Professional Documents
Culture Documents
Different Types of Radiation Prostheses To Minimize Radiation Side
Uploaded by
Ahmad ShoeibOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Different Types of Radiation Prostheses To Minimize Radiation Side
Uploaded by
Ahmad ShoeibCopyright:
Available Formats
See
discussions, stats, and author profiles for this publication at:
https://www.researchgate.net/publication/306065781
DIFFERENT TYPES OF RADIATION
PROSTHESES TO MINIMIZE RADIATION
SIDE
Article in International Journal of Current Research · June 2016
CITATIONS READS
0 444
6 authors, including:
Jayant N. Palaskar Jyoti Himmatrao Wankhade
Sinhgad Technical Education Society Sinhgad Technical Education Society
35 PUBLICATIONS 46 CITATIONS 2 PUBLICATIONS 0 CITATIONS
SEE PROFILE SEE PROFILE
Some of the authors of this publication are also working on these related projects:
Centric relation View project
All content following this page was uploaded by Jayant N. Palaskar on 12 August 2016.
The user has requested enhancement of the downloaded file.
z
Available online at http://www.journalcra.com
INTERNATIONAL JOURNAL
OF CURRENT RESEARCH
International Journal of Current Research
Vol. 8, Issue, 06, pp.33575-33578, June, 2016
ISSN: 0975-833X
RESEARCH ARTICLE
DIFFERENT TYPES OF RADIATION PROSTHESES TO MINIMIZE RADIATION SIDE
SIDE-EFFECTS
1Dr. Jayant Palaskar, *,1Dr. Zankhana S. Mody, 2Dr. Shreyas S. Mohile, 1Dr. Jyoti H. Wankhade,
1Dr. Sayali R. Korde and 1Dr. Nikita M. Virdiya
1Department of Prosthodontics and Crown & Bridge, Sinhgad Dental College and Hospital, Pune
2Department of Oral and Maxillofacial Surgery, Dr. D.Y PatilVidyapeeth’s, Dr. D.Y Patil Dental College and
Hospital, Pimpri, Pune
ARTICLE INFO ABSTRACT
Radiation prosthesis is an artificially fabricated device that aids in the efficient administration of radiotherapy to
Article History: the affected areas and thereby helps in limiting post radiotherapy complications. Radiotherapy is being used as an
th
Received 24 March, 2016 adjunctive form of treatment in the management of head and neck cancer. Adverse tissue reactions are associated
Received in revised form with the use of radiotherapy in the management of patients with head and neck cancer. These reactions are painful
06th April, 2016 and they diminish the quality of life, often discouraging the patient from taking treatment. A prosthodontist can
Accepted 05th May, 2016 help the Radiotherapist in radiotherapy ofof the patient by fabrication of certain devices. These devices are shielding
Published online 30th June, 2016 devices, positioning stents and radiation source carriers. Radiation shielding devices minimize exposure of the
surrounding healthy tissues, positioning devices help in delivering radiation to desired area, while radiation source
Key words: carrier is used for radiation of intraoral localized area. This article aims at displaying the various prostheses that
can be given to oral cancer patients to provide better treatment and decrease post radradiation complications. The use
Radiation prostheses, Radiation stents, of these devices is individualized and close collaboration between the radiotherapist and the prosthodontist is
Head and Neck cancer, Cerroband, essential. Use of these devices minimizes severity of the problems, improves the prognosis and provides comfort to
Radiotherapy. the patient. Radiation therapy is employed by many institutions and the dentist must be aware of the appliances
that can be fabricated to prevent the undesirable side effects of radiation.
Copyright©2016, Dr. Jayant Palaskar et al. This is an open access article distributed under the Creative Commons Att
Attribution License, which permits
unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Citation: Dr. Jayant Palaskar, Dr. Zankhana S. Mody, Dr. ShreyasShreyas S. Mohile, Dr. Jyoti H. Wankhade, Dr. Sayali R. Korde and Dr. Nikita M.
Virdiya, 2016. “Different types of Radiation Prostheses to minimize radiation side-effects”,
side effects”, International Journal of Current Research, 8, (06), 33575-33578.
INTRODUCTION The prosthodontist can actively help in the rehabilitation of
cancer patients by fabricating the whole array of possible
The use of radiation energy has steadily increased since the prosthesis that can be custom made and decrease or prevent the
discovery of X-rays
rays by Roentgen in 1895 and of radium by complications following radiotherapy (Goswami et al., 2013).
Curie in 1898. In the past, lack of knowledge in this type of
radiation too frequently resulted in radiation damage to the Pretreatment
etreatment of Oral Malignancies
patient and to all involved in giving the treatment (Santiago,
1973). Therapeutic responses to intraoral carcinoma include The radiotherapist should consult the dentist before starting
surgery, radiation and chemotherapy. Radiation is divided into radiation therapy in the oral cavity. Complications may
extraoral and intraoral therpy (Kabcenell, 1980). The develop in the tongue, teeth, salivary glands, mucosa, maxillae
radiotherapist should consult the dentist before starting the and mandible. A large number of patients have reported with
radiation therapy in the region of the oral cavity. radiation caries and radionecrosis following the treatment.
Complications may develop in the tongue, teeth, salivary Furthermore, the sense of taste may be impaired, the amount
glands, mucosa, maxilla and mandible. A large number of and consistency of the saliva may be altered and ulcers may be
patients have been reported with radiation caries and produced in the mucosa (San(Santiago, 1965). Rahm and Drane
radionecrosis following treatment. Furthermore, the sense of recommended that the teeth in the field of radiation, those
taste may be impaired, the amount and consistency of saliva periodontally involved, those with extensive carious lesions
may be altered and ulcers may be produced in the mucosa and otherwise questionable teeth be extracted with least
(Santiago, 1973). Prosthesis
thesis used in radiotherapy in the oral possible trauma. They also believed that the teet teeth needing
and paraoral region have been classified by Drane and Rahn as restorations should be treated before radiation therapy and such
locators, carriers and stents (Rahn and Drane, 1967). treatment should be accompanied by topical application of
fluoride before, during and after radiation therapy (Rahn and
*Corresponding author: Zankhana Mody, Department of Prosthodontics and
Crown & Bridge, Sinhgad Dental
ntal College and Hospital, Pune. Drane, 1967).
33576 Dr. Jayant Palaskar et al. Different types of radiation prostheses to minimize radiation side-effects
Radiation therapy in Oral Malignancies Radiation carrier device for edentulous mandible (Figure
2): In this prosthesis, a denture base consisting of radium
Radiation therapy must be directed to the smallest possible needles at the required sites was fabricated by the dentist.
area of the tissue. Dentist can help radiotherapist in treating Afterload radiation carrier device (Figure 3): In this
patients with oral and paraoral lesions. The dentist can make a prosthesis, the dentist provides hollow catheters in
prosthesis that will enable the radiotherapist to provide a better predetermined locations. Once the carrier is in position,
treatment to the patient. Most important the prostheses are radioactive isotopes are threaded into the hollow tubing,
comfortable and immobile while treatment is in process allowing for quick and radiation. The advantages of
(Delclous, 1965). afterload over preload technique (the above two
prostheses), is that, in preload carrier, the radioactive
Post treatment of Oral Malignancies source is positioned within the prosthesis before the carrier
is inserted. This method creates urgency of placement of
Following radiotherapy treatment, dentist should be consulted the prosthesis because the staff members are exposed to
regarding oral problems that may develop. Teeth that become potentially hazardous radiations while performing the
carious need to be restored. Extractions may produce procedure (Derhei et al., 2003).
complications like radionecrosis (Santiago, 1965). Patients
having reduced salivation may be given salivary reservoir
prosthesis by the prosthodontist.
Prosthesis in Radiotherapy
A number of prosthesis made by the dentist help the
radiotherapist in treating patients with malignancies of oral and
paraoral tissues (Santiago, 1965). They can be divided into the
following types: Figure 1.
1. The carrier prosthesis
These prosthesis hold radium or cesium-137 securely in a
planned site during every treatment (Santiago, 1965). These
prosthesis administer radiation to a confined region by means
of capsules, beads or needles of radiation emitting materials.
These carriers are of two types, preloaded carriers and after
loaded carriers. The after loaded carriers are usually
advantageous compared to preloaded carriers as the radioactive
sources are placed after the carrier is in position. Thus
minimizing the radiation exposure to the personnel handling,
positioning and securing such devices. These devices can also
be classified as intracavitory devices and interstitial devices.
Intracavitory devices deliver high doses of radiation to tumours
that are located within 6cm of the skin surface. The doses are
6500-7500 rads for 6-7 weeks. The interstitial devices
(brachytherapy) deliver high doses of radiation for a short
period of time, i.e. 10-15 hours (Goswami et al., 2013). Figure 2.
Interstitial devices place the encapsulated radiation source
(needles, narrow tubes or seeds containing radioactive cesium,
cobalt, gold or iridium) within the tumour or very close to the
surface (Kasat et al., 2010).
Two-piece radiation carrier (Figure 1): Once the
radiotherapist gives the position of the lesion and the
desired field of radiation on the maxillary cast, the
prosthodontist fabricates a two-piece radiation carrier
device which consists of radium needles. The first stent is
constructed on the cast. Grooves are made on this stent to
provide space for the radium needles. Another stent is
made over the first stent and attaches via snap attachment
(magnets, buttons, etc.) The advantage of this prosthesis is
that the radium needles are held securely between the two
stents and can be comfortably worn by the patient for the
required time without dislodgement of the needles
(Kabcenell, 1980). Figure 3.
33577 International Journal of Current Research, Vol. 08, Issue, 06, pp.33568-33574, June, 2016
2. Positioning devices (Figure 4)
Prostheses that displace the movable tissues away from or
towards the source of radiation. Example: the lips, tongue,
cheeks and soft palate may need to be directed away from the
source of radiation to prevent their damage or maybe directed
towards the source when indicated (Santiago, 1965)
Figure 5.
Figure 4.
3. Perioral cone positioning stent (Figure 5, 6)
This prosthesis holds the intraoral cone in a definite position
and also places the tongue away from the field of irradiation
(Goswami et al., 2013; Santiago, 1965) Most intraoral cones in
radiation therapy range from 3-4cm. For treating oral lesions, it Figure 6.
is important that the cone be in contact with the oral mucosa
within the entire perimeter of the treatment field. This is
seldom possible due to varied topography of the mouth (Parel
and Drane, 1975). Whenever there is a space between the
mucosa and the radiation cone, two things may occur: First,
normal tissue outside the radiation field may be irradiated.
Second, the desired dose to the tumour field is diminished by
an amount proportional to the square of the distance between
the end of the metal extension and the tissue (inverse square
rule) (Beder, 1959). Some authors advocated the use of lead
cylinders around the radiation cone to prevent irradiation of
surrounding normal tissues. However, due to hazards
associated with the use of lead, mostly related to its high
melting point and potential toxicity, several alloys that melt at
lower temperatures have been used in place of pure lead for
intraoral shielding. For example, Cerrobend (a bismuth-tin-
lead alloy) is used. Perioral cone positioning stent consists of
three parts: the first part is a cylindrical cone in which the
radiation cone will fit. It is made up of acrylic resin and is 5- Figure 7.
6cm long. The second part consists of a maxillary record base
(edentulous patient) or occlusal indices (dentulous patient). 4. Shielding stent / Protection stent (Figure 7)
The third part consists of another small ring made of cerrobend
alloy which joints the acrylic cone to the denture base A shielding stent of specific thickness of acrylic and
(Santiago, 1975). containing lead or cerrobend can be used to protect structures
33578 Dr. Jayant Palaskar et al. Different types of radiation prostheses to minimize radiation side-effects
which are adjacent to the radiation therapy sites. This prevents procedures, irradiation of the nearby normal tissues including
radiation to the surrounding normal tissues and prevents any the salivary glands can occur, leading to severe consequences.
side effects. Eg: tongue shielding devices, lip shielding devices Prosthodontist can provide radiation prostheses which reduce
(Goswami et al., 2013; Santiago, 1965). When the radiation is or eliminate many oral complications associated with
directed at the buccal mucosa, the skin, mucosa and alveolar radiotherapy. These prostheses reduce the irradiation to the
bone adjacent to it undergo irradiation too. A cheek shielding surrounding normal tissues and thus prevent the adverse
device containing cerrobend can be placed intraorally in the consequences of irradiation. It is thus recommended that
buccal vestibule, thus protecting the intraoral tissues (Aramany a multidisciplinary approach be considered while treating
and Drane, 1972). a patient with head and neck cancer wherein a surgeon,
a radiotherapist and a prosthodontist must be on the team for
5. Radiation measuring stent / Dosimeter positioning consultation before planning the treatment. These measures
stents: will help provide better treatment and improve the quality of
life of the patient.
These prostheses contain lithium fluoride capsules that enable
the radiotherapist to measure radiation received by tissues in REFERENCES
contact with the capsule (Santiago, 1973).
Aramany, M. A. and Drane, J. B. 1972. Radiation protection
6. Tissue recon touring stents prosthesis for edentulous patients. J Prosthet Dent.,
27(3):292-296.
These stents are useful when the beam is adjusted for midlines Beder, O. E. 1959. Surgical and maxillofacial prosthesis,
for treating skin lesions associated with lips. Due to curvature Seattle, The University of Washington Press, P. 25.
of lip, low doses of radiation are delivered at the corner of the Brosky, M., Lee, C., Barlett, T., Lo, S. 2000. Fabrication of
mouth whereas higher doses are delivered at the midline. radiation bolus prosthesis for the maxillectomy patient. J
These stents flatten the lips and the corner of the mouth Prosthet Dent., 83(1):119-120.
thereby placing the entire lip in the same plane and providing Delclous L. Radiotherapy for head and neck cancer teamwork:
equal and exact radiation dose (Goswami et al., 2013). Problems common to physician and dentist. J Prosthet Dent
1965;15:157-167.
Derhei, P. M., Lim, W. C., Timmerman, R. D. and Andres, C.
J. 2003. Use of computed tomography for fabrication of a
custom brachytherapy carrier: A clinical report. J Prosthet
Dent., 89(1):15-18.
Goswami, R., Agarwal, K. and Gaba, N. 2013. Prosthetic
Carriers for Radiation Therapy of Head and Neck. British
Biomedical Bulletin, 1(2):136-146.
Kabcenell, J. L. 1980. A two piece radiation therapy surface
mold. J Prosthet Dent., 43(1):86-88.
Kasat, V., Sahuji, S. and Joshi, M. 2010. Radiotherapy: An
update. JIAOMR, 22(4):26-30.
Mantri, S. S. and Bhasin, A. S. 2010. Preventive
Prosthodontics for Head and Neck Radiotherapy. J
Figure 8. ClinDiagn Res., 4:2958-2962.
Miyamoto, R. H., Fleming, T. J., Davis, M. G. 1992.
7. Tissue bolus compensators / Balloon bolus supporting Radiotherapeutic management of an orocutaneous defect
stents (Figure 8) with a balloon retaining stent. J Prosthet Dent., 68(1):115-
117.
These prostheses help in treatment of superficial lesions of Parel, S. M. and Drane, J. B. 1975. A modified intraoral
face with irregular contours. Due to irregularities in the lesion, prosthesis for directing a radiation beam. J Prosthet Dent.,
some areas within the field maybe untreated while others may 33(6):666-671.
develop isolated hotspots (Mantri and Bhasin, 2010). Bolus is Rahn, A. O. and Drane, J. B. 1967. Dental aspects of the
a tissue equivalent material which is placed directly onto the Problems, Care and Treatment of Irradiated Oral Cancer
irregularities that helps in converting irregular tissue contours Patient. J Am Dent Assoc., 74:957-966.
into flat surfaces which are perpendicular to the central access Santiago, A. 1965. An intraoral stent for the direction of
of the ionizing beam, to thereby more accurately aid in the radiation beam therapy. J Prosthet Dent., 15(5):938-944.
homogenous distribution of the radiation (Brosky et al., 2000). Santiago, A. 1965. Use of intraoral prosthesis in radiotherapy.
Med Rec Ann., 58:3-11.
Conclusion Santiago, A. 1973. The role of the dentist in radiotherapy. J
Prosthet Dent., 30(2):196-201.
Generally patients who have oral cancers have to undergo Santiago, A. 1975. Fabrication of intraoral radiotherapy
surgical resection of the malignant tumour which affects prostheses. J Prosthet Dent., 34(2):212-215.
patient’s quality of life. Radiotherapy plays a significant role in
the treatment modalities of oral cancer. Due to radiation
*******
View publication stats
You might also like
- Attachments Used With Implant Supported Over Denture: Dentistry and Oral HealthDocument5 pagesAttachments Used With Implant Supported Over Denture: Dentistry and Oral HealthAhmad ShoeibNo ratings yet
- 345434Document21 pages345434Ahmad ShoeibNo ratings yet
- PDFDocument4 pagesPDFAhmad ShoeibNo ratings yet
- Neutral Zone Concept and TechniqueDocument6 pagesNeutral Zone Concept and TechniqueJasween KaurNo ratings yet
- PDFDocument4 pagesPDFAhmad ShoeibNo ratings yet
- Marburg Double Crown System For Partial DentureDocument10 pagesMarburg Double Crown System For Partial DentureAhmad Shoeib100% (1)
- 7064 20601 1 PBDocument9 pages7064 20601 1 PBnandillagiofaniearumNo ratings yet
- HTTP WWW - Iusd.iupui - Edu IndexDocument20 pagesHTTP WWW - Iusd.iupui - Edu IndexReema MazenNo ratings yet
- Surveying: British Dental Journal December 2000Document12 pagesSurveying: British Dental Journal December 2000Ahmad ShoeibNo ratings yet
- Saudi Licence Exam For General DentistDocument159 pagesSaudi Licence Exam For General DentistYounus Shaik91% (124)
- Prostho MCQDocument34 pagesProstho MCQSOMVIR KUMAR100% (1)
- QI2012Document13 pagesQI2012Ahmad ShoeibNo ratings yet
- Sensors 16 01244Document10 pagesSensors 16 01244Ahmad ShoeibNo ratings yet
- A 3-Year Follow-Up Study of Overdentures Retained by Mini ImplantDocument7 pagesA 3-Year Follow-Up Study of Overdentures Retained by Mini ImplantAhmad Shoeib100% (1)
- Ijdsr 2 3 6Document4 pagesIjdsr 2 3 6Ahmad ShoeibNo ratings yet
- 2 Dentesits PQR - Oct 15Document28 pages2 Dentesits PQR - Oct 15Ahmad ShoeibNo ratings yet
- Does Mandibular Edentulous Bone Height Affect ProstheticDocument9 pagesDoes Mandibular Edentulous Bone Height Affect ProstheticAhmad ShoeibNo ratings yet
- Management of A Failed Mandibular Staple Implant A Clinical ReportDocument5 pagesManagement of A Failed Mandibular Staple Implant A Clinical ReportAhmad ShoeibNo ratings yet
- 14-19Document6 pages14-19Ahmad ShoeibNo ratings yet
- A Brief Historical Perspective On Dental Implants, Their Surface CoatingsDocument6 pagesA Brief Historical Perspective On Dental Implants, Their Surface CoatingsAhmad ShoeibNo ratings yet
- Omegadyn SensorDocument2 pagesOmegadyn SensorAhmad ShoeibNo ratings yet
- Chrome-Extension Mhjfbmdgcfjbbpaeojofohoefgiehjai Index PDFDocument5 pagesChrome-Extension Mhjfbmdgcfjbbpaeojofohoefgiehjai Index PDFAhmad ShoeibNo ratings yet
- Parametric vs. Non Parametric Tests: To Keep This Site Going, Please Allow Adverts or DonateDocument4 pagesParametric vs. Non Parametric Tests: To Keep This Site Going, Please Allow Adverts or DonateAhmad ShoeibNo ratings yet
- Retention of Maxillary Implant Overdenture Bars of Different DesignsDocument5 pagesRetention of Maxillary Implant Overdenture Bars of Different DesignsAhmad ShoeibNo ratings yet
- Role of Cephalometery in Evaluation of Vertical DimensionDocument4 pagesRole of Cephalometery in Evaluation of Vertical DimensionAhmad ShoeibNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- RMHE08Document2,112 pagesRMHE08Elizde GómezNo ratings yet
- Firestone & Scholl - Cognition Does Not Affect Perception, Evaluating Evidence For Top-Down EffectsDocument77 pagesFirestone & Scholl - Cognition Does Not Affect Perception, Evaluating Evidence For Top-Down EffectsRed JohnNo ratings yet
- Mini-Case 1 Ppe AnswerDocument11 pagesMini-Case 1 Ppe Answeryu choong100% (2)
- Assignment 4 SolutionsDocument9 pagesAssignment 4 SolutionsNengke Lin100% (2)
- Intro Slow Keyofg: Em7 G5 A7Sus4 G C/G D/F# AmDocument2 pagesIntro Slow Keyofg: Em7 G5 A7Sus4 G C/G D/F# Ammlefev100% (1)
- Factors Affecting Physical FitnessDocument7 pagesFactors Affecting Physical FitnessMary Joy Escanillas Gallardo100% (2)
- #Dr. Lora Ecg PDFDocument53 pages#Dr. Lora Ecg PDFمحمد زينNo ratings yet
- RhythmDocument10 pagesRhythmSalcedo NoelNo ratings yet
- Southwest Airlines Final ReportDocument16 pagesSouthwest Airlines Final Reportapi-427311067No ratings yet
- SR6 Core Rulebook Errata Feb 2020Document6 pagesSR6 Core Rulebook Errata Feb 2020yrtalienNo ratings yet
- DNA Mutation and Its Effect To An Individual (w5)Document6 pagesDNA Mutation and Its Effect To An Individual (w5)Cold CoockiesNo ratings yet
- Binet Kamat Test For General Mental AbilitiesDocument54 pagesBinet Kamat Test For General Mental AbilitiesSana Siddiq100% (14)
- 3161 GIS Data ModelsDocument13 pages3161 GIS Data Modelsapi-3788255No ratings yet
- Math 202 Syllabus-Spring18 PDFDocument2 pagesMath 202 Syllabus-Spring18 PDFvonacoc49No ratings yet
- Science Involved in Floating Paper Clip Science Experiment GuidelinesDocument4 pagesScience Involved in Floating Paper Clip Science Experiment GuidelinesSHIELA RUBIONo ratings yet
- Exp6.Single Phase Bridge Inverter Using PWMDocument6 pagesExp6.Single Phase Bridge Inverter Using PWMAbdullah MohammedNo ratings yet
- L2 Biostatistics ProbabilityDocument84 pagesL2 Biostatistics ProbabilityAaron CiudadNo ratings yet
- 10th Aug. 2011 Structural Calculation (For Sub.) - 03Document29 pages10th Aug. 2011 Structural Calculation (For Sub.) - 03Nguyễn Tiến Việt100% (1)
- Igcse Revision BookDocument23 pagesIgcse Revision BookJo Patrick100% (2)
- Index PDFDocument159 pagesIndex PDFHüseyin IşlakNo ratings yet
- YellowstoneDocument1 pageYellowstoneOana GalbenuNo ratings yet
- Genie GS-1930 Parts ManualDocument194 pagesGenie GS-1930 Parts ManualNestor Matos GarcíaNo ratings yet
- YogaDocument116 pagesYogawefWE100% (2)
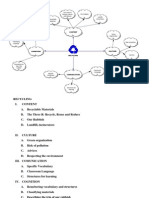
- Recycling Mind MapDocument2 pagesRecycling Mind Mapmsole124100% (1)
- Opex and CapexDocument5 pagesOpex and CapexATM Shafiq Ul AlamNo ratings yet
- Leadership Games and ActivitiesDocument38 pagesLeadership Games and ActivitiesWilliam Oliss100% (1)
- Properties of Matter ReviewDocument8 pagesProperties of Matter Reviewapi-290100812No ratings yet
- Overall Method StatementDocument33 pagesOverall Method Statementsaranga100% (1)
- 7 +Royal+Court+Affairs,+Sultanate+of+OmanDocument12 pages7 +Royal+Court+Affairs,+Sultanate+of+OmanElencheliyan PandeeyanNo ratings yet
- Yadea User Manual For e Scooter 1546004910Document44 pagesYadea User Manual For e Scooter 1546004910Danthe ThenadNo ratings yet