagesAPIC Hand WashingKshitij BasavrajNo ratings yet
- Pico HandwashingDocument21 pagesPico HandwashingAnonymous gkInz9No ratings yet
- Comparative Assessment of Antimicrobial Efficacy of Different HandDocument8 pagesComparative Assessment of Antimicrobial Efficacy of Different HandLe Vu Ky NamNo ratings yet
- Myco R. Garces BSN - 4B Hand Washing, Alcohol-Based Rubs Help Curb Influenza OutbreaksDocument3 pagesMyco R. Garces BSN - 4B Hand Washing, Alcohol-Based Rubs Help Curb Influenza OutbreaksMyco Reyes GarcesNo ratings yet
- Hand Hygiene: Simple and Complex: P.A. JumaaDocument12 pagesHand Hygiene: Simple and Complex: P.A. Jumaafarida nur ainiNo ratings yet
- Hand Hygiene WhoDocument286 pagesHand Hygiene WhoNIKO SARDYNo ratings yet
- WHO Hand Hygiene GuidelinesDocument270 pagesWHO Hand Hygiene GuidelinesAnonNo ratings yet
- Ef Ficacy of Alcohol-Based Hand Sanitizer On Hands Soiled With Dirt and Cooking OilDocument5 pagesEf Ficacy of Alcohol-Based Hand Sanitizer On Hands Soiled With Dirt and Cooking OilAbimanyuMuhammadNo ratings yet
- HH - DR FrankaDocument25 pagesHH - DR FrankaHannan AliNo ratings yet
- Effectiveness of Glycerin and Lemon in Making Hand SanitizerDocument10 pagesEffectiveness of Glycerin and Lemon in Making Hand SanitizerGAIL BARBINo ratings yet
- The Problem and Its Setting: "Hand Washing Is Associated With Voluntary Individualistic Behavior." Dean David HolyoakeDocument3 pagesThe Problem and Its Setting: "Hand Washing Is Associated With Voluntary Individualistic Behavior." Dean David HolyoakeKathleen Camille ManiagoNo ratings yet
- Health Care Workers' Hand Contamination Levels and Antibacterial EfficacyDocument4 pagesHealth Care Workers' Hand Contamination Levels and Antibacterial EfficacyHùng Nguyễn ViệtNo ratings yet
- Alcohol hand rubs may increase hand hygiene complianceDocument2 pagesAlcohol hand rubs may increase hand hygiene complianceJihadul IslamNo ratings yet
- Low-Cost Automatic Alcohol Sanitizer DispenserDocument11 pagesLow-Cost Automatic Alcohol Sanitizer DispenserDave Matthew LibiranNo ratings yet
- 0811 Hand Disinfectant and COVID-19Document54 pages0811 Hand Disinfectant and COVID-19Henrico ImpolaNo ratings yet
- REFERENCIA AIRE PARA SECADO DE MANOSDocument10 pagesREFERENCIA AIRE PARA SECADO DE MANOSLeticia GallardoNo ratings yet
- Arrabaca - Prelim Journal - CPHDocument6 pagesArrabaca - Prelim Journal - CPHREXINNE GLARIAN ARRABACANo ratings yet
- Hand Washing Prevents Disease SpreadDocument38 pagesHand Washing Prevents Disease Spreadgowon love odiriNo ratings yet
- Experiment #6 - Effectiveness of HandwashingDocument8 pagesExperiment #6 - Effectiveness of HandwashingFrancis MagbitangNo ratings yet
- Sdarticle 4Document11 pagesSdarticle 4edwinmadrigal6268No ratings yet
- Hygienic Handrub. Treatment of Hands With An Antiseptic: Historical Perspective On Hand Hygiene in Health CareDocument11 pagesHygienic Handrub. Treatment of Hands With An Antiseptic: Historical Perspective On Hand Hygiene in Health CareOvieNo ratings yet
- GHP 2020 Handwashing Research SummaryDocument12 pagesGHP 2020 Handwashing Research SummaryPeter OkohNo ratings yet
- 2 Hand HygieneDocument44 pages2 Hand HygieneAdelina SilimonNo ratings yet
- Assessment of Alcohol-Based Hand Sanitizers For Long-Term Use, Formulated With Addition of Natural Ingredients in Comparison To WHO Formulation 1Document16 pagesAssessment of Alcohol-Based Hand Sanitizers For Long-Term Use, Formulated With Addition of Natural Ingredients in Comparison To WHO Formulation 1QualityMattersNo ratings yet
- Hand HygieneDocument11 pagesHand HygieneSourabh MishraNo ratings yet
- Global Handwashing Day Planner's Guide Promotes Life-Saving Hygiene HabitsDocument48 pagesGlobal Handwashing Day Planner's Guide Promotes Life-Saving Hygiene HabitsAria BimaNo ratings yet
- How to Make Homemade Hand Sanitizer: Simple and Straightforward Home Recipes for a Healthy Life and FamilyFrom EverandHow to Make Homemade Hand Sanitizer: Simple and Straightforward Home Recipes for a Healthy Life and FamilyNo ratings yet
- Hand Sanitizers and Disinfectants Homemade Recipes For Protecting You & Your FamilyFrom EverandHand Sanitizers and Disinfectants Homemade Recipes For Protecting You & Your FamilyNo ratings yet
- Id Brainstorming-Good-Topics-For-Research-Papers: Present Me The Research!Document2 pagesId Brainstorming-Good-Topics-For-Research-Papers: Present Me The Research!JOEMAR JAVIERNo ratings yet
- IAL Timetable (Jan 2022) - Students (Dec. 22)Document1 pageIAL Timetable (Jan 2022) - Students (Dec. 22)Distance From LoveNo ratings yet
- ClarificationDocument107 pagesClarificationDebasis Das100% (1)
- Philippine Contemporary MusicDocument7 pagesPhilippine Contemporary MusicFLYFLY SEVENTEENNo ratings yet
- Effective Reading Instruction PhasesDocument4 pagesEffective Reading Instruction Phaseshawa ahmedNo ratings yet
- Miss Agnes PaperDocument5 pagesMiss Agnes Paperlambma04No ratings yet
- African Union Teacher Prize PPT v1Document10 pagesAfrican Union Teacher Prize PPT v1jennita boyjonauthNo ratings yet
- Easter Printable PDFDocument34 pagesEaster Printable PDFMotronea Ioan100% (1)
- SITXCCS007 Enhance Customer Service Experiences Student Guide Oct UpdateDocument93 pagesSITXCCS007 Enhance Customer Service Experiences Student Guide Oct Updatesumandeep67% (3)
- C-BSU - at Admission Requirement - 0Document6 pagesC-BSU - at Admission Requirement - 0DanielleSarahCacheroNo ratings yet
- Schedule of PresentationDocument8 pagesSchedule of PresentationSherwin FernandoNo ratings yet
- My Portfolio: Marie Antonette S. NicdaoDocument10 pagesMy Portfolio: Marie Antonette S. NicdaoLexelyn Pagara RivaNo ratings yet
- Build Business Models Sample Syllabus 40chDocument0 pagesBuild Business Models Sample Syllabus 40chlilbouyinNo ratings yet
- Effectiveness of Institutional Student Programs and Services of Sdssu-Lianga Campus A.Y. 2020-2021Document44 pagesEffectiveness of Institutional Student Programs and Services of Sdssu-Lianga Campus A.Y. 2020-2021Mary Mae LlorenteNo ratings yet
- Distance Learning Project Management Courses (PGDPM) - MIT Pune IndiaDocument2 pagesDistance Learning Project Management Courses (PGDPM) - MIT Pune IndiaDistance MbaNo ratings yet
- Notes On MBA SAF Completion - 2023Document3 pagesNotes On MBA SAF Completion - 2023gtNo ratings yet
- Classroom Management and Organization PDFDocument27 pagesClassroom Management and Organization PDFDaniela Soares100% (1)
- Draft HJRS Promtion Policy v2Document5 pagesDraft HJRS Promtion Policy v2Arsalan SidikiNo ratings yet
- Toyota's 5-Step Process for Continuous Improvement ImplementationDocument6 pagesToyota's 5-Step Process for Continuous Improvement Implementationdbryant1435100% (1)
- Ton Duc Thang University Experience Report: Members: Lê Anh ThưDocument10 pagesTon Duc Thang University Experience Report: Members: Lê Anh ThưThư LêNo ratings yet
- FORM 138 Kto12 ElementaryDocument2 pagesFORM 138 Kto12 ElementaryKat Causaren Landrito0% (1)
- THỰC HÀNH CHUYÊN ĐỀ TRỌNG ÂMDocument3 pagesTHỰC HÀNH CHUYÊN ĐỀ TRỌNG ÂMNguyen Viet LovesUlisNo ratings yet
- Israeli Ethiopian Mothers Perceptions of Their Children S Mild MDocument231 pagesIsraeli Ethiopian Mothers Perceptions of Their Children S Mild MifriqiyahNo ratings yet
- Access MBA Guide PDFDocument175 pagesAccess MBA Guide PDFjulita rachmadewiNo ratings yet
- KGH BenefitsDocument6 pagesKGH BenefitscapiNo ratings yet
- Art of Design v2Document337 pagesArt of Design v2lintodd100% (1)
- Sped Teacher IPCRFDocument8 pagesSped Teacher IPCRFprincess delin pasuquin100% (2)
- Intercultural MarketingDocument25 pagesIntercultural MarketingShilpi ChandaNo ratings yet
- Dr. Manzoor Ilahi's prescription for Lohith Vakada's skin conditionDocument1 pageDr. Manzoor Ilahi's prescription for Lohith Vakada's skin conditionlohit dummyNo ratings yet
- Transportation Alphabet PDFDocument27 pagesTransportation Alphabet PDFAprendendo a Aprender Inglês com a TassiNo ratings yet